Abstract
Purpose:
To establish a new scoring system for limbal dermoid, in order to unify the diagnostic criteria and assess the prognosis.
Methods:
A retrospective study was conducted on 261 patients with limbal dermoid. The basic information, clinical features, and pathology of dermoids were recorded, and the prognosis at 1 year after keratoplasty was assessed at follow-up. A new visual scoring system was created for the area of corneal involvement, the area of conjunctival involvement, and the surface shape.
Results:
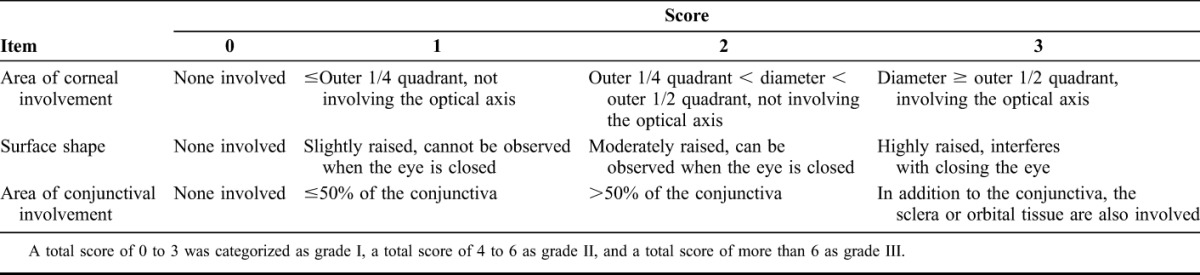
There were 154 females and 107 males with mean age of 4 ± 3 years at surgery. After scoring, 59% (136) of patients were classified as grade I, 26% (60) as grade II, and 14% (33) as grade III. The pathological results were 124 dermoid cases, 76 lipodermoid, 5 complex choristoma, and 10 epibulbar osseous choristoma. Moreover, patients with lower clinical scores presented a better prognosis; the mean logarithm of the minimum angle of resolution (logMAR) best-corrected visual acuity in grade I patients was 0.38 ± 0.05, which was better than the grade II value of 0.61 ± 0.09 (P < 0.05) and the grade III value of 0.94 ± 0.11 (P < 0.001).
Conclusions:
New grading systems for limbal dermoid were useful for clinical diagnosis and may have prognostic value in predicting visual acuity. A lower-grade dermoid exhibited better vision postoperatively.
Key Words: limbal dermoid, new grading system, retrospective study
Limbal dermoids are congenital benign tumors that influence vision and cause visual abnormalities due to the development of astigmatism, encroachment on the visual axis, and fatty component infiltration into the cornea.1,2 They consist of overgrowths of epidermal appendages, connective tissues, skin, fat, sweat glands, lacrimal glands, and neurologic tissues located partly over the cornea and partly over the sclera.1,3–5
Clinically, limbal dermoids present in a dome shape with a keratinized surface, sometimes with hair follicles and cilia. Associated ocular abnormalities include colobomata of the eyelids, lacrimal anomalies, and scleral and corneal staphylomata. In 1972, Benjamin and Allen1 proposed an embryological classification of dermoids into derivatives of the branchial region of the embryo and derivatives of embryonal tissue that give rise to the various parts of the fully formed eye. However, this proposal is speculative and has not been consistently recognized. In 2005, Tasse et al6 defined 3 groups of oculo-auriculo-vertebral spectrum disorders based on the presence of the main clinical findings. Until now, no clinical grading scales have been built, and many aspects of limbal dermoid research have been poorly organized.
In this study, we investigated 261 children with limbal dermoids, analyzed the clinical features, validated a novel visual scoring system, and tested its rationality combined with postoperative pathology and prognosis.
MATERIALS AND METHODS
Study Design and Target Population
A descriptive and retrospective review was conducted on 261 children younger than 12 years old who were diagnosed with limbal dermoids and underwent surgery between 2005 and 2015 at Zhongshan Ophthalmic Center. The registered indices included basic information, such as sex; age at surgery; province; any abnormal condition during pregnancy, such as maternal age, abnormal duration of pregnancy, and abnormal factors; clinical features, for instance, the location and area of the dermoid and macrostomia; surgery performed; and the histopathology results by hematoxylin–eosin (HE) staining. The prognosis at 1 year after keratoplasty was assessed at follow-up. The study was approved by the Investigational Review Board of Zhongshan Ophthalmic Center (approval ID: 2013MEKY004), Sun Yat-sen University, Guangzhou, China. All of the children's parents provided written informed consent. This study adhered to the tenets of the Declaration of Helsinki.
Visual Scoring System
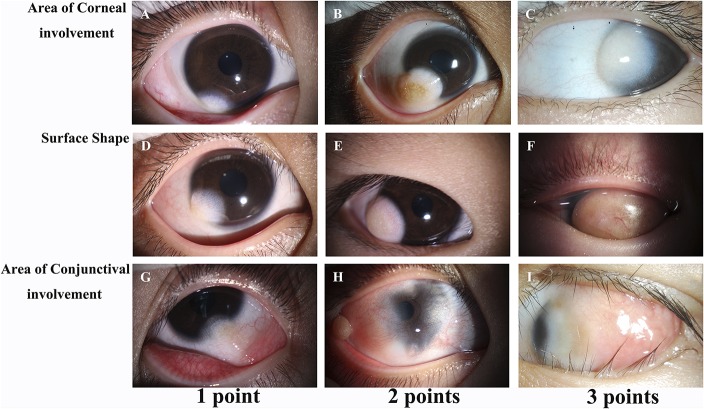
The severity of limbal dermoids was scored visually with a slit lamp. A score of 0 to 3 items was allocated to each of the following 3 criteria: area of corneal involvement, surface shape, and area of conjunctival involvement (Table 1). The scores for the area of corneal involvement were as follows: 0 = none involved; 1 = ≤outer 1/4 quadrant, not involving the optical axis; 2 = outer 1/4 quadrant < diameter < outer 1/2 quadrant, not involving the optical axis; and 3 = diameter ≥ outer 1/2 quadrant, involving the optical axis. The scores for the surface shape are as follows: 0 = none involved; 1 = slightly raised, cannot be observed when the eye is closed; 2 = moderately raised, can be observed when the eye is closed; 3 = highly raised, interferes with closing the eye. The scores for the area of conjunctival involvement are as follows: 0 = none involved; 1 = ≤50% of the conjunctiva; 2 = >50% of the conjunctiva; 3 = in addition to the conjunctiva, the sclera or orbital tissue is also involved. Each patient was given a score from the 3 items above to yield a possible total score ranging from 0 to 9. A total score of 3 or less was classified as grade I, a total score of 4 to 6 as grade II, and a total score of 6 to 9 as grade III.
TABLE 1.
Visual Scoring System for Limbal Dermoid
Statistical Analysis
An unpaired t test was performed to determine the differences in the clinical score of monocular and binocular eyes. Differences in the postoperative best-corrected visual acuity (BCVA) of the different grades and clinical scores of different pathologies were determined using the Mann–Whitney U test. The data were considered statistically significant at P < 0.05.
RESULTS
Clinical Data of Patients
The patient population included 154 males (59%) and 107 females (41%), and their mean age at surgery was 4 ± 3 years; most children received surgery at 1 to 3 years of age. The majority of patients lived in Guangdong Province (177 patients, 68%), which had an average population of 100 million during the study period (available at: www.stats.gov.cn), indicating an approximate annualized incidence of limbal dermoids of 0.177 per million people (assuming that all patients in Guangdong Province were treated at Zhongshan Ophthalmic Center), followed by the neighboring Jiangxi Province (8%) and Hunan Province (8%).
Limbal dermoid affected the left eye in 136 patients (52%), the right eye in 111 patients (43%), and both eyes in 14 patients (5%). The most common location was the bitemporal side in 88% (205) of patients, followed by the nasal side in 4% (10), the inferior side in 3% (8), the center in 1% (2), and the superior side in 1% (1) of patients. The mean area of the limbal dermoid was 25.75 ± 25.36 (0.5–180) mm2; 61% of limbal dermoids were 10 to 50 mm2 in size, 29% were less than 10 mm2 in size, and 10% were 50 to 100 mm2 in size.
Pathogenesis
Mean maternal age of 93 mothers was 26 ± 4 (19–39) years; 38 mothers (41%) gave birth to their children at 26 to 30 years old, 35 mothers (38%) at 20 to 25 years old, 13 mothers (14%) at 30 to 39 years old, and 7 mothers (8%) at less than 20 years old. Of 130 mothers, 79 (61%) reported an abnormal condition during pregnancy, and the remaining 51 pregnancies were normal (39%). Fifty-five mothers (70%) had a history of a possible viral infection, such as rubella, herpetic stomatitis, influenza, or diarrhea; 14 mothers (18%) reported premature birth, fetal hypoxia, or umbilical cord entanglement of the neck of the fetus; and 10 mothers (13%) were influenced by environmental pollution, such as high concentrations of indoor formaldehyde, X-ray contamination, or radiation pollution. Moreover, the majority of mothers (80%, 63 patients) experienced the anomalous conditions described above during the first 3 months of pregnancy, and 10% (8 patients) experienced abnormalities during the middle and later trimesters of pregnancy. The results suggest that most abnormal conditions were possibly induced by viral infection during the first 3 months of the pregnancy. Of 261 mothers, 1 (0.4%) had a female family history of limbal dermoids, and the remaining 260 had no history of the disease, which suggested that limbal dermoids are not caused by a genetic disease.
New Grading System and Clinical Feature
Representative images of the different limbal dermoid scores are shown in Figure 1. After evaluation of the limbal dermoids by the scoring system described in the methods, 136 (59%) children were classified as grade I, 60 (26%) were grade II, and 33 (14%) were grade III (Fig. 2A). Patients with monocular dermoid had a mean score of 3.40 ± 0.16, which was lower than that of the patients with bilateral dermoid, whose mean score for binocular dermoid was 5.58 ± 0.91 (P < 0.01) (Fig. 2B). Moreover, 23 children (9%) had unilateral or bilateral malformed ears with an accessory tragus (Fig. 3A), and another 5 children (2%) had facial asymmetry with hypoplasia (Fig. 3B) and eyelid defects (Figs. 3C, D), respectively.
FIGURE 1.
Visual scoring system of limbal dermoids. Representative images of 3 patients, including the area of the conjunctiva (A–C), surface shape (D–F), and area of conjunctival involvement (G–I) for 3 scores (1, 2, and 3 points) (original magnification ×16).
FIGURE 2.
Different grades of eyes with limbal dermoid. Quantification (A) of dermoid cases in grade I, II, and III patients (A). The clinical scores of patients with monocular dermoid were lower than the mean scores of patients with binocular dermoid (B).
FIGURE 3.

Representative images of ear, mandible, and eyelid abnormities. A, Ear anomaly or a malformed ear with an accessory tragus. B, Transverse facial cleft. C and D, Eyelid defect.
Pathology
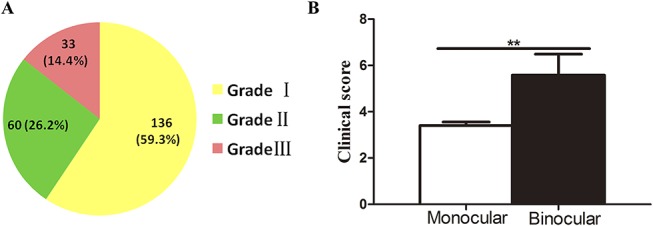
Of the 215 patients who had a clear histopathological diagnosis, there were 4 types of dermoid: dermoid (Fig. 4A), lipodermoid (Fig. 4B), complex choristoma (Fig. 4C), and epibulbar osseous choristoma (Fig. 4D). Dermoid including collagen fiber tissue in the epidermis and dermis (sometimes with hairs) accounted for 124 (58%) cases, which included 72 grade I, 36 grade II, and 16 grade III cases. Lipodermoid consisting of collagen fiber tissue and adipose tissues such as fatty tissue accounted for 76 cases (35%), which included 47 grade I, 17 grade II, and 12 grade III cases. Complex choristoma made up of collagen fiber tissue, smooth muscle, and glandular tissue, for example, lacrimal tissue, sweat glands, and sebaceous glands, accounted for 5 cases (2%), including 2 grade II and 3 grade III cases. Epibulbar osseous choristoma containing collagen fiber tissue, glandular tissue, bone tissue, and nervous tissue accounted for 10 cases (5%), including 1 grade II and 9 grade III cases (Fig. 4E). Dermoid and lipodermoid accounted for most of the grade I cases, and epibulbar osseous choristoma had more grade III cases.
FIGURE 4.
Histopathology pathological sections subjected to hematoxylin–eosin staining showed different types of limbal dermoids. A, Image of dermoid tissue (the yellow arrow indicates collagen fiber tissue). B, Lipodermoid (the green arrow shows collagen fiber and adipose tissue). C, Complex choristoma (the red arrow presents collagen fiber and smooth muscle). D, Epibulbar osseous choristoma (the black arrow reveals collagen fiber and bone tissue); original magnification ×40. E, Different grades in the various types of pathology. F, Comparison of different clinical scores in the various types of pathology. *P < 0.05, **P < 0.01, and ***P < 0.001.
Furthermore, patients diagnosed with dermoid and lipodermoid, which were considered relatively similar mild pathological types, had no significant difference in clinical scores (both P > 0.05). Compared with dermoid and lipodermoid, complex choristoma (both P < 0.05) and epibulbar osseous choristoma (both P < 0.001) displayed higher clinical scores, and epibulbar osseous choristoma had a higher clinical score than that of complex choristoma (P < 0.05), both of which were relatively serious pathological types; epibulbar osseous choristoma was deemed to be more severe (Fig. 4F).
Management and Prognosis
Two hundred twenty children underwent surgery in our study; 199 (90%) patients underwent resection combined with lamellar keratoplasty (LKP), 10 (5%) patients underwent resection with conjunctival autografts, 4 patients (2%) underwent resection with penetrating keratoplasty, and 3 patients (1%) underwent resection combined with amniotic membrane transplantation.
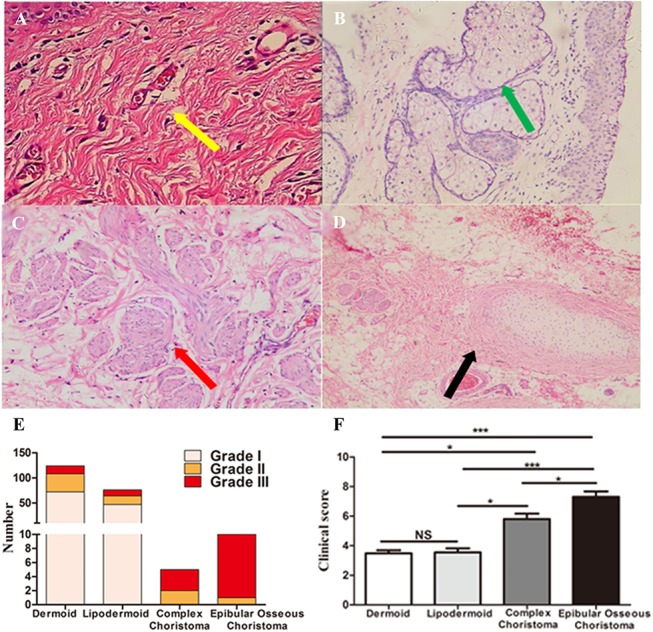
We followed patients of different grades for 1 year after keratoplasty (Fig. 5), and the mean logMAR BCVA in the grade I patients was 0.38 ± 0.05, which was better than that of the grade II patients, who had a BCVA of 0.61 ± 0.09 (P < 0.05), and that of the grade III patients, who had a BCVA of 0.94 ± 0.11 (P < 0.001) and the worst visual prognosis. Conclusively, the patients with severe dermoid with higher grades tended to have a poorer BCVA postoperatively.
FIGURE 5.
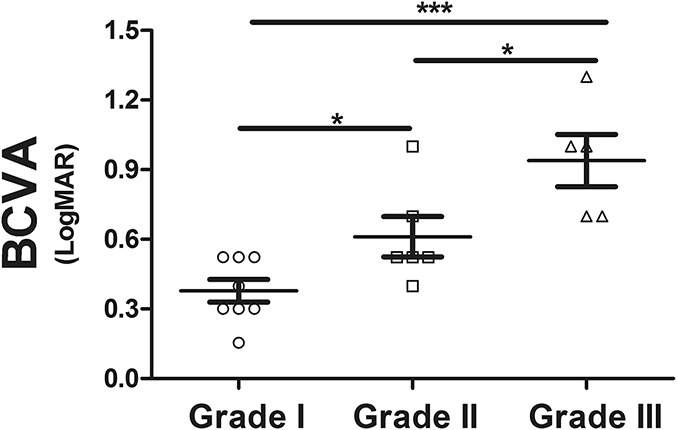
Postoperative prognosis. The prognosis of patients with different grades at 1 year after keratoplasty *P < 0.05; **P < 0.01; ***P <0.001.
DISCUSSION
Limbal dermoids are benign congenital tumors comprising normal tissue in an abnormal location that seriously threatens visual acuity.7 The prevalence of limbal dermoids was approximately 0.177 per million people in our study, compared with 1 to 3 cases per 10,000 in a study by Elsas and Green2 in 1975. Numerous theories have been proposed to account for the development of limbal dermoids. Bloch and Sulzberger in 1926 and 19281 first noted that a viral infection of the mother during pregnancy had teratogenic effects on the branchial arch derivatives. In our study, 69.9% of the 79 interviewed mothers who admitted experiencing an abnormal condition during pregnancy had a history of rubella, herpetic stomatitis, influenza, or diarrhea, which could be considered a possible viral infection. Therefore, it is reasonable to assume that viral infection may be a possible predisposing factor.
Clinically, limbal dermoids are easy to detect and diagnose; however, a grading system to capture all sizes and shapes of limbal dermoids may help with the description of the clinical features of limbal dermoids. Although an embryological classification of dermoids and clinical classification of oculo-auriculo-vertebral spectrum disorders have been proposed,1,6 no clinical grading scales have been targeted at clinical features of limbal dermoids and applied in clinical use to guide therapy and forecast the prognosis. In this study, we created a new limbal visual scoring system, which divided limbal dermoids into 3 different grades by 3 indices including the area of corneal involvement, the surface shape, and the area of conjunctival involvement, using points from 0 to 3. There were 2 main clinical features after reviewing patients with limbal dermoid in our study: first, the majority of patients (59%) belonged to the grade I group (with a score of 0–3 points), followed by grade II (with a score of 4–6 points), and grade III (with a score of 6–9 points); second, patients with monocular dermoid had lower clinical scores, and patients with binocular dermoid had higher mean clinical scores.
Notably, the grading system described in this study was closely associated with the postoperative pathology. Limbal dermoids mainly contained 4 pathological types: dermoid, lipodermoid, complex choristoma, and epibulbar osseous choristoma.8 The majority of the tumors were dermoid,9 consisting of a solid choristoma mass with a surface epithelium resembling the epidermis and dermis and containing some hairs with overlying thick bundles of collagen,10 which made up the bulk of the mass. Lipodermoid was often located superficially and had an abundance of adipose tissue such as fatty tissue but minimal skin adnexa. Complex choristoma included lacrimal tissue, smooth muscle, and neural tissue.11 Epibulbar osseous choristoma was a small, solid, circumscribed red-white bony lesion behind the limbus and between the superior and lateral rectus muscles.12 In our study, complex choristoma and epibulbar osseous choristoma, which were pathologically complex, presented large ratios of grade II or grade III patients, and high clinical scores, whereas dermoid and lipodermoid with mild pathology showed large proportions of grade I patients and low clinical scores. This result demonstrated that dermoid tumors with high clinical scores had a complex pathology and that dermoid tumors with low clinical scores revealed a simple pathology, which demonstrates the close relationship between the clinical score and pathology, as well as the rationality of our scoring system.
Surgery is deemed an effective and necessary treatment.13,14 We proposed a management guideline including surgical methods and time points based on the scoring system.15,16 For grade I, in which optical axis encroachment and visual development interference are absent and the possibility of amblyopia is relatively low, we recommend LKP for patients older than 3 years because the ability to coordinate treatment in infants is poor. For grade II, LKP or deep LKP are suggested, depending on the depth of the dermoid, and should be performed as early as possible, because a larger dermoid increases the degree of astigmatism and compromises visual development beginning at birth. For grade III patients, it is necessary to perform deep LKP or penetrating keratoplasty as soon as possible because severe astigmatism and the obvious optical axis encroachment negatively affect vision and eye development. We followed patients with different grades who accepted keratoplasty and found that grade I patients had the best logMAR BCVA of 0.38 ± 0.05, followed by grade II patients with 0.61 ± 0.09; grade III patients had the worst visual prognosis of 0.94 ± 0.11. The postoperative visual acuity showed little differences compared with the study by Watts et al,20 in which 97% of eyes (29/30) had a visual acuity greater than or equal to 6/24. The preoperative clinical grade and postoperative prognosis showed that low-grade patients had a better visual prognosis, which demonstrates that the grading scale is a reasonable quantitative method that can classify different grades in patients with limbal dermoid and make the therapy more robust.
In summary, a simple, subjective, and useful clinical scoring system for limbal dermoid was established, which showed good predictive value regarding the pathology and prognosis and demonstrated that a lower-grade dermoid has a milder pathological type and better vision postoperatively. Our grading system may be useful for ophthalmologists in assessing the grade of limbal dermoid and in predicting surgical intervention.
Footnotes
Supported by Guangdong Province Science and Technology Projects (303090100502039) and Natural Science Foundation of China (81670826).
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Benjamin SN, Allen HF. Classification for limbal dermoid choristomas and branchial arch anomalies. Presentation of an unusual case. Arch Ophthalmol. 1972;87:305–314. [DOI] [PubMed] [Google Scholar]
- 2.Elsas FJ, Green WR. Epibulbar tumors in childhood. Am J Ophthalmol. 1975;79:1001–1007. [DOI] [PubMed] [Google Scholar]
- 3.Braune S, Kohnen T. Establishment of a quality management system in a department of ophthalmology [in German]. Klin Monbl Augenheilkd. 2009;226:616–623. [DOI] [PubMed] [Google Scholar]
- 4.Daroff RB. Random comments: neurologists and neuro-ophthalmology; the “ocular motor” system; and update on ophthalmoplegic migraine. Semin Neurol. 2000;20:145–149. [DOI] [PubMed] [Google Scholar]
- 5.Dick B, Basad E. Establishing a clinical information system for surgical ophthalmology and orthopedics specialties with reference to GSG '93 [in German]. Klin Monbl Augenheilkd. 1996;208:254–261. [DOI] [PubMed] [Google Scholar]
- 6.Tasse C, Böhringer S, Fischer S, et al. Oculo-auriculo-vertebral spectrum (OAVS): clinical evaluation and severity scoring of 53 patients and proposal for a new classification. Eur J Med Genet. 2005;48:397–411. [DOI] [PubMed] [Google Scholar]
- 7.Vaidya SP, Vaidya PC. Ocular dermoid. Indian Pediatr. 2014;51:333. [PubMed] [Google Scholar]
- 8.Wei QC, Li XH, Hao YR. The pathological analysis of 213 children with ocular tumor [in Chinese]. Zhonghua Yan Ke Za Zhi. 2013;49:37–40. [PubMed] [Google Scholar]
- 9.Watson S, Sarris M, Kuishek M, et al. Limbal dermoid epithelium shares phenotypic characteristics common to both hair epidermal and limbal epithelial stem cells. Curr Eye Res. 2013;38:835–842. [DOI] [PubMed] [Google Scholar]
- 10.del Rocio Arce Gonzalez M, Navas A, Haber A, et al. Ocular dermoids: 116 consecutive cases. Eye Contact Lens. 2013;39:188–191. [DOI] [PubMed] [Google Scholar]
- 11.Jakobiec FA, Nguyen J, Mandell K, et al. Complex palpebral odontogenic choristoma: a reappraisal of the origin of teeth-bearing periocular lesions. Am J Ophthalmol. 2009;147:531–543. [DOI] [PubMed] [Google Scholar]
- 12.Gayre GS, Proia AD, Dutton JJ. Epibulbar osseous choristoma: case report and review of the literature. Ophthalmic Surg Lasers. 2002;33:410–415. [PubMed] [Google Scholar]
- 13.Pirouzian A, Ly H, Holz H, et al. Fibrin-glue assisted multilayered amniotic membrane transplantation in surgical management of pediatric corneal limbal dermoid: a novel approach. Graefes Arch Clin Exp Ophthalmol. 2011;249:261–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pirouzian A, Holz H, Merrill K, et al. Surgical management of pediatric limbal dermoids with sutureless amniotic membrane transplantation and augmentation. J Pediatr Ophthalmol Strabismus. 2012;49:114–119. [DOI] [PubMed] [Google Scholar]
- 15.Watts P, Michaeli-Cohen A, Abdolell M, et al. Outcome of lamellar keratoplasty for limbal dermoids in children. J AAPOS. 2002;6:209–215. [DOI] [PubMed] [Google Scholar]
- 16.Scott JA, Tan DT. Therapeutic lamellar keratoplasty for limbal dermoids. Ophthalmology. 2001;108:1858–1867. [DOI] [PubMed] [Google Scholar]