Abstract
Escherichia coli is the leading cause of Gram-negative neonatal septicemia in the United States. Invasion and passage across the neonatal gut after ingestion of maternal E. coli strains produce bacteremia. In this study, we compared the virulence properties of the neonatal E. coli bacteremia clinical isolate SCB34 with the archetypal neonatal E. coli meningitis strain RS218. Whole-genome sequencing data was used to compare the protein coding sequences among these clinical isolates and 33 other representative E. coli strains. Oral inoculation of newborn animals with either strain produced septicemia, whereas intraperitoneal injection caused septicemia only in pups infected with RS218 but not in those injected with SCB34. In addition to being virulent only through the oral route, SCB34 demonstrated significantly greater invasion and transcytosis of polarized intestinal epithelial cells in vitro as compared to RS218. Protein coding sequences comparisons highlighted the presence of known virulence factors that are shared among several of these isolates, and revealed the existence of proteins exclusively encoded in SCB34, many of which remain uncharacterized. Our study demonstrates that oral acquisition is crucial for the virulence properties of the neonatal bacteremia clinical isolate SCB34. This characteristic, along with its enhanced ability to invade and transcytose intestinal epithelium are likely determined by the specific virulence factors that predominate in this strain.
Introduction
Escherichia coli is the most common Gram-negative bacterium causing neonatal sepsis in the United States. E. coli now surpasses group B streptococcus as the most common cause of neonatal bacteremia in premature newborns and in otherwise normal febrile infants [1–3]. Mortality in newborns with E. coli bacteremia is as high as 40% [4], and meningitis is often a devastating consequence associated with severe neurodevelopmental disabilities in survivors [5]. There is currently no vaccine or any other preventive strategy to control neonatal E. coli sepsis. The incidence of this disease continues to increase and rising antibiotic resistance rates are a public health concern as well since this drastically limits treatment options [6].
The pathogenesis of E. coli bacteremia in newborns is not well understood. Bacterial passage across the neonatal gut after ingestion of maternal E. coli strains around the time of delivery likely is an early step in pathogenesis, as it has been demonstrated in animal models [7, 8]. Neonatal E. coli strains invade and transcytose intestinal epithelial cells prior to septicemia [9, 10]. Although several E. coli virulence factors important for invasion of the blood-brain barrier have been characterized, including the K1 capsule, OmpA, IbeA, Cnf1, and NlpI [11–14], those that contribute to intestinal translocation and neonatal septicemia prior to, or in the absence of meningitis, have not been studied in detail.
We have recently compared the in vitro intestinal invasion ability of several neonatal E. coli bacteremia isolates and demonstrated that some strains invaded intestinal epithelium significantly better than others [15]. Strains that belonged to the increasingly prevalent multi-locus sequence type (ST) 131 were significantly more invasive than those within other STs. Clinical isolate SCB34 was identified among the high invasive ST131 group. Here, we have focused on this contemporary, non-K1 strain and investigated its virulence in newborn animals, its ability to transcytose across polarized intestinal epithelium, and compared its genome to the archetypal meningitic strain RS218. Our results provide evidence that the virulence of SCB34 is dependent on the oral route of inoculation. This is in contrast to RS218, which is fully virulent following introduction into neonatal rats by either oral or intraperitoneal inoculation. Interestingly, SCB34 also was found to be significantly more efficient in traversing polarized intestinal epithelium by transcytosis than strain RS218. Finally, a comparison of the genomes between SCB34 and RS218 revealed the presence of candidate virulence factors in SCB34 not found in RS218 that may be related to the specific virulence properties and increased invasiveness after oral inoculation of this unique clinical isolate.
Materials and methods
E. coli strains and intestinal epithelial cells
SCB34 is a neonatal bacteremia E. coli clinical isolate recovered from a septic newborn as previously described, which was formerly referred to as strain 10 in a prior study [15]. SCB34 is an ST 131 H30 strain that demonstrated resistance to multiple antibiotics including ciprofloxacin and gentamicin, and a high invasion phenotype [16]. RS218 is an archetypal E. coli K1 strain that was isolated from the cerebrospinal fluid of a neonate with meningitis [17]. E. coli laboratory strain DH5α has been described [18]. T84 intestinal epithelial cells were obtained from the American Type Culture Collection (cell line CCL-248). T84 cells were maintained in a 1:1 mixture of Dulbecco's modified Eagle's medium and Ham's F-12 medium (Gibco, Invitrogen; Carlsbad, CA) and 100 U/ml penicillin, 100 μg/ml streptomycin supplemented with 5% (v/v) fetal bovine serum, and incubated at 37°C, 5% CO2. Upon full confluency, T84 cells develop tight junctions and differentiate into polarized monolayers when grown in vitro. The development of T84 epithelial polarization was determined by an increase of transepithelial electrical resistance as described [19].
Newborn rat models of bacteremia
Two distinct models were used to compare the virulence properties of SCB34 and RS218 in newborn animals. DH5α was used as a control nonpathogenic strain. Outbred pregnant Sprague-Dawley rats with timed conception (Charles River Laboratories International Inc., Wilmington, MA) gave birth 7–9 days after arrival in our vivarium. For oral inoculation experiments, newborn (22 to 26 hour-old pups) were randomly cross-fostered among litters prior to receiving each 105 CFU of mid-log bacteria grown in lysogeny broth (LB) medium. The inoculum was mixed in a 10 μL aliquot of PBS/0.1% gelatin and was administered orally with a sterile micropipette in a nontraumatic manner, allowing the pup to actively suck and swallow. Pups were assessed twice daily for signs of illness, and for up to seven days post-infection (p.i.). Humane endpoints were used in these animal experiments, and pups were monitored for possible signs of rapid progression of bacteremia which included: Labored breathing, hypothermia to touch, lethargy, gross weight loss or poor feeding, immobility/loss of righting reflex, or severe tremor. If any of these signs were present, pups were humanely euthanized prior to 7 days. Any mortality was recorded throughout the experiment, and on day 7 p.i. blood was collected to determine the presence of bacteremia. For intraperitoneal experiments, pups of similar age as above were injected with 102 CFU of each strain intraperitoneally (IP). The inoculum was grown in identical fashion and was mixed in a 50 μL PBS/0.1% gelatin aliquot that was injected IP. Identical humane endpoints were also used for the IP animal experiments. The pups were observed twice daily for up to 3 days p.i., and 50 μL of blood was then collected for determination of bacteremia prior to euthanasia after this observation period. In both models, groups of 10 pups per strain were tested. All animals were anesthetized with inhaled isoflurane prior to blood collection to minimize suffering. Humane euthanasia was performed by CO2 inhalation. No unexpected deaths occurred, as all deaths were attributed to bacteremia. The proportion of mortality or bacteremia in each group was compared using the chi-square or Fisher’s test as appropriate; a p value <0.05 was considered significant. All animal experiments were performed with the approval and in strict accordance with the recommendations of the University of Oklahoma Institutional Animal Care and Use Committee (IACUC), under protocol number 15-099-I.
Intestinal epithelial cell invasion assays
To confirm the ability of SCB34 and RS218 to invade intestinal epithelium in vitro, invasion assays were performed similarly to previously described [15], using a modified gentamicin protection assay. The modifications were done taking into account SCB34’s resistance to gentamicin but susceptibility to amikacin, and to improve the efficiency of our methods. Briefly, T84 intestinal epithelial cells were grown to 75 to 80% confluence in 24-well tissue culture plates. Prior to infection, antibiotic-free tissue culture media was substituted overnight. Each E. coli strain was grown to mid-logarithmic phase in tissue culture media (TCM) and 106 CFU of each E. coli isolate were used to infect triplicate wells for an approximate multiplicity of infection of 10 per well. After centrifugation at 800 xg for 5 minutes at 4°C, the infected epithelial monolayers were incubated for 1 hour at 37°C, 5% CO2, to allow bacteria to invade. The monolayers were then washed and treated with amikacin at a concentration of 200 μg/mL (Sigma-Aldrich; St. Louis, MO) for two additional hours to kill extracellular bacteria. After antibiotic treatment, the T84 cells were washed, lysed with 0.1% Triton X-100, and the recovered intracellular bacteria were quantified. The percent invasion was calculated as follows: (CFU recovered/CFU inoculated) x 100. Mean invasion percent was compared among the strains using one-way ANOVA comparisons; a p value <0.05 was considered significant.
In vitro bacterial transcytosis assay
A transcytosis assay was used to assess the ability of the clinical isolates to translocate across polarized T84 cells. T84 cells (104, passage 7–10) were seeded onto 0.3-cm2 growth area semipermeable filter supports with 3.0 μm pores (Corning; Corning, NY). Cells were cultured for 7–14 days until becoming fully confluent and polarized, showing a transepithelial electrical resistance (TEER) of ≥ 1000 Ohm·cm2 measured by a voltmeter and companion electrodes (World Precision Instruments; Sarasota, FL) [20]. Inserts with polarized T84 cells were transferred to antibiotic-free TCM overnight and then were infected on the apical side with 105 mid-log CFU E. coli per insert mixed in antibiotic-free TCM containing 1 mg/mL of fluorescein isothiocyanate (FITC)-dextran 4000Da (FD4) (Sigma-Aldrich; St. Louis, MO) [21]. Non-infected inserts were included as additional controls. The inserts were maintained at 37°C, 5% CO2 throughout the experiment. At 30-minute intervals, the inserts were transferred to collecting wells containing fresh sterile antibiotic-free TCM, and the collecting well TCM from the previous time point was retrieved for CFU quantification on LB agar plates. After the last time point at 6 hours p.i., FD4 concentrations were also determined using the Tecan Infinite® 200 PRO Microplate Fluorescence Reader (Tecan; Männedorf, Switzerland). FD4 measurements allowed us to compare the permeability to this small molecule of the polarized infected T84 cells to that of non-infected monolayers. Baseline and post-infection TEER values were also obtained. Each strain was tested in groups of 5–6 inserts per experiment, in 3 separate experiments. The amount of transcytosed CFU after infection with each strain was analyzed using a mixed-distribution Bayesian model to account for the presence of zeroes, and the variable number of inserts per experiment. An adapted repeated measures, zero-inflation Poisson (ZIP) model [22] fit the data best. The initial, structural zeroes from the ZIP model were analyzed using a discrete-time logistic regression model predicting time until first translocation, and all subsequent well outputs were analyzed using a generalized linear model predicting piece-wise growth for a Poisson outcome. Models were fit using MCMC estimation in WinBUGS [23]. A log-transformation was applied to sum of one plus each data observation. Bayesian 95% confidence intervals were used to determine statistical significance (i.e., intervals for significant contrasts did not contain zero).
Growth curve comparisons in lysogeny broth (LB) and tissue culture media
Growth was compared between SCB34 and RS218 in the two different media that were used in the in vitro and in vivo experiments described above. A single colony from each strain grown overnight on LB agar was used to inoculate 5 mL of either LB or TCM that were incubated overnight at 37°C with shaking at 250 rpm. A 1:100 dilution of these overnight cultures was incubated in either LB or TCM for 2 hours at 37°C, 250 rpm. The two-hour cultures were pelleted by centrifugation and resuspended to an optical density (OD) at 605 nm of 0.7 using LB or TCM as appropriate before inoculating fresh LB or TCM (0.1% v/v). Growth curves were performed in 300 μL volumes with five replicates for each growth condition in each individual experiment. OD measurements were taken at 600 nm at thirty-minute intervals with the Bioscreen C Microbiology Reader (Oy Growth Curves AB Ltd.; Helsinki, Finland) set to incubate at 37°C with constant shaking (machine setting “low”). In addition to OD measurements, growth curves in either LB or TCM were performed for each isolate by CFU plate quantification at 30-min intervals. One-way repeated measures ANOVA was used to compare OD values between the strains. A p value <0.05 was considered significant.
Sequence analysis and comparison among E. coli isolates
To identify and compare the gene content of SCB34 and RS218, we first performed whole-genome sequencing of these two isolates on an Illumina MiSeq using a 250-bp paired-end library. The paired end reads were assembled de novo using the A5 assembly pipeline and annotation was performed using RAST or the National Center for Biotechnology Information (NCBI) Prokaryotic Genomes Annotation Pipeline, respectively [16, 24]. We then compiled a database of SCB34, RS218 and the annotated genomes from 33 phylogenetically diverse strains representative of all E. coli strains deposited in GenBank. Clusters of putative orthologous proteins were generated for all strains examined using CD-hit [25]. The sequence identity threshold utilized was 80% across 80% of the total protein length while all other parameters remained at the default values on CD-hit. From the CD-hit output, a database was generated that contained 22,084 clusters including between 1 and 35 genomes per cluster. Using python scripts, the orthologous protein cluster results from CD-hit were organized into a genome versus protein cluster tables in which the presence or absence of an ortholog in a given genome is identified with either a 1 or 0, respectively. Heatmaps were created from comparison tables using the gplots package in R (version 2.17.0 [http://CRAN.R-project.org/package=gplots]), employing hierarchical clustering to compare rows and columns and to construct the dendrograms. The list of the 22,438 clusters that were included in the CD-hit output, and their respective accession numbers are detailed in S1 Table.
Cluster sequences identified with CD-hit were manually curated by searching the NCBI Microbial Genomes database using the Basic Local Assignment Search Tool (BLAST) and querying all representative genomes, optimizing for highly similar sequences (Megablast).
Results
Clinical E. coli isolates SCB34 and RS218 display unique oral and intraperitoneal virulence phenotypes
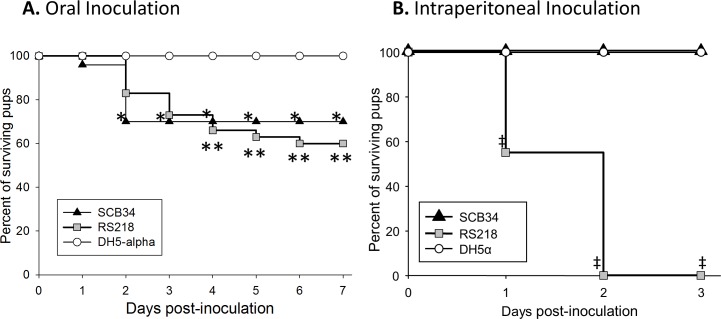
To compare the virulence of SCB34 and RS218 in newborn animals, individual groups of neonatal rats were inoculated orally with either clinical isolate, or the nonpathogenic DH5α strain (Fig 1). Oral inoculation with SCB34 or RS218 resulted in comparable mortality of 30% and 40%, respectively, which was significantly higher than in animals inoculated with DH5α, which demonstrated no illness (Fig 1A). Among surviving animals on day 7 after oral inoculation, bacteremia was present in 14% and 39% of those infected with SCB34 or RS218, respectively (p = ns,S7 Table), and in none infected orally with DH5α. In contrast, IP infection of neonatal pups with SCB34 or DH5α produced no mortality, whereas IP inoculation with RS218 killed all animals within two days (Fig 1B). Bacteremia in survivors 3 days after IP inoculation with SCB34 or DH5α was not significantly different (S7 Table).
Fig 1. Virulence in newborn rats after inoculation with neonatal E. coli isolates SCB34 or RS218.
1A. Animals were inoculated orally and survival post-inoculation is shown (data from three separate experiments, n = 10 animals per group, per experiment). *p<0.05 SCB34 vs. DH5α, **p<0.03 RS218 vs. DH5α. 1B. Survival after intraperitoneal inoculation (data from two separate experiments, n = 10 animals per group, per experiment). ‡p < .001 RS218 vs. SCB34 or RS218 vs. DH5α.
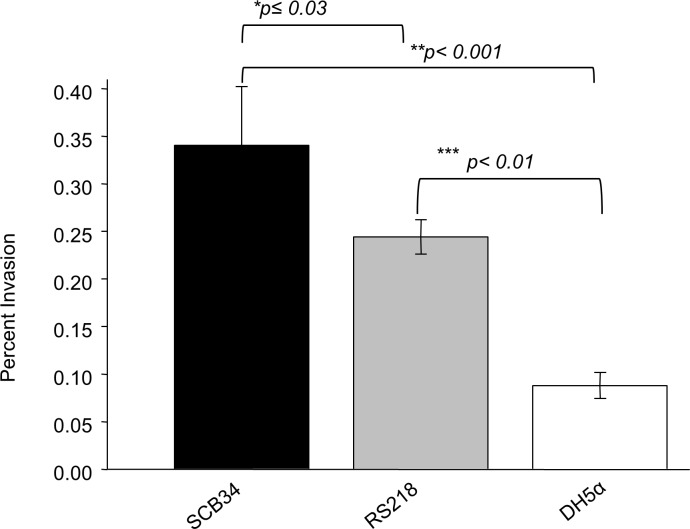
Invasion of intestinal epithelial cells in vitro by neonatal E. coli clinical isolates
We next examined the invasion capacity of SCB34 as compared to RS218. The non-pathogenic laboratory strain DH5α was used as a negative control. In contrast to the results of the virulence assays above, strain SCB34 was significantly more invasive compared to the pathogenic RS218 strain (p≤0.03) and also more invasive than the DH5α laboratory strain (p<0.001) (Fig 2). As expected, RS218 was more invasive than the nonpathogenic DH5α (p<0.01).
Fig 2. Invasion of intestinal T84 epithelial cells by SCB34 and RS218.
The nonpathogenic laboratory strain DH5α was used as control. SCB34 demonstrated the highest invasion ability among the three strains. *SCB34 vs. RS218 (p≤0.03); **SCB34 vs. and DH5α (p<0.001); and ***RS218 vs. DH5α (p<0.01).
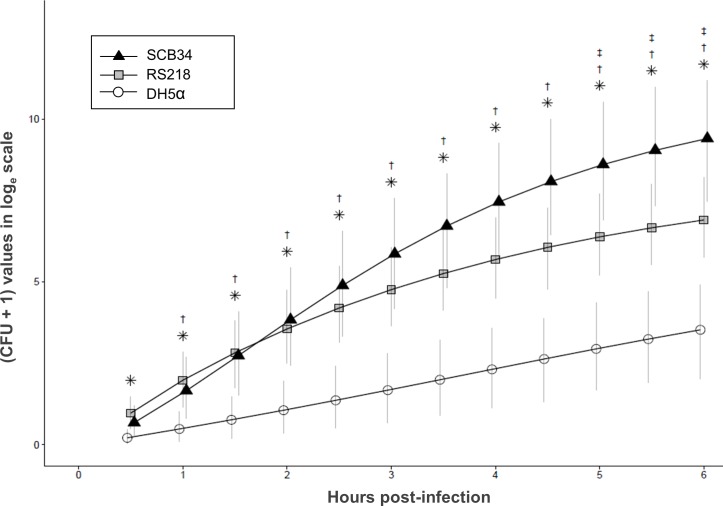
Transcytosis comparisons of neonatal E. coli clinical isolates across polarized intestinal epithelial cells
SCB34 and RS218 were compared regarding their in vitro ability to transcytose polarized intestinal epithelium. Polarized T84 cells grown on permeable inserts were inoculated with both isolates and the number of bacteria recovered in the collecting wells was compared over time. Fig 3 shows the calculated cumulative number of CFU at each 30-min time point after apical inoculation of polarized T84 cells with each strain. Significantly greater numbers of cumulative CFU were recovered from collecting wells of polarized epithelia infected with RS218 or SCB34, starting at 0.5 and 1 hrs. p.i., respectively, as compared to the noninfectious control strain DH5α. When comparing SCB34 and RS218, significantly greater cumulative amounts of CFU transcytosed from SCB34 infected inserts starting at 5 hrs. p.i.. The amount of FD4 recovered at the end of the 6 h incubation in the collecting wells of inserts infected with each E. coli strain was no different compared to non-infected inserts, which indicates that the paracellular permeability of the polarized epithelium did not increase after infection. These results suggest that the bacteria recovered from all inserts passed across the polarized intestinal cell barrier via the transcellular (not the paracellular) route. The integrity of the polarized monolayers throughout the infection process was further corroborated by measuring TEER values at the end of the 6 h incubation, which were maintained through this time point p.i..
Fig 3. Transcytosis of E. coli clinical isolates across polarized intestinal epithelial cells.
*p<0.05 RS218 vs. DH5−α; † p<0.05 SCB34 vs. DH5−α; ‡ p<0.05 SCB34 vs. RS218. Model−calculated mean of cumulative loge (CFU+1) values over time are shown. Error bars reflect 95% Bayesian confidence intervals. Points were jittered to improve clarity (combined data from three separate experiments).
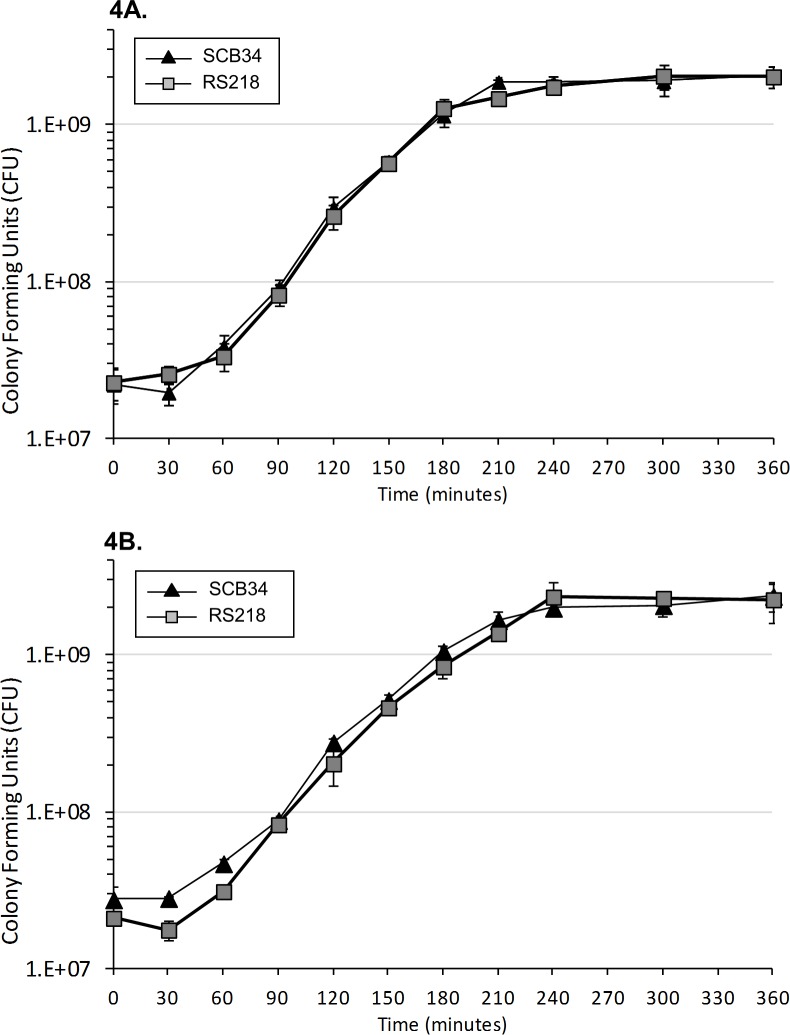
Growth curves of neonatal E. coli isolates
The animal experiments, and tissue culture assays were performed with bacteria from mid-logarithmic phase cultivated in either LB or TCM, respectively. We confirmed that the rate and extent of growth of SCB34 and RS218 was indistinguishable, when measured either by viable count (Fig 4A and 4B) or by optical density, indicating that the differences observed in invasion, virulence, and transcytosis were not likely the result of differences in growth rates among the strains examined.
Fig 4. Growth curves of neonatal E. coli clinical isolates RS218 and SCB34.
Growth curves performed in (4A) LB media and (4B) tissue culture media (TCM) by plate counts. Each plot shows mean CFU values in triplicate samples per time point of each individual clinical isolates. Error bars represent one standard deviation.
Whole-genome comparisons between SCB34, RS218 and other representative E. coli isolates
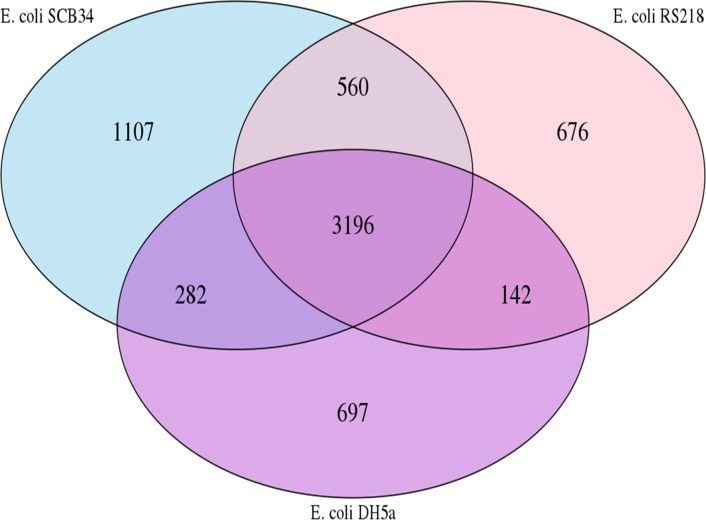
To begin to understand the basis for the phenotypic differences between SCB34 and RS218, we compared the protein coding sequences of these two strains [16, 24] using DH5α as a nonpathogen for comparison. The rationale for this comparison is that the protein coding capacity within each genome largely represents the biologically functional capacity for each strain (regulatory RNAs and non-coding regulatory sequences notwithstanding). Fig 5 displays a comparison of all protein coding sequences found in SCB34, RS218, and DH5α in a Venn diagram. Surprisingly, the number of protein coding sequences unique to strain SCB34 (1,107) was almost twice the number unique to either RS218 (676) or DH5α (697), and so this comparison suggested a greater functional complexity of SCB34 compared to the archetypal neonatal isolate RS218.
Fig 5. Comparison of gene distribution among SCB34, RS218, and DH5α.
The Venn diagram shows genes that are common or unique genes in each isolate. The unique proteins have been determined by comparison between the 3 strains.
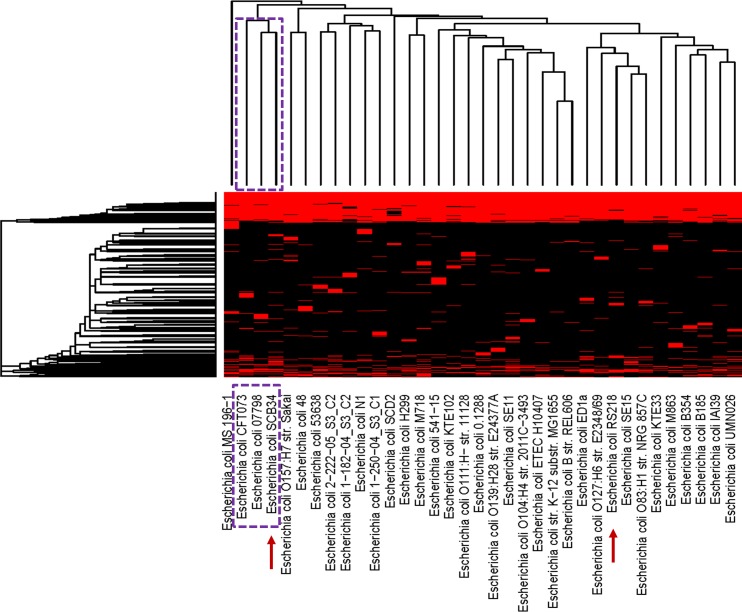
Given the large number of differences observed among these three strains, we next compared the protein coding capacity of SCB34 to that of a representative group of 33 E. coli strains with the goal to focus on the unique biological potential of strain SCB34. The list of all strains and their respective phenotype included in this comparison is included in S4 Table. Informative clusters of orthologous proteins genes (COGs), excluding clusters unique to each genome and core clusters common to all genomes, were used in the analysis to identify patterns between these genomes that might be responsible for the variability in biological activity between strains. These comparisons are summarized in the heat map shown in Fig 6.
Fig 6. Heat map comparing clusters of genes present (red) or absent (black) in each E. coli genome.
SCB34 and RS218 are highlighted by the arrows, among 33 additional representative E. coli strains. The dotted-line boxes highlight the clade that includes SCB34, and the names of the two additional E. coli strains with the most similar protein-coding sequences within the clade. A hierarchical clustering of the genes found in all genomes is found at the left of the heat map, while a tree based on hierarchical clustering of genomes is shown at the top of the heat map.
In this heat map, red and black blocks represent the presence and absence, respectively, of a cluster member in a given genome. Surprisingly, the hierarchical clustering of these strains by protein sequence similarity suggested that SCB34 appears to have a functionally different protein coding capacity than strain RS218. RS218 showed close similarity to E. coli intestinal isolates SE15, a commensal strain isolated from the feces of a healthy adult [26], and to NRG857c, an adherent-invasive O83:H1 E. coli recovered from a patient with Crohn’s disease [27]. Strain SCB34, on the other hand, appears to be most similar to a small clade of strains that includes E. coli CFT073, a prototypic extra-intestinal pathogenic E. coli (ExPEC) isolate recovered from a bacteremic woman with pyelonephritis [28], and to E. coli 07798, an O157:H39 atypical enteropathogenic (aEPEC) strain isolated from a patient with diarrhea [29]. Among the protein coding sequences that are shared by SCB34, CFT073, and 07798, and that show no similarity to RS218, are some proteins encoded by a fim gene cluster, which encode elements of type 1 fimbriae. The FimF protein in this cluster (accession number KDN05313.1) shows 98% similarity to corresponding coding sequences in CFT073 and 07798, and no similar sequence in RS218. In addition, FimD (accession number KDN05314.1) in SCB34 shows 99% similarity with sequences present in both CFT073 and 07798, but these sequences share less than 67% similarity to those encoding this protein in RS218. Another protein coding sequence shared among SCB34, CFT073, and 07798 is sequence KDN05904.1, which is 98% similar to antitoxin HigA present in both CFT073 and 07798. This toxin-antitoxin system is not found in RS218. Furthermore, SCB34 encodes a serine protease autotransporter enterotoxin EspC (accession number KDN06139.1), whose beta-barrel domain is similar to the C-terminus domain of the Pic serine protease precursor also present in CFT073 (WP_001045652.1), and to the C-terminus domain of the SepA autotransporter encoded by 07798 (EKI44969.1) (S1 Fig). This domain is only 67% similar to a sequence annotated as a “disrupted peptidase” present in RS218.
In addition to identifying the above similarities between SCB34 and representative E. coli genomes, the CD-hit analysis also suggested that 282 protein coding genes that were unique to SCB34 (S2 Table). These 282 unique genes include 147 genes that encode hypothetical proteins, and 135 genes with known function. Several of these genes identified as unique based on the thresholds used by CD-hit (80% identity, covering 80% of the sequence), were closely similar to sequences in some of the comparison strains included, e.g., some showed 100% identity to <80% sequence coverage. Therefore, manual curation of the CD-hit generated list was performed using BLASTn as described in Methods section in order to identify the subset of sequences with zero identity to those in strains included in our initial comparison. This additional analysis yielded 58 of such sequences which are presented in S3 Table. Among these 58 SCB34 unique genes with known function we found those encoding a L-lactate permease (KDN05013.1), and a zinc peptidase (KDN08838.1). Another unique sequence in SCB34 encodes an altronate hydrolase, a component of the pathway for the degradation of hexuronates, which are utilized by some intestinal E. coli strains during growth in intestinal mucus [30]. Additional unique protein coding sequences found in SCB34 are those of an O-antigen synthesis cluster that is not present in any strain included in our comparisons. This region encompasses sequences highly similar to those encoding O25b antigens in ST131 strains [31], and includes a dTDP-4-dehydrorhamnose 3, 5-epimerase, several glycosyltransferases, and a Wxz flippase involved in the membrane translocation of O-antigen. We also identified a transcriptional regulator of the Ic1R family (KDN04846.1).
In order to confirm that our analysis reliably identifies unique factors relevant in various E. coli pathotypes, we performed an additional CD-hit comparison that focused on 16 strains among our initial group of 35 for which experimental data exist that confirm the role of some of their individual virulence factors in determining their pathotype. We also included in this additional comparison three of the commensal strains and the laboratory strain selected in our initial analysis (Table 1). This analysis showed that the number of unique genes in each of these 16 strains, when compared to the initial group of 35, is variable. For example, we found 197 and 846 unique genes in each of the AIEC we included, respectively, and a range from 135 to 544 unique genes in UPEC strains. Commensal strains showed a range from 73 to 370 unique genes. The lowest number of unique genes was found in laboratory strain MG1655.
Table 1. Representative pathotypes and number of unique genes in 16 strains selected among all strains included in Fig 6.
| E. coli Strain | Pathotype | Unique genes (n) |
|---|---|---|
| NRG857c | AIEC | 197 |
| 541–15 | AIEC | 846 |
| O104:H4 str. 2011C-3493 | EAEC | 236 |
| Sakai | EHEC | 489 |
| 48 | EHEC | 560 |
| E2348/69 | EPEC | 288 |
| 07798 | aEPEC | 545 |
| ETEC H10407 | ETEC | 252 |
| CFT073 | UPEC | 544 |
| IAI39 | UPEC | 135 |
| UMN026 | UPEC | 212 |
| KTE33 | UPEC | 504 |
| ED1a | Commensal | 370 |
| SE15 | Commensal | 73 |
| SE11 | Commensal | 294 |
| MG1655 | Laboratory strain | 68 |
AIEC, Adherent invasive E. coli; EAEC, enteroaggregative E. coli; EHEC, enterohemorrhagic E. coli; EPEC, enteropathogenic E. coli; aEPEC, atypical enteropathogenic E. coli; ETEC, enterotoxigenic E. coli; UPEC, uropathogenic E. coli.
Although the total number of unique genes in each of these 16 strains did not consistently associate with a particular pathotype, this analysis confirmed that our comparisons can distinguish individual virulence factors that are known to be characteristic of specific pathotypes. Examples of this include the presence of unique genes encoding colicins in strain NRG857c, type II and III secretions system proteins in strain Sakai, agg and aat genes in strain O104:H4 str. 2011C-3493, espC and efa1 in strain E2348/69, tibA in strain ETEC H10407, and unique enterobactin synthesis genes in CFT073. S5 Table contains all the unique protein coding sequences found by CD-hit comparisons in each of these 16 strains compared to the larger group of 35 E. coli strains.
To further understand the phenotypic differences between SCB34 and RS218, we performed an additional analysis to identify unique genes in these two invasive neonatal isolates, compared to the focused group of 16 strains. The CD-hit comparison among these 18 strains demonstrated 471 unique genes in SCB34 and 206 in RS218, thus corroborating the greater complexity of the SCB34 compared to RS218. Moreover, we also confirmed the presence of unique protein coding sequences in RS218 such as those encoding three unique glycotransferases likely involved in the synthesis of O antigen, a fimbrial protein (AJM73146.1), and several membrane proteins including AJM73951.1, AJM73684.1, and AJM73683.1. The unique SCB34 and RS218 genes obtained from the CD-hit comparison are presented in S6 Table.
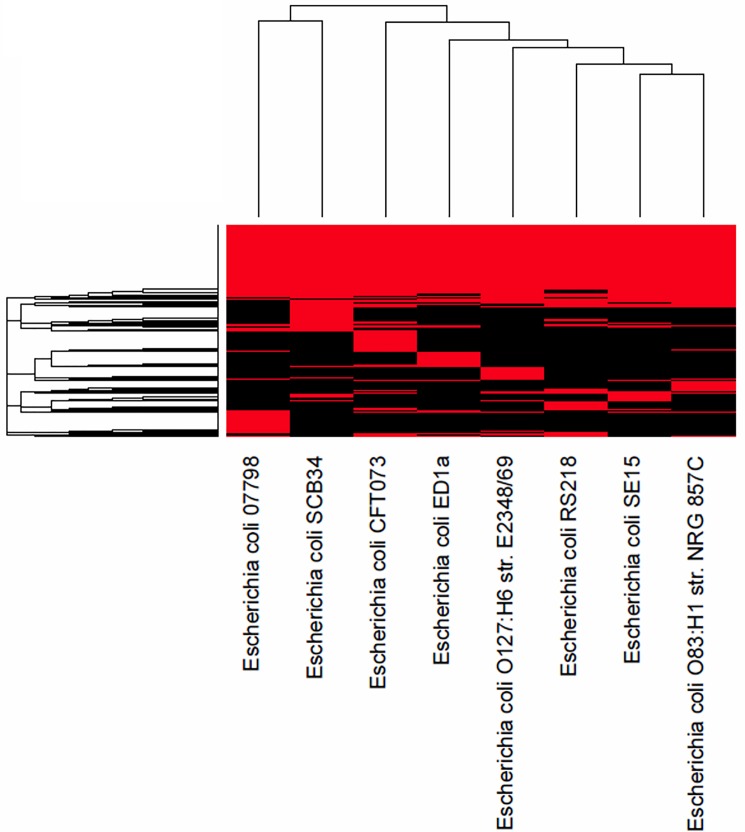
SCB34 and RS218 belong to phylogroup B2, which is overrepresented among E. coli isolates producing extra-intestinal infections. However, despite sharing the same phylogroup, these two neonatal isolates possess unique genotypic characteristics that are likely to determine their individual phenotypes and that distinguish them from each other. This is highlighted in the heatmap shown in Fig 7 which shows a comparison of only the B2 strains among those in Table 1.
Fig 7. Heatmap demonstrating the relationship of E. coli strains belonging to phylogroup B2, including SCB34 and RS218.
Discussion
In this study we have demonstrated that both SCB34 and RS218, two E. coli strains that produced neonatal bacteremia in humans, possess a high invasion ability into intestinal epithelial cells in vitro, and cause septicemia after oral acquisition in newborn animals. E. coli strains belonging to different pathotypes, and other invasive Gram-negative bacteria such as Shigella and Salmonella have shown variable invasion rates of epithelial cells [32, 33]. Our in vitro invasion studies produced comparable results to previous experiments that evaluated the invasion ability of T84 epithelial cells by RS218 and demonstrated a significantly greater invasion by RS218 compared to the nonpathogenic HB101 strain [9].
Other researchers have shown that neonatal invasive E. coli strains produce septicemia in newborn animals after oral inoculation [7, 8, 10, 34–37]. Most prior studies have investigated the virulence of neonatal E. coli isolates after oral inoculation in newborn animals using strains that express the K1 capsule, likely because 70–90% of neonatal meningitis E. coli isolates are known to possess this virulence factor [38–40]. However, only 30–60% of E. coli strains that cause bacteremia without meningitis in young infants carry the K1 capsule [15, 38, 41–43]. Although the K1 capsule plays a significant role in the development of (particularly high-degree) bacteremia, its role is not essential for the development of neonatal sepsis after bacterial oral acquisition as we demonstrated in our experiments performed with SCB34, a non-K1 E. coli neonatal isolate. The K1 capsule and other virulence factors have been identified as relevant in the pathogenesis of neonatal meningitis [13], but the factors that facilitate intestinal invasion and transcytosis of neonatal E. coli isolates have not been fully ascertained. SCB34, a non-K1, contemporary ST131 E. coli clinical isolate produced bacteremia in newborn animals when administered orally but did not after IP injection in our experimental model. In contrast, RS218 produced neonatal bacteremia when administered via either route. This phenomenon could be explained by the presence of virulence factors in SCB34 that determine its lethal phenotype only when acquired orally, and that are dependent on their interaction with the neonatal gut to render this organism fully virulent. Thus, the particular virulence phenotype of SCB34 provides an opportunity to expand our understanding of the mechanisms that determine the development of neonatal bacteremia after oral acquisition of E. coli.
Both SCB34 and RS218, belong to phylogroup B2 which is largely represented among E. coli strains that cause bacteremia in newborns [42, 44]. We speculate that specific virulence factors relevant to the pathogenesis of neonatal bacteremia are present in phylogroup B2 E. coli strains that can cause disease through various mechanisms, and that despite the phenotypic heterogeneity among these isolates, the phylogenetic signal of these strains is not obscured. Phylogroup assignment is thus relevant for the epidemiological characterization of neonatal invasive E. coli strains. However, whole-genome sequencing data provides more precise information of the content and variation of specific virulence factors involved in the pathogenic mechanisms utilized by these strains [45].
Only a few virulence factors have been demonstrated in neonatal invasive E. coli strains to be relevant in the bacterial interaction with intestinal epithelium [46–49]. Oral inoculation with mutants lacking clbA and clbP, which are genes involved in colibactin synthesis and maturation, respectively, resulted in decreased intestinal colonization and virulence in newborn animals [37]. These genes are within the pks 54-kb genomic island present in many ExPEC strains with high virulence characteristics [50]. Interestingly, SCB34 lacks pks-associated genes, including clbA and clbP. This highlights the existence of additional unknown virulence factors that are present in neonatal invasive E. coli strains such as SCB34, that are critical in the process of intestinal translocation that precedes neonatal septicemia. Moreover, and in contrast to RS218, SCB34 does not carry a plasmid [16]. The 114 kb plasmid in RS218 encodes several virulence factors that are relevant to the in vitro invasion properties of this strain, and to its ability to cause septicemia and meningitis in newborn rats [51]. In SCB34, all the necessary virulence factors to cause septicemia after oral infection are on its chromosome.
The cluster analysis revealed that each strain possesses protein compositions that can delineate them from one another, and clustered them with other representative E. coli strains with similar proteomes. The distinct genomic characteristics between RS218 and SCB34 likely determine the phenotypic profile that we observed in our experiments. For example, RS218 carries the neuDBACES genes specific for the K1 capsule, a well-known factor that interferes with complement-mediated killing and phagocytosis [52]. These genes are not present in SCB34, or in any of the strains we included in our comparisons, with the exception of IAI39. This trait would explain at least in part, the ability of RS218 to be pathogenic when injected IP which is contrast to the phenotype that we observed in SCB34.
We found that RS218 was most similar to E. coli isolates SE15 and NRG857c. SCB34, on the other hand, was most similar to E. coli strains 07798 and CFT073. Among the virulence factors shared by SCB34 with CFT073 and 07798, but not with RS218, we found components of type 1 fimbriae, which are known to be relevant in the pathogenesis of urinary tract infections by contributing to bacterial colonization and invasion of uroepithelium, biofilm formation, and establishment of intracellular bacterial communities [53, 54]. The distribution of various fimbrial gene clusters among E. coli is characteristic of particular pathotypes [55]. FimF, for example, is a tip fibrillum component that functions as an adaptor and is involved in the adhesive properties of these structures [56]. FimF is relevant to the epithelial invasion process by E. coli [57] but its role in the pathogenesis of neonatal bacteremia caused by E. coli intestinal invasion and transcytosis in the neonatal gut has not been yet investigated.
Another protein-coding sequence similar among these three strains that is absent in RS218 is the antitoxin HigA, a component of the HigB-HigA type II toxin-antitoxin module ubiquitously present in bacteria [58]. The higBA loci contribute to bacterial adaptation by the generation of persisters, individual cells that have entered a dormant state that renders them tolerant to antibiotics and other environmental stressors [59]. Sequences encoding the beta domain of an EspC protein in SCB34 were also shared with CFT073, and 07798 but not with RS218. EspC is secreted by the T5SS and internalized by the T3SS into intestinal epithelial cells where it causes cytoskeletal damage by cleaving cytoskeleton and focal adhesion proteins [60]. Although the effector domain was not shared among SCB34, CFT073, and 07798, the common beta-barrel structure in these three strains may be a relevant factor by serving as a translocation domain for various effectors possibly relevant to virulence in these strains, as the nonspecificity of the beta domain to a single passenger domain has been suggested [61] Whether these, or other shared virulence factors present in SCB34 could be relevant to the pathogenesis of E. coli strains causing neonatal sepsis remains to be investigated.
Our initial CD-hit analysis also identified 282 unique coding sequences in SCB34, and from this group, manual BLASTn inspection yielded 58 sequences that are absent entirely in all of the representative strains studied. Another unique sequence in SB34 encodes an altronate hydrolase. Altronate hydrolases degrade D-galacturonates, which are present in intestinal mucus and are a nutritional source for pathogenic E. coli strains. Although this degradation pathway does not appear to be directly involved in intestinal colonization [62], it does confer a selective growth advantage in the mammalian intestine [63]. Moreover, genes involved in the metabolism of D-galacturonate were upregulated during growth of pathogenic E. coli in urine, and human blood [64, 65]. The direct role of this metabolic pathway in the pathogenesis of neonatal E. coli sepsis has not been investigated. SCB34 is also unique compared to the strains used in this study in regards to the presence of the O25b antigen, a characteristic common to ST131 strains that have recently disseminated in populations of all ages worldwide, and are known for carrying multiple antibiotics resistance and virulence factor genes [66]. The prevalence of ST131 strains as a cause of invasive disease in newborns and infants continues to increase for reasons that are unclear [15, 67]. It has been proposed that ST131-O25b strains have an enhanced ability to colonize the gut [68]. Colonized hosts by these strains include children in day care who may contribute as a reservoir [69]. Specific O antigens are known to contribute to E. coli virulence by enhancing the bacterial interaction with epithelial barriers. The O6 antigen of CFT073 promotes colonization of the urinary tract by this strain [70]. Moreover, restoration of the O16 antigen in strain MG1655 enabled it to colonize the gut and produce a lethal infection in Caenorhabditis elegans [71]. Whether the O25b antigen present in ST131 strains such as SCB34 specifically enhances the ability of neonatal E. coli strains to colonize, invade and transcytose intestinal epithelium will need to be elucidated. Among the unique proteins in SCB34 we also identified an Ic1R transcriptional regulator. The Ic1R family of regulators controls carbon metabolism and plant virulence in certain enterobacteriaceae, multidrug resistance, solvent tolerance in Pseudomonas, and inactivation of quorum sensing signals in Agrobacterium [72]. It is possible that similar mechanisms controlled by this regulator in SCB34 also play a role in the pathogenesis of intestinal invasion and virulence by this isolate in newborns. Another unique protein we found in SCB34 is YjbH, an outer membrane lipoprotein involved in exopolysaccharide synthesis and predicted to have a β-barrel conformation [73]. Exopolysaccharides in E. coli are relevant to its virulence because they are involved in cell attachment, biofilm formation, and protection against host innate immune responses. The role of this unique protein as a relevant virulence factor to the pathogenesis of SCB34 in newborns will need to be investigated.
Our project has identified unique protein coding sequences in SCB34, a neonatal bacteremia isolate that requires the interaction with the newborn’s gut to produce septicemia. These finding are the basis for additional in vitro and in vivo investigations currently undergoing in our laboratory, aimed at elucidating the role of the unique factors in SCB34 that are relevant to the pathogenesis of neonatal E. coli septicemia.
Conclusions
In summary, we have demonstrated that the E. coli clinical isolate SCB34 has the distinct ability to produce neonatal bacteremia after oral inoculation but not after IP injection, and to invade and transcytose intestinal epithelial cells more efficiently as compared to the archetypal neonatal meningitis isolate RS218. The phenotypic characteristics of SCB34, along with the details of its unique gene repertoire revealed in this study, highlight the existence of several virulence factors that could participate in the development of septicemia after E. coli oral acquisition in newborns. In addition to the known virulence factors unique to SCB34, our study identified 147 hypothetical proteins with a potential role in the pathogenesis of neonatal E. coli bacteremia. The characterization of these factors is underway in our laboratory. Our results provide the foundation for an improved understanding of the pathogenesis of neonatal sepsis, and thus for the development of novel strategies against bacteremia caused by oral route of infection with E. coli in newborns.
Supporting information
(XLSX)
(XLSX)
(DOCX)
(DOCX)
(XLS)
(XLS)
(DOCX)
Comparisons between SCB34 (sequence in the middle), CFT073 (top sequence), and 07798 (bottom sequence) were performed by employing the ACT software tool (Sanger Institute, http://www.sanger.ac.uk). NCBI reference sequence and GenBank numbers are indicated at the left of each sequence.
(TIF)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This research was supported by the Oklahoma INBRE program, award 8P20GM103447 from NIH/NIGMS. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Stoll BJ, Hansen NI, Sanchez PJ, Faix RG, Poindexter BB, Van Meurs KP, et al. Early onset neonatal sepsis: the burden of group B Streptococcal and E. coli disease continues. Pediatrics. 2011;127(5):817–26. Epub 2011/04/27. doi: 10.1542/peds.2010-2217 peds.2010-2217 [pii]. ; PubMed Central PMCID: PMC3081183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Biondi E, Evans R, Mischler M, Bendel-Stenzel M, Horstmann S, Lee V, et al. Epidemiology of bacteremia in febrile infants in the United States. Pediatrics. 2013;132(6):990–6. Epub 2013/11/13. doi: 10.1542/peds.2013-1759 peds.2013-1759 [pii]. . [DOI] [PubMed] [Google Scholar]
- 3.Greenhow TL, Hung YY, Herz AM. Changing epidemiology of bacteremia in infants aged 1 week to 3 months. Pediatrics. 2012;129(3):e590–6. Epub 2012/03/01. doi: 10.1542/peds.2011-1546 peds.2011-1546 [pii]. . [DOI] [PubMed] [Google Scholar]
- 4.Weston EJ, Pondo T, Lewis MM, Martell-Cleary P, Morin C, Jewell B, et al. The burden of invasive early-onset neonatal sepsis in the United States, 2005–2008. Pediatr Infect Dis J. 2011;30(11):937–41. Epub 2011/06/10. doi: 10.1097/INF.0b013e318223bad2 ; PubMed Central PMCID: PMC3193564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stoll BJ, Hansen NI, Adams-Chapman I, Fanaroff AA, Hintz SR, Vohr B, et al. Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA. 2004;292(19):2357–65. Epub 2004/11/18. doi: 292/19/2357 [pii] doi: 10.1001/jama.292.19.2357 . [DOI] [PubMed] [Google Scholar]
- 6.Cotten CM, Smith PB. Duration of empirical antibiotic therapy for infants suspected of early-onset sepsis. Curr Opin Pediatr. 2013;25(2):167–71. Epub 2013/02/15. doi: 10.1097/MOP.0b013e32835e01f6 ; PubMed Central PMCID: PMC3596444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Glode MP, Sutton A, Moxon ER, Robbins JB. Pathogenesis of neonatal Escherichia coli meningitis: induction of bacteremia and meningitis in infant rats fed E. coli K1. Infect Immun. 1977;16(1):75–80. Epub 1977/04/01. ; PubMed Central PMCID: PMC421490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Birchenough GM, Johansson ME, Stabler RA, Dalgakiran F, Hansson GC, Wren BW, et al. Altered innate defenses in the neonatal gastrointestinal tract in response to colonization by neuropathogenic Escherichia coli. Infect Immun. 2013;81(9):3264–75. Epub 2013/06/27. doi: 10.1128/IAI.00268-13 IAI.00268-13 [pii]. ; PubMed Central PMCID: PMC3754193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burns JL, Griffith A, Barry JJ, Jonas M, Chi EY. Transcytosis of gastrointestinal epithelial cells by Escherichia coli K1. Pediatr Res. 2001;49(1):30–7. Epub 2001/01/03. doi: 10.1203/00006450-200101000-00010 . [DOI] [PubMed] [Google Scholar]
- 10.Huang SH, He L, Zhou Y, Wu CH, Jong A. Lactobacillus rhamnosus GG Suppresses Meningitic E. coli K1 Penetration across Human Intestinal Epithelial Cells In Vitro and Protects Neonatal Rats against Experimental Hematogenous Meningitis. International journal of microbiology. 2009;2009:647862 Epub 2009/12/18. doi: 10.1155/2009/647862 ; PubMed Central PMCID: PMC2775688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim KS. Pathogenesis of bacterial meningitis: from bacteraemia to neuronal injury. Nat Rev Neurosci. 2003;4(5):376–85. Epub 2003/05/03. doi: 10.1038/nrn1103 nrn1103 [pii]. . [DOI] [PubMed] [Google Scholar]
- 12.Kim KS. Mechanisms of microbial traversal of the blood-brain barrier. Nat Rev Microbiol. 2008;6(8):625–34. Epub 2008/07/08. doi: 10.1038/nrmicro1952 nrmicro1952 [pii]. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim KS. Current concepts on the pathogenesis of Escherichia coli meningitis: implications for therapy and prevention. Current opinion in infectious diseases. 2012;25(3):273–8. Epub 2012/03/08. doi: 10.1097/QCO.0b013e3283521eb0 . [DOI] [PubMed] [Google Scholar]
- 14.Wang MH, Kim KS. Cytotoxic necrotizing factor 1 contributes to Escherichia coli meningitis. Toxins (Basel). 2013;5(11):2270–80. Epub 2013/11/29. doi: 10.3390/toxins5112270 toxins5112270 [pii]. ; PubMed Central PMCID: PMC3847726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shakir SM, Goldbeck JM, Robison D, Eckerd AM, Chavez-Bueno S. Genotypic and Phenotypic Characterization of Invasive Neonatal Escherichia coli Clinical Isolates. American journal of perinatology. 2014;31(11):975–82. Epub 2014/02/26. doi: 10.1055/s-0034-1370341 . [DOI] [PubMed] [Google Scholar]
- 16.Chavez-Bueno S, Day MW, Toby IT, Akins DR, Dyer DW. Genome Sequence of SCB34, a Sequence Type 131 Multidrug-Resistant Escherichia coli Isolate Causing Neonatal Early-Onset Sepsis. Genome Announc. 2014;2(3):e00514–14. doi: 10.1128/genomeA.00514-14 ; PubMed Central PMCID: PMCPMC4056292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Achtman M, Mercer A, Kusecek B, Pohl A, Heuzenroeder M, Aaronson W, et al. Six widespread bacterial clones among Escherichia coli K1 isolates. Infect Immun. 1983;39(1):315–35. Epub 1983/01/01. ; PubMed Central PMCID: PMC347943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Selvarasu S, Ow DS, Lee SY, Lee MM, Oh SK, Karimi IA, et al. Characterizing Escherichia coli DH5alpha growth and metabolism in a complex medium using genome-scale flux analysis. Biotechnol Bioeng. 2009;102(3):923–34. Epub 2008/10/15. doi: 10.1002/bit.22119 . [DOI] [PubMed] [Google Scholar]
- 19.Odendall C, Dixit E, Stavru F, Bierne H, Franz KM, Durbin AF, et al. Diverse intracellular pathogens activate type III interferon expression from peroxisomes. Nat Immunol. 2014;15(8):717–26. Epub 2014/06/24. doi: 10.1038/ni.2915 ni.2915 [pii]. ; PubMed Central PMCID: PMC4106986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kohler H, Sakaguchi T, Hurley BP, Kase BA, Reinecker HC, McCormick BA. Salmonella enterica serovar Typhimurium regulates intercellular junction proteins and facilitates transepithelial neutrophil and bacterial passage. Am J Physiol Gastrointest Liver Physiol. 2007;293(1):G178–87. Epub 2007/07/07. doi: 293/1/G178 [pii] doi: 10.1152/ajpgi.00535.2006 . [DOI] [PubMed] [Google Scholar]
- 21.Crane JK, Broome JE, Reddinger RM, Werth BB. Zinc protects against Shiga-toxigenic Escherichia coli by acting on host tissues as well as on bacteria. BMC Microbiol. 2014;14:145 Epub 2014/06/07. doi: 10.1186/1471-2180-14-145 1471-2180-14-145 [pii]. ; PubMed Central PMCID: PMC4072484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Neelon BH, O'Malley AJ, Normand SL. A Bayesian model for repeated measures zero-inflated count data with application to outpatient psychiatric service use. Statistical modelling. 2010;10(4):421–39. Epub 2011/02/23. doi: 10.1177/1471082X0901000404 ; PubMed Central PMCID: PMC3039917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lunn DJ, Thomas A, Best N, Spiegelhalter D. WinBUGS—A Bayesian modelling framework: Concepts, structure, and extensibility. Stat Comput. 2000;10(4):325–37. doi: 10.1023/A:1008929526011 PubMed PMID: ISI:000089242200005. [Google Scholar]
- 24.Day MW, Jackson LA, Akins DR, Dyer DW, Chavez-Bueno S. Whole-Genome Sequences of the Archetypal K1 Escherichia coli Neonatal Isolate RS218 and Contemporary Neonatal Bacteremia Clinical Isolates SCB11, SCB12, and SCB15. Genome Announc. 2015;3(1):e01598–14. Epub 2015/02/28. doi: 10.1128/genomeA.01598-14 e01598-14 [pii] 3/1/e01598-14 [pii]. ; PubMed Central PMCID: PMC4342429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang Y, Niu B, Gao Y, Fu L, Li W. CD-HIT Suite: a web server for clustering and comparing biological sequences. Bioinformatics. 2010;26(5):680–2. Epub 2010/01/08. doi: 10.1093/bioinformatics/btq003 btq003 [pii]. ; PubMed Central PMCID: PMC2828112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Toh H, Oshima K, Toyoda A, Ogura Y, Ooka T, Sasamoto H, et al. Complete genome sequence of the wild-type commensal Escherichia coli strain SE15, belonging to phylogenetic group B2. J Bacteriol. 2010;192(4):1165–6. Epub 2009/12/17. doi: 10.1128/JB.01543-09 JB.01543-09 [pii]. ; PubMed Central PMCID: PMC2812965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nash JH, Villegas A, Kropinski AM, Aguilar-Valenzuela R, Konczy P, Mascarenhas M, et al. Genome sequence of adherent-invasive Escherichia coli and comparative genomic analysis with other E. coli pathotypes. BMC Genomics. 2010;11:667 Epub 2010/11/27. doi: 10.1186/1471-2164-11-667 1471-2164-11-667 [pii]. ; PubMed Central PMCID: PMC3091784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Welch RA, Burland V, Plunkett G, 3rd, Redford P, Roesch P, Rasko D, et al. Extensive mosaic structure revealed by the complete genome sequence of uropathogenic Escherichia coli. Proceedings of the National Academy of Sciences of the United States of America. 2002;99(26):17020–4. Epub 2002/12/10. doi: 10.1073/pnas.252529799 252529799 [pii]. ; PubMed Central PMCID: PMC139262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Feng PC, Keys C, Lacher D, Monday SR, Shelton D, Rozand C, et al. Prevalence, characterization and clonal analysis of Escherichia coli O157: non-H7 serotypes that carry eae alleles. FEMS microbiology letters. 2010;308(1):62–7. Epub 2010/05/22. doi: 10.1111/j.1574-6968.2010.01990.x FML1990 [pii]. . [DOI] [PubMed] [Google Scholar]
- 30.Maltby R, Leatham-Jensen MP, Gibson T, Cohen PS, Conway T. Nutritional basis for colonization resistance by human commensal Escherichia coli strains HS and Nissle 1917 against E. coli O157:H7 in the mouse intestine. PLoS One. 2013;8(1):e53957 doi: 10.1371/journal.pone.0053957 ; PubMed Central PMCID: PMCPMC3547972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Szijarto V, Lukasiewicz J, Gozdziewicz TK, Magyarics Z, Nagy E, Nagy G. Diagnostic potential of monoclonal antibodies specific to the unique O-antigen of multidrug-resistant epidemic Escherichia coli clone ST131-O25b:H4. Clin Vaccine Immunol. 2014;21(7):930–9. Epub 2014/05/03. doi: 10.1128/CVI.00685-13 CVI.00685-13 [pii]. ; PubMed Central PMCID: PMC4097449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boudeau J, Glasser AL, Masseret E, Joly B, Darfeuille-Michaud A. Invasive ability of an Escherichia coli strain isolated from the ileal mucosa of a patient with Crohn's disease. Infect Immun. 1999;67(9):4499–509. ; PubMed Central PMCID: PMCPMC96770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jung HC, Eckmann L, Yang SK, Panja A, Fierer J, Morzycka-Wroblewska E, et al. A distinct array of proinflammatory cytokines is expressed in human colon epithelial cells in response to bacterial invasion. J Clin Invest. 1995;95(1):55–65. doi: 10.1172/JCI117676 ; PubMed Central PMCID: PMCPMC295369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pluschke G, Mercer A, Kusecek B, Pohl A, Achtman M. Induction of bacteremia in newborn rats by Escherichia coli K1 is correlated with only certain O (lipopolysaccharide) antigen types. Infect Immun. 1983;39(2):599–608. Epub 1983/02/01. ; PubMed Central PMCID: PMC347994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wullenweber M, Beutin L, Zimmermann S, Jonas C. Influence of some bacterial and host factors on colonization and invasiveness of Escherichia coli K1 in neonatal rats. Infect Immun. 1993;61(5):2138–44. Epub 1993/05/01. ; PubMed Central PMCID: PMC280814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zelmer A, Bowen M, Jokilammi A, Finne J, Luzio JP, Taylor PW. Differential expression of the polysialyl capsule during blood-to-brain transit of neuropathogenic Escherichia coli K1. Microbiology. 2008;154(Pt 8):2522–32. Epub 2008/08/01. doi: 10.1099/mic.0.2008/017988-0 ; PubMed Central PMCID: PMC2572004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McCarthy AJ, Martin P, Cloup E, Stabler RA, Oswald E, Taylor PW. The Genotoxin Colibactin Is a Determinant of Virulence in Escherichia coli K1 Experimental Neonatal Systemic Infection. Infect Immun. 2015;83(9):3704–11. Epub 2015/07/08. doi: 10.1128/IAI.00716-15 ; PubMed Central PMCID: PMC4534652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Korhonen TK, Valtonen MV, Parkkinen J, Vaisanen-Rhen V, Finne J, Orskov F, et al. Serotypes, hemolysin production, and receptor recognition of Escherichia coli strains associated with neonatal sepsis and meningitis. Infect Immun. 1985;48(2):486–91. Epub 1985/05/01. ; PubMed Central PMCID: PMC261353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Johnson JR, Oswald E, O'Bryan TT, Kuskowski MA, Spanjaard L. Phylogenetic distribution of virulence-associated genes among Escherichia coli isolates associated with neonatal bacterial meningitis in the Netherlands. The Journal of infectious diseases. 2002;185(6):774–84. Epub 2002/03/29. doi: 10.1086/339343 . [DOI] [PubMed] [Google Scholar]
- 40.Korczak B, Frey J, Schrenzel J, Pluschke G, Pfister R, Ehricht R, et al. Use of diagnostic microarrays for determination of virulence gene patterns of Escherichia coli K1, a major cause of neonatal meningitis. Journal of clinical microbiology. 2005;43(3):1024–31. Epub 2005/03/08. doi: 10.1128/JCM.43.3.1024–1031.2005 ; PubMed Central PMCID: PMC1081230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Glode MP, Sutton A, Robbins JB, McCracken GH, Gotschlich EC, Kaijser B, et al. Neonatal meningitis due of Escherichia coli K1. The Journal of infectious diseases. 1977;136 Suppl:S93–7. Epub 1977/08/01. . [DOI] [PubMed] [Google Scholar]
- 42.Watt S, Lanotte P, Mereghetti L, Moulin-Schouleur M, Picard B, Quentin R. Escherichia coli strains from pregnant women and neonates: intraspecies genetic distribution and prevalence of virulence factors. Journal of clinical microbiology. 2003;41(5):1929–35. Epub 2003/05/08. doi: 10.1128/JCM.41.5.1929-1935.2003 ; PubMed Central PMCID: PMC154741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Burdet C, Clermont O, Bonacorsi S, Laouenan C, Bingen E, Aujard Y, et al. Escherichia coli bacteremia in children: age and portal of entry are the main predictors of severity. The Pediatric infectious disease journal. 2014;33(8):872–9. Epub 2014/09/16. doi: 10.1097/INF.0000000000000309. . [DOI] [PubMed] [Google Scholar]
- 44.Mahjoub-Messai F, Bidet P, Caro V, Diancourt L, Biran V, Aujard Y, et al. Escherichia coli isolates causing bacteremia via gut translocation and urinary tract infection in young infants exhibit different virulence genotypes. The Journal of infectious diseases. 2011;203(12):1844–9. Epub 2011/05/10. doi: 10.1093/infdis/jir189 jir189 [pii]. . [DOI] [PubMed] [Google Scholar]
- 45.Robins-Browne R, Holt KE, Ingle DJ, Hocking DM, yang J, Tauschek M. Are Escherichia coli Pathotypes Still Relevant in the Era of Whole-Genome Sequencing? Front Cell Infect Microbiol. 2016;6: doi: 10.3389/fcimb.2016.00141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Martindale J, Stroud D, Moxon ER, Tang CM. Genetic analysis of Escherichia coli K1 gastrointestinal colonization. Molecular microbiology. 2000;37(6):1293–305. Epub 2000/09/21. . [DOI] [PubMed] [Google Scholar]
- 47.Fagan RP, Smith SG. The Hek outer membrane protein of Escherichia coli is an auto-aggregating adhesin and invasin. FEMS microbiology letters. 2007;269(2):248–55. Epub 2007/01/24. doi: 10.1111/j.1574-6968.2006.00628.x . [DOI] [PubMed] [Google Scholar]
- 48.Nowrouzian FL, Oswald E. Escherichia coli strains with the capacity for long-term persistence in the bowel microbiota carry the potentially genotoxic pks island. Microbial pathogenesis. 2012;53(3–4):180–2. Epub 2012/06/20. doi: 10.1016/j.micpath.2012.05.011 . [DOI] [PubMed] [Google Scholar]
- 49.Martin P, Marcq I, Magistro G, Penary M, Garcie C, Payros D, et al. Interplay between siderophores and colibactin genotoxin biosynthetic pathways in Escherichia coli. PLoS pathogens. 2013;9(7):e1003437 Epub 2013/07/16. doi: 10.1371/journal.ppat.1003437 ; PubMed Central PMCID: PMC3708854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Johnson JR, Johnston B, Kuskowski MA, Nougayrede JP, Oswald E. Molecular epidemiology and phylogenetic distribution of the Escherichia coli pks genomic island. Journal of clinical microbiology. 2008;46(12):3906–11. Epub 2008/10/24. doi: 10.1128/JCM.00949-08 ; PubMed Central PMCID: PMC2593299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wijetunge DS, Karunathilake KH, Chaudhari A, Katani R, Dudley EG, Kapur V, et al. Complete nucleotide sequence of pRS218, a large virulence plasmid, that augments pathogenic potential of meningitis-associated Escherichia coli strain RS218. BMC Microbiol. 2014;14:203 Epub 2014/08/29. doi: 10.1186/s12866-014-0203-9 s12866-014-0203-9 [pii]. ; PubMed Central PMCID: PMC4155114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Abreu AG, Barbosa AS. How Escherichia coli Circumvent Complement-Mediated Killing. Front Immunol. 2017;8:452 doi: 10.3389/fimmu.2017.00452 ; PubMed Central PMCID: PMCPMC5397495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Melican K, Sandoval RM, Kader A, Josefsson L, Tanner GA, Molitoris BA, et al. Uropathogenic Escherichia coli P and Type 1 fimbriae act in synergy in a living host to facilitate renal colonization leading to nephron obstruction. PLoS pathogens. 2011;7(2):e1001298 doi: 10.1371/journal.ppat.1001298 ; PubMed Central PMCID: PMCPMC3044688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wright KJ, Seed PC, Hultgren SJ. Development of intracellular bacterial communities of uropathogenic Escherichia coli depends on type 1 pili. Cell Microbiol. 2007;9(9):2230–41. doi: 10.1111/j.1462-5822.2007.00952.x . [DOI] [PubMed] [Google Scholar]
- 55.Wurpel DJ, Beatson SA, Totsika M, Petty NK, Schembri MA. Chaperone-usher fimbriae of Escherichia coli. PLoS One. 2013;8(1):e52835 doi: 10.1371/journal.pone.0052835 ; PubMed Central PMCID: PMCPMC3559732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schilling JD, Mulvey MA, Hultgren SJ. Structure and function of Escherichia coli type 1 pili: new insight into the pathogenesis of urinary tract infections. The Journal of infectious diseases. 2001;183 Suppl 1:S36–40. doi: 10.1086/318855 . [DOI] [PubMed] [Google Scholar]
- 57.Boudeau J, Barnich N, Darfeuille-Michaud A. Type 1 pili-mediated adherence of Escherichia coli strain LF82 isolated from Crohn's disease is involved in bacterial invasion of intestinal epithelial cells. Molecular microbiology. 2001;39(5):1272–84. . [DOI] [PubMed] [Google Scholar]
- 58.Yamaguchi Y, Inouye M. Regulation of growth and death in Escherichia coli by toxin-antitoxin systems. Nat Rev Microbiol. 2011;9(11):779–90. doi: 10.1038/nrmicro2651 . [DOI] [PubMed] [Google Scholar]
- 59.Maisonneuve E, Shakespeare LJ, Jorgensen MG, Gerdes K. Bacterial persistence by RNA endonucleases. Proceedings of the National Academy of Sciences of the United States of America. 2011;108(32):13206–11. doi: 10.1073/pnas.1100186108 ; PubMed Central PMCID: PMCPMC3156201. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 60.Navarro-Garcia F, Serapio-Palacios A, Vidal JE, Salazar MI, Tapia-Pastrana G. EspC promotes epithelial cell detachment by enteropathogenic Escherichia coli via sequential cleavages of a cytoskeletal protein and then focal adhesion proteins. Infect Immun. 2014;82(6):2255–65. doi: 10.1128/IAI.01386-13 ; PubMed Central PMCID: PMCPMC4019189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Leyton DL, Sloan J, Hill RE, Doughty S, Hartland EL. Transfer region of pO113 from enterohemorrhagic Escherichia coli: similarity with R64 and identification of a novel plasmid-encoded autotransporter, EpeA. Infect Immun. 2003;71(11):6307–19. doi: 10.1128/IAI.71.11.6307-6319.2003 ; PubMed Central PMCID: PMCPMC219559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fabich AJ, Jones SA, Chowdhury FZ, Cernosek A, Anderson A, Smalley D, et al. Comparison of carbon nutrition for pathogenic and commensal Escherichia coli strains in the mouse intestine. Infect Immun. 2008;76(3):1143–52. doi: 10.1128/IAI.01386-07 ; PubMed Central PMCID: PMCPMC2258830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bai J, McAteer SP, Paxton E, Mahajan A, Gally DL, Tree JJ. Screening of an E. coli O157:H7 Bacterial Artificial Chromosome Library by Comparative Genomic Hybridization to Identify Genomic Regions Contributing to Growth in Bovine Gastrointestinal Mucus and Epithelial Cell Colonization. Front Microbiol. 2011;2:168 doi: 10.3389/fmicb.2011.00168 ; PubMed Central PMCID: PMCPMC3157008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Snyder JA, Haugen BJ, Buckles EL, Lockatell CV, Johnson DE, Donnenberg MS, et al. Transcriptome of uropathogenic Escherichia coli during urinary tract infection. Infect Immun. 2004;72(11):6373–81. doi: 10.1128/IAI.72.11.6373–6381.2004 ; PubMed Central PMCID: PMCPMC523057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pettersen VK, Mosevoll KA, Lindemann PC, Wiker HG. Coordination of Metabolism and Virulence Factors Expression of Extraintestinal Pathogenic Escherichia coli Purified from Blood Cultures of Patients with Sepsis. Mol Cell Proteomics. 2016;15(9):2890–907. doi: 10.1074/mcp.M116.060582 ; PubMed Central PMCID: PMCPMC5013306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Banerjee R, Johnson JR. A new clone sweeps clean: the enigmatic emergence of Escherichia coli sequence type 131. Antimicrob Agents Chemother. 2014;58(9):4997–5004. doi: 10.1128/AAC.02824-14 ; PubMed Central PMCID: PMCPMC4135879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cheng MF, Chen WL, Hung WY, Huang IF, Chiou YH, Chen YS, et al. Emergence of extended spectrum-beta-lactamase-producing Escherichia coli O25b-ST131: a major community-acquired uropathogen in infants. The Pediatric infectious disease journal. 2015;34(5):469–75. Epub 2015/04/17. doi: 10.1097/INF.0000000000000623 00006454-201505000-00002 [pii]. . [DOI] [PubMed] [Google Scholar]
- 68.Nakane K, Kawamura K, Goto K, Arakawa Y. Long-Term Colonization by bla(CTX-M)-Harboring Escherichia coli in Healthy Japanese People Engaged in Food Handling. Applied and environmental microbiology. 2016;82(6):1818–27. doi: 10.1128/AEM.02929-15 ; PubMed Central PMCID: PMCPMC4784029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Blanc V, Leflon-Guibout V, Blanco J, Haenni M, Madec JY, Rafignon G, et al. Prevalence of day-care centre children (France) with faecal CTX-M-producing Escherichia coli comprising O25b:H4 and O16:H5 ST131 strains. J Antimicrob Chemother. 2014;69(5):1231–7. Epub 2014/01/10. doi: 10.1093/jac/dkt519 dkt519 [pii]. . [DOI] [PubMed] [Google Scholar]
- 70.Sarkar S, Ulett GC, Totsika M, Phan MD, Schembri MA. Role of capsule and O antigen in the virulence of uropathogenic Escherichia coli. PLoS One. 2014;9(4):e94786 doi: 10.1371/journal.pone.0094786 ; PubMed Central PMCID: PMCPMC3983267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Browning DF, Wells TJ, Franca FL, Morris FC, Sevastsyanovich YR, Bryant JA, et al. Laboratory adapted Escherichia coli K-12 becomes a pathogen of Caenorhabditis elegans upon restoration of O antigen biosynthesis. Molecular microbiology. 2013;87(5):939–50. doi: 10.1111/mmi.12144 . [DOI] [PubMed] [Google Scholar]
- 72.Molina-Henares AJ, Krell T, Eugenia Guazzaroni M, Segura A, Ramos JL. Members of the IclR family of bacterial transcriptional regulators function as activators and/or repressors. FEMS Microbiol Rev. 2006;30(2):157–86. doi: 10.1111/j.1574-6976.2005.00008.x . [DOI] [PubMed] [Google Scholar]
- 73.Ferrieres L, Aslam SN, Cooper RM, Clarke DJ. The yjbEFGH locus in Escherichia coli K-12 is an operon encoding proteins involved in exopolysaccharide production. Microbiology. 2007;153(Pt 4):1070–80. doi: 10.1099/mic.0.2006/002907-0 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
(XLSX)
(DOCX)
(DOCX)
(XLS)
(XLS)
(DOCX)
Comparisons between SCB34 (sequence in the middle), CFT073 (top sequence), and 07798 (bottom sequence) were performed by employing the ACT software tool (Sanger Institute, http://www.sanger.ac.uk). NCBI reference sequence and GenBank numbers are indicated at the left of each sequence.
(TIF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.