Abstract
Rationale:
Ectopic thyroid carcinoma within a thyroglossal duct cyst (TGDCCa) is an extremely rare entity. Thus, there is no unified appropriate therapeutic strategy, and individual approaches are controversial.
Patients concerns:
We report the case of a 21-year old woman who underwent Sistrunk procedure for a thyroglossal duct cyst (TGDC).
Diagnoses:
During histological evaluation of the resected TGDC a papillary thyroid carcinoma was found.
Interventions:
Due to a tumor size of 1cm and proximity to the surgical border, Sistrunk procedure was extended by total thyroidectomy, followed by radioiodine ablation.
Outcomes:
Except of minimal follicular hyperplasia, the histological examination of the resected thyroid gland was unsuspicious.
Lessons:
Therapeutic management of TGDCCa is of interdisciplinary debate due to relative infrequence of the disease and consequently lack of unified therapeutic guidelines. We suggest a personalized therapeutic approach adjusted to individual risk stratification. In young patients with small tumor size and with confirmation of TGDCCa representing the primary tumor, Sistrunk procedure alone may reflect adequate treatment. In all other cases, total thyroidectomy and radioiodine ablation should be evaluated. Overall TGDCCa have an excellent prognosis with a 5-year survival rate of more than 90%.
Keywords: ectopic papillary thyroid carcinoma, Sistrunk procedure, thyroglossal duct cyst carcinoma, thyroglossal duct cyst
1. Introduction
Thyroglossal duct cysts (TGDCs) represent the most common midline neck mass in children and the majority of manifestations initially present as an anterior, painless, infrahyoid mass freely moving with deglutition. TGDCs arise from the failure of the thyroglossal duct to obliterate during embryologic development. The duct passes close to the hyoid bone during its descent, resulting in the subsequent close relationship between these two structures.[1]
Most diagnoses of TGDCs emerge from incidental palpation of soft swelling at the neck during physical examination by the pediatrician. In 22% to 43% of the cases, patients present with swallowing difficulties or relapsing infections of the throat.[2]
The diagnostic steps following the suspected diagnosis of a TGDC involve morphological imaging of the neck by ultrasound or magnetic resonance tomography. Only the presence of solid tissue within the thyroglossal mass or pathologies within the thyroid bed usually lead to further investigations such as scintigraphy or fine needle aspiration. Therapy of choice of all TGDCs is the surgical resection by Sistrunk procedure.[3]
Ectopic thyroid tissue within TGDCs is a common finding. But only in about 1% to 6.5% of cases scattered thyroid tissue within TGDC becomes malignant and particularly develops papillary thyroid carcinomas.[4–6] To our knowledge, worldwide there are less than 250 cases of TGDCCa documented. In most cases thyroid carcinoma is diagnosed incidentally by histological investigation after resection of a TGDC.[4] Considering the rarity of this type of carcinoma, no consensus exists about the appropriate treatment approach and particularly the radical extent of oncological therapy.
We report the incidental finding of a papillary thyroid carcinoma within a TGDC, resected by the Sistrunk procedure in a 21-year old woman.
2. Case presentation
A 21-year old woman presented with a histologically prediagnosed TGDCCa to the Department of Endocrinology of the University Hospital of Freiburg Germany seeking a second opinion about treatment options. About 6 months prior, the patient sought medical attention due to a growing painless soft swelling mass located in the anterior midline of her neck. Subsequently, she was referred to an Otorhinolaryngology Department of a regional hospital. An ultrasound revealed a supralaryngeal cyst of 2 cm in diameter cranial to the hyoid bone, including solid tissue within the cyst (Fig. 1).
Figure 1.
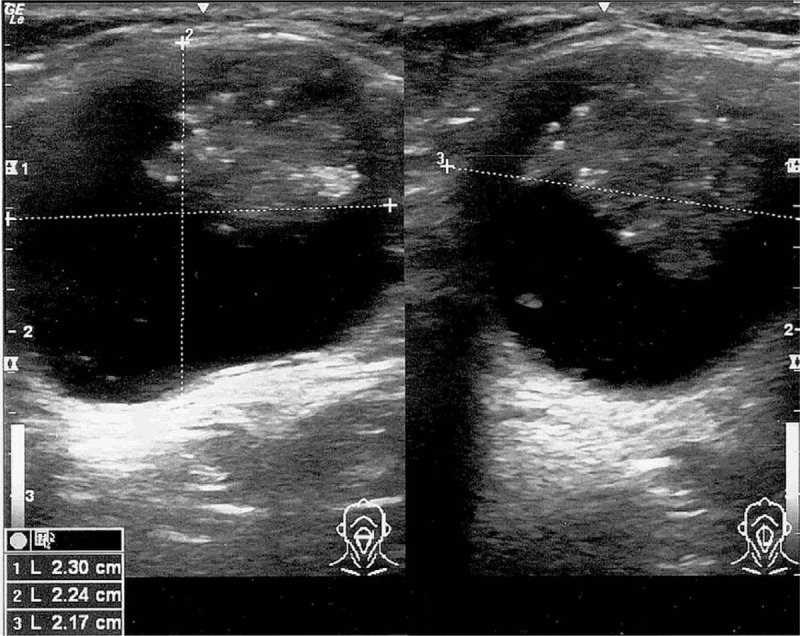
Ultrasound of thyroglossal duct cyst. Ultrasound of the neck detected a supralaryngeal cyst in size of 2.30 × 2.24 × 2.17 cm above the hyoid bone, including solid tissue within the cyst. Ultrasound of the thyroid gland and cervical lymph nodes remain unsuspicious.
Two months later, Sistrunk procedure was performed. The histopathological examination of the resected tissue detected malignant degenerated thyroid cells of a papillary thyroid carcinoma within the wall of the TGDC. Histological tumor size was 1 cm in total. The distance to the resection border was minimal 1 mm (Fig. 2).
Figure 2.
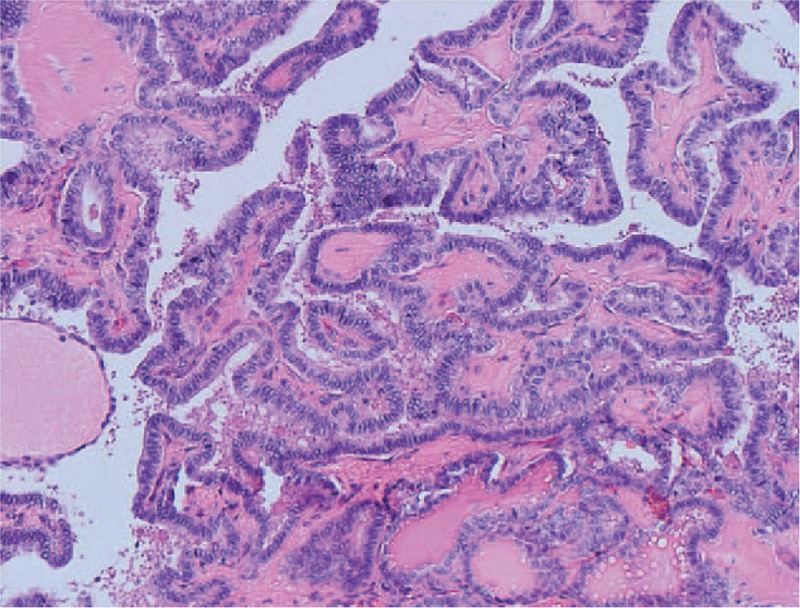
Histology of resected papillary thyroglossal duct cyst carcinoma (TGDCCa). Histologically the TGDC was enclosed by a thin wall, consisting of connective tissue. Within the cyst there was a branched framework of papillary glands, filled with colloid. The papillae were covered by a single layer of epithelial tumor cells with cell nuclei showing typical alterations. The distance to the resection border was minimal 1 mm, equivalent to the cyst wall. There was no vascular invasion detectable. TGDC = thyroglossal duct cyst, TGDCCA = thyroglossal duct cyst carcinoma.
The patient neither had any pre-existing diseases, nor a history of radiation exposure. Independently however, there was a strong positive family history for thyroid disorders. Thyroidectomy was performed in both parents because of cold nodules, postoperatively turning out as benign lesions. Her sister suffers from the Hashimoto thyroiditis.
After the diagnosis of TGDCCa, the following staging investigations were performed. The ultrasound of the thyroid gland detected multiple thyroid cysts, without any indicators suspicious for malignancy. A thyroid scintigraphy confirmed the tumors representing uncomplicated thyroid cysts. Physical examination including lymph node palpation as well as x-ray of the chest remained unsuspicious. Laboratory examination confirmed a euthyroid metabolic state without thyroid-specific medication. Thyroglobulin level was 8.2 μg/L.
After detailed discussion of the case in an interdisciplinary tumorboard, total thyroidectomy with subsequent radioiodine ablation was recommended.
A few weeks later, total thyroidectomy with autotransplantation of the left upper parathyroid gland was performed. The histological examination of the removed thyroid tissue revealed benign thyroid cells with minimal follicular hyperplasia. A single removed and histologically examined perithyroidal lymph node was tumor free. Postoperative thyroglobulin level fell to 3.38 μg/L. Two weeks after the operation, ablative radioiodine treatment was performed. Follow-up surveillance including ultrasound imaging of the neck, as well as marker analysis of thyroglobulin are planned every 6 months for a period of 5 years.
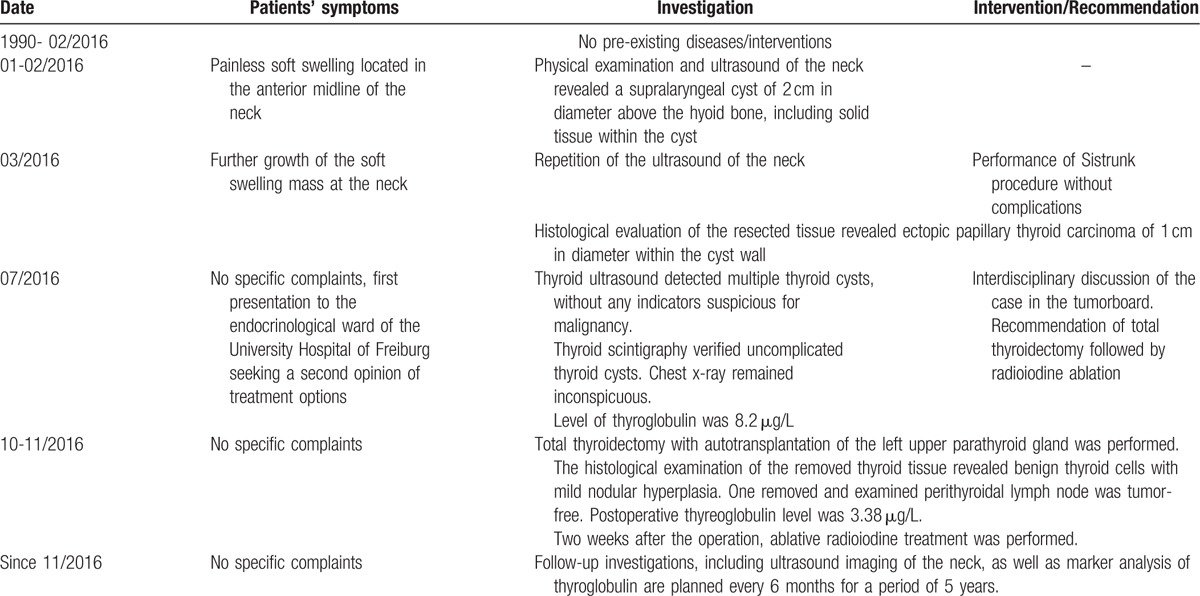
The timeline of the patient's medical history is shown in Table 1.
Table 1.
Timeline of the patient's medical history.
3. Discussion and conclusions
Thyroglossal cysts are the most common congenital anomaly around the neck.[1] As reported in this case, most patients present with painless swelling in the midline of the neck, only rarely accompanied by dysphagia or dyspnea.[2]
Ectopic thyroid tissue within TGDC can frequently be histologically detected. However, the development of thyroid cancer from ectopic thyroid tissue within the TGDC is a very rare disease with only about 250 cases ever described worldwide.[4]
While infrequent, the initial assessment of all TGDCs nevertheless should always include consideration of possibly existing ectopic thyroid tissue and TGDCCa. Thus, clinical examination of TGDC has to be complemented by investigation of the cervical lymph nodes, as well as thyroid function and imaging, and possibly thyroglobulin analysis. Apart from morphological suspiciousness of the thyroid gland, the rare pathology of absent thyroid tissue in the thyroid bed has to be ruled out by thyroid sonography, because in this case, Sistrunk procedure would remove all functionally active thyroid cells.[3,4]
Clinical signs of malignancy, such as solid tissue within the TGDC, as well as hard, fixed and rapidly growing tumors should lead to further investigations including scintigraphy and/or fine needle aspiration.[7] However, TGDCCas often emerge without apparent abnormalities within the thyroid gland or cervical lymph nodes.[4,5] Even fine needle aspiration comes with a high false negative rate, resulting in the fact, that TGDCCas often are an incidental outcome of histopathological evaluation of resected cysts.[8]
Most TGDCCas represent papillary thyroid carcinomas (85.5%–94%).[4] Only about 6% are squamous cell carcinomas with a significantly worse prognosis.[7,9] To our knowledge, distant metastases from papillary thyroid carcinoma in a TGDC at the stage of diagnosis have never been reported so far.[4,5,7] However, cervical lymph node metastases are prevalent in 7.7% to 15% of the cases.[4] Therefore, we consider imaging of the neck as well as lymph node palpation to be sufficient for clinical staging.
Until now, neither the European nor the American Thyroid Association Guidelines address the therapeutic management of TGDCCa, resulting in interdisciplinary debates regarding the need for thyroidectomy and radioiodine ablation following Sistrunk procedure.[10]
Our case reports of a young patient presenting with a TGDCCa of limited size of 1 cm. Thyroid imaging by ultrasound and scintigraphy was unsuspicious except of multiple intrathyroidal cysts. According to the 2009 American Thyroid Association Initial Risk Stratification Guidelines, an intrathyroidal papillary thyroid carcinoma with the same histological and clinical characteristics as the TGDCCa of our patient would have been categorized as of low risk for recurrent disease.[10] However, since concomitant intrathyroidal tumors even of small tumor size (mean 1.4 cm) occur in 30%, with TGDCCa then being interpreted as distant metastases, we suppose TGDCCa to follow other principles of tumor progression than classical intrathyroidal papillary thyroid carcinomas.[5]
Mandatory for the elaboration of a standardized therapeutic management of these rare carcinomas is the understanding of the origin of this malignant formation. In fact, two possibilities for the development of a TGDCCa exist.
Some authors consider the ectopic thyroid tissue within the cyst to be the primary origin of the malignant cells. In this case, the presence of thyroglossal remnant and an epithelial lining of thyroid cells within the cyst wall with concurrent unsuspicious thyroid tissue were proposed to be indicators of TGDC being the primary origin.[4] Consequently, in young patients with small tumors inferior to 1 cm without extracystic invasion and normal thyroid and lymph node investigation, Sistrunk procedure may be considered sufficient as therapy.[4,5]
Other authors refer to the possibility of TGDCCa representing a distant metastasis of a pre-existing thyroid carcinoma within the thyroid gland itself.[11] Consequently, many authors recommend more extensive therapy for TGDCCa with at least total thyroidectomy often followed by radioiodine ablation.[6]
Regarding the borderline tumor size of the TGDCCa of our patient, but short distance of the resection border to the malignant cells without extracystic invasion, we consider both Sistrunk procedure with close clinical follow-up as well as additional thyroidectomy with radioiodine ablation to be reasonable therapeutic approaches. However, due to the patient's request for a therapy being as safe as possible and to enable facilitated follow-up care by thyroglobulin measurement, we decided to perform total thyroidectomy with subsequent radioiodine ablation. The postoperative histological examination of the resected thyroid gland excluded concomitant carcinoma.
Several case reports describe postoperative local or lymph node recurrence in 20% of the cases.[6] Therefore, we arranged regular follow-up examinations including clinical examination and thyroglobulin measurement every 6 months, and thyroid imaging by ultrasound once a year. Until now, 12 month after surgery and radioiodine ablation the patient remained tumor free.
The present case illustrates the challenging objective of choosing the appropriate individual therapeutic strategy for an incidentally detected TGDCCa. We propose to adjust the therapeutic approach for TGDCCa according to the probability whether the TGDC is the primary origin of this tumor or a metastatic lesion of an intrathyroid primary tumor. While Sistrunk procedure represents an adequate therapy for young patients with small carcinomas and unsuspicious staging investigations, total thyroidectomy with subsequent radioiodine ablation should be conducted in patients who exhibit any risk factors such as tumor size above 1 cm, extracystic invasion and suspicion resulting from thyroid imaging. In borderline cases, total thyroidectomy constitutes a safe therapeutic strategy offering the advantage of easy follow-up care by thyroglobulin measurement and scintigraphy. However, a maximum of safety may also be accompanied by potential overtreatment.
Overall the prognosis of TGDCCa is very good with a five-year-survival rate of 95%.[8]
Footnotes
Abbreviations: TGDC = thyroglossal duct cyst, TGDCCA = thyroglossal duct cyst carcinoma.
Declarations: Ethics approval and consent to participate: Not applicable.
Consent for publication: The patient has given her informed written consent for publishing this case report.
Availability of data and material: The authors declare that the data supporting the findings of this study are available within the article.
Competing interests: The authors declare that they have no competing interests.
Authors’ contributions: OE made the initial diagnosis of the thyroglossal duct cyst and performed the Sistrunk procedure. ST performed the histological examination of the thyroglossal duct cyst. NR, KL, and JS took care over the patient after diagnosis of thyroglossal duct cyst carcinoma and managed therapy as well as the postoperative follow-up examinations. NR was the major contributor in writing this manuscript. All authors listed above have participated in critical revision of the article and gave their final approval of this version of the manuscript to be published.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Oomen K, Modi V, Maddalozzo J. Thyroglossal duct cyst and ectopic thyroid: surgical management. Otolaryngol Clin North Am 2015;48:15–27. [DOI] [PubMed] [Google Scholar]
- [2].Shah R, Gow K, Sobol SE. Outcome of thyroglossal duct cyst excision is independent of presenting age or symptomatology. Int J Pediatr Otorhinolaryngol 2007;71:1731–5. [DOI] [PubMed] [Google Scholar]
- [3].Enepekides D. Management of congenital anomalies of the neck. Facial Plast Surg Clin North Am 2001;9:131–45. [PubMed] [Google Scholar]
- [4].Carter Y, Yeutter N, Mazeh H. Thyroglossal duct remnant carcinoma: beyond the Sistrunk procedure. Surg Oncol 2014;23:161–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Thompson LD, Herrera HB, Lau SK. Thyroglossal duct cyst carcinomas: a clinicopathologic series of 22 cases with staging recommendations. Head Neck Pathol 2016;11:175–85. (Epub ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Forest V, Murali R, Clark J. Thyroglossal duct cyst carcinoma: case series. J Otolaryngol Head and Neck Surgery 2011;40:151–6. [PubMed] [Google Scholar]
- [7].Ferrer C, Ferrández A, Dualde D, et al. Squamous cell carcinoma of the thyroglossal duct cyst: report of a new case and literature review. J Otolaryngol 2000;29:311–4. [PubMed] [Google Scholar]
- [8].Patel N, Sheykholeslami K. Papillary carcinoma in thyroglossal duct cyst: two case reports and review of the literature. Ear Nose Throat J 2016;95:E36–8. [PubMed] [Google Scholar]
- [9].Shah S, Kadakia S, Khorsandi A, et al. Squamous cell carcinoma in a thyroglossal duct cyst: a case report with review of the literature. Am J Otolaryngol 2015;36:460–2. [DOI] [PubMed] [Google Scholar]
- [10].Haugen B, Alexander E, Bible K, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016;1:1–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Baglam T, Binnetoglu A, Yumusakhuylu A, et al. Does papillary carcinoma of thyroglossal duct cyst develop de novo. Case Rep Otolaryngol 2015;2015:382760. [DOI] [PMC free article] [PubMed] [Google Scholar]


