Supplemental Digital Content is available in the text
Keywords: cardiovascular diseases, epidemiology, obesity, risk factors, underweight
Abstract
Obesity is a well-established risk factor for cardiovascular disease (CVD), but the underweight population of body mass index (BMI) below 18.5 kg/m2 has not been an object of concern. The objective of this study is to investigate whether underweight could be an independent risk factor for CVD in a population-based cross-sectional study.
Cross-sectional data of 2013 Behavioral Risk Factor Surveillance System (BRFSS) database encompassing 491,773 US adult subjects were used to assess risk for CVD. Primary outcomes were the incidence and relative risks (RRs) of CVD including stroke, heart attack/myocardial infarction, or coronary artery disease according to BMI category. All analyses used weighted sampling probabilities of data source.
The underweight population had a 19.7% greater risk of CVD than did the normal-weight, and the overweight and obese population had a 50% and 96% increased risk, respectively. When adjusted with covariates, the relative risk for CVD elevated in underweight population (adjusted RR 1.34 [95% confidence interval (CI) 1.335–1.348]). Conversely, the adjusted relative risk was significantly attenuated in the obese group (adjusted RR 1.149 [95% CI 1.147–1.151]) and it was even insignificant in the overweight group (adjusted RR 1.00 [95% CI 1.000–1.003]). In subanalysis for each CVD category, being underweight among BMI status was the strongest independent risk factor for stroke (adjusted RR 1.441 [95% CI 1.431–1.450]), heart attack/ myocardial infarction (MI) (adjusted RR 1.23 [95% CI 1.217–1.233]), and angina/coronary artery disease (adjusted RR 1.20 [95% CI 1.189–1.206]). Especially among the population below 40-year old, relative risk estimates remained increased in the underweight population; persons who were underweight had a 2.3-fold greater adjusted relative risk of CVD as compared with those with normal weight when we stratified with age.
Underweight below BMI 18.5 kg/m2 may be another risk factor for CVD, and CVD risk of the overweight and obese population largely depended on other comorbidities accompanied by obesity.
1. Introduction
As obesity has become a worldwide epidemic, a potential increase of obesity-related morbidity and mortality has been one of the major issues in the field of public medicine.[1,2] Obesity is widely accepted as an independent risk factor for cardiovascular disease (CVD) as well as other numerous comorbidities including hypertension, dyslipidemia, type 2 diabetes, and certain cancers.[3,4] In clinical studies and daily practice, the degree of obesity is usually expressed via body mass index (BMI), a measure obtained by dividing a person's weight by the square of the person's height.[5,6] There is a general consensus on the increasing incidence of CVD as the degree of BMI increases.[4] However, recent evidence of a U- or J-shaped relationship between mortality and BMI namely “obesity paradox” implies a higher mortality in the normal-weight rather than the overweight population and it poses a significant challenge to this obesity-disease paradigm.[7] In this context, the increased mortality of the underweight population becomes an emerging issue as well.[8,9]
Most researchers have been regarding that being underweight is not a risk of CVD itself, and it might result from the lower incidence of CVD-related risk factors such as hypertension, dyslipidemia, and insulin resistance in the underweight population.[10] In addition, evidences from large cohort studies investigating CVD risk factors have not indicated being underweight as a risk for CVD.[11–19] The low proportion of the underweight to the entire population, an average of 1% to 4% in developed countries, may lead to the underweight group to be frequently regarded as a category of normal-weight population in most studies, which made it hard to find a clinical implication of being underweight.[11–16] Even if treated as an independent group, the low proportion of underweight subjects resulted in large variability and conflict results among studies in previous studies.[17,18,20] The objective of this study is to investigate whether underweight could be an independent risk factor for CVD in a population-based cross-sectional study.
2. Methods
2.1. Study design and data source
We conducted a cross-sectional study using data from the 2013 Behavioral Risk Factor Surveillance System (BRFSS) of Centers for Disease Control and Prevention (CDC) (http://www.cdc.gov/brfss/annual_data/annual_data.htm). The BRFSS is a US nationwide annually-conducted randomized telephone-based surveillance system designed to measure behavioral risk factors for the adult population over the age of 18.[19] The 2013 BRFSS database encompassed a total of 491,773 questionnaires among which BMI data were available in 465,052 subjects. Ethical approval was not necessary owing to the nature of the data (secondary data analysis of anonymized files).
2.2. Definition of variables
The person with a history of CVD was defined as if he answered yes to any of questions about three categories of CVD such as a heart attack including myocardial infarction (MI), angina, or coronary artery disease (CAD), and stroke; (Ever told) you had a heart attack, also called a MI, (Ever told) you had angina or CAD, and (Ever told) you had a stroke. When he/she answered “Donot know/Not sure” or refused to answer, it was regarded as a missing value. The main independent variable, BMI was defined according to WHO classification; BMI of less than 18.5 kg/m2 is considered underweight, between 18.5 and 24.9 corresponds to a healthy weight, between 25.0 and 29.9 is overweight, and above 30 is obese.[6]
In addition to major variable, we included covariates defined as major risk factors for CVD by the American Heart Association (AHA), including advanced age, diabetes mellitus, hypertension, hypercholesterolemia, cigarette smoking, and physical inactivity.[4] Age was categorized into 5-year groups with 14 levels from age 18 to 24 to age 80 or older. The subject with hypertension was defined as one who reported yes to following survey question; “Have you EVER been told by a doctor, nurse, or other health professional that you have high blood pressure.” Hypercholesterolemia was defined if respondents who have had their cholesterol checked have been told by a doctor, nurse, or other health professional that it was high. The diabetes mellitus was defined as a positive history of diagnosis of diabetes mellitus and pre- or borderline glucose status. Women once diagnosed with maternal diabetes but who now maintained a normal glucose level were excluded. Smoking status was defined as current, former, and never-smoker; never-smoked was defined as having smoked fewer than 100 cigarettes in the subject's lifetime. Former smokers included individuals who had smoked more than 100 cigarettes over the subject's lifetime but who had quit smoking any time prior to survey enrollment. Current smoker was the subject now smoking cigarettes some or every day, totaling more than 100 cigarettes over the subject's lifetime. Finally, respondents with physical activity were classified as meeting both the aerobic and muscle-strengthening guidelines.[21]
2.3. Statistical analysis
All analyses took into account the complex survey design and weighted sampling probabilities of the data source. We used the final weight variable in 2013BRFSS dataset (the code name of _LLCPWT) which is ranking weighted to 8 demographic dimensions including age group by gender, detailed race/ethnicity, educational level, marital status, home owner or renter status, gender by race/ethnicity, age group by race/ethnicity, and telephone source (landline telephone only, both landline and cell phone, or cell phone only).[22] Relative risks (RRs) and 95% confidence intervals (95% CIs) for CVD according to categorized BMI were assessed with unadjusted and covariate-adjusted analysis using binary logistic regression model. In multivariate-adjusted analysis, we stratified our analyses by the important CVD risk terms of age, sex, presence of diabetes, hypercholesterolemia, and hypertension, smoking status (current smoker, former-smoker, and never-smoked), and physical inactivity.[4] The incidence of cardiovascular diseases with normal BMI (from 18.5 to 24.99) was specified as the reference level, and RRs of the other groups were calculated by comparing to normal BMI group. In case of smoking status, the incidence of never-smoked population was treated as a reference level. All analyses were performed using Statistical Package for the Social Sciences version 18.0 (SPSS Inc, Chicago, IL).
3. Results
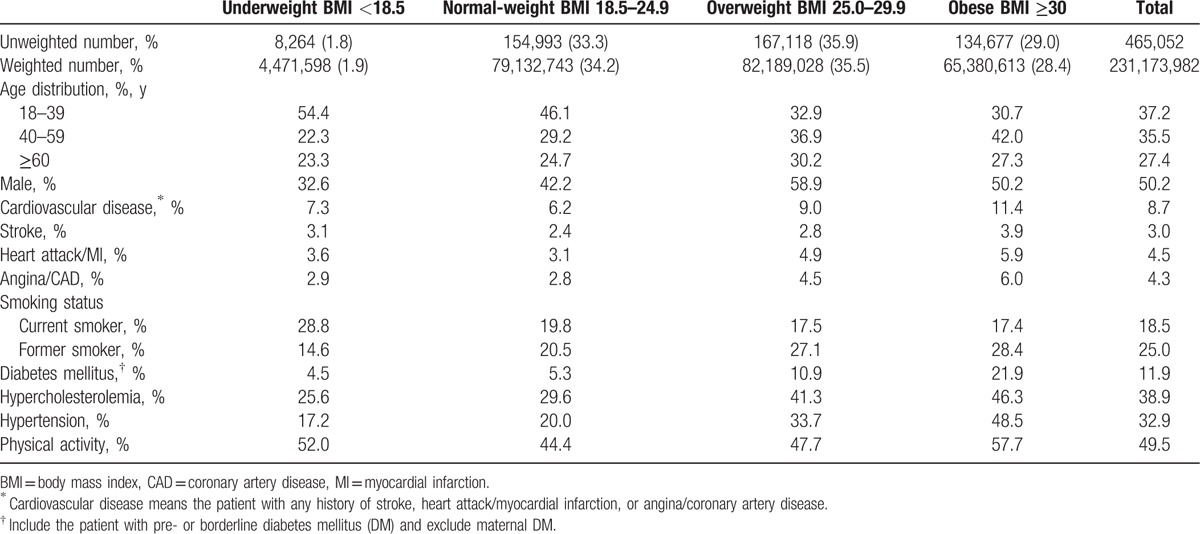
The study population (n = 465,052) whose BMI result was available was representative of more than 231 million US adults over the age of 18. Of these, 28.4% were obese, 63.9% were either overweight or obese, and just 1.9% were underweight. The weighted proportion of males was 50.2%, and 27.4% of the subjects were over 60 years old. The weighted incidence of CVD was 8.7%, which was comprised of stroke, 3.0%, heart attack/MI, 4.5%, and angina/ CAD, 4.3%. The rate of current cigarette smokers and former-smokers was 18.5% and 25.0%, respectively. The weighted incidence of diabetes including pre- and borderline diabetes mellitus was 11.9%, hypercholesterolemia 38.9%, and hypertension 32.9%. Underweight population was common in female and the younger age group below 40-year old and they had a lower incidence of the major CVD risk factors such as hypertension, dyslipidemia, and diabetes mellitus compared with other BMI groups (Table 1).
Table 1.
Demographic and clinical characteristics of 2013 behavioral risk factor surveillance data by Centers for Disease Control and Prevention (CDC).
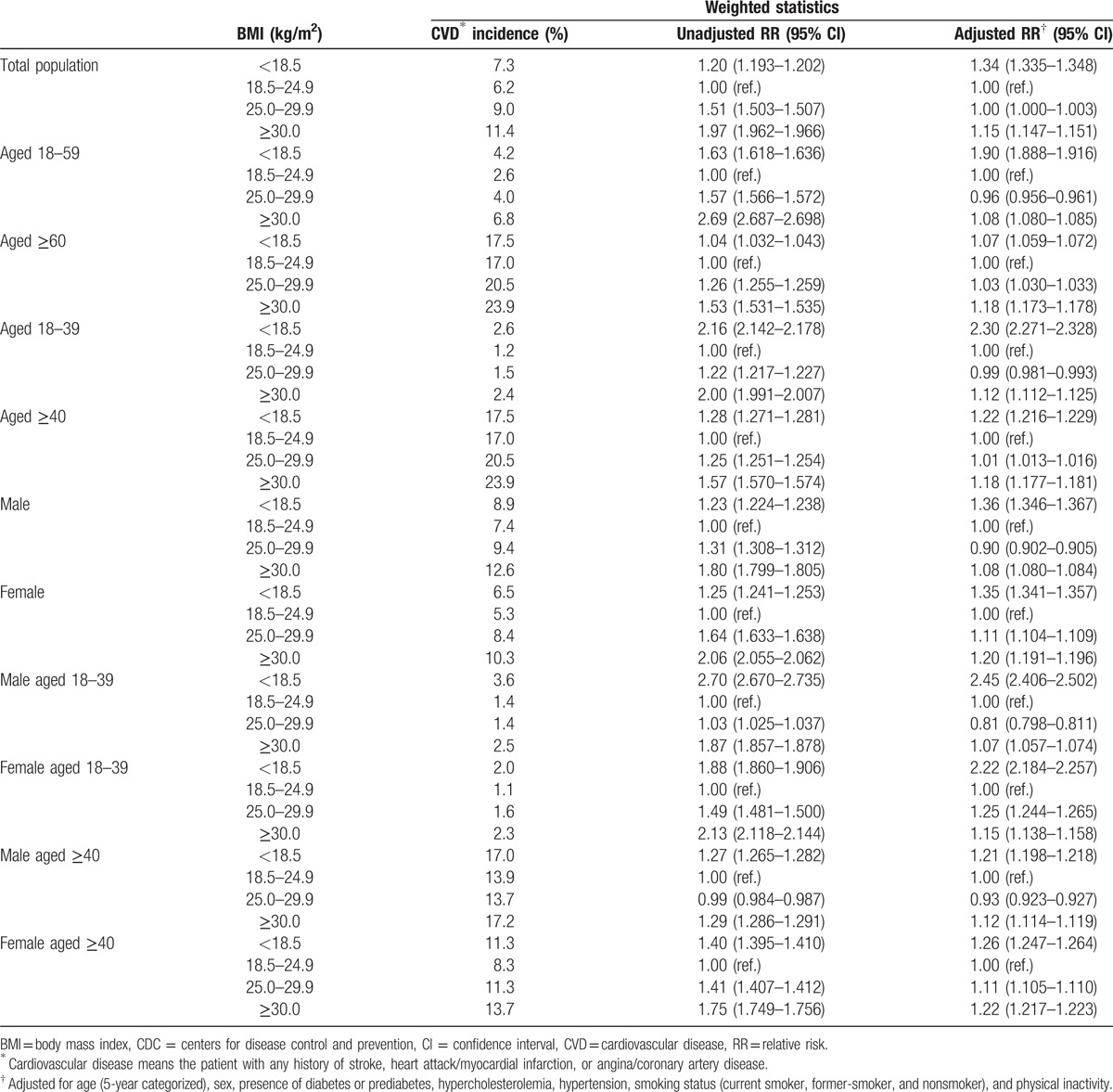
When we assessed the effect of BMI on CVD, the underweight population with BMI below 18.5 kg/m2 had a higher incidence of CVD (7.3%) than normal weight group (6.2%); compared with the normal weight group, being underweight was associated with a 1.20-fold increased risk of CVD, as was being overweight (1.51-fold) and obese (1.96-fold). When the estimates were adjusted with well-known risk factors for CVD, such as age, sex, hypertension, hypercholesterolemia, diabetes, smoking status, and physical inactivity, the relative risk increased for underweight population (adjusted RR 1.34 [95% CI 1.335–1.348]). However, adjustment with covariates made the overweight group lose its statistical significance (adjusted RR 1.00 [95% CI 1.000–1.003]) and it attenuated the relative risk of obese group for total CVD (adjusted RR 1.15 [95% CI 1.147–1.151]), suggesting the elevated risk of overweight and obese group was to a large extent driven by obesity-related comorbidities. When we stratified with age, relative risk estimates remained increased in the underweight population; especially among the population below 60-year old, persons who were underweight had a 1.9-fold greater adjusted relative risk of CVD as compared with those with normal weight. Although underweight population was common in female (Table 1), the stratification with sex revealed a similar risk of CVD between male and female group of underweight population (Table 2, Supplementary Table 1–5). Among the population below 40-year old, moreover, persons who were underweight had a 2.30-fold greater adjusted relative risk of CVD as compared with those with normal weight (Table 2). The stratification with sex revealed a similar risk of CVD between male and female group of underweight population below 40-year old (Table 2).
Table 2.
Age- and sex-specific relative risk for the cardiovascular disease (CVD) according to body mass index (BMI) in CDC behavioral risk factor surveillance data 2013.
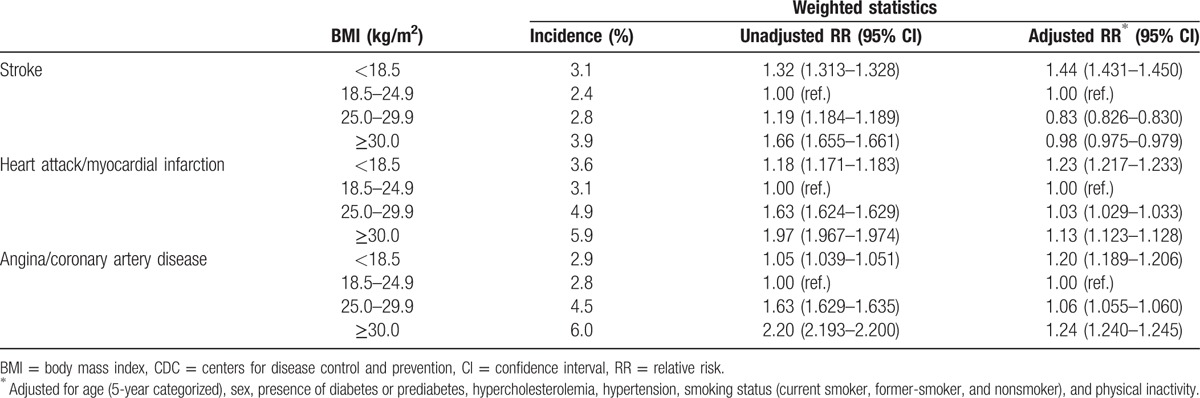
We then investigated whether the underweight had a different impact on individual CVD categories of stroke, heart attack/MI, and angina/CAD. Among these categories, the impact of underweight was most profound in stroke; the relative risk estimate of underweight population was 1.32-fold higher than that of controls. When adjusted with multiple compound factors, the stroke risk increased only in the underweight group (adjusted RR 1.44 [95% CI 1.431–1.450]). The risk of heart attack/MI was 1.18-fold higher in the underweight group than in the normal weight control, which remained statistically significant after adjustment with CVD-related covariates (adjusted RR 1.23 [95% CI 1.217–1.233]). Although the degree of relative risk was lower than stroke and heart attack/MI, there was a significant association between being underweight and risk of angina/CAD; underweight population had a 4.5% higher risk of angina/CAD than normal weight controls, which was accentuated by covariate-adjustment (adjusted RR 1.20 [95% CI 1.189–1.206]). Although overweight and obese populations had a higher risk than underweights in stroke, heart attack/MI and angina/CAD under univariate analyses, their statistical significance was significantly attenuated in heart attack/MI and angina/CAD and revealed to be even protective in stroke after covariant adjustment (Table 3, Supplementary Table 6–8).
Table 3.
Individual cardiovascular disease-specific relative risk according to body mass index in CDC behavioral risk factor surveillance data 2013.
Based on these results, we analyzed a distribution of relative risks for total CVD and each CVD entity per unit of BMI. The age- and sex- adjusted relative risk of total CVD and individual diseases was lowest in the BMI range between 21.0 and 21.9 kg/m2, which served as a control group. Overall distribution of relative risks for CVD showed U-shaped pattern according to BMI. The relative risks for CVD were more than 1.5-fold in the subjects with BMI below 17 kg/m2 and above 30 kg/m2 compared with controls, as was stroke, and heart attack/MI (Fig. 1).
Figure 1.
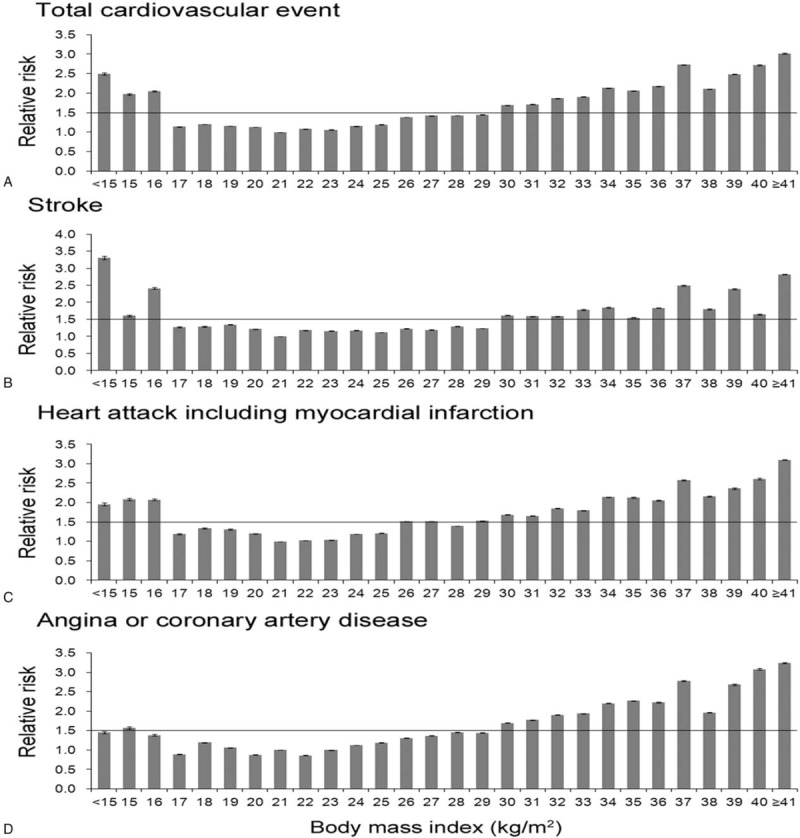
Relative risk of total and individual cardiovascular disease per unit of BMI. The risk of BMI between 21.0 and 21.9 kg/m2 was used as reference level and relative risks were obtained from binary logistic regression model adjusted with age and sex. Error bars represent the 95% confidence intervals of the relative risks. BMI = body mass index.
4. Discussion
In this cross-sectional study using database of BRFSS 2013, we found that underweight below 18.5 kg/m2 of BMI may be an independent risk factor for CVD with which BMI had a U-shaped curve relationship. This underweight effect on the association with CVD was more prominent in subjects under age 60. In a CVD subgroup analysis, the association was most significant for stroke compared with other CVD entities.
The major studies that serve as a stepping stone in concluding obesity as a major risk for CVD have not included the underweight subjects or merged them into normal-weight group in a statistical analysis.[11–15,23] To our knowledge, there have been few studies investigating the underweight population as an independent group in CVD risk assessment.[17,18,20] The prospective Finnish cross-sectional survey data revealed that underweight women have a significantly higher risk for stroke than do normal weight controls, but this risk was rather lower in underweight men.[17] Other data analyzed from the 20 years of follow-up in the Nurses’ Health Study (NHS) showed that the risk of coronary heart disease (CHD) in underweight group was similar to normal weight.[18] However, the underweight women in former-smoker sub-group had an 85% greater risk of CHD than normal-weight controls, but not in never-smoked and current smoker group.[18] These conflicting results even in the same study can be explained by the small number of disease cases in underweight population, such as a total of 17 stroke cases in Finnish data (15 in women and 2 cases in men) and 35 CHD cases of NHS data.[17,18] A large cohort surveillance study including 104,928 Japanese revealed that underweight subjects had an increased risk for stroke and CVD, showing a U-shaped association with BMI.[20] They used a control group with BMI between 23.0 to 24.9 kg/m2 that had the lowest risk for CVD among BMI subgroups, and it can accentuate the CVD risk of the underweight group and a U-shaped association of BMI with CVD.[20] Although the previous studies were frequently underpowered to detect a significant association between being underweight and CVD, the direction of the effect was largely consistent across studies.[17,18,20]
This unexpected result of the increased CVD risk in underweight group can be associated with various clinical factors, such as aging, sarcopenia, and poor nutritional status in underweight population. However, our data showed that the CVD risk of underweight was more prominent in the younger population below 40 years old. Considering previous studies that low body muscle mass may be a risk factor for CVD,[24,25] this may be due to the fact that the underweight of this population may have a relatively large decline in body muscle mass than the older population, because the body muscle mass tends to occupy a relatively large portion of body weight in the younger population.
In addition, a problem of poor nutritional status in underweight individuals can also be a possible explanation, because they tend to have a relative deficiency of vitamins and minerals compared with those in other BMI categories.[26] However, there is no clear evidence connecting between nutritional deficiency and CVD risks. On the other hand, this association can be explained by the so-called “reverse causality,” which refers to the fact that an individual's weight may be a reflection of their CVD. It is hard to discuss the causality with this cross-sectional data. However, the average BMI reduction after CAD was just about 0.5 kg/m2, which was more common in obesity group.[27] Another explanation can have to do with the presence of “metabolically obese underweight” population that is in the underweight range on BMI but has an increased proportion of visceral fat and metabolic abnormalities, including dyslipidemia or insulin resistance. Actually, a large Japanese cohort study reported that underweight is associated with risk of diabetes among older adults.[28] However, our results showed that the CVD risk of underweight group was maintained or rather increased after adjustment with well-known CVD risk factors, suggesting that underweight group has different types of risk mechanisms contributing to CVD. To our knowledge, there have been few studies targeted on the underweight population and further investigations are required to elucidate the pathophysiologic mechanisms of this paradoxical phenomenon.
Another important point of this study is that the overweight in and of itself did not increase the risk of CVD and being obese has only a small effect that increased about 15% of CVD risk in multivariate analysis. It is widely accepted that obesity can directly increase CVD risk through a variety of mechanisms including systemic inflammation, hypercoagulability, and activation of the sympathetic and renin-angiotensin systems.[29–33] However, there have been several evidences suggesting that the CVD risk associated with obesity is largely secondary to obesity-related comorbid conditions.[13,34–37] A recent study showed that three obesity-related risk factors of hypertension, hypercholesterolemia, and diabetes mellitus can explain about 50% of excess risk for CHD and 75% of the risk for stroke in high BMI group.[35] Among three risk factors, the effect of hypertension was most profound; hypertension alone mediated 31% of excess risk of CAD and about 60% of excess risk of stroke in obesity population.[35] Taken together, our results provide consistent evidence that the direct effects of obesity on CVD are relatively weak, and the effects are largely dependent on a variety of obesity-related comorbidities such as dyslipidemia, insulin resistance, and hypertension. In other aspects, our data suggest that being overweight or moderately obese without any comorbidity may not be deleterious in CVD, which raise a question whether an aggressive weight reduction for CVD risks is reasonable for an overweight person without comorbidity.
This study has several limitations. First, as a result of the cross-sectional design, the results only demonstrated an association between underweight and CVD and could not infer the causality between them. That means the association of underweight and CVD can be affected by other factors that also led to underweight. By analyzing the relative risk based on age, however, we showed that the relative risk of CVD in younger age groups was higher than that of the older age groups. That means that underwater may not be secondary due to CVD of older age group. To clarify the relationship between CVD and underweight, a long-term follow-up study will be necessary in the future. Second, telephone-based self-reporting method may lead to measurement error or misclassification, especially in BMI and comorbid conditions.[38] And the data of BRFSS does not capture family history of CVD that is an important and clear risk factor for CVD. Further studies are needed to clarify the causal association between underweight and CVD.
In conclusion, this study provides evidence that being underweight of BMI below 18.5 kg/m2 may be another risk factor for CVD, especially in the population below 40-year old. Among CVD categories, the underweight-associated risk was most profound in stroke and heart attack/MI, whereas that was relatively small in angina/CAD. On the other hand, the CVD risk of overweight and obese population was largely dependent on the obesity-related comorbid conditions.
Supplementary Material
Footnotes
Abbreviations: 95% CI = 95% confidence interval, AHA = American Heart Association, BMI = body mass index, BRFSS = behavioral risk factor surveillance system, CAD = coronary artery disease, CDC = centers for disease control and prevention, CHD = coronary heart disease, CVD = cardiovascular disease, MI = myocardial infarction, NHS = nurses’ health study, RR = relative risk.
This study was supported by a grant to SH from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute, which is funded by the Ministry of Health and Welfare, Republic of Korea (Grant Number: HI15C1780).
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and Future Planning (NRF-2017R1D1A1B03033127).
Obtaining data: Data from the 2013 Behavioral Risk Factor Surveillance System (BRFSS) of Centers for Disease Control and Prevention (CDC) (http://www.cdc.gov/brfss/annual_data/annual_data.htm).
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Flegal KM, Kit BK, Orpana H, et al. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA 2013;309:71–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Cepeda-Valery B, Pressman GS, Figueredo VM, et al. Impact of obesity on total and cardiovascular mortality—fat or fiction? Nat Rev Cardiol 2011;8:233–7. [DOI] [PubMed] [Google Scholar]
- [3].Malik VS, Willett WC, Hu FB. Global obesity: trends, risk factors and policy implications. Nat Rev Endocrinol 2013;9:13–27. [DOI] [PubMed] [Google Scholar]
- [4].Grundy SM, Pasternak R, Greenland P, et al. Assessment of cardiovascular risk by use of multiple-risk-factor assessment equations: a statement for healthcare professionals from the American Heart Association and the American College of Cardiology. Circulation 1999;100:1481–92. [DOI] [PubMed] [Google Scholar]
- [5].Lee CM, Huxley RR, Wildman RP, et al. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. J Clin Epidemiol 2008;61:646–53. [DOI] [PubMed] [Google Scholar]
- [6].WHO. Obesity: preventing and managing the global epidemic. Report of a WHO Consultation. WHO Technical Report Series 894. Geneva: World Health Organization; 2000. [PubMed] [Google Scholar]
- [7].Lavie CJ, De Schutter A, Milani RV. Healthy obese versus unhealthy lean: the obesity paradox. Nat Rev Endocrinol 2015;11:55–62. [DOI] [PubMed] [Google Scholar]
- [8].Roh L, Braun J, Chiolero A, et al. Mortality risk associated with underweight: a census-linked cohort of 31,578 individuals with up to 32 years of follow-up. BMC Public Health 2014;14:371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Kelly SJ, Lilley JM, Leonardi-Bee J. Associations of morbidity in the underweight. Eur J Clin Nutr 2010;64:475–82. [DOI] [PubMed] [Google Scholar]
- [10].Jonsson S, Hedblad B, Engstrom G, et al. Influence of obesity on cardiovascular risk. Twenty-three-year follow-up of 22,025 men from an urban Swedish population. Int J Obes Relat Metab Disord 2002;26:1046–53. [DOI] [PubMed] [Google Scholar]
- [11].Abbasi F, Brown BW, Jr, Lamendola C, et al. Relationship between obesity, insulin resistance, and coronary heart disease risk. J Am Coll Cardiol 2002;40:937–43. [DOI] [PubMed] [Google Scholar]
- [12].Arnlov J, Ingelsson E, Sundstrom J, et al. Impact of body mass index and the metabolic syndrome on the risk of cardiovascular disease and death in middle-aged men. Circulation 2010;121:230–6. [DOI] [PubMed] [Google Scholar]
- [13].Kurth T, Gaziano JM, Rexrode KM, et al. Prospective study of body mass index and risk of stroke in apparently healthy women. Circulation 2005;111:1992–8. [DOI] [PubMed] [Google Scholar]
- [14].Strazzullo P, D’Elia L, Cairella G, et al. Excess body weight and incidence of stroke: meta-analysis of prospective studies with 2 million participants. Stroke 2010;41:e418–26. [DOI] [PubMed] [Google Scholar]
- [15].Wolk R, Berger P, Lennon RJ, et al. Body mass index: a risk factor for unstable angina and myocardial infarction in patients with angiographically confirmed coronary artery disease. Circulation 2003;108:2206–11. [DOI] [PubMed] [Google Scholar]
- [16].Berrington de Gonzalez A, Hartge P, Cerhan JR, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med 2010;363:2211–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Cui R, Iso H, Toyoshima H, et al. Body mass index and mortality from cardiovascular disease among Japanese men and women: the JACC study. Stroke 2005;36:1377–82. [DOI] [PubMed] [Google Scholar]
- [18].Hu G, Tuomilehto J, Silventoinen K, et al. Body mass index, waist circumference, and waist-hip ratio on the risk of total and type-specific stroke. Arch Intern Med 2007;167:1420–7. [DOI] [PubMed] [Google Scholar]
- [19].Li TY, Rana JS, Manson JE, et al. Obesity as compared with physical activity in predicting risk of coronary heart disease in women. Circulation 2006;113:499–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].OECD/WHO. “Underweight and overweight”, in Health at a Glance: Asia/Pacific 2012, OECD Publishing. Available at: http://dx.doi.org/10.1787/9789264183902-20-en. Accessed November 1, 2015. [Google Scholar]
- [21].CDC. Behavioral risk factor surveillance system, overview: BRFSS 2013. Available at: http://www.cdc.gov/brfss/annual_data/2013/pdf/Overview_2013.pdf. Accessed March 1, 2015. [Google Scholar]
- [22].US Department of Health and Human Services. 2008 physical activity guidelines for Americans. Hyattsville, MD: US Department of Health and Human Services; 2008. Available at: http://www.health.gov/paguidelines. Accessed November 1, 2015. [Google Scholar]
- [23].CDC. Behavioral Risk Factor Surveillance System; Weighting the Data (2011 Weighting Formula). Available at: http://www.cdc.gov/brfss/annual_data/2011/2011_weighting.htm. Accessed November 21, 2014. [Google Scholar]
- [24].Mora S, Yanek LR, Moy TF, et al. Interaction of body mass index and framingham risk score in predicting incident coronary disease in families. Circulation 2005;111:1871–6. [DOI] [PubMed] [Google Scholar]
- [25].Sahin S, Eroglu M, Selcuk S, et al. Intrinsic factors rather than vitamin D deficiency are related to insulin resistance in lean women with polycystic ovary syndrome. Eur Rev Med Pharmacol Sci 2014;18:2851–6. [PubMed] [Google Scholar]
- [26].Lopez-Jimenez F, Wu CO, Tian X, et al. Weight change after myocardial infarction—the Enhancing Recovery in Coronary Heart Disease patients (ENRICHD) experience. Am Heart J 2008;155:478–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Sairenchi T, Iso H, Irie F, et al. Underweight as a predictor of diabetes in older adults: a large cohort study. Diabetes Care 2008;31:583–4. [DOI] [PubMed] [Google Scholar]
- [28].Samad F, Ruf W. Inflammation, obesity, and thrombosis. Blood 2013;122:3415–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Johnson AR, Milner JJ, Makowski L. The inflammation highway: metabolism accelerates inflammatory traffic in obesity. Immunol Rev 2012;249:218–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Rocha VZ, Libby P. Obesity, inflammation, and atherosclerosis. Nat Rev Cardiol 2009;6:399–409. [DOI] [PubMed] [Google Scholar]
- [31].Esler M, Straznicky N, Eikelis N, et al. Mechanisms of sympathetic activation in obesity-related hypertension. Hypertension 2006;48:787–96. [DOI] [PubMed] [Google Scholar]
- [32].Kalupahana NS, Moustaid-Moussa N. The renin-angiotensin system: a link between obesity, inflammation and insulin resistance. Obes Rev 2012;13:136–49. [DOI] [PubMed] [Google Scholar]
- [33].Canoy D, Boekholdt SM, Wareham N, et al. Body fat distribution and risk of coronary heart disease in men and women in the European Prospective Investigation Into Cancer and Nutrition in Norfolk cohort: a population-based prospective study. Circulation 2007;116:2933–43. [DOI] [PubMed] [Google Scholar]
- [34].Lu Y, Hajifathalian K, Ezzati M, et al. Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration (BMI Mediated Effects). Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1.8 million participants. Lancet 2014;383:970–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Wormser D, Kaptoge S, Di Angelantonio E, et al. Emerging Risk Factors Collaboration. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet 2011;377:1085–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Wilson PW, Bozeman SR, Burton TM, et al. Prediction of first events of coronary heart disease and stroke with consideration of adiposity. Circulation 2008;118:124–30. [DOI] [PubMed] [Google Scholar]
- [37].Pierannunzi C, Hu SS, Balluz L. A systematic review of publications assessing reliability and validity of the Behavioral Risk Factor Surveillance System (BRFSS), 2004–2011. BMC Med Res Methodol 2013;13:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Niedhammer I, Bugel I, Bonenfant S, et al. Validity of self-reported weight and height in the French GAZEL cohort. Int J Obes Relat Metab Disord 2000;24:1111–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


