Abstract
Rationale:
Primary pulmonary NK/T cell lymphoma is extremely rare, and only a few cases have reported so far. Its diagnosis is mainly dependent on open-lung biopsy.
Patient concerns:
Here, we report a 44-year-old male who was initially misdiagnosed as having pneumonia according to the clinical characteristics and computed tomography (CT) findings.
Diagnosis:
The first lung biopsy indicated a large number of coagulative necrotic lesions, and definite diagnosis was made after the second lung biopsy following non-response to 6-day wide spectrum antibiotic therapy. The second lung biopsy showed the tumor cells were positive for LCA, CD3ε, CD30, TIA-1, Ki67 and negative for CD20, CD56, CD1a, MPO, CK, S-100, desmin, and CD34.
Interventions:
This patient refused to receive further therapy and died 1 month after confirmed diagnosis.
Outcomes:
Clinically, it is difficult to differentiate pneumonia from NK/T cell lymphoma in pathology due to the presence of plenty of focal necrosis in primary pulmonary NK/T cell lymphoma.
Lessons:
The diagnosis of primary pulmonary NK/T cell lymphoma should be based on lung biopsy (usually multiple lung biopsies are required), immunohistochemistry and clinical and imaging findings.
Keywords: extranodal NK/T cell lymphoma, literature review, misdiagnose, pneumonia
1. Introduction
Extranodal natural killer/T-cell lymphoma (ENKTL), nasal type, is deviated from either activated NK cells or cytotoxic T cells. Although it may involve nasal cavity, skin, upper respiratory tract, gastrointestinal tract, testes, brain, salivary glands, pancreas, soft tissues, adrenal glands, bone marrow and other extranodal sites, the nasal cavity is the most common site of involvement.[1,2] In cases of ENKTLs, only a few cases reported involving the lung.[3,4] Primary pulmonary NK/T cell lymphoma originates from lung parenchyma, bronchi, and/or its regional lymph nodes. Primary pulmonary NK/T cell lymphoma is extremely rare and represents 0.4% of all lymphoma, 3 to 4% of all extranodal manifestations and 0.5 to 1% of all primary pulmonary malignancies.[5,6] Although this lymphoma can occur in subjects of any age group, it appears has a higher incidence in subjects aged 20 to 80 years (median: 50 years) and occurs more commonly in men than women.[2,7,8] The imaging findings of primary pulmonary NK/T cell lymphoma are nonspecific, and thus it is easily misdiagnosed as pneumonia in the early stage. Here, we report a case of primary pulmonary NK/T cell lymphoma in a 44-year-old Chinese male patient and its clinical characteristics, computed tomography (CT) findings, pathological characteristics and immunophenotype are described.
2. Case report
A 44-year-old Chinese male presented with weakness, cough, and intermittent fever for half a month. Moist rales were noted at the base of both lungs on auscultation. Laboratory examinations showed white blood cell count and percentage of neutrophils elevated moderately (white blood cells: 11.2×109/L; neutrophils: 88%). The Epstein–Barr virus test showed positive. Immune function tests and sputum culture displayed negative. CT of the chest showed multiple lesions in both lungs (Fig. 1). Bronchoscopy failed to find abnormalities (Fig. 2). CT-guided lung biopsy revealed a large amount of necrotic tissues in the right lung, in which a small amount of inflammatory cells, fibroblasts and some atypical small–medium-sized cells were observed. Only a small number of lymphocytes were found in the left lung. Staining of gram stain and special stains for atypical organisms including mycobacteria, fungi, and pneumocystis carinii also showed negative. He was diagnosed as pneumonia and treated with broad spectrum antibiotics for 6 days, but symptoms remained unchanged and he showed persistent fever, fatigue, and poor appetite. Meanwhile, the counts of white blood cells and platelets decreased progressively. A second CT of the chest showed diffuse infiltration in both lungs, measuring up to 7 cm in diameter, with consolidation and atelectasis in the middle lobe of right lung. Obvious mediastinal and hilar lymphadenopathy was not observed (Fig. 3).
Figure 1.
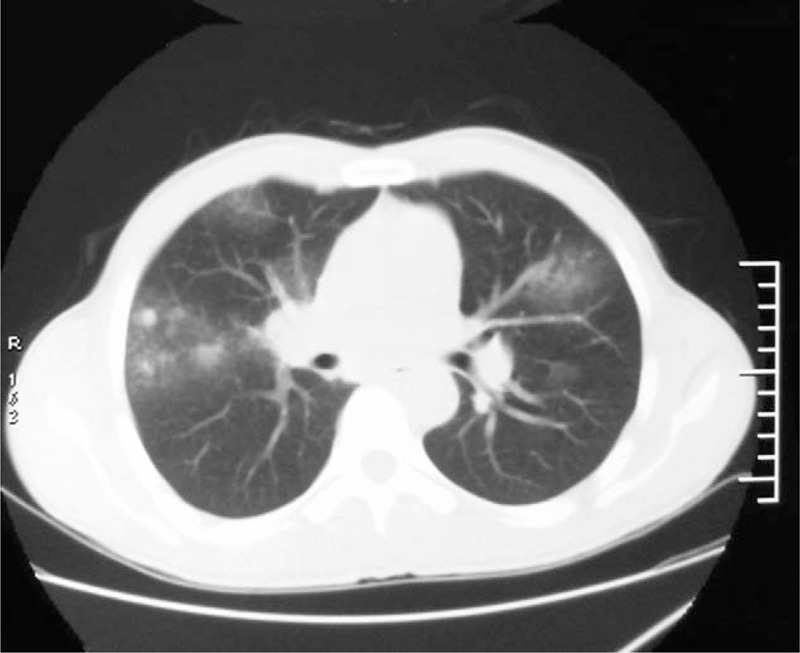
CT of the chest showed multiple nodules and masses of variable sizes in both lungs. Halo signs were observable in some masses. CT = computed tomography.
Figure 2.
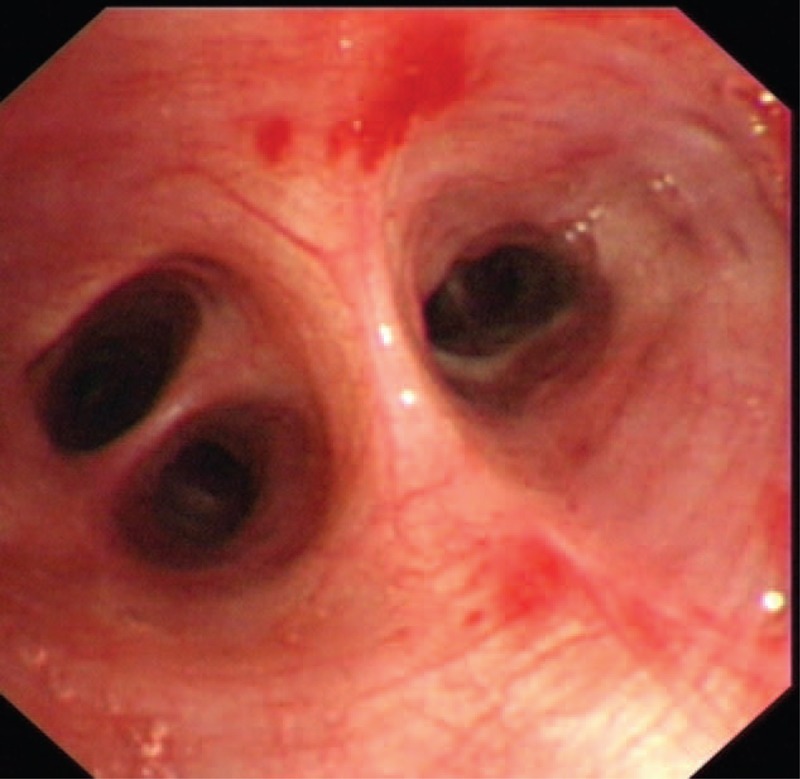
Bronchoscopy showed normal.
Figure 3.
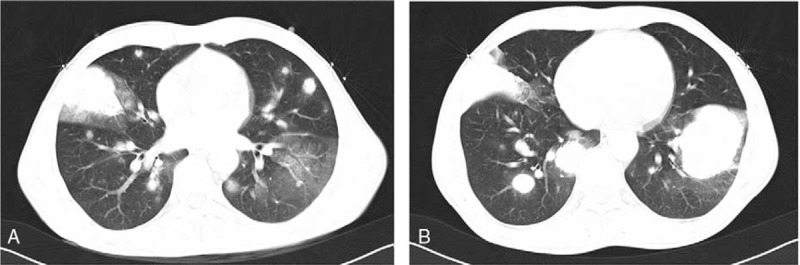
CT of the chest after 6-day treatment. (A) 20×30 mm mass was observed in the right lung and halo signs were observable. Some nodules of variable sizes were found in both lungs. (B) 30×40 mm mass was noted in the left lung, but not found on the previous CT. CT = computed tomography.
Then, the patient received a second lung biopsy which showed atypical lymphoid cells infiltration with necrosis in the lung (Fig. 4). The tumor cells were positive for LCA, CD3ε, CD30, TIA-1, and Ki67, but negative for CD20, CD56, CD1a, MPO, CK, S-100, desmin, and CD34. In situ hybridization showed that tumor cells were positive for Epstein–Barr virus encoded RNA (EBER). Examination of the bone marrow showed the infiltration of diffused or clustering lymphocytes, and cells were positive for CD3ε and CD20, but negative for granzyme B and CD56. Therefore, the patient was diagnosed as having primary pulmonary extranodal NK/T-cell lymphoma of nasal type. Unfortunately, the patient refused further therapy and died 1 month later.
Figure 4.

The lesions showed extensive coagulative necrosis and infiltration of atypical lymphoid cells. (A) Hematoxylin and eosin staining (200×); (B, C) hematoxylin and eosin staining (400×); (D) cells were positive for CD3 (400×); (E) tumor cells were positive for Epstein–Barr virus-encoded RNA (EBER) (in situ hybridization; 400×); (F) cells were negative for CD56 (200×); (G) cells were positive for KI67 (400×).
3. Discussion
Primary pulmonary NK/T cell lymphoma is a rare and aggressive malignancy, and only a few cases have been reported so far in Japan, Korea, the United States, China, and Taiwan.[1,2,5,9–12] It is rare in the United States and Europe, but more prevalent in Asia, South and Central America, and Mexico. Reviewing literatures indicated a total of 12 cases were reported between 1990 and 2017 except for the case we reported (Table 1). The clinical characteristics of these cases are summarized in Table 1. Of 12 patients, 2 were from Taiwan China, three from United States, and six from China mainland. The prevalence is significantly higher in yellow race than in white race, which might be ascribed to the geographical and ethnic susceptibility, but there are no specific epidemiological data available.[13–15] The available patients ranged from 23 to 83 years and with a female-to-male ratio of approximately 1:1. Patients present with fever, cough, dyspnea, and other symptoms, which however are nonresponsive to antibiotics. The common radiographical findings are the consolidation, nodules, and masses. Hilar adenopathy, pleural effusion, and atelectasis have also been reported.[10,15–18]
Table 1.
Primary pulmonary NK/T cell lymphoma reported since 1990.

CT findings of the primary pulmonary NK/T cell lymphoma usually vary and are nonspecific. These findings can be divided into 3 types—nodular or mass-like, mesenchyma-like, and pneumonia-like.[12,16] Thus, it is difficult to differentiate primary pulmonary NK/T cell lymphoma from pneumonia if CT of the chest shows pneumonia-like features. In this patient, halo signs were also found, and bleeding was observed surrounding the halo signs. The halo signs can be found mostly in invasive aspergillosis, and rarely in tumor. Lymphoma cells can invade blood vessels leading to the bleeding of surrounding tissues. Thus, the halo signs can also be observed in primary pulmonary NK/T cell lymphoma.
The diagnosis of NK/T cell lymphoma is on the basis of following features: (1) Lesions occur in the nose, skin, facial midline, lung, and other soft tissues. (2) In situ hybridization shows being positive for EBER. (3) The lymphoma infiltrates in a diffuse pattern and is usually angiocentric and angiodestructive with coagulative necrosis and apoptotic bodies. (4) Cells are positive for CD2, cytoplasmic CD3ε, CD56, cytotoxic granule-associated proteins (such as granzyme B, TIA1, and perforin.).[19–21] This patient was positive for EBER, LCA, CD3ε, CD30, TIA-1, and Ki67. Although he was negative CD56 as a marker, this patient met the diagnostic criteria in the 2008 WHO classification of lymphomas. Most NK/T lymphoma patients show extensive necrosis in the lung and thus they are often misdiagnosed as having infectious lesions. Therefore, repeated lung biopsy is needed.
The prognosis of primary pulmonary NK/T-cell lymphoma is very poor and the longest survival time was less than 6 months in available reports.[1,5] Correct diagnosis and timely treatment may have benefits for prognosis. The patient we reported presenting with rapidly growing lung mass and positive EBER would mean a poor prognosis.[22] The optimal treatment has not been clearly established, although more than 70% of NK/T cell lymphoma patients received CHOP (cyclophosphamide, adriamycin, vincristine, and prednisone) based chemotherapy and surgical resection in the literatures.[23] It is reported that NK/T cell lymphoma is not sensitive to chemotherapy because of multidrug resistance gene expression. The recurrence rate is very high, and the skin and hypoderm are the most common sites of recurrence.[24] Some patients may be responsive to initial treatment, but this effectiveness lasts a short time, and patients will develop local recurrence, and distant metastasis soon after initial treatment. A definite diagnosis was not achieved in this patient until a second lung biopsy was performed. The disease condition of this patient deteriorated rapidly and he refused further therapy.
Footnotes
Abbreviations: CT = computed tomography, EBER = Epstein–Barr virus encoded RNA, ENKTL = Extranodal natural killer/T-cell lymphoma.
This study was approved by the ethics committee of People's Hospital of DeYang city. The patient consented to the publication of this study.
The authors have no conflicts of interest to disclose.
References
- [1].Chien CC, Lee HS, Lin MH, et al. Primary extranodal natural killer/T-cell lymphoma of bronchus and lung: a case report and review of literature. Thorac Cancer 2016;7:140–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Ding W, Wang J, Zhao S, et al. Clinicopathological study of pulmonary extranodal nature killer/T-cell lymphoma, nasal type and literature review. Pathol Res Pract 2015;211:544–9. [DOI] [PubMed] [Google Scholar]
- [3].Du J, Ma PP, Wang QY, et al. Extranodal NK/T-cell lymphoma, nasal type: a case report of 7-year natural course and review of literature. Int J Clin Exp Pathol 2015;8:9620–8. [PMC free article] [PubMed] [Google Scholar]
- [4].Gao LM, Liu WP, Yang QP, et al. Aggressive natural killer-cell leukemia with jaundice and spontaneous splenic rupture: a case report and review of the literature. Diagn Pathol 2013;8:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Gui W, Yang B, Shen Q, et al. Successful treatment with L-asparaginase-based regimen for primary pulmonary NK/T cell lymphoma: a case report and review of the literature. Clin Respir J 2015;9:493–6. [DOI] [PubMed] [Google Scholar]
- [6].Kwong YL, Kim WS, Lim ST, et al. SMILE for natural killer/T-cell lymphoma: analysis of safety and efficacy from the Asia Lymphoma Study Group. Blood 2012;120:2973–80. [DOI] [PubMed] [Google Scholar]
- [7].Hoshino T, Tatsuno K, Shimauchi T, et al. Epstein-Barr virus-associated T-cell lymphoproliferative disorder affecting skin and lung in an elderly patient. J Dermatol 2014;41:837–40. [DOI] [PubMed] [Google Scholar]
- [8].Zheng S, Ouyang Q, Li G, et al. Primary intestinal NK/T cell lymphoma: a clinicopathologic study of 25 Chinese cases. Arch Iran Med 2012;15:36–42. [PubMed] [Google Scholar]
- [9].Laohaburanakit P, Hardin KA. NK/T cell lymphoma of the lung: a case report and review of literature. Thorax 2006;61:267–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Oshima K, Tanino Y, Sato S, et al. Primary pulmonary extranodal natural killer/T-cell lymphoma: nasal type with multiple nodules. Eur Respir J 2012;40:795–8. [DOI] [PubMed] [Google Scholar]
- [11].Tsukahara T, Takasawa A, Murata M, et al. NK/T-cell lymphoma of bilateral adrenal glands in a patient with pyothorax. Diagn Pathol 2012;7:114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Xiao YL, Zhang DP, Wang Y. Primary pulmonary involvement of NK/T-cell lymphoma: report of two cases with literature review. Zhonghua Nei Ke Za Zhi 2007;46:988–91. [PubMed] [Google Scholar]
- [13].Gong L, Wei LX, Huang GS, et al. Identification of genuine primary pulmonary NK cell lymphoma via clinicopathologic observation and clonality assay. Diagn Pathol 2013;8:140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Liu CH, Wang HH, Perng CL, et al. Primary extranodal NK/T-cell lymphoma of the lung: mimicking bronchogenic carcinoma. Thorac Cancer 2014;5:93–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Reyes VE, Jr, Al-Saleem T, Robu VG, et al. Extranodal NK/T-cell lymphoma nasal type: efficacy of pegaspargase. Report of two patients from the United Sates and review of literature. Leuk Res 2010;34:e50–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Hamaguchi R, Saito H, Kegasawa K, et al. A case of extranodal NK/T-cell lymphoma, nasal type, with skin ulceration and multiple nodules in the lung. Nihon Kokyuki Gakkai Zasshi 2009;47:614–9. [PubMed] [Google Scholar]
- [17].Morovic A, Aurer I, Dotlic S, et al. NK cell lymphoma, nasal type, with massive lung involvement: a case report. J Hematop 2010;3:19–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Tababi S, Kharrat S, Sellami M, et al. Extranodal NK/T-cell lymphoma, nasal type: report of 15 cases. Eur Ann Otorhinolaryngol Head Neck Dis 2012;129:141–7. [DOI] [PubMed] [Google Scholar]
- [19].Mansoor A, Pittaluga S, Beck PL, et al. NK-cell enteropathy: a benign NK-cell lymphoproliferative disease mimicking intestinal lymphoma: clinicopathologic features and follow-up in a unique case series. Blood 2011;117:1447–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Pongpruttipan T, Kummalue T, Bedavanija A, et al. Aberrant antigenic expression in extranodal NK/T-cell lymphoma: a multi-parameter study from Thailand. Diagn Pathol 2011;6:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Pongpruttipan T, Sukpanichnant S, Assanasen T, et al. Extranodal NK/T-cell lymphoma, nasal type, includes cases of natural killer cell and alphabeta, gammadelta, and alphabeta/gammadelta T-cell origin: a comprehensive clinicopathologic and phenotypic study. Am J Surg Pathol 2012;36:481–99. [DOI] [PubMed] [Google Scholar]
- [22].Cao MS, Cai HR, Yin HL, et al. Primary natural killer/T cell lymphoma of the lung: two cases report and clinical analysis. Zhonghua Jie He He Hu Xi Za Zhi 2008;31:120–4. [PubMed] [Google Scholar]
- [23].Kim SJ, Kim K, Kim BS, et al. Phase II trial of concurrent radiation and weekly cisplatin followed by VIPD chemotherapy in newly diagnosed, stage IE to IIE, nasal, extranodal NK/T-Cell Lymphoma: consortium for improving survival of lymphoma study. J Clin Oncol 2009;27:6027–32. [DOI] [PubMed] [Google Scholar]
- [24].Kohrt H, Advani R. Extranodal natural killer/T-cell lymphoma: current concepts in biology and treatment. Leuk Lymphoma 2009;50:1773–84. [DOI] [PMC free article] [PubMed] [Google Scholar]


