Key Points
Pretreatment near-tetraploidy is associated with advanced Rai stage, deletion of 17p, and complex karyotype.
Pretreatment near-tetraploidy is an independent risk factor for ibrutinib discontinuation via Richter transformation.
Abstract
Ibrutinib is a highly effective targeted therapy for chronic lymphocytic leukemia (CLL). However, ibrutinib must be discontinued in a subset of patients due to progressive CLL or transformation to aggressive lymphoma (Richter transformation). Transformation occurs early in the course of therapy and has an extremely poor prognosis. Thus, identification of prognostic markers associated with transformation is of utmost importance. Near-tetraploidy (4 copies of most chromosomes within a cell) has been reported in various lymphomas, but its incidence and significance in CLL has not been described. Using fluorescence in situ hybridization, we detected near-tetraploidy in 9 of 297 patients with CLL prior to beginning ibrutinib treatment on 1 of 4 clinical trials (3.0%; 95% confidence interval [CI], 1.4%-5.7%). Near-tetraploidy was associated with aggressive disease characteristics: Rai stage 3/4 (P = .03), deletion 17p (P = .03), and complex karyotype (P = .01). Near-tetraploidy was also associated with ibrutinib discontinuation due to Richter transformation (P < .0001), but not due to progressive CLL (P = .41). Of the 9 patients with near-tetraploidy, 6 had Richter transformation with diffuse large B-cell lymphoma. In a multivariable model, near-tetraploidy (hazard ratio [HR], 8.66; 95% CI, 3.83-19.59; P < .0001) and complex karyotype (HR, 4.77; 95% CI, 1.42-15.94; P = .01) were independent risk factors for discontinuing ibrutinib due to transformation. Our results suggest that near-tetraploidy is a potential prognostic marker for Richter transformation to assess in patients going on ibrutinib.
Visual Abstract
Introduction
Ibrutinib is a first-in-class oral covalent inhibitor of Bruton tyrosine kinase (BTK)1 approved to treat chronic lymphocytic leukemia (CLL), mantle cell lymphoma, and Waldenstrom macroglobulinemia. Ibrutinib has rapidly changed the landscape of CLL treatment, with high response rates and prolonged remission durations in both relapsed/refractory CLL and previously untreated patients.2-5 Despite these strides, a subset of patients relapse on ibrutinib. Patients relapse primarily with progressive CLL or Richter transformation, an aggressive transformation into lymphoma, predominantly diffuse large B-cell lymphoma.6 Most patients progressing with CLL acquire mutations in either the C481 ibrutinib-binding pocket of BTK or downstream activating mutations in PLCG2 that bypass the need for signaling through BTK.7,8 However, identifiable resistance mutations are considerably less frequent in patients who progress via disease transformation.6 Identifying prognostic markers associated with Richter transformation is critical at this time as an increasing number of patients have begun to receive ibrutinib and those whose CLL transforms have very aggressive disease and poor prognosis.6,9 Complex karyotype (≥3 unrelated chromosomal abnormalities) has been associated with ibrutinib discontinuation due to progressive CLL or transformation.6,10 In addition, various biomarkers in CLL have been associated with risk of Richter transformation, including inactivation of TP53 or CDKN2A, CMYC abnormalities, NOTCH1 mutation, and CD38 expression.11-16 However, for patients receiving ibrutinib, there are currently no specific risk factors associated with developing Richter transformation.
Near-tetraploidy has been reported as a rare abnormality in various lymphomas, but to our knowledge, its incidence in CLL has not been examined.17,18 Tetraploidy in cancer cells may promote chromosome instability while buffering the cells from the deleterious effects.19 In this study, we examined the presence of near-tetraploidy and its association with discontinuation of ibrutinib for progression, including Richter transformation.
Methods
All patients provided written informed consent to participate in protocols approved by The Ohio State University Cancer Institutional Review Board in accordance with the Declaration of Helsinki. Patient population characteristics and the 4 ibrutinib clinical trials have been described previously.2,3,6,20,21 We retrospectively reviewed fluorescence in situ hybridization (FISH) results to identify near-tetraploid cases. Cytogenetic procedures were performed as previously described22 on peripheral blood or bone marrow collected prior to starting ibrutinib therapy. For each patient, 7 to 10 probes, plus controls, were analyzed (supplemental Table 1). Given our probe set, we defined near-tetraploidy as the presence of 4 or more probes with 4 signals and confirmed each positive case by the presence of at least 1 near-tetraploid cell by karyotype.
Cytogenetic results were available for 297 patients. Baseline variables were compared between patients with and without near-tetraploidy using the Fisher exact test or the Wilcoxon rank-sum test. Time to treatment discontinuation was measured from the date of first treatment until the off-study date. We censored 134 patients who remained on ibrutinib at the date of last contact, and 13 patients who went off study for transplant or went offsite. Cumulative incidence of ibrutinib discontinuation due to progression or histologic transformation was estimated, with discontinuation for other reasons treated as a competing risk. The Gray test was used to test for cumulative incidence differences between groups. Multivariable models were fit using Fine and Gray models.23 Variables considered for model inclusion were age, sex, number of prior therapies, baseline lactate dehydrogenase level, FISH abnormalities [del(17)(p13.1), del(11)(q22.3), trisomy 12, del(13)(q14), MYC gain, and BCL6 gain], complex karyotype, and IGHV mutational status. The multivariable model for transformation adjusted for monotherapy with ibrutinib vs combination therapy with ibrutinib and ofatumumab, regardless of statistical significance. Overall survival (OS) was measured from the date of first treatment with ibrutinib until the date of death, censoring those alive at last follow-up. OS estimates were calculated by the Kaplan-Meier method and differences between curves were tested with the log-rank test. All tests were 2-sided; statistical significance was declared at α = 0.05.
Results
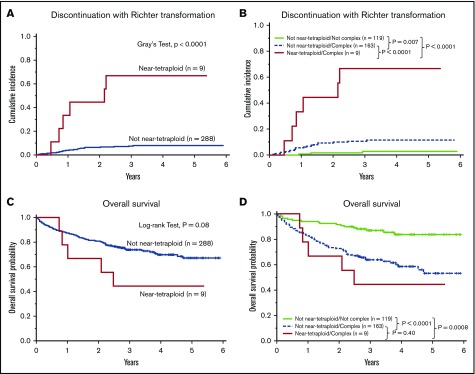
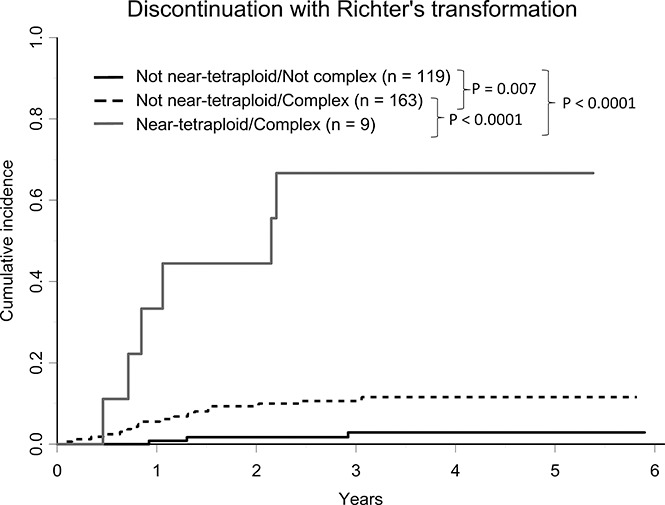
A near-tetraploid clone (supplemental Tables 2-4) was identified in 9 of 297 patients analyzed (3.0%; 95% confidence interval [CI], 1.4%-5.7%). Clinical and molecular characteristics for each of the 9 patients are described in Table 1. Near-tetraploidy was associated with the baseline characteristics Rai stage III/IV (P = .03), deletion 17p13 (P = .03), and complex karyotype (P = .01) (Table 2). With a median follow-up of 3.4 years, 133 patients (45%) remain on therapy, 12 (4%) received transplant or therapy elsewhere, 52 (18%) discontinued ibrutinib due to progressive CLL, 28 (9%) discontinued due to disease transformation, and 72 (24%) discontinued for other adverse events (supplemental Table 5). Among the 9 near-tetraploid patients, 6 have undergone Richter transformation, 1 had progressive CLL, and only 2 remain on treatment at 4.3 and 5.4 years. The estimated cumulative incidence of disease transformation is significantly higher in near-tetraploid patients vs those without near-tetraploidy (P < .0001; Figure 1A; supplemental Table 5), with an estimated cumulative incidence of disease transformation at 3 years of 66.7% (95% CI, 23.5-89.3) and 7.6% (95% CI, 4.8-11.1), respectively. Because all 9 near-tetraploid patients had a complex karyotype and complex karyotype has been associated with progression on ibrutinib,6 cumulative incidence curves are presented for near-tetraploidy and complex karyotype (Figure 1B). Patients with neither abnormality had a low incidence of ibrutinib discontinuation due to transformation. Patients with only complex karyotype had a significantly higher cumulative incidence compared with patients without either feature (P = .007). Patients with both features had a significantly higher cumulative incidence compared with those with only complex karyotype (P < .0001). The importance of these variables was supported by a multivariable model in which both near-tetraploidy (hazard ratio = 8.66; 95% CI, 3.83-19.59; P < .0001) and complex karyotype (hazard ratio = 4.77; 95% CI, 1.42-15.94; P = .01) were independent risk factors for discontinuing ibrutinib due to transformation. Near-tetraploidy was not significantly associated with discontinuation due to progressive CLL (P = .41; supplemental Table 5). Near-tetraploidy showed a trend toward decreased OS (P = .08; Figure 1C; supplemental Table 5). Although the survival curve is lowest in patients who have both near-tetraploidy and complex karyotype and highest in patients with neither feature, the data were insufficient to claim that near-tetraploidy provided prognostic information for OS independent of complex karyotype (P = .40; Figure 1D). The small number of patients with near-tetraploidy and complex karyotype, as well as the presence of 18 patients whose CLL had transformed, and the majority of CLL progressions being in the complex-karyotype-alone subgroup likely contributed to this nonsignificant finding.
Table 1.
Clinical and molecular characteristics of near-tetraploid patients
| Characteristics | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | Patient 7 | Patient 8 | Patient 9 |
|---|---|---|---|---|---|---|---|---|---|
| Classification for discontinuation | CLL | Richter | Richter | Richter | Richter | Richter | Richter | — | — |
| Study | p12024 | p10032 | p10032 | p11133 | p10053 | p12024 | p11133 | p10053 | p10053 |
| Ibrutinib monotherapy | Y | Y | Y | Y | N | Y | Y | N | N |
| Age, y | 60 | 76 | 60 | 69 | 73 | 53 | 52 | 79 | 64 |
| Sex | M | M | M | M | M | F | F | F | F |
| Rai stage | IV | IV | III | IV | IV | IV | IV | IV | IV |
| LDH, U/L | 214 | 375 | 142 | 211 | 765 | 308 | 198 | 356 | 227 |
| Elevated LDH | Y | Y | N | Y | Y | Y | Y | Y | Y |
| No. of prior therapies | 4 | 5 | 5 | 3 | 5 | 3 | 8 | 5 | 2 |
| Gain of BCL6 | Y | N | N | N | Y | N | N | N | N |
| Gain of MYC | Y | N | N | Y | N | Y | Y | N | N |
| Trisomy 12 | Y | N | N | Y | N | Y | N | Y | N |
| del(13q) | Y | N | Y | N | N | N | N | Y | Y |
| del(11q) | N | N | Y | N | N | N | N | Y | N |
| del(17p) | Y | Y | N | Y | N | Y | Y | Y | Y |
| Complex karyotype | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| IGHV | UM | UM | UM | UM | Unknown | Unknown | UM | UM | UM |
| Time to discontinuation or last contact, y | 2.50 | 2.15 | 1.06 | 0.85 | 0.46 | 0.71 | 2.20 | 5.38 | 4.33 |
| Richter treatment | — | R + DXM | OFAR | R-EPOCH | R-EPOCH | Unknown | Unknown | — | — |
| OS, y | 3.77 | 2.48 | 2.08 | 1.01 | 0.83 | 0.73 | 3.97 | 5.38 | 4.33 |
| Survival status | A | D | D | D | D | D | A | A | A |
—, Not applicable; A, alive; D, dead; del, deletion; F, female; LDH, lactate dehydrogenase; M, male; N, no; OFAR, oxaliplatin, fludarabine, cytarabine, and rituximab; R + DXM, rituximab and dexamethasone; R-EPOCH, rituximab, etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin; UM, unmutated; Y, yes.
Table 2.
Near-tetraploidy is associated with aggressive disease characteristics
| Characteristic | Total, n = 297 | Not tetraploid, n = 288 | Tetraploid, n = 9 | P |
|---|---|---|---|---|
| Study, no. (%) | .25 | |||
| OSU-10032 | 48 (16) | 46 (16) | 2 (22) | |
| OSU-10053 | 68 (23) | 65 (23) | 3 (33) | |
| OSU-11133 | 145 (49) | 143 (50) | 2 (22) | |
| OSU-12024 | 36 (12) | 34 (12) | 2 (22) | |
| Monotherapy with ibrutinib, no. (%) | .43 | |||
| No | 68 (23) | 66 (23) | 3 (33) | |
| Yes | 229 (77) | 223 (77) | 6 (67) | |
| Age, y | .85 | |||
| Median | 65 | 65 | 64 | |
| Range | 26-91 | 26-91 | 52-79 | |
| Sex, no. (%) | .29 | |||
| Male | 211 (71) | 206 (72) | 5 (56) | |
| Female | 86 (29) | 82 (28) | 4 (44) | |
| Rai stage, no. (%) | .03 | |||
| 0/I/II | 101 (34) | 101 (35) | 0 (0) | |
| III/IV | 196 (66) | 187 (65) | 9 (100) | |
| LDH, U/L | .19 | |||
| Median | 220 | 220 | 227 | |
| Range | 96-1485 | 96-1485 | 142-765 | |
| No. of prior therapies | .12 | |||
| Median | 3 | 3 | 5 | |
| Range | 0-16 | 0-16 | 2-8 | |
| Gain of BCL6, no. (%) | .15 | |||
| No | 274 (92) | 267 (93) | 7 (78) | |
| Yes | 23 (8) | 21 (7) | 2 (22) | |
| Gain of CMYC, no. (%) | . | .09 | ||
| No | 235 (79) | 230 (80) | 5 (56) | |
| Yes | 62 (21) | 58 (20) | 4 (44) | |
| Trisomy 12, no. (%) | .05 | |||
| No | 245 (82) | 240 (83) | 5 (56) | |
| Yes | 52 (18) | 48 (17) | 4 (44) | |
| Del(13q), no. (%) | .75 | |||
| No | 145 (49) | 140 (49) | 5 (56) | |
| Yes | 152 (51) | 148 (51) | 4 (44) | |
| Del(11q), no. (%) | 1.00 | |||
| No | 214 (72) | 207 (72) | 7 (78) | |
| Yes | 83 (28) | 81 (28) | 2 (22) | |
| Del(17p), no. (%) | .03 | |||
| No | 177 (60) | 175 (61) | 2 (22) | |
| Yes | 120 (40) | 113 (39) | 7 (78) | |
| Complex karyotype, no. (%) | .01 | |||
| No | 119 (41) | 119 (42) | 0 (0) | |
| Yes | 172 (59) | 163 (58) | 9 (100) | |
| IGHV, no. (%) | .35 | |||
| Mutated | 53 (20) | 53 (21) | 0 (0) | |
| Unmutated | 212 (80) | 205 (79) | 7 (100) | |
Associations between near-tetraploidy and demographic, clinical, and molecular variables. Associations were tested using the Fisher exact for categorical variables and Wilcoxon rank-sum tests for continuous variables.
Figure 1.
Near-tetraploidy is associated with Richter transformation on ibrutinib. (A) Cumulative incidence curves for transformation on ibrutinib with and without near-tetraploidy. (B) Cumulative incidence curves for transformation by near-tetraploidy and complex karyotype status. (C) Kaplan-Meier curves of OS for patients with or without near-tetraploidy. (D) Kaplan-Meier curves of OS by near-tetraploidy and complex karyotype status.
Discussion
As a retrospective study, there are several limitations. The sampling time varied from days to months before beginning treatment. Because serial samples were unavailable for most patients, we were unable to determine whether the frequency of the near-tetraploid clones changed during treatment, or if gain of near-tetraploidy after starting treatment is associated with Richter transformation. We were also unable to assess whether the transformed lymphoma was clonally related to the preceding CLL. To address these questions, it would be useful to monitor patients serially for near-tetraploidy before and throughout treatment, as well as analyze lymph node tissue at the time of transformation. Interestingly, in 3 near-tetraploid patients with FISH results available near the time of transformation, the near-tetraploid clone was still present, whereas for the 2 patients who have not progressed, the near-tetraploid clone is no longer detectable.
Our study suggests that near-tetraploidy may be a prognostic marker for progression on ibrutinib through Richter transformation and provides rationale for further interrogation of this biomarker in CLL. It will be important to confirm the relationship with Richter transformation on ibrutinib in a second, independent cohort, as well as to examine the frequency and clinical associations of near-tetraploidy with transformation in other settings (eg, other therapies, at diagnosis, etc). Using FISH probes for regions prone to variation in CLL complicates the identification and quantification of near-tetraploidy, thus there is a need for further research to optimize detection. Near-tetraploid cells are typically unstable and this may serve as a mechanism for generating diverse subclones that could promote transformation in CLL. Future studies to interrogate downstream effects and identify the mechanisms driving near-tetraploidy in CLL are of considerable interest.
Supplementary Material
The full-text version of this article contains a data supplement.
Acknowledgments
This work was supported by the D. Warren Brown Foundation, Michael and Judy Thomas, the Four Winds Foundation, The Leukemia & Lymphoma Society, an American Society of Clinical Oncology Young Investigator Award, an American Society of Hematology Scholar Award, the National Institutes of Health, National Institute of General Medical Sciences (T32 GM068412), and National Cancer Institute (R01 CA197870, R01 CA183444, R01 CA177292, K23 CA178183, P50 CA140158, P01 CA095426, R35 CA197734, and R01 CA182905). Clinical trials were funded all or in part by Pharmacyclics.
Authorship
Contribution: C.R.M., A.S.R., J.A.W., and J.C.B. wrote the manuscript; C.R.M., A.S.R., N.A.H., K.J.M., J.L., H.B., G.L., J.S.B., K.A.R., F.T.A., W.Z., A.L.G., J.A.J., J.M.F., S.M.J., L.A.A., K.A.B., M.R.G., A.J.J., L.V.A., E.K.H., J.A.W., and J.C.B. collected and analyzed data, reviewed the paper, and approved the final version; and J.A.W. and J.C.B. supervised the study.
Conflict-of-interest disclosure: M.R.G. is a paid consultant for Pharmacyclics. The remaining authors declare no other competing financial interests.
Correspondence: John C. Byrd, The Ohio State University, 455B OSUCCC, 410 West 12th Ave, Columbus, OH 43210; e-mail: john.byrd@osumc.edu.
References
- 1.Honigberg LA, Smith AM, Sirisawad M, et al. . The Bruton tyrosine kinase inhibitor PCI-32765 blocks B-cell activation and is efficacious in models of autoimmune disease and B-cell malignancy. Proc Natl Acad Sci USA. 2010;107(29):13075-13080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Byrd JC, Furman RR, Coutre SE, et al. . Targeting BTK with ibrutinib in relapsed chronic lymphocytic leukemia. N Engl J Med. 2013;369(1):32-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Byrd JC, Brown JR, O’Brien S, et al. ; RESONATE Investigators. Ibrutinib versus ofatumumab in previously treated chronic lymphoid leukemia. N Engl J Med. 2014;371(3):213-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’Brien S, Furman RR, Coutre SE, et al. . Ibrutinib as initial therapy for elderly patients with chronic lymphocytic leukaemia or small lymphocytic lymphoma: an open-label, multicentre, phase 1b/2 trial. Lancet Oncol. 2014;15(1):48-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Byrd JC, Furman RR, Coutre SE, et al. . Three-year follow-up of treatment-naïve and previously treated patients with CLL and SLL receiving single-agent ibrutinib. Blood. 2015;125(16):2497-2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maddocks KJ, Ruppert AS, Lozanski G, et al. . Etiology of ibrutinib therapy discontinuation and outcomes in patients with chronic lymphocytic leukemia. JAMA Oncol. 2015;1(1):80-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu TM, Woyach JA, Zhong Y, et al. . Hypermorphic mutation of phospholipase C, γ2 acquired in ibrutinib-resistant CLL confers BTK independency upon B-cell receptor activation. Blood. 2015;126(1):61-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Woyach JA, Furman RR, Liu TM, et al. . Resistance mechanisms for the Bruton’s tyrosine kinase inhibitor ibrutinib. N Engl J Med. 2014;370(24):2286-2294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jain P, Keating M, Wierda W, et al. . Outcomes of patients with chronic lymphocytic leukemia after discontinuing ibrutinib. Blood. 2015;125(13):2062-2067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Woyach JA, Ruppert AS, Guinn D, et al. . BTK(C481S)-mediated resistance to ibrutinib in chronic lymphocytic leukemia. J Clin Oncol. 2017;35(13):1437-1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jain P, O’Brien S. Richter’s transformation in chronic lymphocytic leukemia. Oncology (Williston Park). 2012;26(12):1146-1152. [PubMed] [Google Scholar]
- 12.Scandurra M, Rossi D, Deambrogi C, et al. . Genomic profiling of Richter’s syndrome: recurrent lesions and differences with de novo diffuse large B-cell lymphomas. Hematol Oncol. 2010;28(2):62-67. [DOI] [PubMed] [Google Scholar]
- 13.Chigrinova E, Rinaldi A, Kwee I, et al. . Two main genetic pathways lead to the transformation of chronic lymphocytic leukemia to Richter syndrome. Blood. 2013;122(15):2673-2682. [DOI] [PubMed] [Google Scholar]
- 14.Rossi D, Cerri M, Capello D, et al. . Biological and clinical risk factors of chronic lymphocytic leukaemia transformation to Richter syndrome. Br J Haematol. 2008;142(2):202-215. [DOI] [PubMed] [Google Scholar]
- 15.Rossi D, Spina V, Deambrogi C, et al. . The genetics of Richter syndrome reveals disease heterogeneity and predicts survival after transformation. Blood. 2011;117(12):3391-3401. [DOI] [PubMed] [Google Scholar]
- 16.Fabbri G, Khiabanian H, Holmes AB, et al. . Genetic lesions associated with chronic lymphocytic leukemia transformation to Richter syndrome. J Exp Med. 2013;210(11):2273-2288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ott G, Kalla J, Ott MM, et al. . Blastoid variants of mantle cell lymphoma: frequent bcl-1 rearrangements at the major translocation cluster region and tetraploid chromosome clones. Blood. 1997;89(4):1421-1429. [PubMed] [Google Scholar]
- 18.Kaneko Y, Rowley JD, Variakojis D, et al. . Prognostic implications of karyotype and morphology in patients with non-Hodgkin’s lymphoma. Int J Cancer. 1983;32(6):683-692. [DOI] [PubMed] [Google Scholar]
- 19.Storchova Z, Kuffer C. The consequences of tetraploidy and aneuploidy. J Cell Sci. 2008;121(Pt 23):3859-3866. [DOI] [PubMed] [Google Scholar]
- 20.Jaglowski SM, Jones JA, Flynn JM, et al. A phase 1b/2 study evaluating activity and tolerability of the BTK inhibitor ibrutinib in combination with ofatumumab in patients with chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) and related diseases [abstract]. J Clin Oncol. 2014;32(suppl 15). Abstract 7009. [Google Scholar]
- 21.Maddocks K, Flynn J, Andritsos L, et al. . A phase 2 study of the BTK inhibitor ibrutinib in genetic risk-stratified relapsed and refractory patients with chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL) [abstract]. Haematologica. 2014;99(suppl 1). Abstract 522. [Google Scholar]
- 22.Muthusamy N, Breidenbach H, Andritsos L, et al. . Enhanced detection of chromosomal abnormalities in chronic lymphocytic leukemia by conventional cytogenetics using CpG oligonucleotide in combination with pokeweed mitogen and phorbol myristate acetate. Cancer Genet. 2011;204(2):77-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496-509. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.