Abstract
Rationale:
Central nervous system (CNS) metastases are rarely seen in patients with nasopharyngeal carcinoma (NPC).
Patient concerns:
Two NPC patients developed CNS metastases were collected in Fudan University Shanghai Cancer Center. The medical records were reviewed to document patients’ characteristics, treatment, and outcomes. In addition, we also provide an overview of the literature concerning this scenario.
Diagnoses:
Both patients were staged T4N1M0 with pathologically confirmed CNS metastases from nasopharyngeal carcinoma.
Interventions:
After the completion of initial chemoradiotherapy, metastases to CNS including brain and/or spine occurred during follow-up. Surgical resection combined with palliative chemoradiation was offered to alleviate the symptoms.
Outcomes:
Although multiple treatment modalities were given, both patients succumbed to disease progression.
Lessons:
The mechanism for CNS metastases is postulated through hematogenous route or cerebral spinal fluid spread. Good symptoms amelioration can be achieved with aggressive treatments such as surgery followed by palliative chemoradiation, but prognoses are ominous due to systematic disease dissemination.
Keywords: central nervous system metastases, cerebral spinal fluid spread, hematogenous dissemination, nasopharyngeal carcinoma
1. Introduction
Nasopharyngeal carcinoma (NPC) is one of the most common malignancies in Southern China. Although combined chemotherapy with radiotherapy has been widely used in treating locally advanced lesions, distant metastasis remains an obstacle of curing this disease. As we know, the most frequent sites of distant failure are lung, bone and liver. However, metastasis to the central nervous system (CNS) in NPC patients is considered to be quite rare. For patients with locally advanced NPC, it is not infrequent that the primary tumor directly invades the intracranial sites such as cavernous sinus through the skull base, but the true brain metastases are very scarce. CNS metastases are sparsely reported in NPC,[1–9] whereas the scenario can arise in other malignancies, especially common in primary lung and breast cancers.[10–17] The mechanism of CNS metastases was presumed either through hematogenous route or cerebral spinal fluid (CSF) spread. As a rare entity, a few patients with CNS metastases from NPC have been reported in the English literature till now. Herein we present 2 NPC patients developed CNS metastases with pathologically confirmed after completing the initial treatment in our institution. Furthermore, we overviewed the reports of cases with CNS metastases from NPC in the literature, hoping to obtain more insight into this uncommon phenomenon.
2. Methods and materials
2.1. Patients selection
Two NPC patients developed CNS metastases after completing the initial chemoradiotherapy, which had pathologically confirmed by surgery, were collected in Fudan University Shanghai Cancer Center. Both of them provided their written informed consent to participate in the study. The medical records including clinical features, treatment options, and outcomes were shown in detail as follows.
3. Case reports
3.1. Brain and spinal metastases
The patient was a 47-year-old female who presented with hearing impairment and neck mass in 2012. On admission, a local and systemic work-up which included magnetic resonance imaging (MRI) of the nasopharynx (NP) and the whole neck region, chest computed tomography (CT), abdominal ultrasound, and bone isotope scan were done in our institution. Pathology from biopsy specimen of NP was showed nonkeratinizing, undifferentiated carcinoma. MRI scan of the NP and neck revealed that the primary tumor infiltrated the skull base and the cavernous sinus, and metastasized to both lateral retropharyngeal and right upper neck lymph nodes. According to 7th edition of AJCC/UICC staging system, stage IV (T4N1M0) was diagnosed onset. Therefore, the patient received 2 cycles of neoadjuvant chemotherapeutic regimen of cisplatin, docetaxel, and 5-FU (TPF) followed by concurrent chemoradiotherapy. A total dose of 70.4 Gy to the primary tumor in 32 fractions using intensity modulated radiation therapy (IMRT) was delivered with concomitant weekly cisplatin. After completing the treatment, there was no evidence of tumor both in physical examination and radiological images.
This patient remained well until approximately 16 months after the completion of radiotherapy. She experienced chest pain, radiating to the lower extremity, and urinary incontinence. MRI scan of the spine demonstrated spindle-shaped lesions in 5th and 11th thoracic segments (Fig. 1). Considering the patient's neurological symptoms deteriorated, a standard thoracic laminectomy and intraspinal masses excision were performed. Pathologic observations using immunohistochemical staining validated that the lesions were squamous cell carcinoma metastasized from the nasopharynx (Fig. 2). Postoperative radiotherapy to T5/T11 metastases with total dose of 45 Gy in 25 fractions was given. Neurological deficits were ameliorated after the treatment. However, at a close follow-up after that, MRI scans of the spine demonstrated multiple extramedullary and intramedullary lesions in cervical and lumbus segments, and also an enhancing mass in the right frontal lobe (Fig. 3). To relieve the compressive symptoms such as pain and motor-sensory disorders, partial surgery on L1–3 segments was done and the pathology was also consistent with that from the nasopharyngeal carcinoma. Epstein-Barr virus-encoded RNA (EBER) staining using in situ hybridization (ISH) was positive in the surgical specimen (Fig. 4). Systemic and local treatments including chemotherapy and radiotherapy were offered to control the dissemination of the disease and improve the neurological handicaps. Unfortunately, despite of these aggressive therapies, the disease was exacerbation. She succumbed approximately 20 months from her diagnosis of CNS metastases.
Figure 1.
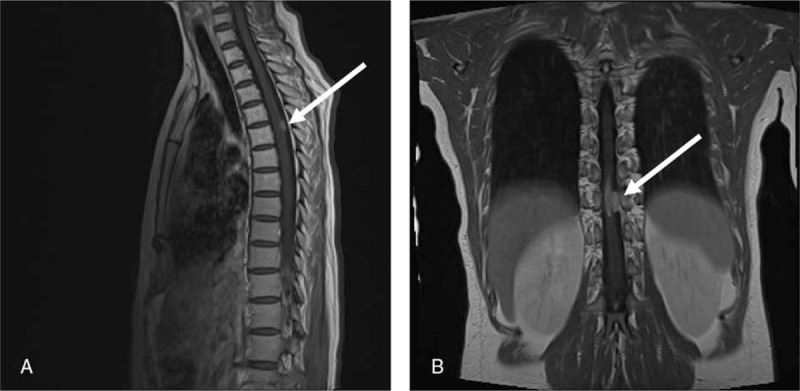
Sagittal and coronal MR images of the spine demonstrated multiple enhancing nodules in 5th (A) and 11th thoracic (B) segments (arrows).
Figure 2.
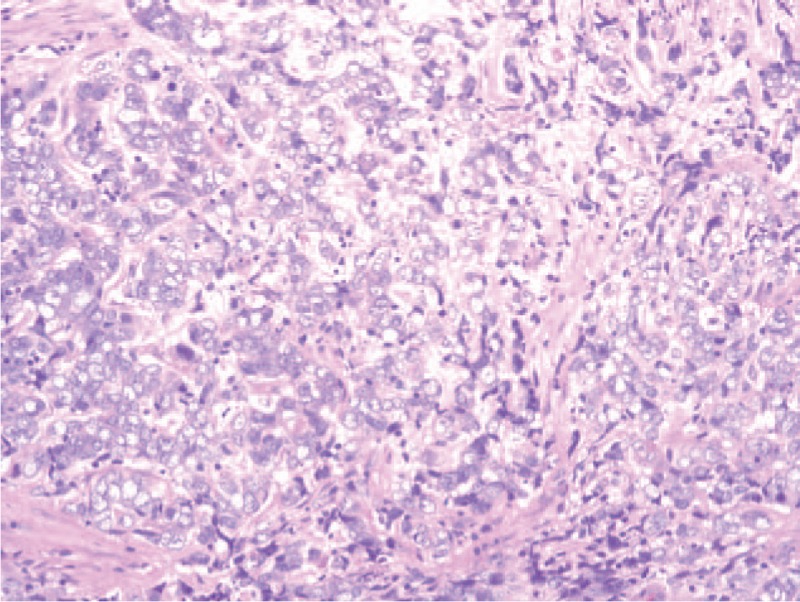
Histopathology of the surgical specimen showed undifferentiated carcinoma (Hematoxylin and eosin stain).
Figure 3.
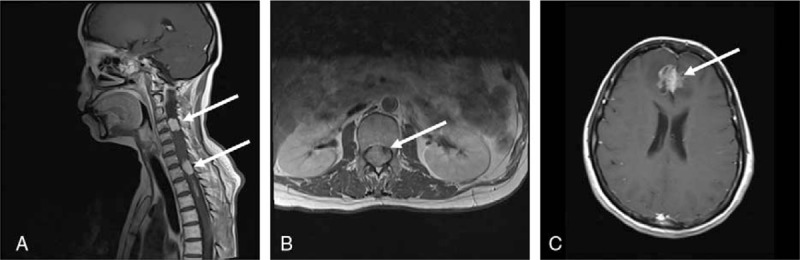
Sagittal and axial MR images of the cervical (A) and lumbar (B) spine showed extramedullary and intramedullary foci; and axial MR image of brain demonstrated frontal mass (C) (arrows).
Figure 4.
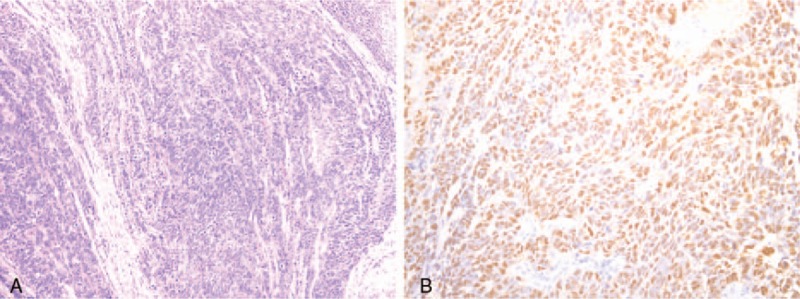
Histopathology of the surgical lumbus spinal specimen showed undifferentiated carcinoma (Hematoxylin and eosin stain) (A); and Epstein-Barr virus-encoded RNA (EBER) staining using in situ hybridization (ISH) was positive (B).
3.2. Brain metastasis
A 47-year-old man suffered from an 8-month headache and tinnitus in 2009. A local and systemic work-up were routinely done in the clinic. Physical examination showed 2 palpable lymph nodes in the left upper neck. Fiber optic endoscopy found a bulky neoplasm in the NP, and pathology of the biopsy specimen was confirmed nonkeratinizing, undifferentiated carcinoma. MRI scan revealed an irregularly-shaped tumor mainly located in the left lateral side of the NP, extending to left parapharyngeal space and pterygoid plate. Superiorly, it eroded the left petrous apex, clivus and also invaded into the left cavernous sinus. Furthermore, there was a retropharyngeal node enlargement and multiple lymph nodes metastases showed in the left neck with a maximum diameter of 3 cm on MRI scans. No distant lesions were found by systemic examination. Therefore, the patient was diagnosed with stage IV (T4N1M0) based on the criteria of 7th AJCC/UICC edition.
This patient received three cycles of neoadjuvant chemotherapy consisted of cisplatin and gemcitabine (GP) followed by radical IMRT combined with concurrent nimotuzumab weekly. There was partial regression of the NP tumor and metastatic lymph nodes at the completion of the treatment, so 1 month later, 2 cycles of adjuvant chemotherapy with the same GP regimen were offered.
In November 2010, 8 months after the end of the treatment, lung metastases were shown in routine chest computed tomography. Therefore, palliative chemotherapy with TPF regimen was given to control the distant lesions, and complete regression of lung metastases was achieved after 6 cycles of chemotherapy. In July 2012, he complained of continuous pain in the forehead, and brain MRI revealed an isolated lesion in the right frontal lobe. The patient was sent to the neurological surgery department and underwent intracranial neoplasm resection. The pathology of the specimen was squamous cell carcinoma, consistent with that obtained from the NP. The patient was assigned for systemic chemotherapy without local radiation. Unfortunately, nearly 7 months after surgery, a recurred nodule was found in the former intracranial site (Fig. 5). Palliative irradiation confined to brain metastatic lesion with total dose of 50 Gy in 25 fractions was given aiming to control the progression of the tumor. However, this patient also experienced multiple organs dissemination to bone and liver during the follow-up. Irrespective of receiving aggressive treatments such as chemotherapy and interventional therapy, he died 31 months after his brain metastasis had been diagnosed.
Figure 5.
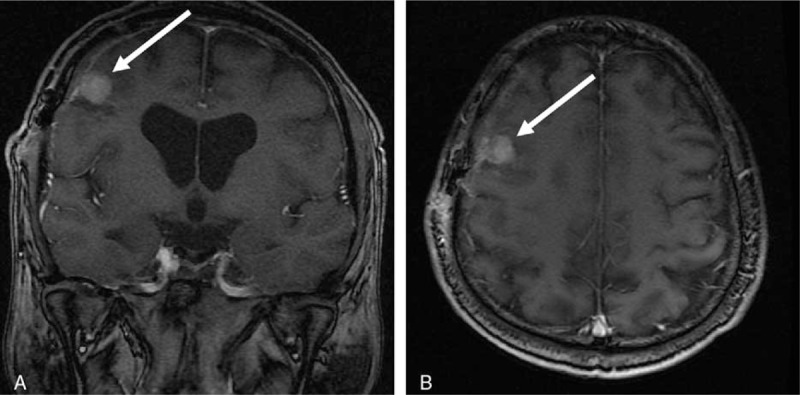
Coronal and axial MR images of brain showed a single frontal lobe lesion (A and B).
4. Discussion
Nasopharyngeal carcinoma is a malignancy with its predilection for both lymphatic and hematogenous spread. Continuous dissemination via lymphatic vessels to the cervical areas has been commonly reported in the locally advanced stage of disease. Meanwhile, tumor spread occurs hematogenously via the atrial or venous system frequently, mainly to the liver, lung, and bone. However, CNS metastasis from NPC is considered to be a conspicuous rarity, and this phenomenon is also a striking entity when the relevant literature is reviewed.
There are scarce cases of CNS metastases from NPC in a PubMed database in English. Our article encompasses both brain and spinal spread and also makes an overview on this issue. There are several reports only focusing on brain metastases in the literature. Khor et al[1] reported 3 of 99 patients experienced CNS dissemination from NPC, and described that a case with an isolated temporal lobe nodule that appeared 45 months after the end of the chemoradiotherapy. After systemic examination, there was no evidence of other sites of metastasis. Therefore, the brain metastasis was completely dissected by craniotomy, and whole-brain radiotherapy with total dose of 30 Gy in 10 fractions was given. Liaw et al[2] described a case of nasopharyngeal carcinoma with bilateral occipital lobes of brain metastases and diffuse bone involvement at present. The brain lesion was pathologically proven through the computed-tomographic guidance stereotactic biopsy. Because of the advanced lesions of this 69-year-old man, systemic chemotherapy and palliative radiotherapy were given aiming to relieve the symptoms. In 2002, Ngan et al[3] reported another case of occipital lobe metastases from NPC. A 33-year-old Chinese man was diagnosed with undifferentiated nasopharyngeal carcinoma of Ho stage IV (T2N3M0) disease in Hong Kong. The patient presented with lung involvement preceding brain metastasis 58 months from the end of definite chemoradiotherapy. A 3-cm cystic mass with surrounding cerebral edema was found in the left occipital lobe, and the craniotomy of macroscopic total excision was performed to exclude the primary glioma. The pathology using immunohistochemical staining confirmed NPC metastasis. Although multiple chemotherapy regimens were rendered, the patient succumbed 6 months from the diagnosis of brain metastasis because of the progression of lung lesions. Another case reported by Kaidar-Person et al[4] developed cervical lymph nodes, lung, and brain metastases after completing the initial radical chemoradiotherapy. Biopsies taken from lung and brain lesions were proven to be metastatic NPC. The patient received systemic chemotherapy and palliative radiation to the solitary occipital lobe nodule with total dose of 40 Gy. However, the patient suffered from his tumor deterioration, which mad him intolerance to antitumor therapies but only best supportive care was offered. The site of brain metastasis was most commonly seen in the occipital lobes as reported in the literature,[2–4] which was quite different from our series, where both patients developed the frontal lobe metastases.
Besides brain metastasis, tumor cells from nasopharyngeal carcinoma can also disseminate to the spine occasionally. These patients often have rapidly progressing neurological deficits, and spinal MR scan is helpful for diagnosis. To our knowledge, Morariu et al[6] first described a patient who had the intramedullary cervical cord metastasis from nasopharyngeal carcinoma in 1974. Three years after primary radiotherapy, this patient emerged with cervical spinal cord metastasis which was confirmed by immunohistochemical pathology, and the patient died 11 weeks after supportive care. Elango et al[7] reported a case with thoracic spinal cord metastasis who was treated with surgery and palliative radiotherapy, but the patient suffered from persist paraparesis. The ultimate survival time was not mentioned by the authors. Other articles described spinal cord metastases without histological confirmation. Most of these cases were also accompanied by other visceral organs involvement, such as lung and liver. High-dose steroid and radiotherapy were the main treatment rendered and the symptoms were lightened. However, the condition of survival for these patients was not reported in both studies either.[18,19] One NPC patient reported by Ngan et al[3] had lumbosacral spinal nerve roots involvement, and pathology of resected specimen was proven NPC metastases. Aiming to relieve the symptoms, palliative radiotherapy was given. After completing the surgery and second course radiotherapy for recurrent spine lesions, the patient almost survived 40 months from the diagnosis of CNS metastasis. With the accumulation and recognition of this entity, surgical operation with or without radiotherapy was suggested for these NPC patients with CNS metastases to relieve neurological impairment.
As described above, both patients in our institution developed brain metastases after completing the radical chemoradiotherapy. The sites of brain metastases were both in the frontal lobes, which were different from the most reported distant sites of brain, the occipital lobes, according to the previous literature. However, there is no reasonable explanation why circulating NPC cells favor to settle into the occipital lobe. To our knowledge it was the first finding that the brain metastasized lesion from NPC was located in the frontal lobes rather than the occipital ones. Brain metastases, usually accompanied by other visceral dissemination, might spread through blood stream, just as most authors deemed.[1–5] For one of our patients with brain metastasis and lung and liver failures, the hematogenous spread was the most possible assumption. Nevertheless, the other patient mentioned in our article who had multiple extramedullary and intramedullary dissemination besides brain metastasis, was more seldom in this scarce entity. For this female patient, different segments including cervical, thoracic, and lumbar spine were involved asynchronously. Spread through CSF was postulated as the most likely pathway in this patient. The reasons were just as what Ngan et al[3] clarified in their report. First, the initial primary NP tumor for this female patient extended the skull base and cavernous sinus. Tumor cells might dislodge through the disrupted dural barriers into the CSF. With the fluxion of the CSF, tumor cells might seed down to the spinal cord and proliferate to metastasized masses which could be seen on radiological images. The observation of Cvitkovic et al[20] supported the theory above. Second, the preferential sites of distant metastasis from NPC were visceral organs such as lung, bone, and liver. However, this female patient developed multiple CNS disseminations without distant metastases to these predilection sites in long follow-up, suggesting that the route of spreading was through the CSF rather than blood.
Both of our patients presented with CNS metastases treated with surgery and postoperative radiotherapy. The aim of surgery was not only to get a histological proof, but also to relieve the neurological compression. Best supportive care, surgery, palliative radiotherapy, and chemotherapy were the choices of these patients.[3–7,18,19,21] The optimal strategies were still controversial, and selection of treatment modalities should rely on many factors such as the patient performance, neurological symptoms, and oncologists’ preference. Aggressive local therapy such as surgery with or without radiation might relieve the neurological compression and prolong the survival time, especially for patients without extracranial metastases or those whose visceral metastases were well-controlled by chemotherapy.[3] In spite of the application of various local and systemic methods, the prospect of these patients diagnosed with CNS was dismay. Most of patients in the reports suffered from exacerbated neurological deficits and succumbed finally.[3,6] Although 2 patients in our series did have symptoms improvement after local dissection and RT, they died of disease progression afterwards, with survival duration of 20 and 31 months respectively after the advent of CNS metastases.
5. Conclusions
CNS metastases from NPC are considered to be quite rare, and patients usually suffer from neurological deficits. The most likely routes of tumor spread to CNS are postulated either by hematogenous dissemination or through CSF. Multiple distant organs involvement might accompany with CNS metastases. The optional treatment modalities include best supportive care, surgery and palliative chemoradiotherapy. Given aggressive local surgery and RT, patients might have the neurological symptoms improvement, and a hopefully prolonged survival time especially for those without other visceral organ involvement. However, prognosis of these patients is usually poor because of tumor progression ultimately.
Footnotes
Abbreviations: CNS = central nervous system, CSF = cerebral spinal fluid, CT = computed tomography, EBER = Epstein-Barr virus-encoded RNA, GP = cisplatin, gemcitabine, IMRT = intensity modulated radiation therapy, ISH = in situ hybridization, MRI = magnetic resonance imaging, NP = nasopharynx, NPC = nasopharyngeal carcinoma, TPF = cisplatin, docetaxel, 5-FU.
The authors declare no conflicts of interest.
References
- [1].Khor TH, Tan BC, Chua TE. Distant metastases in nasopharyneal carcinoma. Clin Radiol 1978;1:27–30. [DOI] [PubMed] [Google Scholar]
- [2].Liaw CC, Ho YS, NG KK, et al. Nasopharyngeal carcinoma with brain metastasis: a case report. J Neuro Oncol 1994;22:227–30. [DOI] [PubMed] [Google Scholar]
- [3].Ngan RK, Yiu HH, Cheng HK, et al. Central nervous system metastasis from nasopharyngeal carcinoma: a report of two patients and a review of the literature. Cancer 2002;94:398–405. [DOI] [PubMed] [Google Scholar]
- [4].Kaidar-Person O, Kuten J, Atrash F, et al. Brain metastasis of nasopharyngeal carcinoma: a case report and literature review. Case Rep Med 2012;2012:405917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Rafee S, Elamin YY, Cronin K, et al. A rare case of nasopharyngeal carcinoma with widespread CNS metastases. Ir Med J 2014;107:180–1. [PubMed] [Google Scholar]
- [6].Morariu MA, Serban M. Intramedullary cervical cord metastasis from a nasopharynx carcinoma. Eur Neurol 1974;11:317–22. [DOI] [PubMed] [Google Scholar]
- [7].Elango S, Kareem BA, Chandrasekaran S, et al. Nasopharyngeal carcinoma with spinal secondaries. J Laryngol Otol 1991;105:772–3. [DOI] [PubMed] [Google Scholar]
- [8].Kuo CL, Ho DM, Ho CY. Dural metastasis of nasopharyngeal carcinoma: rare, but worth considering. Singapore Med J 2014;55:e82–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Karunanithi S, Jain S, Shrma P, et al. Asymptomatic cauda equine metastasis in a patient with nasopharyngeal carcinoma: detection by (18)F-FDG PET/CT. Indian J Nucl Med 2014;29:177–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Kalayci M, Cagavi F, Gul S, et al. Intramedullary spinal cord metastases: diagnosis and treatment: an illustrated review. Acta Neurochir (Wien) 2004;146:1347–54. [DOI] [PubMed] [Google Scholar]
- [11].Zebrowski A, Wilson L, Lim A, et al. Intramedullary spinal cord metastases in breast cancer are associated with improved longer- term systemic control. Future Oncol 2010;6:1517–9. [DOI] [PubMed] [Google Scholar]
- [12].Lin HC, Hsu KH, Chang SN, et al. Increased survival with the combination of stereotactic radiosurgery and gefitinib for non-small cell lung cancer-brain metastasis patients: a nationwide study in Taiwan. Radiat Oncol 2015;10:127–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].de Bree R, Mehth DM, Snow GB, et al. Intracranial metastases in patients with squamous cell carcinoma of the head and neck. Otolaryngol Head Neck Surg 2001;124:217–22. [DOI] [PubMed] [Google Scholar]
- [14].Wu ZB, Xu S, Zhong CL, et al. Intramedullary conus medullaris metastasis from prostate carcinoma: a case report and review of the literature. Oncol Lett 2014;7:717–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Niu H, Zhou J, Maan H, et al. Treatment of leptomeningeal metastases in a patient with non-small cell lung cancer harboring EGFR T790 M mutation. Case Rep Oncol 2017;10:840–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Yuan P, Gao SL. Management of breast cancer brain metastases: focus on human epidermal growth factor receptor2-postive breast carcinoma. Chronic Dis Transl Med 2017;8:21–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Altundag K. Metastasis-acquired changes in clinically actionable genes in triple negative breast carcinoma patients with central nervous system metastases: focus on HER2 targeted therapies. J BUON 2017;22:1081. [PubMed] [Google Scholar]
- [18].Lii FN, Chen YM, Shu JM, et al. Metastatic nasopharyngeal carcinoma with epidural spinal cord compression: report of an unusual and catastrophic event. Chuang Hua I Hsueh Tsa Chih (Chin Med) 1995;55:195–8. [PubMed] [Google Scholar]
- [19].Lee C, Chan AT, Teo PM, et al. Intramedullary metastases in nasopharyngeal carcinoma. Oncol Forum 1999;3:7–9. [Google Scholar]
- [20].Cvitkovic E, Bachouchi M, Boussen H, et al. Leukemoid reaction, bone marrow invasion, fever of unknown origin, and metastatic pattern in the natural history of advanced undifferentiated carcinoma of nasopharyngeal type: a review of 255 consecutive cases. J Clin Oncol 1993;11:2434–42. [DOI] [PubMed] [Google Scholar]
- [21].Fakhry C, Bajaj G, Aygun N, et al. Long-term survival of a patient with leptomeningeal involvement by nasopharyngeal carcinoma after treatment with high-dose intravenous methotrexate. Head Neck 2012;34:296–300. [DOI] [PMC free article] [PubMed] [Google Scholar]


