Key Points
AICC has been used since 1977 to control bleeding in patients with hemophilia with inhibitors.
AICC is associated with a low incidence of TEEs, especially when administered prophylactically.
Abstract
Anti-inhibitor coagulant complex (AICC), an activated prothrombin complex concentrate, has been available for the treatment of patients with inhibitors since 1977, and thromboembolic events (TEEs) have been reported after infusion of AICC in patients with congenital or acquired hemophilia. With the aim of estimating the TEE incidence rate (IR) related to AICC exposure in these patients, a systematic review of the literature was carried out in Medline, according to PRISMA guidelines, from inception date to March 2017. The IR of TEEs was estimated through a meta-analytic approach by using a generalized linear mixed model based on a Poisson distribution. Thirty-nine studies were included (1980-2016). Overall, 46 TEEs were reported; of these, 13 were reported as disseminated intravascular coagulations, 11 as myocardial infarctions, and 3 as thrombotic cerebrovascular accidents. The pooled TEE IR was 2.87 (95% confidence interval [CI], 0.32-25.40) per 100 000 AICC infusions (5.42 in retrospective studies [95% CI, 0.92-31.82]; 1.09 in prospective studies [95% CI, 0.01-238.77]). The TEE rate was 5.09 (95% CI, 0.01-1795.60) per 100 000 AICC infusions administered on demand, whereas no TEEs were reported with prophylaxis. Interestingly, the estimated IR in patients with congenital hemophilia was <0.01 per 100 000 infusions. These findings provide robust evidence of safety of AICC over almost 40 years of published studies.
Visual Abstract
Introduction
The development of factor VIII (FVIII) inhibitory antibodies is a major challenge in the treatment of hemophilia, because it hinders FVIII replacement for the treatment and prevention of bleeding events.1 Two products are currently available to control bleeding in patients with inhibitors: anti-inhibitor coagulant complex (AICC), an activated prothrombin complex concentrate (FEIBA [FVIII inhibitor bypassing activity] NF; Shire, Lexington, KY) and recombinant activated factor VII (NovoSeven; Novo Nordisk, Bagsvaerd, Denmark). Both agents have shown similar efficacy, with some patients responding better to 1 product than to the other.2 Both agents have been associated with the development of thromboembolic events (TEEs).3
AICC has been used for >40 years to control bleeding in patients with hemophilia with high-titer inhibitors. It is a plasma-derived concentrate that contains various prothrombin complex coagulation factors, in their zymogenic and enzymatic forms, and natural anticoagulant factors in a hemostatic balance.4
The aim of this study was to estimate the TEE incidence rate (IR) in patients with congenital hemophilia with inhibitors or acquired hemophilia exposed to AICC, using a meta-analytic approach based on published scientific literature.
Methods
We performed a literature search in MedLine using PubMed from its inception date to 23 March 2017 using the following terms: “hemophilia A,” “hemophilia B,” “blood coagulation factors,” “FEIBA,” and “CS849DUN3M” (ie, FEIBA US Food and Drug Administration registration number). The full research string was: (((“hemophilia A” [MeSH Terms] OR “hemophilia B” [MeSH terms] OR (“haemophilia A” [tiab] OR “hemophilia A” [tiab] OR “haemophilia B” [tiab] OR “hemophilia B” [tiab])) AND “blood coagulation factors” [MeSH terms] AND (“FEIBA” [tiab] OR “FEIBA” [supplementary concept] OR “CS849DUN3M” [RN])) NOT (“case reports” [publication type] OR “letter” [publication type])) NOT (animal [MeSH terms] NOT human [MeSH terms]). For the sake of completeness, we further reviewed the references of all relevant retrieved articles to identify additional published studies. Prospective and retrospective, interventional and noninterventional studies on patients with hemophilia A or B with inhibitors or with acquired hemophilia treated with AICC reporting safety data were included in the meta-analysis.
Two of the authors (M.R. and P.A.C.) independently evaluated eligibility of all the studies retrieved from the electronic literature search. Two other reviewers (A.G. and R.C.) were also involved to reach consensus in case of disagreement.
For each included study, we extracted the following data: first author last name, publication year, geographic area of the study, study design (prospective or retrospective, interventional or noninterventional), hemophilia type (A or B, congenital or acquired), treatment modality (on demand, prophylaxis, or surgery), number of patients treated with AICC and their mean age if reported, number of patients reporting TEEs together with the total number and type of TEEs, and estimated number of AICC infusions.
Exposure to AICC was mandatory to compute the IR of TEEs. If the number of AICC infusions was not detailed in the publication, the number of infusions was estimated according to the treatment modality (on demand, prophylaxis, or surgery) and calculated based on the mean duration of treatment and/or the mean overall dose per kilogram of body weight reported. When not otherwise specified, 2 AICC infusions were assumed for each on-demand bleeding treatment.2,5
Given that TEEs are rare, standard statistical meta-analytic methods cannot be applied. In fact, standard errors from studies reporting 0 TEEs cannot be estimated unless a continuity correction factor is used. To overcome this limitation, we estimated study-specific TEE IRs and their associated 95% exact Poisson confidence intervals (CIs), as well as the pooled TEE IR, through a random-intercept generalized linear mixed model based on a Poisson distribution.6
Stratified analyses according to study design (prospective vs retrospective), publication year (1980-2004, 2005-2010, or 2011-2016), hemophilia type (congenital vs acquired), and treatment modality (on demand, prophylaxis, or surgery) were conducted. A metaregression model was fitted to test for the effect of publication year on the pooled TEE IR.
We performed all analyses with R software (version 3.4.0; R Foundation for Statistical Computing, Vienna, Austria) through the metarate function of the meta package.7
Results
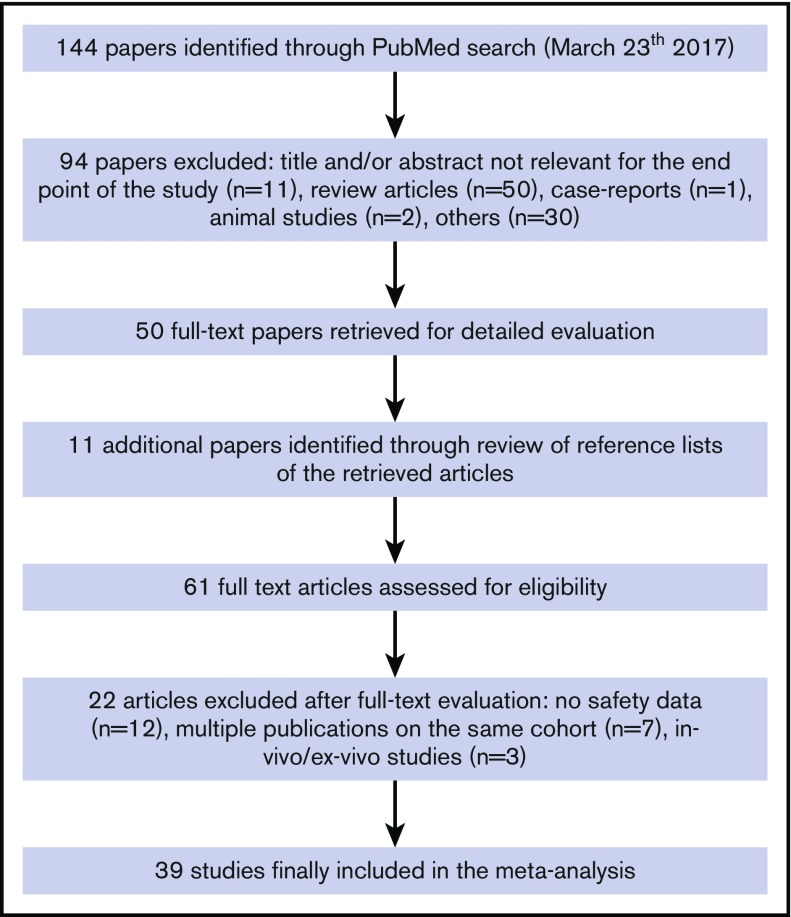
We identified a total of 144 articles through the electronic literature search. After the exclusion of 94 nonrelevant references, 50 articles were fully evaluated for inclusion in the meta-analysis, with other 11 additional articles identified through review of reference lists of retrieved articles. Of the 61 fully evaluated publications, 39 studies with safety data related to the use of AICC in patients with congenital hemophilia with inhibitors or acquired hemophilia were included in the meta-analysis2,3,5,8-43 (Figure 1).
Figure 1.
Flow diagram of study selection process.
The studies included2,3,5,8-43 were published from 1980 to 2016 and provided information on safety related to 678 447 AICC infusions (7291 as on-demand treatment,2,5,8-11,15-18,23,28,29,32,33,36,37,39,42,43 77 203 as prophylaxis,13,18,21,26,31,33,39,41,43 3296 in surgery,14,17-20,22,24,27,30,34,38 and 590 657 with unmentioned treatment modalities3,12,25,35,40) in >750 patients with inhibitors. Of 39 included studies,2,3,5,8-43 5 were controlled randomized clinical trials,2,5,9,33,39 10 were uncontrolled prospective studies,8,10,11,25,28,31,38,40,42,43 and the remaining 24 were retrospective studies.3,12-24,26,27,29,30,32,34-37,41 A majority of the studies (69%) included only patients with congenital hemophilia,2,5,8-11,13,16,18,20-33,36,37,39,41 and 10% only patients with acquired hemophilia.15,17,40,42 In the remaining 21% of studies involving both patients with acquired and those with congenital hemophilia,3,12,14,19,34,35,38,43 it was not possible to differentiate the number of infusions administered for 1 or the other condition, except in 1 study.
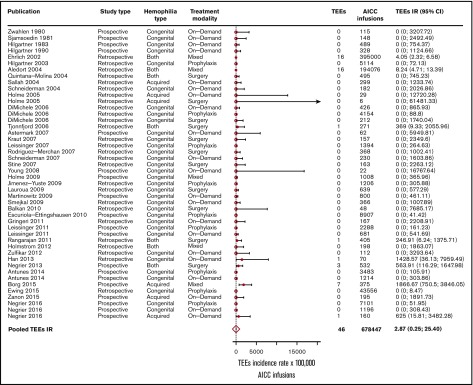
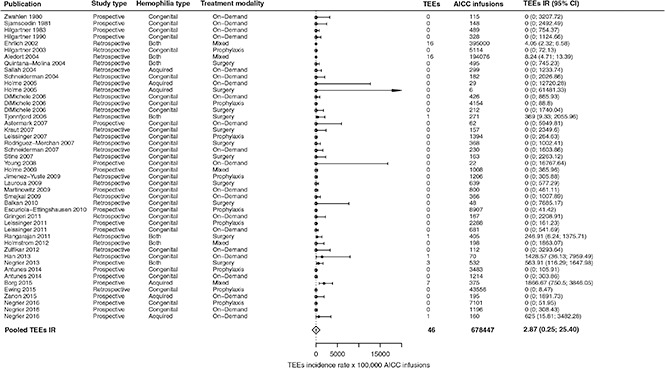
In the overall included 39 studies,2,3,5,8-43 46 TEEs were reported: 13 disseminated intravascular coagulations, 11 myocardial infarctions, 4 pulmonary embolisms, 3 thrombotic cerebrovascular accidents, 3 deep vein thromboses, 3 superficial vein thromboses, 6 unspecified thromboses (unreported locations), and 3 fibrinogen reductions. No thrombotic microangiopathic events were reported. Of the 39 included studies, 31 (79%) reported no TEEs. The pooled TEE estimated IR was 2.87 (95% CI, 0.32-25.40) per 100 000 AICC infusions (Figure 2), with significant heterogeneity among studies (P < .01). When stratifying for retrospective3,12-24,26,27,29,30,32,34-37,41 and prospective studies,2,5,8-11,25,28,31,33,38-40,42,43 35 TEEs per 649 343 AICC infusions (pooled IR, 5.42 per 100 000 infusions; 95% CI, 0.92-31.82) and 11 TEEs per 29 104 AICC infusions (pooled IR, 1.09 per 100 000 infusions; 95% CI, 0.01-238.77) were reported, respectively. We further stratified the studies according to year of publication to evaluate a potential time effect by defining 3 groups of studies: from 1980 to 2004 (10 studies3,8-16), 2005 to 2010 (17 studies2,5,17-31), and 2011 to March 2017 (12 studies32-43). The pooled IRs were 5.46 (95% CI, 3.39-8.87), 0.51 (95% CI, 0-2806.06), and 8.30 (95% CI, 0.49-139.33) per 100 000 AICC infusions, respectively, with no statistically significant effect of publication year on TEE IR as evaluated by the metaregression model (P = .18).
Figure 2.
Forest plot for the meta-analysis of TEE IR in patients with congenital hemophilia with inhibitors or acquired hemophilia exposed to AICC. Results are expressed per 100 000 AICC infusions.
The pooled TEE IR in patients with acquired hemophilia15,17,40,42,43 was 287.79 (95% CI, 31.04-2668.08) per 100 000 AICC infusions, whereas in patients with congenital hemophilia,2,5,8-11,13,16,18,20-33,36,37,39,41,43 it was <0.01 per 100 000 infusions. Moreover, the pooled IR in patients treated on demand with AICC2,5,8-11,15-18,23,28,29,32,33,36,37,39,42,43 was 5.09 (95% CI, 0.01-1795.60) per 100 000 infusions, whereas in patients treated with prophylaxis,13,18,21,26,31,33,39,41,43 no TEEs were reported.
When considering 11 studies in patients with hemophilia with inhibitors undergoing surgery,14,17-20,22,24,27,30,34,38 5 TEEs were reported (Table 1), with a pooled IR of 112.03 (95% CI, 24.66-509.08) per 100 000 AICC infusions.
Table 1.
Description of 5 thromboembolic events reported in 4 patients who had undergone surgery
| Reference | Study type | Type of hemophilia | Procedure type | AICC dose | TEE | Notes |
|---|---|---|---|---|---|---|
| 19 | Observational retrospective | Congenital hemophilia A | Major sigmoidectomy | 104 U/kg per day × 13 d | Non-ST elevation myocardial infarction | |
| 34 | Observational retrospective | Congenital hemophilia A | Hernia repair | 158 U/Kg per day × 7 d | Numerous cerebral infarcts | Patient seemed confused after 6 d from surgery, and at day 7, he was agitated with expressive dysphasia. The symptoms resolved within 2 mo. |
| 38 | Observational prospective | Not reported (congenital or acquired hemophilia A) | Total hip replacement | Not reported | DVT in the brachial vein | Treatment with FEIBA was stopped, and the patient did not receive any specific anticoagulant therapy. Three days later, ultrasonographic analysis revealed that the DVT had resolved, but the SVT persisted. When ultrasonography was repeated 5 d later, no further progression was observed in the SVT, and the swelling had resolved. The patient resumed treatment with FEIBA and did not experience any additional thrombotic complications. |
| SVTs in the basilic and cephalic veins of the left arm | ||||||
| 38 | Observational prospective | Not reported (congenital or acquired hemophilia A) | Moderate-risk surgery | Not reported | Clot in an arteriovenous fistula | In this instance, FEIBA administration was permanently discontinued, and heparin (IV) was administered throughout the night, after which the patient recovered completely. A tranexamic acid-soaked gauze, applied locally to the patient’s hand, was unlikely to have contributed to thrombosis in this instance. |
DVT, deep vein thrombosis; SVT, superficial vein thrombosis.
Discussion
In summary, the overall pooled IR was lower than 3 TEEs per 100 000 AICC infusions, confirming previous figures reported in smaller and retrospective cohorts.3,12 Stratified analysis showed low TEE incidence in patients with congenital hemophilia compared with those with acquired hemophilia. This finding can probably be explained by the potential presence of other thrombotic risk factors in patients with acquired hemophilia A.44-46 Interestingly, no TEEs were reported during prophylaxis with AICC (ie, repeated AICC exposure for long periods of time with the consequent supernormal levels of factor X and prothrombin and increased thrombin generation and endogenous thrombin potential).4
To estimate how many AICC infusions to which a single patient with hemophilia with inhibitors would be exposed during his or her lifetime, we applied the prophylactic and on-demand regimens reported in the Pro-FEIBA clinical trial33 to a time horizon of 70 years. We estimated that a patient treated with AICC prophylaxis would receive in his or her lifetime 203 infusions per year (183 for prophylaxis and 20 to manage 10 breakthrough bleeds), corresponding to 14 210 infusions in 70 years of treatment. A patient treated on demand would experience 53 AICC infusions per year to manage 26.2 bleeds (ie, 3710 infusions in 70 years). This information is useful to understand the possible impact of the TEE IR estimated in our analysis.
We chose to include only data from published clinical trials, noninterventional prospective studies, and retrospective studies to obtain reliable information on exposure to AICC, which would allow us to estimate the IR of TEEs according to number of infusions. Case reports and spontaneous reports were not considered unless previously included in published studies, as was the case for the studies by Ehrlich et al12 and Aledort.3 Case reports were not included in the meta-analysis, because they cannot provide a reliable estimate of exposure to AICC, and consequently of the IR of TEEs, being specifically focused on describing a single event without considering all treated patients who did not experience any TEEs.47,48 Because of the nature of these 2 studies by Ehrlich et al12 and Aledort,3 which were based on published and unpublished spontaneously reported TEEs documented through the Baxter BioScience Pharmacovigilance Program and the US Food and Drug Administration MedWatch databases, respectively, we carried out a sensitivity analysis by removing them; the pooled IR then decreased to 1.13 (95% CI, 0.04-35.05).
In conducting a meta-analysis based on published aggregated data without access to individual patient data, we could not address potential confounders or evaluate associated risk factors (eg, ICC dose). A large cohort study or individual patient-level meta-analysis should be performed to adjust the TEE IR for confounders or associated risk factors. However, because congenital and acquired hemophilia are rare diseases, and TEEs occurring in those receiving AICC even rarer, such study designs would require longer times and multicenter collaborations, which can often be difficult and resource demanding. Nevertheless, our analysis showed a higher incidence of TEEs in patients with acquired hemophilia, in whom the potential association between TEEs, age, and comorbidities might play a role, and in those with congenital hemophilia who had undergone surgery.49
Because TEEs are rare, the classic meta-analytic model based on the inverse variance approach could not be fitted. Data were analyzed with a generalized linear mixed model based on a Poisson distribution6 to account for the presence of sparse data, thus avoiding the use of a correction factor for studies reporting 0 events; however, CIs were somewhat wide because of the small number of TEEs reported in the 39 studies included in the meta-analysis.
No thrombotic microangiopathic events were reported. However, a recently published article50 reporting results from the HAVEN 1 clinical trial in patients with hemophilia A and inhibitors treated prophylactically with emicizumab described 5 severe adverse events (2 thromboembolic events and 3 thrombotic microangiopathies), which occurred in 5 of 28 patients to whom AICC was administered as rescue therapy for the treatment of breakthrough bleeds. The reported thrombotic microangiopathies were diagnosed as hemolytic uremic syndromes. Hemolytic uremic syndromes such as those observed in the HAVEN 1 study had never been observed with AICC or published before. Moreover, the overall frequency of TEEs observed in that study (1 event per 13-52 estimated infusions) seems higher than that in any other published study.
In conclusion, our systematic review and meta-analysis of published study data provide a comprehensive and exhaustive estimate of the overall, 40-year thromboembolic safety profile of AICC in patients with hemophilia with inhibitors, showing that AICC is associated with a low incidence of TEEs.
Acknowledgment
This study was supported in part by research funding from Shire, Chicago, IL.
Authorship
Contribution: M.R. and P.A.C. carried out the systematic literature review and meta-analysis; all authors had full access to the data, take responsibility for data integrity and analysis, discussed the results, and contributed to the article preparation; and P.A.C., M.R., and L.G.M. had final responsibility for the decision to submit for publication.
Conflict-of-interest disclosure: P.A.C. received a research grant from Baxalta, now part of Shire, and speaking honoraria from Pfizer. L.G.M. reports personal fees from Pfizer and Bayer Healthcare. A.G. and R.C. are employed by Shire. M.R. declares no competing financial interests.
Correspondence: Paolo A. Cortesi, Research Centre on Public Health, University of Milan-Bicocca, Via G. Pergolesi 33, 20900 Monza, Italy; e-mail: paolo.cortesi@unimib.it.
References
- 1.Leissinger CA, Singleton T, Kruse-Jarres R. How I use bypassing therapy for prophylaxis in patients with hemophilia A and inhibitors. Blood. 2015;126(2):153-159. [DOI] [PubMed] [Google Scholar]
- 2.Astermark J, Donfield SM, DiMichele DM, et al. ; FENOC Study Group. A randomized comparison of bypassing agents in hemophilia complicated by an inhibitor: the FEIBA NovoSeven Comparative (FENOC) study. Blood. 2007;109(2):546-551. [DOI] [PubMed] [Google Scholar]
- 3.Aledort LM. Comparative thrombotic event incidence after infusion of recombinant factor VIIa versus factor VIII inhibitor bypass activity. J Thromb Haemost. 2004;2(10):1700-1708. [DOI] [PubMed] [Google Scholar]
- 4.Varadi K, Tangada S, Loeschberger M, et al. Pro- and anticoagulant factors facilitate thrombin generation and balance the haemostatic response to FEIBA(®) in prophylactic therapy. Haemophilia. 2016;22(4):615-624. [DOI] [PubMed] [Google Scholar]
- 5.Young G, Shafer FE, Rojas P, Seremetis S. Single 270 microg kg(-1)-dose rFVIIa vs. standard 90 microg kg(-1)-dose rFVIIa and APCC for home treatment of joint bleeds in haemophilia patients with inhibitors: a randomized comparison. Haemophilia. 2008;14(2):287-294. [DOI] [PubMed] [Google Scholar]
- 6.Stijnen T, Hamza TH, Ozdemir P. Random effects meta-analysis of event outcome in the framework of the generalized linear mixed model with applications in sparse data. Stat Med. 2010;29(29):3046-3067. [DOI] [PubMed] [Google Scholar]
- 7.Schwarzer G. meta: An R package for meta-analysis. R News. 2007;7(3):40-45. [Google Scholar]
- 8.Zwahlen H, Beck EA. Effects of low-dose ‘factor VIII inhibitor bypassing activity (FEIBA)’ in resistant haemophilia. Acta Haematol. 1980;64(1):12-17. [DOI] [PubMed] [Google Scholar]
- 9.Sjamsoedin LJ, Heijnen L, Mauser-Bunschoten EP, et al. The effect of activated prothrombin-complex concentrate (FEIBA) on joint and muscle bleeding in patients with hemophilia A and antibodies to factor VIII. A double-blind clinical trial. N Engl J Med. 1981;305(13):717-721. [DOI] [PubMed] [Google Scholar]
- 10.Hilgartner MW, Knatterud GL. The use of factor eight inhibitor by-passing activity (FEIBA immuno) product for treatment of bleeding episodes in hemophiliacs with inhibitors. Blood. 1983;61(1):36-40. [PubMed] [Google Scholar]
- 11.Hilgartner M, Aledort L, Andes A, Gill J; FEIBA Study Group. Efficacy and safety of vapor-heated anti-inhibitor coagulant complex in hemophilia patients. Transfusion. 1990;30(7):626-630. [DOI] [PubMed] [Google Scholar]
- 12.Ehrlich HJ, Henzl MJ, Gomperts ED. Safety of factor VIII inhibitor bypass activity (FEIBA): 10-year compilation of thrombotic adverse events. Haemophilia. 2002;8(2):83-90. [DOI] [PubMed] [Google Scholar]
- 13.Hilgartner MW, Makipernaa A, Dimichele DM. Long-term FEIBA prophylaxis does not prevent progression of existing joint disease. Haemophilia. 2003;9(3):261-268. [DOI] [PubMed] [Google Scholar]
- 14.Quintana-Molina M, Martínez-Bahamonde F, González-García E, et al. Surgery in haemophilic patients with inhibitor: 20 years of experience. Haemophilia. 2004;10(Suppl 2):30-40. [DOI] [PubMed] [Google Scholar]
- 15.Sallah S. Treatment of acquired haemophilia with factor eight inhibitor bypassing activity. Haemophilia. 2004;10(2):169-173. [DOI] [PubMed] [Google Scholar]
- 16.Schneiderman J, Nugent DJ, Young G. Sequential therapy with activated prothrombin complex concentrate and recombinant factor VIIa in patients with severe haemophilia and inhibitors. Haemophilia. 2004;10(4):347-351. [DOI] [PubMed] [Google Scholar]
- 17.Holme PA, Brosstad F, Tjønnfjord GE. Acquired haemophilia: management of bleeds and immune therapy to eradicate autoantibodies. Haemophilia. 2005;11(5):510-515. [DOI] [PubMed] [Google Scholar]
- 18.Dimichele D, Négrier C. A retrospective postlicensure survey of FEIBA efficacy and safety. Haemophilia. 2006;12(4):352-362. [DOI] [PubMed] [Google Scholar]
- 19.Tjønnfjord GE. Surgery in patients with hemophilia and inhibitors: a review of the Norwegian experience with FEIBA. Semin Hematol. 2006;43(2 Suppl 4):S18-S21. [DOI] [PubMed] [Google Scholar]
- 20.Kraut EH, Aledort LM, Arkin S, Stine KC, Wong WY. Surgical interventions in a cohort of patients with haemophilia A and inhibitors: an experiential retrospective chart review. Haemophilia. 2007;13(5):508-517. [DOI] [PubMed] [Google Scholar]
- 21.Leissinger CA, Becton DL, Ewing NP, Valentino LA. Prophylactic treatment with activated prothrombin complex concentrate (FEIBA) reduces the frequency of bleeding episodes in paediatric patients with haemophilia A and inhibitors. Haemophilia. 2007;13(3):249-255. [DOI] [PubMed] [Google Scholar]
- 22.Rodriguez-Merchan EC, Quintana M, Jimenez-Yuste V, Hernández-Navarro F. Orthopaedic surgery for inhibitor patients: a series of 27 procedures (25 patients). Haemophilia. 2007;13(5):613-619. [DOI] [PubMed] [Google Scholar]
- 23.Schneiderman J, Rubin E, Nugent DJ, Young G. Sequential therapy with activated prothrombin complex concentrates and recombinant FVIIa in patients with severe haemophilia and inhibitors: update of our previous experience. Haemophilia. 2007;13(3):244-248. [DOI] [PubMed] [Google Scholar]
- 24.Stine KC, Shrum D, Becton DL. Use of FEIBA for invasive or surgical procedures in patients with severe hemophilia A or B with inhibitors. J Pediatr Hematol Oncol. 2007;29(4):216-221. [DOI] [PubMed] [Google Scholar]
- 25.Holme PA, Glomstein A, Grønhaug S, Tjønnfjord GE. Home treatment with bypassing products in inhibitor patients: a 7.5-year experience. Haemophilia. 2009;15(3):727-732. [DOI] [PubMed] [Google Scholar]
- 26.Jiménez-Yuste V, Alvarez MT, Martín-Salces M, et al. Prophylaxis in 10 patients with severe haemophilia A and inhibitor: different approaches for different clinical situations. Haemophilia. 2009;15(1):203-209. [DOI] [PubMed] [Google Scholar]
- 27.Lauroua P, Ferrer AM, Guérin V. Successful major and minor surgery using factor VIII inhibitor bypassing activity in patients with haemophilia A and inhibitors. Haemophilia. 2009;15(6):1300-1307. [DOI] [PubMed] [Google Scholar]
- 28.Martinowitz U, Livnat T, Zivelin A, Kenet G. Concomitant infusion of low doses of rFVIIa and FEIBA in haemophilia patients with inhibitors. Haemophilia. 2009;15(4):904-910. [DOI] [PubMed] [Google Scholar]
- 29.Smejkal P, Brabec P, Matyskova M, et al. FEIBA in treatment of acute bleeding episodes in patients with haemophilia A and factor VIII inhibitors: a retrospective survey in regional haemophilia centre. Haemophilia. 2009;15(3):743-751. [DOI] [PubMed] [Google Scholar]
- 30.Balkan C, Karapinar D, Aydogdu S, et al. Surgery in patients with haemophilia and high responding inhibitors: Izmir experience. Haemophilia. 2010;16(6):902-909. [DOI] [PubMed] [Google Scholar]
- 31.Ettingshausen CE, Kreuz W. Early long-term FEIBA prophylaxis in haemophilia A patients with inhibitor after failing immune tolerance induction: a prospective clinical case series. Haemophilia. 2010;16(1):90-100. [DOI] [PubMed] [Google Scholar]
- 32.Gringeri A, Fischer K, Karafoulidou A, Klamroth R, López-Fernández MF, Mancuso E; European Haemophilia Treatment Standardisation Board (EHTSB). Sequential combined bypassing therapy is safe and effective in the treatment of unresponsive bleeding in adults and children with haemophilia and inhibitors. Haemophilia. 2011;17(4):630-635. [DOI] [PubMed] [Google Scholar]
- 33.Leissinger C, Gringeri A, Antmen B, et al. Anti-inhibitor coagulant complex prophylaxis in hemophilia with inhibitors. N Engl J Med. 2011;365(18):1684-1692. [DOI] [PubMed] [Google Scholar]
- 34.Rangarajan S, Yee TT, Wilde J. Experience of four UK comprehensive care centres using FEIBA® for surgeries in patients with inhibitors. Haemophilia. 2011;17(1):28-34. [DOI] [PubMed] [Google Scholar]
- 35.Holmström M, Tran HT, Holme PA. Combined treatment with APCC (FEIBA®) and tranexamic acid in patients with haemophilia A with inhibitors and in patients with acquired haemophilia A--a two-centre experience. Haemophilia. 2012;18(4):544-549. [DOI] [PubMed] [Google Scholar]
- 36.Zülfikar B, Aydogan G, Salcioglu Z, et al. ; FEIBA Investigators Team. Efficacy of FEIBA for acute bleeding and surgical haemostasis in haemophilia A patients with inhibitors: a multicentre registry in Turkey. Haemophilia. 2012;18(3):383-391. [DOI] [PubMed] [Google Scholar]
- 37.Han MH, Park YS. Sequential therapy with activated prothrombin complex concentrates and recombinant activated factor VII to treat unresponsive bleeding in patients with hemophilia and inhibitors: a single center experience. Blood Res. 2013;48(4):282-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Négrier C, Lienhart A, Numerof R, et al. SURgical interventions with FEIBA (SURF): international registry of surgery in haemophilia patients with inhibitory antibodies. Haemophilia. 2013;19(3):e143-e150. [DOI] [PubMed] [Google Scholar]
- 39.Antunes SV, Tangada S, Stasyshyn O, et al. Randomized comparison of prophylaxis and on-demand regimens with FEIBA NF in the treatment of haemophilia A and B with inhibitors. Haemophilia. 2014;20(1):65-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Borg JY, Négrier C, Durieu I, Dolimier E, Masquelier AM, Lévesque H; FEIBHAC Study Group. FEIBA in the treatment of acquired haemophilia A: results from the prospective multicentre French ‘FEIBA dans l’hémophilie A acquise’ (FEIBHAC) registry. Haemophilia. 2015;21(3):330-337. [DOI] [PubMed] [Google Scholar]
- 41.Ewing N, Escuriola-Ettingshausen C, Kreuz W. Prophylaxis with FEIBA in paediatric patients with haemophilia A and inhibitors. Haemophilia. 2015;21(3):358-364. [DOI] [PubMed] [Google Scholar]
- 42.Zanon E, Milan M, Gamba G, et al. Activated prothrombin complex concentrate (FEIBA®) for the treatment and prevention of bleeding in patients with acquired haemophilia: a sequential study. Thromb Res. 2015;136(6):1299-1302. [DOI] [PubMed] [Google Scholar]
- 43.Negrier C, Voisin S, Baghaei F, et al. ; FEIBA PASS Study Group. Global Post-Authorization Safety Surveillance Study: real-world data on prophylaxis and on-demand treatment using FEIBA (an activated prothrombin complex concentrate). Blood Coagul Fibrinolysis. 2016;27(5):551-556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Collins P, Baudo F, Huth-Kühne A, et al. Consensus recommendations for the diagnosis and treatment of acquired hemophilia A. BMC Res Notes. 2010;3(1):161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Huth-Kühne A, Baudo F, Collins P, et al. International recommendations on the diagnosis and treatment of patients with acquired hemophilia A. Haematologica. 2009;94(4):566-575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sumner MJ, Geldziler BD, Pedersen M, Seremetis S. Treatment of acquired haemophilia with recombinant activated FVII: a critical appraisal. Haemophilia. 2007;13(5):451-461. [DOI] [PubMed] [Google Scholar]
- 47.Girolami A, Scandellari R, Zanon E, Sartori R, Girolami B. Non-catheter associated venous thrombosis in hemophilia A and B. A critical review of all reported cases. J Thromb Thrombolysis. 2006;21(3):279-284. [DOI] [PubMed] [Google Scholar]
- 48.Girolami A, Ruzzon E, Fabris F, Varvarikis C, Sartori R, Girolami B. Myocardial infarction and other arterial occlusions in hemophilia a patients. A cardiological evaluation of all 42 cases reported in the literature. Acta Haematol. 2006;116(2):120-125. [DOI] [PubMed] [Google Scholar]
- 49.Hermans C, Hammer F, Lobet S, Lambert C. Subclinical deep venous thrombosis observed in 10% of hemophilic patients undergoing major orthopedic surgery. J Thromb Haemost. 2010;8(5):1138-1140. [DOI] [PubMed] [Google Scholar]
- 50.Oldenburg J, Mahlangu JN, Kim B, et al. Emicizumab prophylaxis in hemophilia A with inhibitors. N Engl J Med. 2017;377(9):809-818. [DOI] [PubMed] [Google Scholar]