Abstract
Approximately half of all people living with HIV in the US are age 50 and older. Existing research highlights the health challenges of these individuals, but little work has focused on gathering input about concerns in participating in HIV and aging research. Prior to designing a prospective cohort study on HIV and aging, we elicited feedback from potential participants on general attitudes toward participation in a prospective HIV cohort study, and perspectives on important research topics relevant to older adults living with HIV.
Three qualitative focus groups were formed.
Three focus groups (5–7 participants each; N = 18) were held with older adults living with HIV. All discussions were audiorecorded and transcribed. Transcripts were analyzed using content analysis.
Participants emphasized the importance of data confidentiality, shared concerns about study biases arising from sponsored research, and suggested that conflicts of interest should be independently assessed by “representative” boards made of community members. They urged researchers to be mindful of research “burnout,” because many people with HIV participate in multiple research studies. A number of priority research areas emerged, including the gap in provision of end-of-life services.
Many older adults with HIV are knowledgeable about the research process and offer valuable insights to researchers. Addressing participant concerns can facilitate inclusion and enhance HIV research success.
Keywords: aging and human immunodeficiency virus, community perspectives, community-engaged, research barriers
1. Introduction
The population of older adults with HIV (human immunodeficiency virus) is growing.[1] People 50 years of age and above made up 43% of all people with HIV in the US in 2014.[2] Many older adults with HIV face multiple health challenges, including chronic pain[3] and other HIV associated non-AIDS (acquired immune deficiency syndrome) conditions,[4] representing additional burdens to health. Because the HIV-positive population demographic of the is shifting, there is a need to better understand the phenomenon of aging with HIV. This includes research toward understanding the unique ways in which older adults living with HIV may experience challenges or cope with health burdens.[4] Physicians and community members in the Coachella Valley of Riverside County, CA are planning a prospective cohort study in response to this research need but first sought feedback from potential participants about the study design and research aims.
The value of the inclusion of participant voices in the development of research has been demonstrated in the HIV field. To develop health care measures for people living with HIV/AIDS, Davis-Michaud et al[5] conducted focus groups and found differences in quality preferences across gender and race/ethnicity. In one study of adults living with HIV,[6] researchers explored participants’ views on research incentives. Participants were mindful of the knowledge and power dynamic between researchers and participants and research as a transactional process in which each party received something for giving something. These examples highlight how participants and researchers may have different perspectives on research processes that enforce the importance of incorporating participant viewpoints into research development.
In the present article, we present the findings from focus groups aimed at eliciting participants’ general attitudes toward participation in a prospective HIV cohort study, and perspectives on important research topics relevant to older adults living with HIV.
2. Methods
Participants for this study were recruited through Positive Life, a monthly seminar series providing HIV treatment education to the Coachella Valley's community of HIV survivors. Participants had to be at least 55 years old and self-report as HIV positive. Focus groups were led by 2 facilitators using a structured interview guide and were conducted at the Desert AIDS Project (DAP), a medical and support services provider for people living with HIV/AIDS. A physician speaker was present at each discussion to address clinical concerns. We asked participants to share their thoughts about protection of health information, sources of funding for the project including industry relationships, participant burden, banking of biological samples, sharing of discouraging findings in regard to aging with HIV, and priority research areas.
Discussions were audio recorded and transcribed verbatim. Transcripts were analyzed using line-by-line coding in ATLAS.ti qualitative analysis software. After transcripts were coded, all codes were extracted and sorted into categories and themes and discussed by 2 investigators to ensure accurate reflection of the topics discussed in the focus groups.[7,8] This study was reviewed and approved by the University of California, Riverside Institutional Review Board.
3. Results
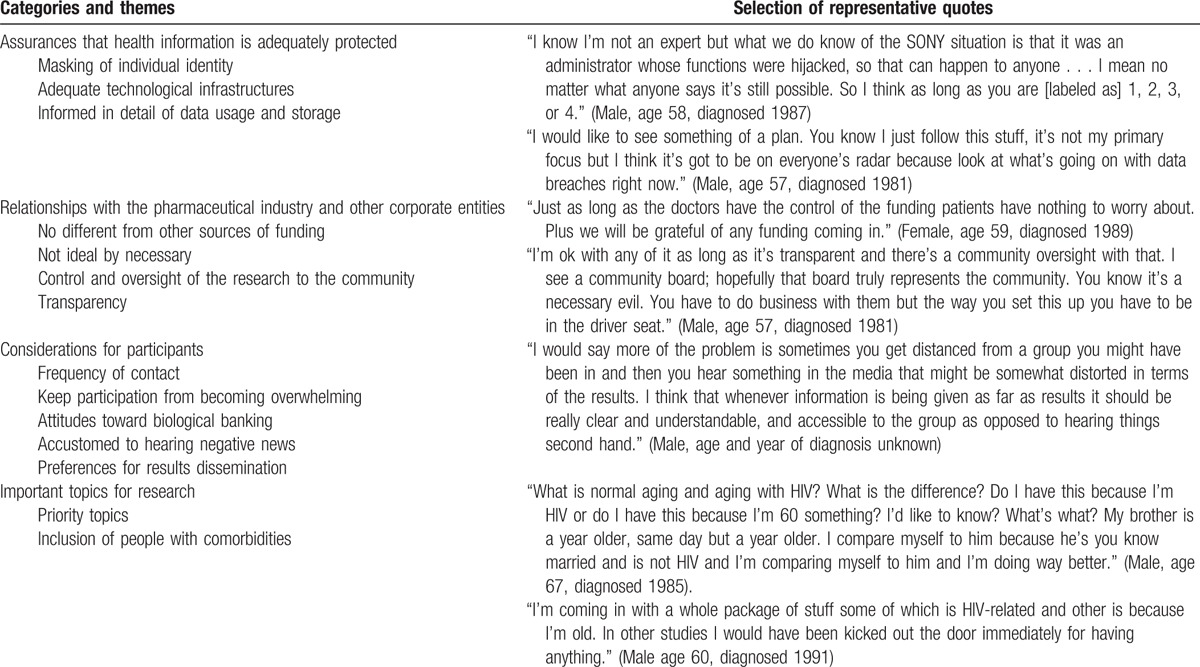
Eighteen participants were recruited over 3 months. Three focus groups were held with 5 to 7 people in each group with each lasting 90 minutes to 2 hours. Participants were between 56 and 69 years old (mean age 62 years), the majority (89%) identified as male, and time living with HIV ranged from 15 to 36 years (mean 26 years). Two participants did not report their age and 3 did not report their years living with HIV. Fourteen relevant themes emerged during the coding process, which were later merged under 4 different categories (Table 1).
Table 1.
List of categories, themes, and quotes extracted from focus group transcripts.
3.1. Category 1: Assurances that health information is adequately protected
All participants agreed that it was crucial for researchers to protect participants’ health information, particularly HIV status. Two participants recounted specific incidences where providers revealed their HIV status to third parties without their consent. One participant described the breach as occurring within a clinical care setting and the other described an incident within a nonclinical, social service setting. Steps that participants suggested for ensuring adequate protection of data included: masking identifiers through the use of identification numbers to label data, using adequate technology to prevent cyber hacking, and informing participants how their data would be used and stored. Two participants asserted that researchers should share with participants a detailed data security plan and technology protocol for data storage.
3.2. Category 2: Researcher relationships with corporate entities
Participants were asked their opinions on research funded by pharmaceutical and other corporate entities. Many participants made no distinction between pharmaceutical funding and other sources of funding, including philanthropic sources for research. Others were less enthusiastic about pharmaceutical and corporate funded research. One person (male, age 57) referred to research relationships with pharmaceutical companies as a “necessary evil.” The main hesitation regarding corporate funding sources was concern about research bias. Suggestions for ways to mitigate study bias were prompted and included: giving oversight of the research to the community by creating an advisory board that is “truly representative of the community…and in the driver's seat” (male, age 57), releasing study protocols for public review, and requiring disclosure of conflicts of interest from investigators.
3.3. Category 3: Considerations for participants
When asked about perceived burdens of participating in research, a robust discussion emerged about “participant burn-out” due to frequency or length of contact for data collection as well as participation in multiple research studies at a time. One participant suggested that any frequency of contact with participants for research purposes would be fine as long as it “got the job done” (male, age 67). However, most participants were concerned about being overwhelmed with too much contact and suggested limiting contact frequency. They urged researchers to use electronic data collection whenever possible and to periodically “check in with each participant” to ensure they are not feeling overwhelmed. One participant (male, age 66) recalled a particularly taxing experience with a research study and described how he felt after participating in an 8 hour, 1500 question survey session:
“I found it all intriguing but I went to dinner with [name] and I just started sobbing for a variety of reasons. But my mind, I felt like I was seizing. I felt like there was smoke coming out of my ears”
When asked about banking blood or other biological samples, all participants found it to be an acceptable part of research and many had experience donating biological samples. Some participants stated they would opt in to biobanking as long as it was voluntary and samples were securely stored. Because negative findings are always a possibility in research, participants were asked how they might feel about receiving discouraging information (eg, if the study discovered that older adults with HIV were at increased risk for death or certain diseases). Participants stated they were accustomed to hearing negative news because there was always “bad news about aging and HIV” but agreed that it was more important for investigators to be transparent and honest with the results. When asked about preferences for results dissemination, face-to-face dissemination (eg, through town halls) was preferred.
3.4. Category 4: Important topics for research
Specific topics that participants wanted to see in research related to aging with HIV included: differences between normal aging and aging with HIV, mental health issues, neurological symptoms, quality of life, HIV-related comorbidities, efficacy of alternative and complementary medicine, lifestyle behaviors, and access to end-of-life services. Some participants noted that adults living with HIV experience the same health and social challenges as the general elderly population but do not meet the age criteria to qualify for senior services (ie, 65 years old). At the same time, one participant suggested that HIV/AIDS-related services are not comprehensive enough to address the needs of older people:
“There are a lot of people that will help in recovery but outside of that, when someone comes to the end of their life and they have no family and they have nobody else, it's quite often that they are just dropped completely. There should be something that will address that.” (Male, age 65)
Many people stated that they were frustrated by the number of HIV-related research studies that excluded people with comorbidities, because many people living with HIV experience comorbidities such as depression, chronic illnesses, and neurological diseases.
4. Discussion
The findings from this study provide useful considerations for research focused on HIV and aging and for research in general. People with HIV may be accustomed to participating in research and some individuals may look to study compensation as a regular source of income.[6] This population may therefore be particularly savvy about issues of confidentiality, protection of data, and participant burden and respect. Participants offered practical suggestions to mitigate concerns about study biases and promote transparency, including giving study oversight to participant members. This is akin to the community advisory board (CAB) model widely used in community-based participatory research (CBPR), as a strategy to diffuse power dynamics between researchers and the community and ensure representation of community voices.[9] CABs have been successfully proposed and used to influence research processes from improvement of informed consent[10] to social change via decades-long partnerships between researchers and community groups.[11]
Longitudinal cohort studies focused on HIV, including the Multicenter AIDS Cohort Study (MACS)[12] and the Women's Interagency HIV study (WIHS)[13] do not primarily focus on issues related to aging with HIV. The participants in our study identified priority topics for HIV and aging research, including the need to evaluate provisioning of end-of-life services. It is particularly salient that participants described a perceived gap in which adults with HIV may be at an age where they do not qualify for senior services but are also unable to access needed services from traditional AIDS service organizations. Whether this perceived gap is due to an actual dearth of services or misinformation is an important area for future research. One study found that, among patients with HIV in an urban medical center, the use of hospice and palliative care was low despite availability.[14]
Limitations of this study include the small sample size and geographical area of recruitment, which inhibit the generalizability of findings to populations outside of the sample. Apart from age, gender, and time living with HIV, we were unable to collect demographic data that could have impacted interview responses, such as race/ethnicity, income, and experience with research. However, the concerns and priority research areas addressed by the participants in this study, members of the HIV and aging community, have useful and broad application to HIV-related aging research.
5. Conclusion
Following the suggestions given by the participants, we plan to follow CBPR strategies to create a shared governance structure to emphasize power sharing across all research activities, intended to increase the capacity of community partners and enhance patient participation. While HIV/AIDS research has a long history of fostering relationships among community representatives, community-based organizations, and researchers for HIV prevention,[15] less work has been done to intervene and develop effective approaches to ensure healthy aging with HIV. This is an important area of research with real and significant implications for the daily lives of individuals living with HIV.
Acknowledgments
Thanks to the study participants for sharing their perspectives on research. Thanks to Jo Gerrard for assistance with copyediting and to Jonathan Goldman for assistance with the project.
Footnotes
Abbreviations: AIDS = acquired immune deficiency syndrome, CAB = community advisory board, CBPR = community-based participatory research, DAP = Desert AIDS Project, HIV = human immunodeficiency virus, MACS = Multicenter AIDS Cohort Study, WIHS = Women's Interagency HIV Study.
RL conceived and supervised the study. AN completed the data analysis and led the writing with BB. JT and ME assisted with the study. All authors contributed to writing the paper.
AN and BB received support from the University of California, Los Angeles (UCLA) and Charles Drew University (CDU), Resource Centers for Minority Aging Research Center for Health Improvement of Minority Elderly (RCMAR/CHIME) under NIH/NIA Grant P30-AG021684, and from the UCLA Clinical and Translational Science Institute (CTSI) under NIH/NCATS Grant Number UL1TR001881. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. BB also received support from NIH 3R01AI114617–03S1.
The authors have no conflicts of interest to disclose.
References
- [1].Samji H, Cescon A, Hogg RS, et al. Closing the gap: increases in life expectancy among treated HIV-positive individuals in the United States and Canada. PloS One 2013;8:e81355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].CDC. Diagnoses of HIV infection among adults aged 50 years and older in the United States and dependent areas, 2010-2014; 2016. [Google Scholar]
- [3].Balderson BH, Grothaus L, Harrison RG, et al. Chronic illness burden and quality of life in an aging HIV population. AIDS Care 2013;25:451–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].High KP, Brennan-Ing M, Clifford DB, et al. HIV and aging: state of knowledge and areas of critical need for research. A report to the NIH Office of AIDS Research by the HIV and Aging Working Group. J Acquir Immune Defic Syndr 2012;60(suppl 1):S1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Davis-Michaud M, Yurk R, Lansky D, et al. Quality care for people with HIV/AIDS: patients’ perspectives. HIV Clin Trials 2004;5:406–15. [DOI] [PubMed] [Google Scholar]
- [6].Collins AB, Strike C, Guta A, et al. “We’re giving you something so we get something in return”: Perspectives on research participation and compensation among people living with HIV who use drugs. Int J Drug Policy 2017;39:92–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277–88. [DOI] [PubMed] [Google Scholar]
- [8].Patton MQ. Qualitative Research and Evaluation Methods. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- [9].Newman SD, Andrews JO, Magwood GS, et al. Community advisory boards in community-based participatory research: a synthesis of best processes. Prev Chronic Dis 2011;8:A70. [PMC free article] [PubMed] [Google Scholar]
- [10].Strauss RP, Sengupta S, Quinn SC, et al. The role of community advisory boards: involving communities in the informed consent process. Am J Public Health 2001;91:1938–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Silvestre AJ, Quinn SJ, Rinaldo CR. A twenty-two-year-old community advisory board: health research as an opportunity for social change. J Community Pract 2010;18:58–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Kaslow RA, Ostrow DG, Detels R, et al. The Multicenter AIDS Cohort Study: rationale, organization, and selected characteristics of the participants. Am J Epidemiol 1987;126:310–8. [DOI] [PubMed] [Google Scholar]
- [13].Barkan SE, Melnick SL, Preston-Martin S, et al. The Women's Interagency HIV Study. WIHS Collaborative Study Group. Epidemiology 1998;9:117–25. [PubMed] [Google Scholar]
- [14].Rhodes RL, Nazir F, Lopez S, et al. Use and predictors of end-of-life care among HIV Patients in a safety net health system. J Pain Symptom Manage 2016;51:120–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Rhodes SD, Malow RM, Jolly C. Community-based participatory research: a new and not-so-new approach to HIV/AIDS prevention, care, and treatment. AIDS Educ Prev 2010;22:173–83. [DOI] [PMC free article] [PubMed] [Google Scholar]


