Abstract
Rationale:
Hemivertebrae, which are the most frequent cause of congenital scoliosis, pose a challenge in terms of prognosis and therapy. The current gold standard treatment congenital scoliosis due to a lumbar and thoracic hemivertebra would be hemivertebra resection and short level posterior spinal fusion. Paucity literatures are reported for the treatment of hemivertebra by convex fusion with posterior hemivertebra excision.
Patient concerns:
The patient was first noticed to have a spinal problem at 7 years of age. A radiograph showed two full segment hemivertebra respectively at T10, between L4 and L5, with the spine deviating to the right side. No treatment was given, but he was followed with serial radiographs. At the 15 month follow up, a surgery was performed due to scoliosis progression, consisting of a unilateral instrumentation from L4 to L5 without hemivertebrectomy or epiphysiodesis. One year after surgery, the thoracic curve became larger and larger and hump started to progress as he grew.
Diagnoses:
Congenital scoliosis; Full segment hemivertebra at T10 and L4/5.
Interventions:
The full segment hemivertebra between L4 and L5 was excised and fusion in revision procedure. Transpedicular screws were inserted on the convex side in L4 and S1 and a rod was applied. A chart and radiological review were record at 8 years after final surgery.
Outcomes:
Eight years after the final surgery, the patient was completely pain-free, motion of the lumbar spine was preserved and the physiological curvatures were maintained. Good coronal and sagittal alignment of the spine was observed clinically and radiographically.
Lessons:
In summary, our case showed that unilateral instrumentation without hemivertebrectomy can result in an unacceptable deformity. However, the excellent outcome can be achieved when hemivertebra was excised. Although this is only a single case, the good result with a long follow-up suggests the technique is worthwhile for very young children with lumbosacral hemivertebra. Early recognition and resection combined with limited fusion were needed for these patients.
Keywords: congenital scoliosis, hemivertebra, pedicle screw fixation, revision surgery
1. Introduction
Congenital scoliosis is usually the result of failure of formation and/or segmentation. Hemivertebrae, which are the most frequent cause of congenital scoliosis, pose a challenge in terms of prognosis and therapy.[1] With the exception of some incarcerated types, hemivertebrae have growth potential and create a wedge-shaped deformity that progresses during further spinal growth. It is usually difficult to correct by conservative treatment such as back brace, cast, and halotraction, which often requires surgery for correction in most cases with curve progression.[2–4]
Determining the appropriate timing and type of surgery is important but difficult because natural evolution of a hemivertebra does not always lead to severe deformities and worsening of spinal deformities can occur during the pubertal growth spurt. The form of a curve is usually more severe than the local malformation. The probability of progression depends on the type of hemivertebra and whether a combination of developmental failure in formation and segmentation is present.[5] In previous study, it was reported by Repko insufficient correction of the deformity if fusion was performed without resection of the hemivertebra, resulteing in a correction of the scoliosis of just 22.1%. Compared with in situ bony fusion alone, the rate of correction was up to 61% after instrumented hemivertebra resection with simultaneous anterior and posterior fixation.[6] For these congenital deformities, the early diagnosis and treatment by resection and short-level fusion appear to result in better deformity correction than when correction is performed at a later age.[7–9] Furthermore, there is some suggestion that the use of a posterior approach alone results in a better long-term correction compared with a combined anterior/posterior approach.[6,10]
Posterior hemovertebral resection in pediatrics has been reported as the curative treatment of congenital scoliosis with successful results.[7,11] Herein, we report a case with long-term follow-up of revision surgery for lumbar hemivertebra following instrumented posterior spinal fusion in congenital scoliosis at a young age.
2. Ethics and consent
The study was approved by the Ethical Committee for The Second Hospital, Shanxi Medical University. Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editor of this journal.
3. Case report
This male patient was first noticed to have a spinal problem at 7 years of age. At that time, a radiograph showed 2 full-segment hemivertebra, respectively, at T10, between L4 and L5, with the spine deviating to the right side. No treatment was given, but he was followed with serial radiographs. At the 15-month follow-up visit, his spine became further and further deviated to the right; the lumbar curve had progressed 12 degrees (Figs. 1 and 2).
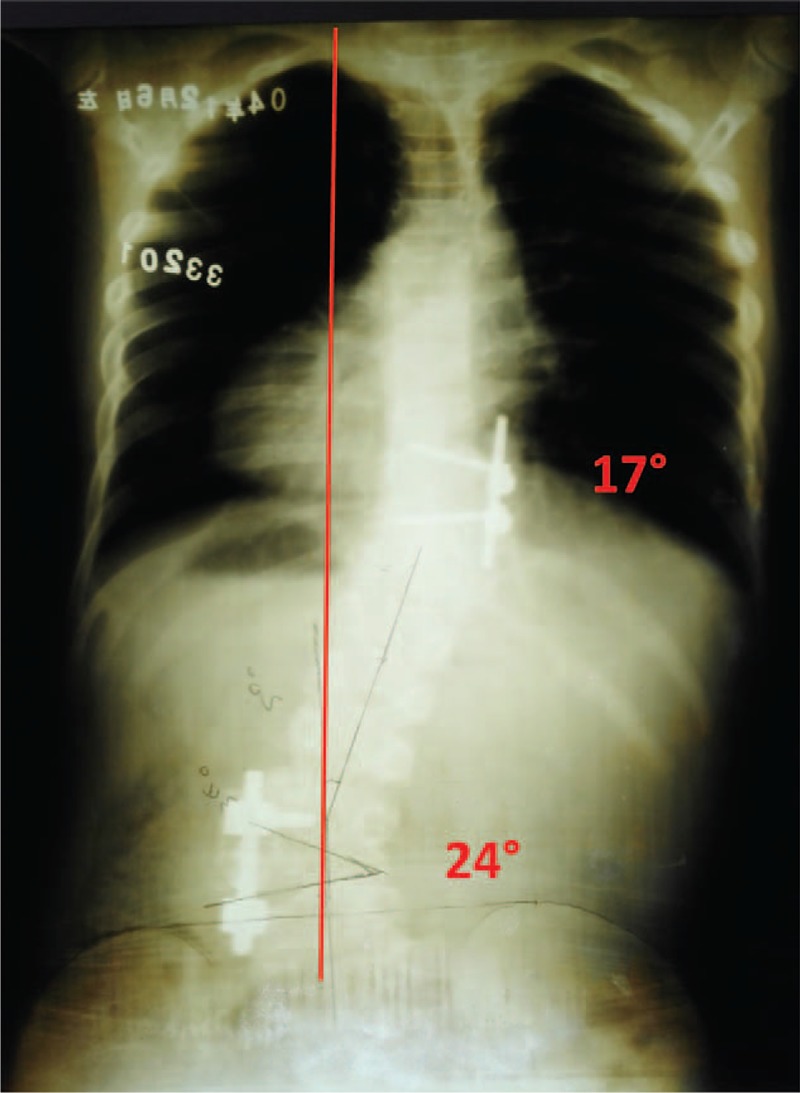
Figure 1.
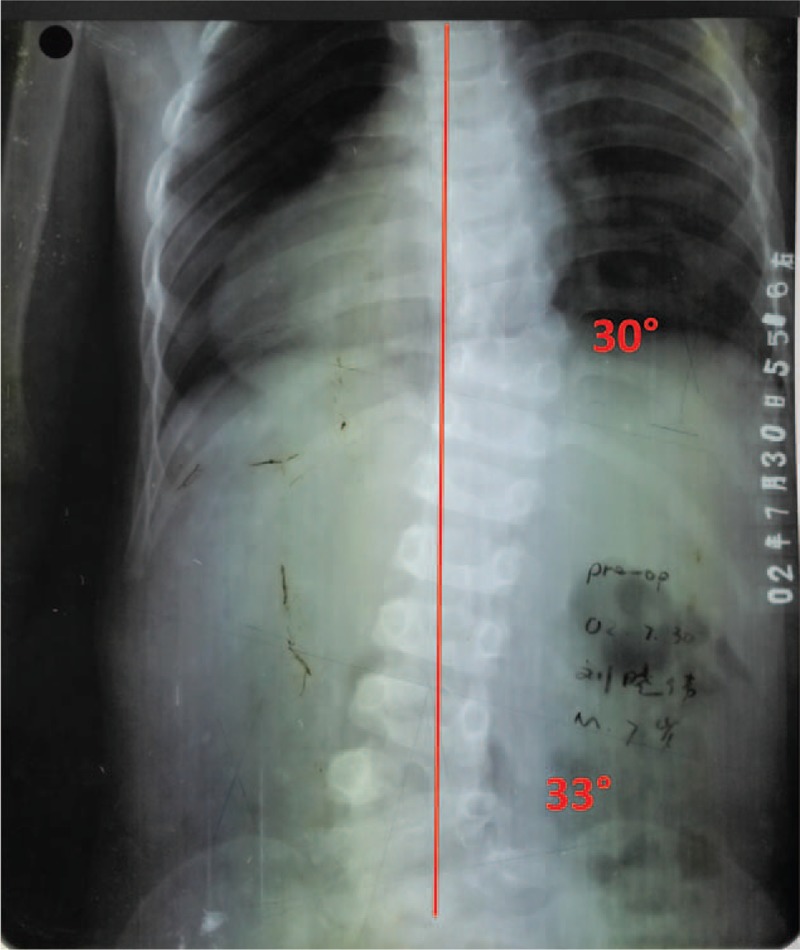
A supine radiograph when first seen at 7 years of age.
Figure 2.
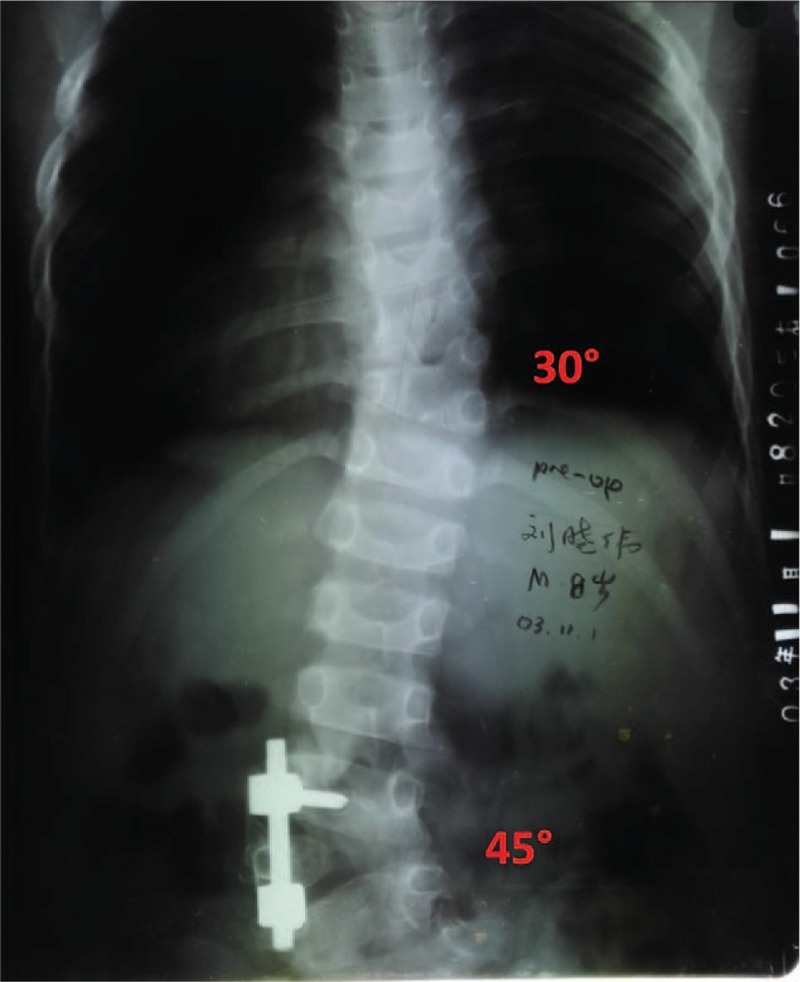
A standing radiograph first post-operation (posterior instrumentation at 8 years of age).
On clinical examination, the patient was noted to have right thoracic scoliosis and left lumbar scoliosis, but no complain of any subjective symptoms including pain. Thorough physical examination including investigation of foot or leg asymmetry, craniofacial malformation, and cardiac and urinary malformations was performed, with unremarkable findings.
In 2003, at 8 years of age, a surgery was performed, consisting of a unilateral instrumentation from L4 to L5 without hemivertebra resection or anterior and posterior epiphysiodesis. This was done in his local hospital. The preoperative degree of lumbar scoliosis (45 degree) was maintained after surgery (Fig. 2). The patient had no subjective symptoms and did well after surgery. However, 1 year after surgery, the thoracic curve became larger and larger and hump started to progress as he grew.
At the age of 9 years, he had right thoracic scoliosis of 36 degree (T9–11) to a T10 hemivertebra (Fig. 3). Because of the known progression of this vertebral anomaly, surgery was recommended. He was referred to the senior doctor in 2004 for further treatment. His only complaint was the deformity, which consisted of a prominent hump and shoulder asymmetry. On physical examination, he was neurologically normal, and his leg lengths were equal. Magnetic resonance imaging was available at that time.
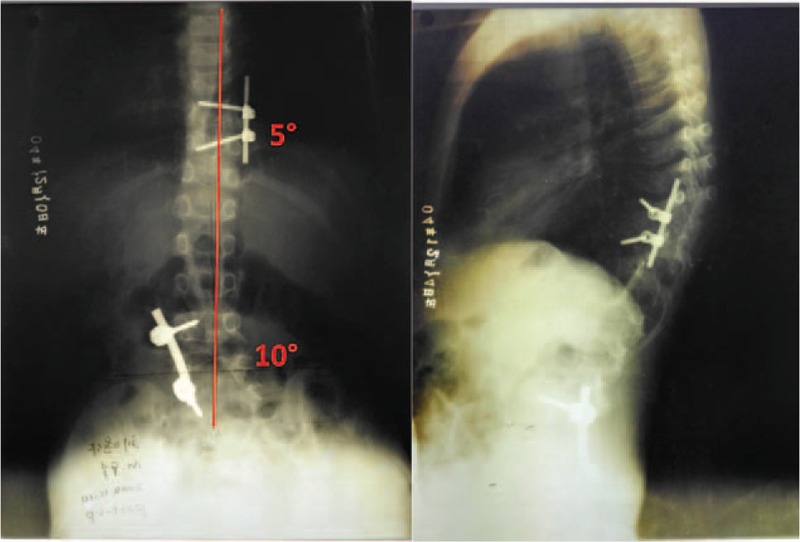
Figure 3.
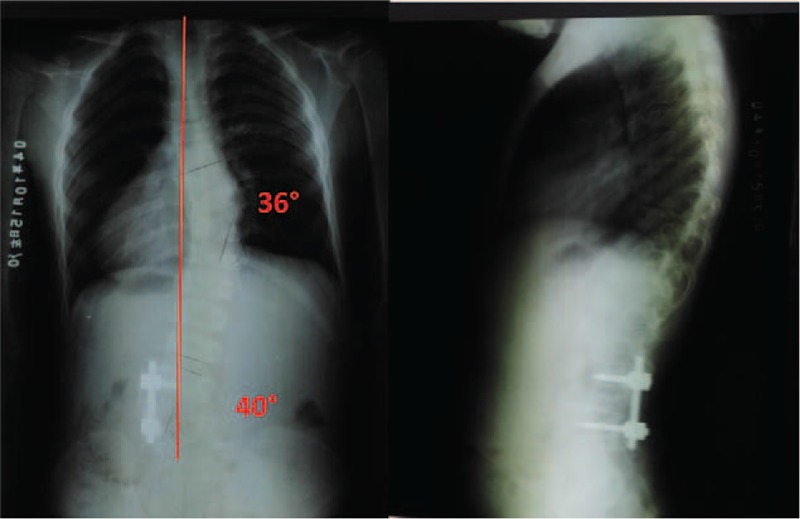
A standing radiograph at 1 year postoperation (at 9 years of age).
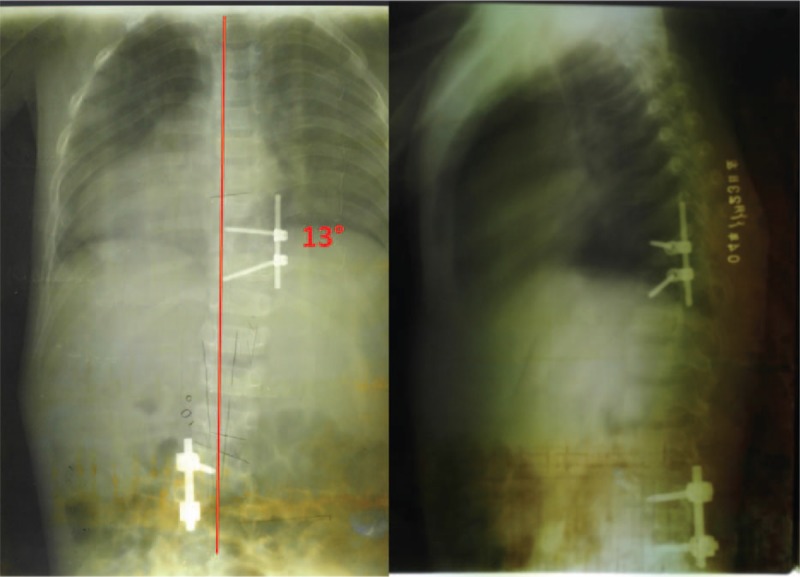
The surgical plan was to perform an anterior excision of the body of the hemivertebra of T10 with vertebral screw fixation from T9 to T11 (Fig. 4). Followed 2 weeks later, the preoperative degree of thoracic scoliosis (36 degree) was improved to 13 degree. But his spine became further and further deviated to the right. The trunk shift was 3 cm to the right (Fig. 5). Considering the severe tilted of the fourth lumbar vertebra owing to below hemivertebra, the revision surgery was performed by a posterior L4/5 hemivertebra excision, convex instrumentation, and intervertebral fusion from L4 to S1. Figure 6 shows the spine after the third surgery.
Figure 4.
A standing radiograph at the second post-operation (anterior T10 HV excision).
Figure 5.
A standing radiograph 2 weeks later at the second post-operation.
Figure 6.
A supine radiograph at the third post-operation (posterior L4/5 HV resection).
The second procedure went without difficulty, and there were no neurological or vascular complications. During the third procedure, the previous operative area was identified with an intraoperative radiograph. After removing the implants, convex pedicle screws were inserted into L4 and S1 vertebra using free hand technique because of the difficulty in L5 pedicle screw (Fig. 6). The hemivertebra was removed by posterior approach. Briefly speaking, the posterior parts of the pedicle were removed firstly. This was followed by excision of the inferior articular process of the hemivertebra and the superior articular process of the vertebra below. The spinal cord and the nerve roots were identified and protected. Epidural veins were cauterized by bipolar cautery to allow clear visualization. The remnants of the vertebral body of the hemivertebra and the adjacent disks were removed. The vertebral cartilage end plates of the convex side were cut down to the bone, and the contralateral end plate was retained. The concave side was not exposed as continued spinal growth on this side will improve the correction. At last, a precontoured rod was connected to the screws on the convex side. Gradual compression was applied until the gap was closed. Bones retrieved during osteotomy were used as graft material for fusion of the posterior elements. The blood loss was 350 mL, and there were no neurological complications. Neurological monitoring was not available at that time.
After surgery, he was fitted with a rigid brace to protect the instrumentation for 6 months. The fusion looked so solid that no further brace was felt necessary. Further follow-up was done by her referring orthopedist. At a 44-months and 60-month follow-up, the fusion was solid; he had no symptoms (Fig. 7). The last available radiograph was obtained in December 2012, which was 96 months after the third procedure (Fig. 8).
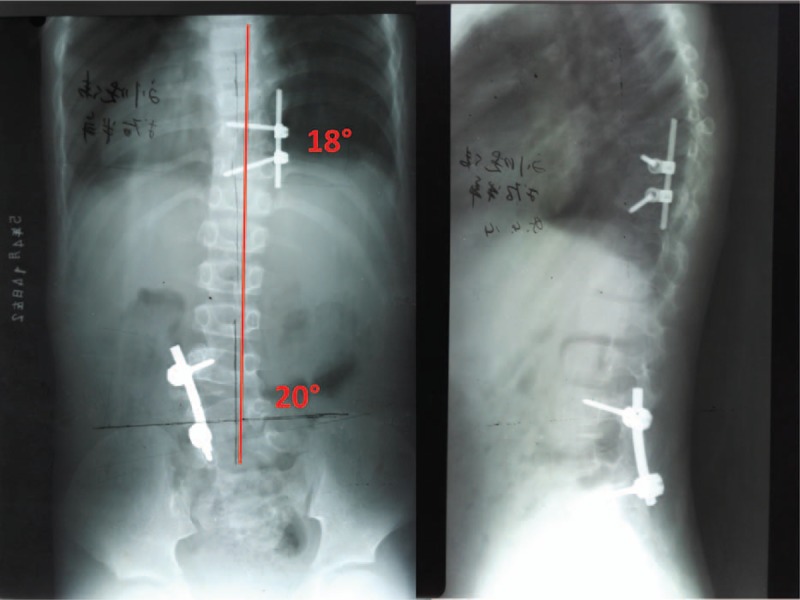
Figure 7.
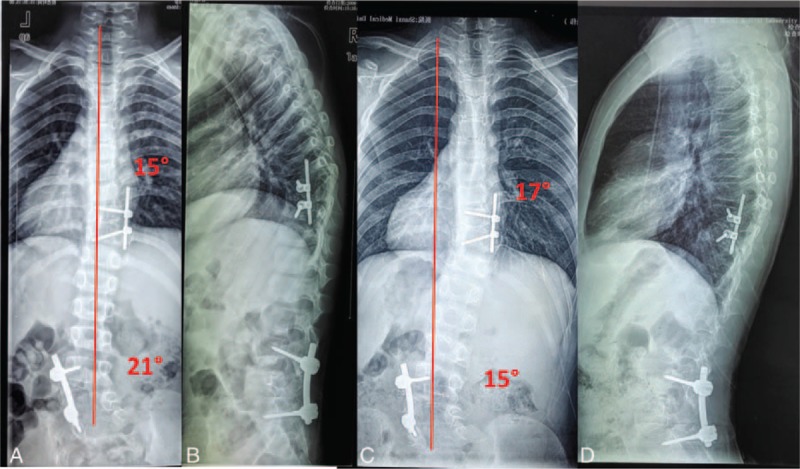
A standing radiograph 44 months (A and B), 60 months (C and D) at the third post-operation.
Figure 8.
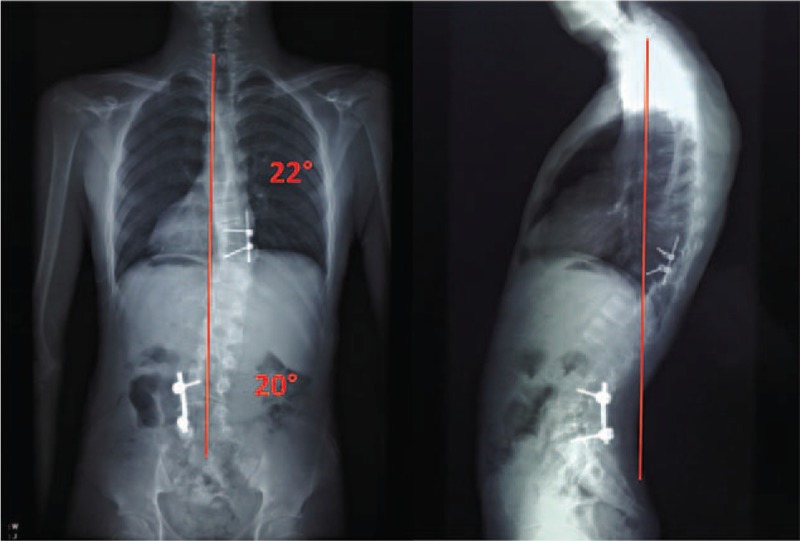
A standing radiograph 96 months at the third post-operation (at 17 years of age).
Overall, clinical and radiological follow-ups were performed at 4 months, 44 months, 5 years, and 8 years at the third postoperatively (Figs. 7, 8 and 9). Good coronal and sagittal alignment of the spine was observed clinically and radiographically at the final follow-up. A slight lumbar scoliotic deviation was detected on the radiographs taken at the 5-year follow-ups, which was obviously improved at 8-year final follow-up (Fig. 8). He had led an almost normal life since his surgery, avoiding most physical exercise except hiking. His complaints were of some mild back pain in the morning of about 1 years’ duration. He ambulated without a limp. Heel and toe stance was normal bilaterally. The Trendelenburg was negative bilaterally. The motor strength was normal bilaterally. Patellar and Achilles reflexes were normal bilaterally.
Figure 9.
A standing radiograph 4 months at the third post-operation (at 10 years of age).
4. Discussion
In theory, a hemivertebra should be treated at the earliest age possible if surgery is indicated, which was before the deformity progresses and structural change takes place in adjacent spinal segments.[12] Surgical procedures may include: in situ fusion, convex growth arrest, anterior and posterior fusion with or without instrumentation, hemivertebra excision, and fusion via a combined anterior and posterior approach in 1 or 2 stages.[9,13,14] The best permanent corrective surgery may be removal of the hemivertebra. Because it is very important to remove the pathogenic factor for spine deformities.
With modern techniques of surgery, including hemivertebra removal by a posterior-only approach, pedicle fixation, and the use of neurological monitoring, patients can avoid the dual approach, longer fusion, and extensive casting that this patient required. A more recent publication is that by Chang et al in 2015.[14] They reported on 18 children, aged 2.6 to 9.8 years, by posterior hemivertebra resection and bilateral pedicle screw fixation. They reported a mean preoperative curve of 34.4 degree with a final correction to 12.9 degree. Another recent publication is that of Zhuang et al in 2016.[15] They reported on 14 patients with a mean follow-up of 38.4 months. All patients were lumbosacral hemivertebrae, and the mean age at surgery was 10 years. The average preoperative curve was 30 degree and was 4 degree at final follow-up.
This case illustrates what was not suitable in the treatment of congenital scoliosis, which is what caused significant curve progression and trunk imbalance. In first procedure, the hemivertebra was not excision. Preoperative radiograph clearly showed that a fully segmented hemivertebra was causing the patient's condition. In other words, the first operation should have been a hemivertebral resection or at least an anterior-posterior epiphysiodesis, not simply a posterior segmental fixation, because remnant hemivertebral segments can grow and lead to increasing deformity. At the age of 8 years, for thoracic scoliosis, we decided to conduct an operation via anterior approach even though the patient had a relatively small Cobb angle of 36 degree, which might be considered excessively aggressive treatment.
A hemivertebra of L4/5 OR L5 creates a special problem. As the hemivertebra grows, it causes a progressive tilting of L4. This causes the lumbar spine to be progressively displaced laterally. The normal compensatory mechanism could result in a secondary curve beginning at L4 distally and usually going up into the lower thoracic spine. With progressive tilting of L4, this secondary curve becomes larger and larger. With time, it will develop structural changes such as rotation and rigid. Therefore, indications for surgery must be determined mainly on the basis of trunk imbalance from a large curve induced by the vertebral malformation, not only on the Cobb angle of the short curve around the hemivertebra. Spinal deformities can worsen during pubertal growth, usually taking the form of a wider scoliosis curve than the local malformative curve. A hemivertebrectomy via anterior or posterior approach should have been considered to achieve a sagittal and coronal balance of the spine. However, that extensive surgery was not carried out in a young child as there was a high risk of complications such as excessive blood loss and neurologic complications. The final decision for revision surgery was hemivertebra resection and short-segment fusion combined with unilateral instrumentation. In this way, more growing segments and motor units were preserved. Meanwhile, only convex exposure and fixation can preserve concave growth potential.
There is a limitation to our study: most cases differ greatly even though they may present with similar symptoms, so we are unable to draw definite conclusions from a single case report. However, there are very few previously published case reports on long-term follow-up for curve progression and trunk imbalance after posterior instrumentation in congenital scoliosis towing to dual hemivertebra in thoracic and lumbosacral region at a young age, so this report is valuable. In addition, radiograph information of this case was incomplete. Especially in the early, limited to insufficient equipment, the whole spine radiograph can’t be filmed. Nevertheless, most of the important information of patient can be obtained.
In summary, our case showed that both unilateral instrumentation without hemivertebra excision and fusion resulting in an unacceptable deformity and the excellent outcome that can be achieved with resection. Congenital scoliosis owing to hemivertebra at a young age could be treated by hemivertebra resection or anterior and posterior epiphysiodesis as definitive surgical treatment. Thus, early recognition and very early resection and limited fusion were needed for this patient.
Acknowledgments
The authors thank the center’ colleagues and the devotion of the patient.
Footnotes
Abbreviations: L = Lumbar, S = Sacral, T = Thoracic.
The authors report no conflicts of interest.
References
- [1].Ruf M, Jensen R, Letko L, et al. Hemivertebra resection and osteotomies in congenital spine deformity. Spine (Phila Pa 1976) 2009;34:1791–9. [DOI] [PubMed] [Google Scholar]
- [2].Chu G, Huang J, Zeng K, et al. A modified surgical procedure for congenital kyphoscoliosis: selective partial hemivertebrectomy via posterior-only approach. Childs Nerv Syst 2015;31:923–9. [DOI] [PubMed] [Google Scholar]
- [3].Shono Y, Abumi K, Kaneda K. One-stage posterior hemivertebra resection and correction using segmental posterior instrumentation. Spine (Phila Pa 1976) 2001;26:752–7. [DOI] [PubMed] [Google Scholar]
- [4].Ruf M, Harms J. Posterior hemivertebra resection with transpedicular instrumentation: early correction in children aged 1-6 years. Spine (Phila Pa 1976) 2003;28:2132–8. [DOI] [PubMed] [Google Scholar]
- [5].McMaster MJ, Ohtsuka K. The natural history of congenital scoliosis. A study of two hundred and fifty-one patients. J Bone Joint Surg Am 1982;64:1128–47. [PubMed] [Google Scholar]
- [6].Repko M, Krbec M, Burda J, et al. Simple bony fusion or instrumented hemivertebra excision in the surgical treatment of congenital scoliosis. Acta Chir Orthop Traumatol Cech 2008;75:180–4. [PubMed] [Google Scholar]
- [7].Ruf M, Jensen R, Jeszenszky D, et al. Hemivertebra resection in congenital scoliosis: early correction in young children. Z Orthop Ihre Grenzgeb 2006;144:74–9. [DOI] [PubMed] [Google Scholar]
- [8].Hedequist D, Emans J, Proctor M. Three rod technique facilitates hemivertebra wedge excision in young children through a posterior only approach. Spine (Phila Pa 1976) 2009;34:E225–9. [DOI] [PubMed] [Google Scholar]
- [9].Holte DC, Winter RB, Lonstein JE, et al. Excision of hemivertebrae and wedge resection in the treatment of congenital scoliosis. J Bone Joint Surg Am 1995;77:159–71. [DOI] [PubMed] [Google Scholar]
- [10].Piantoni L, Francheri Wilson IA, Tello CA, et al. Hemivertebra resection with instrumented fusion by posterior approach in children. Spine Deform 2015;3:541–8. [DOI] [PubMed] [Google Scholar]
- [11].Qureshi MA, Pasha IF, Khalique AB, et al. Outcome of hemivertebra resection in congenital thoracolumbar kyphosis and scoliosis by posterior approach. J Pak Med Assoc 2015;65(11 suppl 3):S142–6. [PubMed] [Google Scholar]
- [12].Ruf M, Harms J. Pedicle screws in 1- and 2-year-old children: technique,complications, and effect on further growth. Spine (Phila Pa 1976) 2002;27:E460–6. [DOI] [PubMed] [Google Scholar]
- [13].Callahan BC, Georgopoulos G, Eilert RE. Hemivertebral excision for congenital scoliosis. J Pediatr Orthop 1997;17:96–9. [PubMed] [Google Scholar]
- [14].Chang DG, Kim JH, Ha KY, et al. Posterior hemivertebra resection and short segment fusion with pedicle screw fixation for congenital scoliosis in children younger than 10 years: greater than 7-year follow-up. Spine (Phila Pa 1976) 2015;40:E484–91. [DOI] [PubMed] [Google Scholar]
- [15].Zhuang Q, Zhang J, Li S, et al. One-stage posterior-only lumbosacral hemivertebra resection with short segmental fusion: a more than 2-year follow-up. Eur Spine J 2016;25:1567–74. [DOI] [PubMed] [Google Scholar]


