Introduction
The differential diagnosis of cutaneous ulcers is broad, including infection, neoplasm, vascular disease, trauma, and inflammatory processes such as pyoderma gangrenosum. Nodulo-ulcerative lesions on an extremity are a common presentation of sporotrichosis, an infection with a saprophytic dimorphic fungus. A high index of suspicion for infection is required when chronic ulcers do not respond to treatment.
Case report
A 57-year-old woman with obesity and asthma presented with a 10-month history of 3 enlarging, painful ulcers on the left upper arm. Initially she noticed an erythematous nodule overlying the left elbow, attributed to an arthropod bite at a county fair. This nodule became exquisitely painful, with eventual ulceration and purulent drainage. Minocycline led to mild improvement initially, but the lesion then progressed. Incisional biopsy performed at an external institution found changes interpreted as an epidermoid cyst with granulomatous reaction. The ulceration continued to expand after biopsy, and 2 additional nodulo-ulcerative lesions developed proximally. The patient was treated with intravenous levofloxacin, ceftriaxone, and methylprednisolone for a presumed diagnosis of pyoderma gangrenosum with secondary infection. There was no improvement, and incision and drainage of the site led to further ulcer progression, prompting the patient to seek a second opinion. At presentation to our institution, the patient was taking penicillin, 500 mg 4 times daily, and prednisone, 60 mg daily, and was applying clobetasol ointment daily to wound edges. She complained of subjective fevers, chills, and fatigue. Physical examination of the left upper arm found 3 tender, irregularly shaped superficial ulcers in a linear distribution, each lesion 1.3 to 8.5 cm in diameter, with central granulation tissue and undermined edges (Fig 1). There were a few surrounding ill-defined smaller violaceous papules adjacent to the ulcers. There was no lymphadenopathy. Two 4-mm punch biopsy specimens were obtained from the border of the most proximal ulcerated lesion for routine histopathologic evaluation and tissue cultures for bacteria, fungi, and atypical mycobacteria.
Fig 1.

Cutaneous sporotrichosis mimicking pyoderma gangrenosum. At presentation, the left upper arm showed linearly arranged irregularly bordered, superficial ulcers with surrounding ill-defined erythematous-violaceous papules.
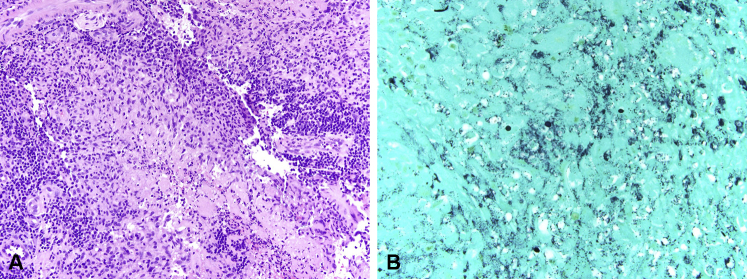
The biopsy findings showed diffuse suppurative and granulomatous inflammation in the dermis. Gomori methenamine silver stain for fungal elements highlighted rare fungal spores approximately 4 to 6 μm in size (Fig 2, A and B). Special stains for bacteria and acid-fast bacilli were negative. Deep tissue culture grew Sporothrix schenckii, confirming a diagnosis of cutaneous sporotrichosis.
Fig 2.
Cutaneous sporotrichosis, histopathologic evaluation. A, Small aggregates of neutrophils with karyorrhectic debris surrounded by granulomatous and lymphoplasmacellular inflammation. B, Round-to-oval fungal spores approximately 4 to 6 μm in size. (A, Hematoxylin-eosin stain; B, Gomori methenamine silver stain; original magnifications: A, ×200; B, ×600.)
Treatment with itraconazole, 200 mg/d orally, was initiated for 3 months. Slow improvement in lesion size, pain, and systemic symptoms was noted. Upon evaluation, the itraconazole level was found to be subtherapeutic. The dosage was increased to 200 mg orally twice daily. Our patient continues to improve.
Discussion
Sporotrichosis is a chronic granulomatous infection caused by the saprophytic dimorphic fungus S schenckii, present as a mold in environmental sources such as soil, plant debris, hay, and sphagnum moss.1, 2 It is uncommon in the United States, but sporotrichosis is endemic in tropical and subtropical regions and can be found worldwide. Sporotrichosis has been referred to as rose gardener's disease because of its prevalence on rose bushes. There have also been cases of zoonotic transmission, including cases transmitted through scratches and bites from infected cats, particularly in Brazil.3, 4 Traumatic inoculation or contamination of a preexisting wound by the mold form, which converts in the host to a yeast form, leads to cutaneous infection.2 Occupational and recreational exposure can occur through activities such as gardening, forestry, or caring for infected animals.4 In our patient's case, there was no history of activities such as gardening nor any certain trauma.
Clinically, sporotrichosis typically manifests as a lymphocutaneous eruption, beginning as a papule or nodule that develops often within days at the site of inoculation. Progressive nodulo-ulcerative lesions following the underlying lymphatics then arise proximally, as illustrated by our patient. Often, an affected patient can identify the source of inoculation. Extracutaneous involvement is rare but can occur. The lungs may become involved through inhalation of organisms, and joints and rarely other organs may become infected through hematogenous spread.2 Disseminated involvement has been described, particularly in the setting of HIV5 and also in the setting of iatrogenic immunosuppression.6
The differential diagnosis of cutaneous ulcers is broad, including infection, neoplasm, vascular disease, trauma, and inflammatory processes such as pyoderma gangrenosum. A high level of clinical suspicion for infection is required when treating any ulcer, particularly one that fails to respond to initial treatment approaches. A sporotrichoid or progressive distal-to-proximal distribution of subcutaneous nodules suggests lymphangitic spread and should increase the clinical suspicion for an infectious etiology.7 Appropriate evaluation includes biopsies for both histopathologic evaluation and tissue culture. Histologic features are fairly nonspecific although typically suggest infection with a suppurative or granulomatous infiltrate. The organisms may be difficult to identify in tissue and are often very few in number. Oval or elongated cigar-shaped yeast cells, 2 to 6 μm in diameter, are characteristic.2 In immunosuppressed patients, organisms may be more numerous. In our patient's case, there may have been an element of iatrogenic immunosuppression given the initial presumptive diagnosis and treatment for pyoderma gangrenosum.8 Tissue culture on Sabouraud dextrose agar is the gold standard for diagnosis9; growth typically occurs within 5 days but can take weeks, and colonies are cream colored and can darken over time.
Timely treatment is essential to prevent chronicity and morbidity. The treatment of choice is itraconazole, 200 mg/d orally, typically for 3 to 6 months. Treatment should be continued for 2 to 4 weeks after the lesions have healed. This regimen leads to resolution in most lymphocutaneous cases.10
Cutaneous sporotrichosis should be considered in the differential diagnosis of cutaneous ulcers, particularly if unresponsive to first-line therapies. Biopsy for tissue culture is the gold standard for diagnosis. Accurate and timely diagnosis will spare patient morbidity, including inappropriate immunosuppression.
Acknowledgments
The authors thank Harrold Carter for his clinical photography expertise.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Ramos-e-Silva M., Vasconcelos C., Carneiro S., Cestari T. Sporotrichosis. Clin Dermatol. 2007;25:181–187. doi: 10.1016/j.clindermatol.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 2.Kauffman C.A. Endemic mycoses: blastomycosis, histoplasmosis, and sporotrichosis. Infect Dis Clin North Am. 2006;20:645–662. doi: 10.1016/j.idc.2006.07.002. vii. [DOI] [PubMed] [Google Scholar]
- 3.Schubach A., Barros M.B., Wanke B. Epidemic sporotrichosis. Curr Opin Infect Dis. 2008;21:129–133. doi: 10.1097/QCO.0b013e3282f44c52. [DOI] [PubMed] [Google Scholar]
- 4.Chakrabarti A., Bonifaz A., Gutierrez-Galhardo M.C., Mochizuki T., Li S. Global epidemiology of sporotrichosis. Med Mycol. 2015;53:3–14. doi: 10.1093/mmy/myu062. [DOI] [PubMed] [Google Scholar]
- 5.al-Tawfiq J.A., Wools K.K. Disseminated sporotrichosis and Sporothrix schenckii fungemia as the initial presentation of human immunodeficiency virus infection. Clin Infect Dis. 1998;26:1403–1406. doi: 10.1086/516356. [DOI] [PubMed] [Google Scholar]
- 6.Gottlieb G.S., Lesser C.F., Holmes K.K., Wald A. Disseminated sporotrichosis associated with treatment with immunosuppressants and tumor necrosis factor-alpha antagonists. Clin Infect Dis. 2003;37:838–840. doi: 10.1086/377235. [DOI] [PubMed] [Google Scholar]
- 7.Tobin E.H., Jih W.W. Sporotrichoid lymphocutaneous infections: etiology, diagnosis and therapy. Am Fam Physician. 2001;63:326–332. [PubMed] [Google Scholar]
- 8.Byrd D.R., El-Azhary R.A., Gibson L.E., Roberts G.D. Sporotrichosis masquerading as pyoderma gangrenosum: case report and review of 19 cases of sporotrichosis. J Eur Acad Dermatol Venereol. 2001;15:581–584. doi: 10.1046/j.1468-3083.2001.00363.x. [DOI] [PubMed] [Google Scholar]
- 9.Barros M.B., de Almeida Paes R., Schubach A.O. Sporothrix schenckii and Sporotrichosis. Clin Microbiol Rev. 2011;24:633–654. doi: 10.1128/CMR.00007-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kauffman C.A., Bustamante B., Chapman S.W., Pappas P.G. Infectious Diseases Society of, A. Clinical practice guidelines for the management of sporotrichosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis. 2007;45:1255–1265. doi: 10.1086/522765. [DOI] [PubMed] [Google Scholar]