Abstract
Background
Little is known about synergistic effects of several risk factors on asthma. We developed a risk score in Puerto Rican children, and then used this score to estimate the combined effects of multiple risk factors on asthma at school age in Puerto Rican and Swedish children.
Methods
Case-control study in 609 Puerto Rican children (aged 6–14 years) and longitudinal birth cohort study of 2,290 Swedish children followed up to age 12 years (The Children, Allergy, Milieu, Stockholm, Epidemiological Survey [BAMSE] Study). In both cohorts, there was data on parental asthma, sex, obesity, allergic rhinitis, and early-life second-hand smoke (SHS); data on diet and (in children ≥9 years) lifetime exposure to gun violence were also available in the Puerto Rico study. Asthma was defined as physician-diagnosed asthma and ≥1 episode of wheeze in the previous year.
Results
In a multivariable analysis in Puerto Rican children, male sex, parental asthma, allergic rhinitis, early-life SHS, an unhealthy diet and (in children ≥9 years) gun violence were each significantly associated with asthma. We next created a risk score using these variables (range, 0 to 5–6 in Puerto Rico and 0 to 4 in BAMSE). Compared with Puerto Rican children without any risk factors (i.e. a score of 0), Puerto Rican children with 2, 3, and at least 4 risk factors had 3.6 times (95% CI=1.4–9.2), 10.4 times (95% CI=4.0–27.0), and 21.6 times (95% CI=7.2–64.9) significantly higher odds of asthma, respectively. In BAMSE, the presence of 2, 3, and at least 4 risk factors was significantly associated with 4.1 times (95% CI=2.3–7.4), 6.3 times (95% CI=3.0–13.3), and 17.2 times (95% CI=4.1–73.2) increased odds of asthma at age 12 years.
Conclusions
Our findings emphasize the multifactorial etiology of asthma, and suggest that concurrent eradication or reduction of several modifiable risk factors may better prevent or reduce the burden of childhood asthma.
Keywords: asthma, risk score, children, multifactorial
INTRODUCTION
Asthma is the most common chronic respiratory disease and a major public health problem among children worldwide, including those living in the United States (U.S.) and Sweden (1). In the U.S., the prevalence of asthma at school age is higher in Puerto Ricans (16.1%) than in non-Hispanic (NH) blacks (11.2%), NH whites (7.7%) or Mexicans (5.4%)(2). Among Swedish children aged 7 to 8 years, estimates of the prevalence of physician-diagnosed asthma and current wheeze were 7.4% and 13% in 2006 (3).
A growing body of literature supports a multifactorial etiology for childhood asthma, including combined or interacting effects of non-modifiable (i.e. heredity and sex) and modifiable (i.e. environment and behavior) risk factors. Indeed, current evidence suggests causal roles for potentially modifiable exposures or behaviors on asthma, including but not limited to secondhand smoke (SHS), overweight or obesity, unhealthy dietary patterns, changes in the gut microbiome, chronic pre- and perinatal stress, and indoor and outdoor pollutants (4). Although children in high-risk populations are often concurrently exposed to several of these risk factors, most published studies have focused on a single risk factor (adjusting for the presence of other risk factors) or on the interaction between two risk factors for asthma (5, 6).
In this study, we aimed to estimate the combined effects of risk factors for asthma in two studies of school-aged children. We first identified risk factors for asthma in a cross-sectional case-control study of Puerto Rican children ages 6 to 14 years, and built a risk score based on this information. We then tried to replicate our findings for the risk score in a longitudinal birth cohort study of Swedish children, in whom risk factors were identified at ages 1 to 4 years, and asthma was then assessed at the ages of 8 and 12 years. Using the risk score, we then estimated the combined effects of several risk factors on childhood asthma in two studies that differ with regard to overall design, geographic location, and population characteristics (e.g., racial ancestry, environment, and socioeconomic factors).
METHODS
Subject recruitment and study procedures
Puerto Rico
Details on subject recruitment and study design have been previously described (7). In brief, from March 2009 to June 2010, children were recruited from randomly selected households in San Juan, using a multistage probabilistic sampling design. A household was eligible if ≥1 resident was a child aged 6 to 14 years who had four Puerto Rican grandparents and had lived in the household for at least one year. Of 1,111 eligible households, 438 (~39%) had ≥1 child with asthma (defined as physician-diagnosed asthma and at least one episode of wheeze in the prior year). From those 438 households, one child with asthma was selected (at random, if there was more than one such child). Similarly, one child without asthma was randomly selected from the remaining 673 households. In an effort to reach a target sample size of ~700 children (which would give us ≥90% power to detect an odds ratio (OR) ≥2 for exposures with a prevalence ≥25%), we attempted to enroll a random sample (n=783) of these 1,111 children. Parents of 105 of these 783 eligible households refused to participate or could not be reached. There were no significant differences in age, gender, or area of residence between eligible children who did (n=678 [86.6%]) and did not (n=105 [13.4%]) agree to participate. Of the 678 study participants, 609 (89.8%) had complete data on body mass index (BMI), and are thus included in the current analysis.
The caretaker of study participants (usually [≥93%] the mother) completed two questionnaires, the first on the child’s general and respiratory health (which was used to obtain information on demographics, socioeconomic status, family history and SHS), and the second on the child’s food consumption in the prior week. The Exposure to Violence (ETV) survey (8) was also administered to participants 9 years and older. Internal consistency, test-retest reliability and validity have been established for both the English and Spanish versions of the ETV survey (9). Height and weight were measured in all participants to the nearest centimeter and pound, respectively.
Written parental consent was obtained for participating children, from whom written assent was also obtained. The study was approved by the Institutional Review Boards of the University of Puerto Rico (San Juan, PR) and the University of Pittsburgh (Pittsburgh, PA).
The Children, Allergy, Milieu, Stockholm, Epidemiological Survey (BAMSE) Study
Subject recruitment and baseline characteristics of participants in the BAMSE Swedish birth cohort study have been previously described (10, 11). In brief, between 1994 and 1996, 4,089 newborn infants were recruited and questionnaire data were obtained. Subjects were recruited from central and northwestern parts of Stockholm, including both urban and suburban districts. Questionnaires on environment and lifestyle, as well as symptoms related to asthma and other allergic diseases were administered to the parents of participants when they were 1, 2, 4, 8 and 12 years of age. The response rates at ages 1, 2, 4, 8 and 12 years were 96%, 94%, 91%, 84%, and 82%, respectively. In this study, we included children with complete data up to 8 (n=2,339) and 12 (n=2,290) years.
The study was approved by the ethics committee at the Karolinska Institute, and parental consent was obtained for all children included in this report.
Statistical Analysis
The primary outcome of interest was asthma, defined in both the Puerto Rico study and in BAMSE as physician-diagnosed asthma and at least one episode of wheeze in the previous year.
On the basis of their prior association with childhood asthma in our study in Puerto Rico, we examined the following variables: age, sex, low household income (defined as <$15,000/year, the median household income for Puerto Rico in 2008–2009) (12), parental (paternal or maternal) history of asthma, exposure to SHS in early life (in utero or before age 2 years)(13), allergic rhinitis (defined as physician-diagnosed allergic rhinitis and naso-ocular symptoms apart from colds in the previous year) (14), obesity (defined as a BMI z-score ≥95th percentile)(15), an unhealthy diet (a score of 1 or 2 in a diet scale, indicating higher consumption of sweets and dairy products)(16), and (in children 9 years and older only) lifetime exposure to gun violence (defined as having heard two or more gunshots) (17). Parental asthma, early-life SHS, allergic rhinitis (at age 4 years, when this diagnosis is more common), and obesity (at age 4 years) were defined in BAMSE in the same manner as in the Puerto Rico study. Data on exposure to violence or diet were not available in BAMSE.
Bivariate analyses were conducted using Fisher’s exact tests for binary variables and two-tailed t-tests for pairs of binary and continuous variables. A backward stepwise regression approach was used to build the multivariable models in the Puerto Rico study. The initial models included all variables listed above. Variables that were significantly associated with asthma at P <0.05 or changed the effect estimate ([OR]) ≥10% were included in the final models. In Puerto Rico, separate models were built for all children (ages 6 to 14 years) and for children 9 years and older. Variables from the final models were then used to create a risk score for each age group in Puerto Rico, and then in BAMSE.
For the risk score, population attributable risk (PAR) estimates proportion of the incidence of a disease in the population (exposed and unexposed) that is due to the exposure. It is the incidence of disease in the population that would be eliminated if exposure were eliminated. The PAR was calculated by subtracting the incidence in the unexposed (Iu) from the incidence in total population (exposed and unexposed) (Ip). Population attributable risk percent (PAR%) was then calculated by dividing the PAR by the incidence in the total population and then multiplying by 100: [(Ip−Iu)/Ip]*100.
SAS version 9.3 (SAS Institute, Cary, NC) and STATA (release 13; Stata Corp., College Station, TX, USA) were used for data analysis.
RESULTS
The main characteristics of the 609 participants in the Puerto Rico study are summarized in Table 1. Compared with control subjects, children with asthma (cases) were significantly younger and more likely to be male, to have been exposed to SHS in early life, and to have a parental history of asthma, allergic rhinitis and an unhealthy diet. Among 426 children ages 9 and older, cases were also more likely to have ever been exposed to gun violence than control subjects. There was no significant difference in household income between cases and control subjects.
Table 1.
Main characteristics of participants in the Puerto Rico and BAMSEa studies
| Puerto Rico | BAMSE (Sweden) | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Subjects aged 6 to 14 years (n=609) | Subjects aged 9 to 14 years (n=426) | At age 8 years (n=2,339) | At age 12 years (n=2,290) | |||||
|
|
||||||||
| Variableb | Controls (n=297) | Cases (n=312) | Controls (n=215) | Cases (n=211) | Controls (n=2,211) | Cases (n=118) | Controls (n=2,169) | Cases (n=121) |
| Age (years) | 10.51 (2.7) | †10.06 (2.6) | 11.87 (1.8) | †11.47 (1.9) | 8.17 (0.5) | 8.19 (0.4) | 12.97 (0.83) | 12.92 (0.77) |
| Male sex | 143 (48.2%) | 185 (59.3%)‡ | 101 (46.9%) | †123(58.3%) | 1086 (48.9%) | 71 (60.2%)† | 1062 (49.0%) | ‡80 (66.1%) |
| Parental asthmac | 93 (31.4%) | 210 (67.5%)‡ | 69 (32.2%) | 137 (64.9%)‡ | 405 (18.2%) | 43 (36.4%)† | 386 (17.8%) | ‡44 (36.4%) |
| Obesityd | 53 (17.9%) | 69 (22.1%) | 36 (16.74%) | 48 (22.8%) | 194 (8.7%) | 17 (14.4%)† | 189 (8.7%) | 16 (13.2%) |
| Allergic rhinitise | 16 (5.4%) | 51 (16.5%)‡ | 13 (6.1%) | 36 (17.2%)‡ | 26 (1.2%) | 8 (6.8%)‡ | 22 (1.0%) | ‡10 (8.3%) |
| Early-life second-hand smoke (SHS)f | 121 (40.9%) | 158 (50.6%)‡ | 83 (38.8%) | 107 (50.7%)† | 598 (26.9%) | 35 (30.0%) | 576 (26.6%) | 41 (33.9%) |
| Household income >$15,000 per yearg | 100 (35.3%) | 98 (32.1%) | 84 (40.2%) | 69 (33.2%) | – | – | – | – |
| Unhealthy diet8 | 85 (28.6%) | 142 (45.5%)‡ | 56 (26.1%) | 102 (48.3%)‡ | – | – | – | – |
| Heard more than two gunshots (lifetime) | – | – | 111 (51.9%) | 141 (68.0%)‡ | – | – | – | – |
Children, Allergy, Milieu, Stockholm, Epidemiological Survey
Data shown as mean (standard deviation) for age, and as number (percentage for all other variables).
Paternal or maternal history of asthma;
A body mass-index z-score >95th percentile (at school-age in Puerto Rico, at age 4 years in BAMSE),
Physician-diagnosed allergic rhinitis and naso-ocular symptoms apart from colds in the previous year (at school-age in Puerto Rico, at age 4 years in BAMSE);
In utero or before age 2 years;
Above the median household income in Puerto Rico at the time of the study, and 8 a diet high in dairy products, sweets, snacks and soda
P-value <.05 and
P-value <.01 for the comparison between cases and controls
The main characteristics of the BAMSE participants at ages 8 and 12 years are shown in Table 1. Compared with control subjects, cases were significantly more likely to be male and to have a parental history of asthma, to have a diagnosis of allergic rhinitis at age 4 years, and to be obese at age 4 years.
Table 2 shows the results of the bivariate and multivariable analyses of asthma in Puerto Rico. After adjusting for age and household income, the following variables remained significantly associated with increased odds of asthma among the 609 Puerto Rican participants aged 6 to 14 years: male sex, parental asthma, allergic rhinitis, early-life SHS, and an unhealthy diet. In the multivariable analysis restricted to 426 Puerto Rican children aged 9 and older, male sex, parental asthma, allergic rhinitis, an unhealthy diet, and lifetime exposure to gun violence were significantly associated with increased odds of asthma. In both age groups, there was also a non-statistically significant trend for an association between obesity and asthma (P=0.06–0.07).
Table 2.
Analysis of asthma among children participating in the Puerto Rico study
| At ages 6 to 14 years (n=609) | At ages 9 to 14 years (n=426) | |||
|---|---|---|---|---|
|
| ||||
| Odds ratio (95% confidence interval), P value | ||||
| Unadjusted | Adjustedg | Unadjusted | Adjustedg | |
| Male sex | 1.6 (1.1–2.2), <0.01 | 1.9 (1.3–2.8), <0.01 | 1.6 (1.1–2.3), <0.01 | 1.9 (1.2–3.2), <0.01 |
| Parental asthmaa | 4.5 (3.2–6.4), <0.01 | 4.6 (3.1–6.7), <0.01 | 3.9 (2.6–5.8), <0.01 | 4.5 (2.8–7.3), <0.01 |
| Obesitya | 1.3 (0.9–1.9), 0.19 | 1.6 (0.97–2.4), 0.07 | 1.5 (0.9–2.4), 0.12 | 1.7 (0.98–3.0), 0.06 |
| Allergic rhinitisc | 3.4 (1.9–6.2), <0.01 | 3.9 (1.9–7.6), <0.01 | (3.2 (1.6–6.2), <0.01 | 3.9 (1.8–8.4), <0.01 |
| Early-life second-hand smoke (SHS)d | 1.5 (1.1–2.0), 0.02 | 1.5 (1.0–2.2), 0.03 | 1.6 (1.1–2.4), 0.01 | 1.5 (0.9–2.4), 0.09 |
| Unhealthy diete | 2.1 (1.5–2.9), <0.01 | 2.3 (1.6–3.4), <0.01 | 2.7 (1.8–4.0), <0.01 | 2.9 (1.8–4.7), <0.01 |
| Heard more than two gunshots, lifetimef | – | – | 2.0 (1.3–2.9), <0.01 | 1.8 (1.1–2.9), 0.02 |
Paternal or maternal history of asthma
A body mass-index z-score >95th percentile
Physician-diagnosed allergic rhinitis and naso-ocular symptoms apart from colds in the previous year;
In utero or before age 2 years
A diet high in dairy products, sweets, snacks and soda; and
Only children 9 and older answered questions on exposure to violence
Model adjusted for age and household income, in addition to the variables listed in each column
On the basis of the findings described above, we next evaluated the risk factors identified in the Puerto Rico study in BAMSE (except for diet and lifetime exposure to gun violence, which were not available in BAMSE). In a multivariable analysis, male sex, parental asthma, and allergic rhinitis at age 4 years were each significantly associated with asthma at ages 8 and 12 years (Table 3).
Table 3.
Analysis of asthma among children participating in BAMSEa
| At age 8 years (n=2,339) | At age 12 years (n=2,290) | |||
|---|---|---|---|---|
|
|
||||
| Odds ratio (95% confidence interval), P value | ||||
| Unadjusted | Adjusted | Unadjusted | Adjusted | |
| Male sex | 1.6 (1.1–2.3), 0.02 | 1.5 (1.0–2.2), 0.04 | 2.0 (1.4–3.0), <0.01 | 1.9 (1.3–2.8), <0.01 |
| Parental asthmab | 2.6 (1.7–3.8), <0.01 | 2.5 (1.7–3.7), <0.01 | 2.6 (1.8–3.9), <0.01 | 2.5 (1.7–3.7), <0.01 |
| Obesity at age 4 years | 1.8 (1.0–3.0), 0.04 | 1.7 (1.0–3.0), 0.06 | 1.6 (0.9–2.8), 0.09 | 1.5 (0.9–2.7), 0.15 |
| Allergic rhinitis at age 4 yearsd | 6.1 (2.7–14.0), <0.01 | 5.1 (2.2–11.8), <0.01 | 9.2 (4.2–20.4), <0.01 | 7.8 (3.5–17.6), <0.01 |
| Early-life second hand smoke (SHS)e | 1.1 (0.8–1.7), 0.52 | 1.1 (0.7–1.7), 0.60 | 1.4 (1.0–2.1), 0.08 | 1.4 (0.9–2.1), 0.09 |
The Children, Allergy, Milieu, Stockholm, Epidemiological Survey
Paternal or maternal history of asthma
A body mass-index z-score >95th percentile
Physician-diagnosed allergic rhinitis and naso-ocular symptoms apart from colds in the previous year
In utero or before age 2 years;
On the basis of our results in the Puerto Rico study, we included male sex, parental asthma, allergic rhinitis, obesity, an unhealthy diet and (in children 9 and older only) lifetime exposure to gun violence for risk score analyses in Puerto Rican children. In BAMSE, the following variables were included in the risk score: male sex, parental asthma, allergic rhinitis at age 4 years, and obesity at age 4 years. Thus, the risk score ranged from 0 (no risk factors) to: 4 (in BAMSE), 5 (in Puerto Rican children aged 6 to 14 years), and 6 (in Puerto Rican children 9 years and older).
Figure 1 and Supplemental Table e1 show the results of the analysis of the risk score and asthma in Puerto Rico and BAMSE. Compared with Puerto Rican children without any risk factors (i.e. a score of 0), Puerto Rican children with 2, 3, and at least 4 risk factors had 3.6 times, 10.4 times, and 21.6 times significantly higher odds of asthma, respectively (Fig. 1, Panel A). Among Puerto Rican children 9 years and older (Fig. 1, Panel B), the presence of 3 and at least 4 risk factors was significantly associated with 9.2 times and 16.3 times increased odds of asthma. In BAMSE, the presence of 2, 3, and 4 risk factors was associated with 3.3 times, 4.7 times, and 25.1 times increased odds of asthma at age 8 years (Fig. 1, Panel C), respectively. In BAMSE, the presence of 3 and at least 4 risk factors was significantly associated with 6.3 times and 17.2 times increased odds of asthma at age 12 years (Fig. 1, Panel D).
Figure 1. Odds ratios (log10 scale) of asthma by predicted risk score among children in the Puerto Rico study and BAMSEa (Sweden) study.
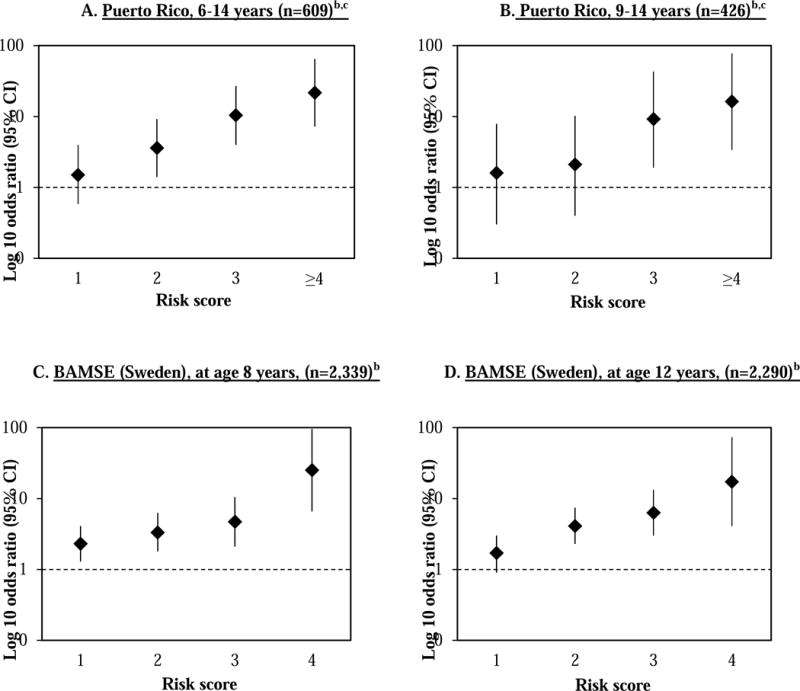
aThe Children, Allergy, Milieu, Stockholm, Epidemiological survey
bThe risk score included four variables in both cohorts: male sex, parental asthma, obesity (at age 4 years in BAMSE, and at the time of the study in Puerto Rico), allergic rhinitis (at age 4 years in BAMSE, and at the time of the study in Puerto Rico), and early-life second-hand smoke (assessed at ages 1–2 years in BAMSE, and at the time of the study in Puerto Rico)
cIn the Puerto Rico cohort, the risk score included all four variables listed above, plus unhealthy diet and (in children ages 9 to 14 years) exposure to gun violence.
Table 4 shows the prevalence and PAR for each modifiable risk factor among children in the Puerto Rico and BAMSE studies. In all Puerto Rican children, the PAR of asthma was: 2.6% for obesity, 8.8% for early-life SHS, and 13.1% for an unhealthy diet. Among Puerto Rican children aged 9 years and older, the PAR of asthma was: 3.8% for obesity, 10.9% for early-life SHS, 17.9% for an unhealthy diet, and 19.9% for exposure to gun violence. In BAMSE, the PAR of asthma at age 8 years was: 5.9% for obesity and 3.6% for early-life SHS; and that at age 12 years was: 4.5% for obesity and 9.5% for early-life SHS.
Table 4.
Population Attributable Risk (PAR) in the Puerto Rico and BAMSE studies
| Puerto Rico | All Children | Children 9 and older | ||
|---|---|---|---|---|
|
|
||||
| Prevalence | P.A.R. (%) | Prevalence | P.A.R. (%) | |
| Obesity | 20.0% | 2.6% | 19.7% | 3.8% |
| Early-life SHS | 45.9% | 8.8% | 44.7% | 10.9% |
| Unhealthy diet | 37.3% | 13.1% | 37.1% | 17.9% |
| Gun violence exposure | – | – | 60.3% | 19.9% |
|
| ||||
| BAMSE | 8years | 12 years | ||
|
|
||||
| Prevalence | P.A.R. (%) | Prevalence | P.A.R. (%) | |
|
| ||||
| Obesity | 9.0% | 5.9% | 9.0% | 4.5% |
| Early-life SHS | 27.1% | 3.6% | 26.9% | 9.5% |
DISCUSSION
Among Puerto Rican school-aged children, we show that the presence of three risk factors is associated with ten- to eleven-fold increased odds of asthma, compared to having no risk factors. In these children, having four or more risk factors is associated with nineteen- to twenty-one-fold increased odds of asthma. In a separate cohort of Swedish children, the presence of three of the identified risk factors at age 4 years was associated with approximately five to six times increased odds of asthma at age 8 or 12 years, and that of four or more risk factors at age 4 years was associated with seventeen to twenty-five increased odds of asthma at age 8 or 12 years.
Our findings emphasize the multifactorial etiology of asthma, and suggest that concurrent eradication or reduction of several modifiable risk factors in early childhood may better prevent or reduce asthma burden later in life. In particular, joint interventions to prevent or ameliorate SHS exposure and obesity in early childhood are likely to have a more beneficial effect on asthma at school age than either intervention alone (18, 19). Moreover, comprehensive approaches to the prevention of obesity at school age would include developing healthy dietary habits, along with engaging in regular physical activity, at an early age. This could further improve the impact of combined interventions, as dietary patterns such as a “Mediterranean diet” may have beneficial effects on asthma (20). Indeed, we previously showed that a diet characterized by frequent consumption of vegetables and grains, and low consumption of dairy products and sweets, is associated with reduced odds of asthma among Puerto Rican children at school age (adjusted odds ratio (aOR)= 0.64, 95% confidence interval (CI)= 0.53–0.77) (16). Moreover, recent data from the BAMSE cohort show that a diet with high total antioxidant capacity at age 8 years may decrease the risk of developing atopy and atopic asthma in adolescence (21). Early intervention efforts from single-food randomized controlled trials on fish oil-derived fatty acid, vitamin C or vitamin D supplementation during pregnancy also show promising effects on offspring asthma risk and lung function development (22–25).
Puerto Rican children are often exposed to violence (17). We previously showed that exposure to violence is associated with asthma in Puerto Rican school-aged children, in whom such association may be partly mediated by genetic and epigenetic variation in ADCYAP1R1 (the gene for adenylate cyclase activating polypeptide 1 receptor type 1, which has been implicated in the pathogenesis of post-traumatic stress disorder and childhood anxiety) (26). Moreover, we have also demonstrated that lifetime exposure to gun violence is linked to childhood asthma in Puerto Ricans (27). Although there has been no clinical trial of stress-reduction or violence avoidance in children, our results further support policy measures aimed to reduce violence, including gun violence, in under-served communities.
Atopy, atopic asthma and allergic diseases such as allergic rhinitis are common in Puerto Rican and Swedish children (11, 28). Moreover, allergic rhinitis is a frequent co-morbidity of atopic asthma (14, 29) and thus yet-to-be identified preventive measures against atopy and allergic rhinitis is likely to further impact the prevention of childhood asthma. Whereas parental asthma is a non-modifiable risk factor, any future multifactorial clinical trials should assess whether the impact of such interventions is greater in children with such parental history.
Our study has several limitations. First, the study in Puerto Rico was cross-sectional, thus precluding our ability to examine temporal relationships. However, we obtained similar results for a modified score (i.e. including fewer risk factors) in a longitudinal birth cohort study in Sweden. Second, we did not have data on some potentially important risk factors for childhood asthma in either Puerto Rico or Sweden, such as the gut microbiome, environmental microbial exposure or individual exposure to outdoor air pollution. Although genetic risk markers were not assessed in our predictive score, we included risk factors that are clinically relevant and do not involve laboratory studies. Moreover, genetic variants have not added much information to similar risk scores for other multifactorial diseases (30, 31).
In summary, our results highlight the synergistic effects of non-modifiable (parental asthma, male sex) and modifiable (obesity, an unhealthy diet, allergic rhinitis, early-life SHS, and exposure to gun violence) risk factors on childhood asthma. Clinical trials that concurrently address several modifiable risk factors (i.e. diet, obesity and SHS), together with sound policies to prevent severe violence in high-risk populations, may be more likely to have a beneficial effect on asthma prevention than single-factor interventions. Our results and study interpretation are thus in agreement with recent suggestions for prevention (32), but whether multifactorial interventions have an even greater effect on children with parental asthma and/or young boys should be addressed in the context of future trials.
Supplementary Material
HIGHLIGHTS.
-
-
Little is known about synergistic effects of multiple risk factors on childhood asthma.
-
-
We first developed a risk score in a case-control study of Puerto Rican children, and then used this score to estimate the combined effect of multiple risk factors on asthma at school age in our Puerto Rican study and in a longitudinal birth cohort study of Swedish children (BAMSE).
-
-
We found that the presence of four or more risk factors is significantly associated with 16-times to 25-times increased odds of asthma at school age in Puerto Rican and Swedish children.
-
-
Our findings suggest that interventions or policies that concurrently address several modifiable risk factors (i.e. diet, obesity and second-hand smoke) may have a more beneficial effect on asthma prevention than single-factor interventions.
Capsule Summary.
The presence of four or more risk factors was significantly associated with 16-times to 25-times increased odds of asthma at school age in Puerto Rican and Swedish children.
Clinical Implications.
Interventions or policies that concurrently address several modifiable risk factors (i.e. diet, obesity and second-hand smoke) may be more likely to have a beneficial effect on asthma prevention than single-factor interventions.
Acknowledgments
Funding
This work was supported by grants HL079966, HL117191, and HL119952 from the U.S. National Institutes of Health (NIH), and by The Heinz Endowments. The BAMSE study was supported by the Swedish Research Council, FORMAS, the Swedish Heart-Lung Foundation, the Stockholm County Council (ALF), and the SFO (Strategic Research Area) Epidemiology Program at Karolinska Institutet. Dr. Forno’s contribution was supported by grant HL125666 from the U.S. NIH.
Abbreviations
- OR
odds ratio
- CI
confidence interval
- SHS
second-hand smoke
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Contributions
SS, OG, EM and JCC conceived of the study, and helped draft the manuscript. SS, OG, EF, and YYH performed statistical analysis. EAP, ACS, AB, IK, MA, and GC participated in the design and implementation of the study. All authors read and approved the final manuscript.
The authors declare no conflicts of interest.
References
- 1.Lai CK, Beasley R, Crane J, Foliaki S, Shah J, Weiland S, et al. Global variation in the prevalence and severity of asthma symptoms: phase three of the International Study of Asthma and Allergies in Childhood (ISAAC) Thorax. 2009;64:476–83. doi: 10.1136/thx.2008.106609. [DOI] [PubMed] [Google Scholar]
- 2.Akinbami LJ, Moorman JE, Bailey C, Zahran HS, King M, Johnson CA, et al. Trends in asthma prevalence, health care use, and mortality in the United States, 2001–2010. NCHS Data Brief. 2012;94:1–8. [PubMed] [Google Scholar]
- 3.Bjerg A, Sandstrom T, Lundback B, Ronmark E. Time trends in asthma and wheeze in Swedish children 1996–2006: prevalence and risk factors by sex. Allergy. 2010;65(1):48–55. doi: 10.1111/j.1398-9995.2009.02105.x. [DOI] [PubMed] [Google Scholar]
- 4.Castro-Rodriguez JA, Forno E, Rodriguez-Martinez CE, Celedon JC. Risk and protective factors for childhood asthma: what is the evidence? J Allergy Clin Immunol Pract. 2016;4:1111–1122. doi: 10.1016/j.jaip.2016.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Szentpetery SE, Forno E, Canino G, Celedon JC. Asthma in Puerto Ricans: Lessons from a high-risk population. J Allergy Clin Immunol. 2016;138(6):1556–8. doi: 10.1016/j.jaci.2016.08.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gref A, Kebede Merid S, Gruzieva O, Ballereau S, Becker A, Bellander T, et al. Genome-wide interaction analysis of air pollution exposure and childhood asthma with functional follow-up. Am J Respir Crit Care Med. 2017;195(10):1373–1383. doi: 10.1164/rccm.201605-1026OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brehm JM, Acosta-Perez E, Klei L, Roeder K, Barmada M, Boutaoui N, et al. Vitamin D insufficiency and severe asthma exacerbations in Puerto Rican children. Am J Respir Crit Care Med. 2012;186(2):140–6. doi: 10.1164/rccm.201203-0431OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martinez P, Richters JE. The NIMH community violence project: II. Children’s distress symptoms associated with violence exposure. Psychiatry. 1993;56(1):22–35. doi: 10.1080/00332747.1993.11024618. [DOI] [PubMed] [Google Scholar]
- 9.Selner-O’Hagan MB, Kindlon DJ, Buka SL, Raudenbush SW, Earls FJ. Assessing exposure to violence in urban youth. J Child Psychol Psychiatry. 1998;39(2):215–24. [PubMed] [Google Scholar]
- 10.Wickman M, Kull I, Pershagen G, Nordvall SL. The BAMSE project: presentation of a prospective longitudinal birth cohort study. Pediatr Allergy Immunol. 2002;13(Suppl 15):11–3. doi: 10.1034/j.1399-3038.13.s.15.10.x. [DOI] [PubMed] [Google Scholar]
- 11.Ballardini N, Bergstrom A, Wahlgren CF, van Hage M, Hallner E, Kull I, et al. IgE antibodies in relation to prevalence and multimorbidity of eczema, asthma, and rhinitis from birth to adolescence. Allergy. 2016 Mar;71(3):342–9. doi: 10.1111/all.12798. [DOI] [PubMed] [Google Scholar]
- 12.Household income for States: 2008 and 2009: US Census Bureau. [October 4, 2011]. Available from: http://www.census.gov/prod/2010pubs/acsbr09-2.pdf.
- 13.Akuete K, Oh SS, Thyne S, Rodriguez-Santana JR, Chapela R, Meade K, et al. Ethnic variability in persistent asthma after in utero tobacco exposure. Pediatrics. 2011;128(3):e623–30. doi: 10.1542/peds.2011-0640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jacobs TS, Forno E, Brehm JM, Acosta-Perez E, Han YY, Blatter J, et al. Underdiagnosis of allergic rhinitis in underserved children. J Allergy Clin Immunol. 2014;134(3):737–9 e6. doi: 10.1016/j.jaci.2014.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosser F, Forno E, Cooper PJ, Celedon JC. Asthma in Hispanics. An 8-Year Update. Am J Respir Crit Cae Med. 2014;189:1316–27. doi: 10.1164/rccm.201401-0186PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Han YY, Forno E, Brehm JM, Acosta Perez E, Alvarez M, Colon-Semidey A, et al. Diet, interleukin-17, and childhood asthma in Puerto Ricans. Annals Allergy Asthma Immunol. 2015;115:288–93. doi: 10.1016/j.anai.2015.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crouch J, Hanson R, Saunders B, Kilpatrick D, Resnick H. Income, race/ethnicity, and exposure to violence in youth: results from the national survey of adolescents. J Community Psychol. 2000;28:625–41. [Google Scholar]
- 18.Morgan WJ, Crain EF, Gruchalla RS, O’Connor GT, Kattan M, Evans R, 3rd, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004;351(11):1068–80. doi: 10.1056/NEJMoa032097. [DOI] [PubMed] [Google Scholar]
- 19.La Rosa PS, Warner BB, Zhou Y, Weinstock GM, Sodergren E, Hall-Moore CM, et al. Patterned progression of bacterial populations in the premature infant gut. Proc Natl Acad Sci U S A. 2014;111(34):12522–7. doi: 10.1073/pnas.1409497111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nurmatov U, Devereux G, Sheikh A. Nutrients and foods for the primary prevention of asthma and allergy: systematic review and meta-analysis. J Allergy Clin Immunol. 2011;127(3):724–33. e1–30. doi: 10.1016/j.jaci.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 21.Gref A, Rautiainen S, Gruzieva O, Håkansson N, Kull I, Pershagen G, Wickman M, Wolk A, Melén E, Bergström A. Dietary total antioxidant capacity in early school age and subsequent allergic disease. Clin Exp Allergy. 2017;47(6):751–759. doi: 10.1111/cea.12911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bisgaard H, Stokholm J, Chawes BL, Vissing NH, Bjarnadottir E, Schoos AM, Wolsk HM, Pedersen TM, Vinding RK, Thorsteinsdottir S, Folsgaard NV, Fink NR, Thorsen J, Pedersen AG, Waage J, Rasmussen MA, Stark KD, Olsen SF, Bonnelykke K. Fish oil-derived fatty acids in pregnancy and wheeze and asthma in offspring. N Eng J Med. 2016;375:2530–2539. doi: 10.1056/NEJMoa1503734. [DOI] [PubMed] [Google Scholar]
- 23.McEvoy CT, Schilling D, Clay N, Jackson K, Go MD, Spitale P, Bunten C, Leiva M, Gonzales D, Hollister-Smith J, Durand M, Frei B, Buist AS, Peters D, Morris CD, Spindel ER. Vitamin C supplementation for pregnant smoking women and pulmonary function in their newborn infants: a randomized clinical trial. JAMA. 2014;311:2074–2082. doi: 10.1001/jama.2014.5217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Litonjua AA, Carey VJ, Laranjo N, Harshfield BJ, McElrath TF, O’Connor GT, Sandel M, Iverson RE, Jr, Lee-Paritz A, Strunk RC, Bacharier LB, Macones GA, Zeiger RS, Schatz M, Hollis BW, Hornsby E, Hawrylowicz C, Wu AC, Weiss ST. Effect of prenatal supplementation with vitamin D on asthma or recurrent wheezing in offspring by age 3 Years: The VDAART randomized clinical trial. JAMA. 2016;315:362–370. doi: 10.1001/jama.2015.18589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chawes BL, Bonnelykke K, Stokholm J, Vissing NH, Bjarnadottir E, Schoos AM, Wolsk HM, Pedersen TM, Vinding RK, Thorsteinsdottir S, Arianto L, Hallas HW, Heickendorff L, Brix S, Rasmussen MA, Bisgaard H. Effect of vitamin D3 supplementation during pregnancy on risk of persistent wheeze in the offspring: a randomized clinical trial. JAMA. 2016;315:353–361. doi: 10.1001/jama.2015.18318. [DOI] [PubMed] [Google Scholar]
- 26.Chen W, Boutaoui N, Brehm JM, Han YY, Schmitz C, Cressley A, et al. ADCYAP1R1 and asthma in Puerto Rican children. Am J Respir Crit Care Med. 2013 Mar 15;187(6):584–8. doi: 10.1164/rccm.201210-1789OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ramratnam S, Han Y, Rosas-Salazar C, Forno E, Brehm J, Rosser F, et al. Exposure to gun violence and asthma among children in Puerto Rico. Respir Med. 2015;109(8):975–81. doi: 10.1016/j.rmed.2015.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nazario S, Zaragoza R, Velazquez V, Ramos-Valencia G, Acantilado C, Rodriguez R, et al. Allergen sensitivity (mites, insects, and pets) in a Puerto Rican population. PR Health Sci J. 2012;31(1):24–8. [PubMed] [Google Scholar]
- 29.Pinart M, Benet M, Annesi-Maesano I, von Berg A, Berdel D, Carlsen KC, et al. Comorbidity of eczema, rhinitis, and asthma in IgE-sensitised and non-IgE-sensitised children in MeDALL: a population-based cohort study. Lancet Respir Med. 2014;2(2):131–40. doi: 10.1016/S2213-2600(13)70277-7. [DOI] [PubMed] [Google Scholar]
- 30.Vassy JL, Hivert MF, Porneala B, Dauriz M, Florez JC, Dupuis J, et al. Polygenic type 2 diabetes prediction at the limit of common variant detection. Diabetes. 2014;63(6):2172–82. doi: 10.2337/db13-1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Meigs JB, Shrader P, Sullivan LM, McAteer JB, Fox CS, Dupuis J, et al. Genotype score in addition to common risk factors for prediction of type 2 diabetes. N Engl J Med. 2008;359(21):2208–19. doi: 10.1056/NEJMoa0804742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Beasley R, Semprini A, Mitchell EA. Risk factors for asthma: is prevention possible? Lancet. 2015;386(9998):1075–85. doi: 10.1016/S0140-6736(15)00156-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


