INTRODUCTION
The U.S. hospital industry is currently engaged in a series of efforts to pursue quality, variously measured by the patient’s experience of care, physician adherence to processes of care, or clinical outcomes (Berwick, Nolan, & Whittington, 2008). The majority of efforts for improving patient safety involve reducing active failures by clinicians, through the systematic implementation of clinical guidelines, checklists, electronic health records, financial incentives, and disciplinary measures. Typically, each of these measures invites greater managerial oversight. Patient safety has improved in important ways, but progress has been much slower than expected (Makary & Daniel, 2016). The increased management layer required to pursue various patient safety initiatives financially contrains human resources, resulting in fewer clinicans; after some initial improvement, the effects on quality of care and patient safety are small and diminishing.
A different approach for improving quality of care and patient safety builds on theories of human capital that emphasize the productive capacities of clinicians that are embedded in their education and experience (Sweetland, 1996). Innovation that transforms organizational work place design can release embedded human capital. Thus, professionals can exert more autonomy and exercise clinical judgment to effectively implement evidence-based practice to have greater impact on patient safety.
One such organizational innovation in work environment redesign is Magnet hospital recognition through the American Nurses Credentialing Center (ANCC). The Magnet designation recognizes hospitals with excellent nurse work environments and improved patient care — as reflected in clinical workforce satisfaction, patient satisfaction, and better patient outcomes. Importantly, there is research that suggests that Magnet is not only a signal of high quality, but that it can be a transformative intervention for improving care quality and patient safety. Hospitals that achieve Magnet recognition appear to improve in terms of nurse outcomes (i.e. job satisfaction, burnout, intent to leave), patient outcomes (i.e., mortality, failure-to-rescue), and performance measures (i.e., value-based purchasing), more significantly than other hospitals not on the same journey (Kutney-Lee et al., 2015; Lasater, Germack, Small, & McHugh, 2017; McHugh et al., 2013). Thus, Magnet adoption may actively contribute to the achievement of quality goals. At present, only about 10% or 400 U.S. hospitals have obtained Magnet recognition.
Given the potential positive impact of Magnet status on quality, it is important to understand the conditions that foster adoption and diffusion. Prior research has identified a number of organizational characteristics (e.g., large, teaching facilities) and market forces (e.g., emulation of others in the local market) that promote adoption. However, there has been little research and no evidence regarding Magnet adoption and diffusion among hospital systems (Abraham, Jerome-D’Emilia, & Begun, 2011). This is remarkable, given the continuing spread of systems, which now account for roughly 60 percent of all community hospitals, as well as the growing concentration of local hospital markets into a smaller number of larger systems (Brown, Werling, Walker, Burgdorfer, & Shields, 2012; Dafny, 2014). Part of the reason may be that prior research has found few positive or consistent effects of hospital systems on quality (Gaynor, Kleiner, & Vogt, 2015; Henke et al., 2016; Tsai & Jha, 2014). However, research on the impact of hospital systems has typically relied on simplistic binary indicators of membership. It may be the case that some types of hospital systems (e.g., centralized structures) are better poised to improve quality and cost performance through innovation, including their differential adoption of Magnet status (Rosko, Proenca, Zinn, & Bazzoli, 2007).
This paper examines Magnet adoption in hospital systems. We conceptualize innovation in line with definitions in the literature that characterize innovation, not as something new per se, but as something that is new to the unit considering adoption (Zaltman, Duncan, & Holbek, 1973). Thus, although Magnet is a concept that has been around, it is potentially new to a large number of institutions. Our work advances the literature in several novel ways. First, it examines whether hospital system structure (e.g., centralized versus decentralized), rather than system membership, impacts adoption. Second, it compares the hierarchical effect exerted by emulating other hospitals in the same system that have adopted with the market effect of emulating competitor hospitals that have adopted. Third, it compares the effect of local market emulation (adoption) with the effect exerted by adoption in more distant markets (i.e., by hospitals both within and outside the same system).
In contrast to prior research (Abraham et al., 2011), our study takes a longitudinal view and models Magnet uptake among hospital system affiliates over time to capture how Magnet adoption differs both within and across systems. The paper suggests that Magnet adoption is associated with (a) centralized hospital systems (structural effect), (b) emulation of other hospitals in the same system that have adopted (hierarchy effect of common governance), (c) emulation of other local hospitals that have adopted (market effect of competitors), and (d) proximity to other adopters in the local market rather than in more distant markets (center versus periphery effect). Our results thus speak to the relative importance of structure, hierarchy, and market influences on hospital innovation and quality improvement such as Magnet recognition. Such efforts have the potential to have a bigger effect on quality than narrow clinical interventions that are likely contingent on the underlying organizational quality and professional clinical human capital that Magnet aims to improve. The resulting data patterns are useful to nursing leaders, health care administrators, and policymakers interested in the diffusion of organization-wide best practices related to the health care work environment and quality care delivery.
CONCEPTUAL BACKGROUND
DiMaggio and Powell (1983) have suggested that organizations increasingly become isomorphic; i.e., they become more similar to one another. Although one form of isomorphism is based on competition, they posit that the more common form is normative (institutional) pressure exerted through professional networks, particularly in the face of uncertainty. We argue that this is largely the case for hospitals as they seek legitimacy and power. Prior research has analyzed Magnet hospital status from an innovation adoption lens (Rye & Kimberly, 2007). For example, Abraham, Jerome-D’Emilia, and Begun (2011) analyzed adoption as a function of organizational characteristics (size, teaching status), slack resources (low percent Medicaid inpatient days), organizational connectedness (system member, presence of affiliated members in local market), market competition (hospital concentration), nursing labor supply, and imitation (adoption by others in the local metro area). Adoption was associated in their cross-sectional design with size, teaching status, slack, nursing supply, and presence of other Magnet hospitals (reflecting both competition and imitation). Adoption was associated with neither system membership nor the presence of other hospitals in the market from the same system. What the researchers did not examine was the presence of other hospitals in the market from the same system that had already adopted Magnet status, the structure of the system to which these hospitals belonged, the presence of competitor hospitals outside the market that had already adopted, and the diffusion over time. It is in this institutional context that we seek to understand the process of Magnet adoption among hospitals that are part of systems.
One source of institutional isomorphism is normative pressure arising out of professionalization as professions seek to advance and legitimize their autonomy (DiMaggio & Powell, 1983). The Magnet hospital concept originated as a means of identifying organizations that had a reputation for successful recruitment and retention of a highly qualified nursing workforce. In the early 1990s, the American Nurses Credentialing Center (ANCC) formalized the Magnet designation, which became a voluntary program. The pursuit of Magnet recognition was driven largely by nurse leaders, and recognized and rewarded by the profession. We expect that such normative pressures would be greater for hospitals that are part of systems and Magnet status would be pursued more in hospital systems where other local affiliates have already adopted as an effort to standardize nursing care and the professionalization of nursing within the system.
Hypothesis 1: Hospitals are likely to adopt Magnet status when other affiliates of the same system in the local market have already adopted.
Researchers have argued that the structure of hospital systems is a good summary indicator of their strategic and structural differences, and their ability to deliver cost-effective care (Shortell, Bazzoli, Dubbs, & Kralovec, 2000). There is recent evidence that the type of hospital system makes a difference for system behavior and performance. For example, while most of the literature shows that systems do not out-perform freestanding hospitals in terms of their operating costs, there is some evidence that smaller and more centralized systems have lower costs (Burns et al., 2015). This evidence suggests that hospitals in the most centralized systems had 3.3% lower costs, while hospitals in moderately centralized or decentralized systems had 1.1% higher costs. Such disparate effects may cancel themselves out in studies that fail to distinguish hospital system structures.
Prior research has examined variations in quality across hospitals within systems of differing levels of centralization (Hines & Joshi, 2008). The researchers found that centralized systems reported significantly higher Centers for Medicare and Medicaid Services (CMS) quality scores in one of four clinical conditions (pneumonia) compared to moderately centralized and decentralized/independent systems.
These findings are quite relevant to adoption of Magnet status. By definition, more centralized systems are able to centralize their product and service offerings through standardization and programmatic rationalization (Muller & Kruse, 2015). We expect that, since Magnet is driven by nursing leadership and a strong culture of professional nursing, institutional isomorphism is likely to be greater among more centralized systems. They are also better positioned to gain scale economies from local branding and marketing campaigns, due to their smaller size and clustering in one local market. Since the system’s brand is usually built around a core academic medical center (AMC) hub, systems often feel pressure to make investments in local affiliate non-teaching hospitals to raise them to the same quality level and brand expectations. In the case of the University of Pennsylvania Health System, for example, the system, driven by strong nursing leadership, invested in the latter hospitals to achieve the same Magnet status as the AMC hub (Muller & Kruse, 2015). Locally-based systems may therefore be more likely to roll out Magnet status to their members; i.e., after achieving Magnet status in one hospital, other local affiliates may be encouraged to emulate their example. This reflects increasingly coherent nursing leadership aiming to achieve a system-wide culture of professional nursing. Centralized systems are more likely to enjoy conscious support by the system’s administration (hierarchy effect) to pursue Magnet recognition as an exercise of centralized decision-making and governance (Alexander, Lee, & Bazzoli, 2003), for example, to achieve some branding and promotion economies (Besanko, Dranove, Shanley, & Schaefer, 2009).
Hypothesis 2: Hospitals in centralized hospital systems are likely to exhibit higher levels of Magnet adoption than hospitals in moderately centralized or decentralized systems when other local affiliates have already adopted.
In addition to the above hierarchical effects of common governance and system-enhancing efficiencies, Magnet adoption may be prompted by market competition via the emulation of local competitors. Due to reimbursement pressures and calls for “value-based care” from public and private payers, hospital systems face pressures to lower costs, achieve efficiencies, and demonstrate economies where they can. The research literature suggests few economies of scale in hospital systems, particularly in larger and more geographically dispersed systems (Burns et al., 2015; Gaynor et al., 2015). Hospital executives have publicly stated that scale economies are harder to achieve in clinical services provided by physicians, but are more available in administrative and nursing services. As the Magnet concept evolved and the empirical foundation grew, Magnet has become an indicator of professional nursing excellence that signifies not just a good place for nurses to work, but one consistently linked with positive patient outcomes. Recent evidence suggests that Magnet can be a good value investment for the bottom-line (Jayawardhana, Welton, & Lindrooth, 2014; Lasater et al., 2017).
There is considerable prior research that the presence of other adopters can promote the imitation of organizational innovations through either normative or competitive pressures (Rye & Kimberly, 2007). Prior adoption can either make it more legitimate for hospitals and their nursing staff to seek Magnet recognition, or increase pressure to compete for nursing personnel through such recognition. Thus, we anticipate that Magnet adoption is likely, not only when affiliated hospitals in the same system have already adopted, but also when competing, non-affiliated hospitals have adopted. This emulation effect may be heightened when dominant hospitals are not the first to adopt, but observe adoption by competitors. Such organizations have been observed to be “fast followers” as part of a diffusion process that extends from the periphery to the center in the local market (Becker, 1970; Zaltman et al., 1973).
Hypothesis 3: Hospitals are more likely to adopt Magnet when local, non-system competitors have already adopted. This effect may be especially pronounced among dominant hospitals in the local market.
Finally, the hierarchy and market effects described above are likely to be stronger in local rather than distant markets. With regard to hierarchy effects, systems report that standardization and system rationalization efforts are more difficult to achieve when their hospital operations are more geographically dispersed rather than concentrated. With regard to market effects, the adage that “all healthcare is local” may be an important consideration. Adoption of an innovation like Magnet, driven by nursing leadership, is likely influenced more by normative rather than economic pressures. We might therefore expect diffusion and emulation forces to be stronger in local rather than non-local contexts as hospitals sharing the same local area have nurse leaders and frontline staff influenced and involved in the same professional networks. This may be less true for centralized systems than for less centralized systems; at the same time, however, centralized systems tend to be more geographically concentrated (Burns, Wholey, McCullough, Kralovec, & Muller, 2012). Opportunities for standardization likely diminish as systems grow larger in size and geographic spread (Burns et al., 2015).
Hypothesis 4: Hospitals are more likely to adopt Magnet status if there has been adoption by non-local affiliates but this effect will not be as large as if there has been prior adoption by local affiliates. The effect of prior adoption by distant hospitals may be stronger in centralized systems.
METHODS
Data and Sample
We use the annual surveys from the American Hospital Association (AHA) spanning 1998 – 2012 and restrict our observations to non-federal adult acute-care service hospitals that are in systems. As our study is longitudinal in nature, we drop hospitals that are present for three waves or less (<1% of the data) due to their limited analytic information. Although we use data from freestanding hospitals not in systems to create variables describing regional environments, our modeling of outcomes is limited to hospitals reporting system membership. A hospital system is a horizontally integrated organization with ownership over multiple facilities; however, system “affiliates” — institutions within the same system— may be located geographically close or far from any given hospital as systems can span multiple markets and state boundaries.
Variables
Outcome
Our primary outcome of interest was a binary variable for Magnet recognition for each individual hospital that belonged to a system in each year.
Explanatory Variables
Our goal was to understand the likelihood of a system hospital being a Magnet hospital based on a variety of local environmental conditions, Magnet adoption patterns among system affiliates and non-affiliates in the local area, as well as Magnet adoption patterns among system affiliates and non-affiliates in markets that are geographically distant from the reference hospital. First, we created measures of Magnet adoption behavior near the reference hospital; i.e., in the same geographic area. We used the Hospital Referral Region (HRR) to define the geographic area and then created the following explanatory variables to examine their relationship to Magnet adoption among system hospitals: (a) prior adoption by an affiliate within the same HRR; (b) prior adoption by a non-affiliate within the same HRR; and (c) prior adoption by a non-affiliate within the same HRR, but limited to evaluating the outcome for the “dominant” market leading hospital. We created an alternative version of the variable capturing prior adoption of non-affiliates, but used the state as the relevant geographic market. Next, we created an explanatory variable to characterize the prior adoption behaviors of distant system affiliates; i.e., outside the HRR. For each of our explanatory variables, we also constructed a binary measure indicating at least 5% of system affiliates in the HRR having Magnet recognition, and then likewise for the proportion outside the HRR. Of note, models using the continuous measure of system affiliates’ Magnet adoption as well as alternative cutoffs (e.g., other than the 5% adoption threshold) did not qualitatively change our pattern of results.
Hospital characteristics
We created time-varying indicators for several hospital characteristics. They include the number of competitors within the HRR, the HRR’s Herfindahl-Hirschman Index (HHI) based on bed counts, a binary “dominant market leader” indicator for the hospital having at least a 25% share of all beds in the HRR, a binary indicator of teaching status if the hospital had physician residents and fellows or not, a binary indicator for non-profit ownership status, and a binary indicator for being a hospital with advanced treatment technology. The latter is equal to one when a hospital reports being able to perform open-heart surgery, organ transplantation, or both. Additionally, we had two covariates (both binary) to capture if the hospital just joined a system in a given year or if the hospital changed systems in a given year.
Last, we (separately) examined whether the relationships between our primary explanatory variables and Magnet adoption were conditional on the type of system a hospital belonged to based on the taxonomy developed by Bazzoli and colleagues (1999) that organizes systems vis-a-vis differentiation, centralization, and integration. The original approach identified whether systems fall into one of five clusters. A Centralized Health System is one that centrally organizes individual hospital service, physician arrangements, and insurance products. These systems offer a moderate number of different products and services. A Centralized Physician/Insurance Health System is one with highly centralized physician arrangements and insurance products, but relatively decentralized hospital services. Overall, the number of different products/services offered across the system is moderate, but individual hospitals exercise independent discretion over the services they provide. A Moderately Centralized Health System is one with both centralized and decentralized hospital services, physician arrangements, and insurance products. Such systems offer a moderate number of different products/services. A Decentralized Health System is highly decentralized with respect to hospital services, physician arrangements, and insurance product development with very little overarching structure for coordination. Finally, an Independent Hospital System represents a very decentralized, loosely affiliated group of hospitals with limited differentiation.
Given the somewhat random fluctuation over time in the cluster in which hospitals get classified, we followed the example of Burns and colleagues (2012) and created a three-category variable where cluster codes 1 or 2 (Centralized Health System, Centralized Physician/Insurance Health System) are deemed “centralized cluster;” systems identified as cluster code 3 (Moderately Centralized Health System) are “moderately centralized cluster;” and systems with cluster codes of 4 or 5 (Decentralized Health System, Independent Hospital System) as “decentralized cluster.” This allowed us to examine whether any relationship between our explanatory variables and an individual hospital’s likelihood of becoming a Magnet varied by system type.
Analysis
We estimated a series of individual-level hospital fixed-effects regressions to reflect changes in a given system hospital’s Magnet recognition status over time. Fixed-effects models are commonly used with panel data and are often referred to as the “within” estimator since they focus on variation within an observational unit over the study period. The method also controls for all time-invariant or “fixed” differences across individual hospitals to reduce bias in the subsequent estimates. Each model that we estimated included the additional covariates described previously. Lastly, we estimated these models, with an interaction between our primary explanatory variables (separately) and the three-category system type indicator.
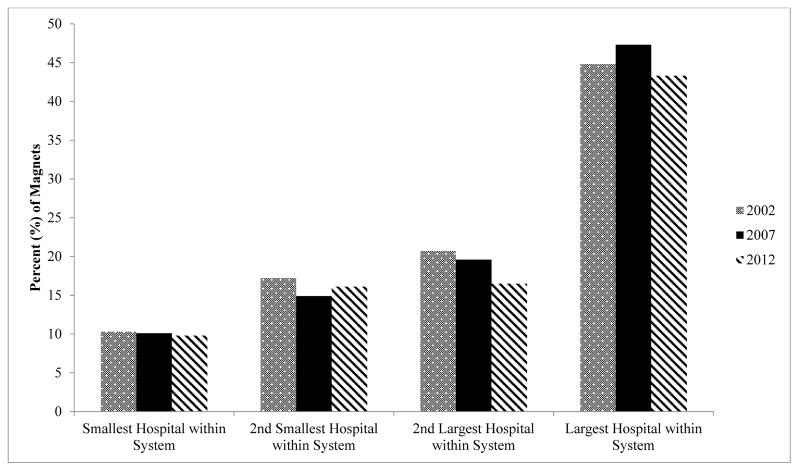
Following our fixed-effects regression analyses, we performed a final descriptive exercise related to hospital size within its system. Research focused on hospital technology adoption has documented the influence of size (Furukawa, Raghu, Spaulding, & Vinze, 2008; Ladapo, Horwitz, Weinstein, Gazelle, & Cutler, 2009; Wang, Wan, Burke, Bazzoli, & Lin, 2005), and Abraham, Jerome-D’Emilia, and Begun (2011) similarly showed that hospitals with more beds are more likely to be Magnets in the cross-section. For these reasons, we ranked all hospitals within a system in a given year by bed count. We then examined the allocation of Magnets within systems in 2002, 2007, and 2012 to determine the tendency of hospital systems to pursue Magnet recognition among particular hospitals (e.g., their largest facilities) at different points in time.
FINDINGS
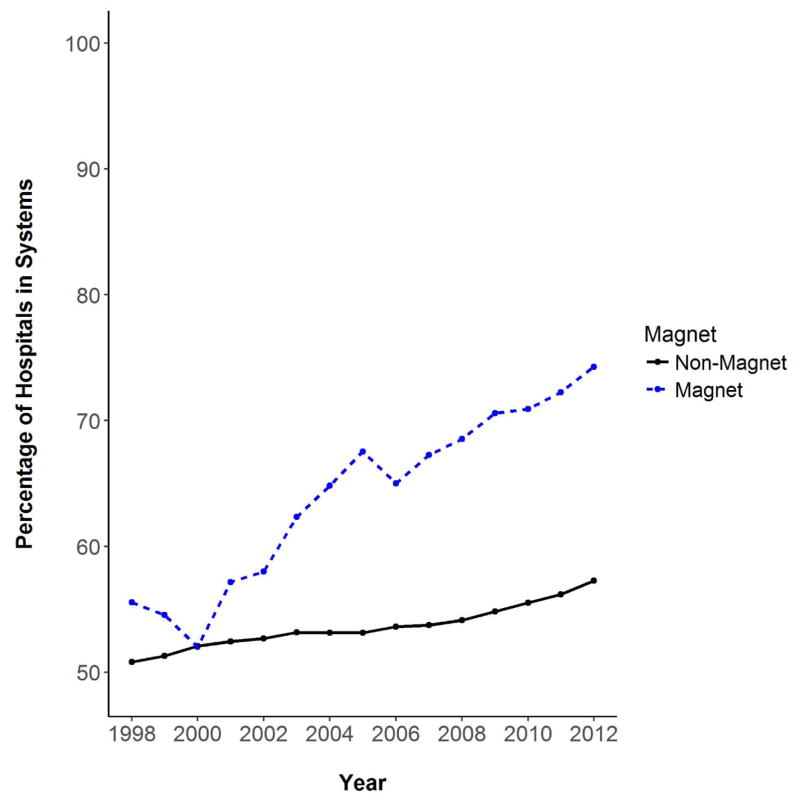
Figure 1 captures the percent of existing Magnet and non-Magnet hospitals that were affiliated with a health care system from 1998–2012. We know that the number of Magnets is trending upward during this period (Richards, Lasater, & McHugh, in press), but Figure 1 clearly shows that the proportion belonging to a hospital system is as well. By 2012, nearly 75% of all non-federal, adult acute-care Magnet hospitals were hospital system affiliates compared to just over 50% in the early 2000s.
Figure 1.
Percent of Magnet and non-Magnet hospitals that are part of a hospital system 1998 – 2012
Source: AHA data, restricting to adult acute care facilities that are not government owned. Figure only includes Magnet hospitals present in a given year
Overall, just over 70% of system hospitals were non-teaching and nearly 75% were nonprofit (Table 1). By 2012, almost 10% of system hospitals that we observed had achieved Magnet recognition. Additionally, 40% of system hospitals were the ‘market leader’ within their respective HRR at baseline.
Table 1.
Characteristics of system hospitals 1998 – 2012
| 1998 (N=2,417) | 2007 (N=2,630) | 2012 (N=2,606) | |
|---|---|---|---|
| System hospitals achieving Magnet recognition | 0.2% | 5.6% | 9.8% |
| Baseline system hospital characteristics | |||
| Non-teaching | 70% | 71% | 69% |
| Non-profit | 75% | 73% | 75% |
| High tech status | 25% | 28% | 29%% |
| No. of competitors in hospital referral region | 18% | 18% | 17.7 |
| Market leader in hospital referral region | 42% | 40% | 40.9% |
Sample restricted to AHA acute care hospitals that are not government owned and are part of a hospital system. Baseline characteristics reflect the first year of data a system hospital provided. Market leader is defined as a hospital with at least 25% market share within a given hospital referral region-year (based off of HHI calculation using total number of beds)
Table 2 shows results of our regression analyses. Each row represents a separate model capturing within-hospital changes in Magnet recognition for system hospitals over time. The key explanatory variables were indicators of: 1) prior adoption by system affiliates within the same HRR; 2) prior adoption by at least 5% of system affiliates within the same HRR; 3) prior adoption by non-affiliates within the same HRR; 4) prior adoption by a non-affiliate within the same HRR, but limited to effects on market leader Magnet adoption; 5) prior adoption by at least 5% of non-affiliates within the same HRR; 6) prior adoption by non-affiliates within the same state; 7) prior adoption by at least 5% of non-affiliates within the same state; 8) prior adoption by system affiliates outside the HRR; and 9) prior adoption by at least 5% of affiliates outside the HRR. All models include hospital-level, time-varying controls and dummy variables for year.
Table 2.
Association between Magnet adoption and prior adoption by hospitals inside and outside the same market area
| Hospital Fixed Effects Coef. (SE) | |
|---|---|
| Prior adoption by affiliates within the same HRR | |
|
| |
| Prior adoption by affiliate | 0.074 (0.015)*** |
| Prior adoption by at least 5% of affiliates | 0.074 (0.014)*** |
|
| |
| Prior adoption by non-affiliates within the same HRR | |
|
| |
| Prior adoption by a non-affiliate | 0.027 (0.006)*** |
| Prior adoption by a non-affiliate on the market leader | 0.040 (0.006)*** |
| Prior adoption by at least 5% of non-affiliates | 0.041(0.008)*** |
|
| |
| Adoption by non-affiliates within the same state | |
|
| |
| Prior adoption by a non-affiliate within the same state | −0.007 (0.005) |
| Prior adoption by at least 5% of non-affiliates within the same state | 0.031 (0.006)*** |
|
| |
| Adoption by affiliates outside the HRR | |
|
| |
| Prior adoption by affiliate outside the HRR | −0.0005 (0.004) |
| Prior adoption by at least 5% of affiliates outside the HRR | 0.035 (0.008)*** |
P value at 0.01
P value at 0.05
P value at 0.10, robust standard errors in parentheses.
Sample restricted to acute care hospitals that are not government owned and are part of a hospital system. All models include dummy variables for year and hospital covariates including number of competitors within the HRR, the HRR’s Herfindahl-Hirschman Index (HHI), a binary indicator for the hospital being the “market leader”), teaching status, high technology status, and non-profit ownership status.
The first row suggests that prior adoption by an affiliate within the same HRR was associated with a 7.4 percentage point increase in the likelihood of a given system hospital becoming a Magnet. The effect was similar (7.4%) if at least 5% of affiliates had previously been Magnet recognized. Next, we found that prior adoption by a non-affiliate within the same HRR was associated with a given system hospital being Magnet recognized; however, the effect was smaller (2.7%) than was found for local affiliates. When we limited our attention to evaluate if Magnet adoption by a local non-affiliate hospital had a significant impact on market leaders, the likelihood of adoption by market leaders was 4.0 percentage points greater. If there was prior adoption by at least 5% of local non-affiliates, then the likelihood of a given system hospital adopting was 4.1 percentage points higher. When we expanded the geographic area to look at the effect of prior adoption by a non-affiliate within the state (vs. the HRR), a single non-affiliate hospital’s prior adoption was not associated with an increased likelihood of a system hospital adopting. However, if at least 5% of non-affiliates within the state had previously adopted Magnet, then the likelihood of a system hospital adopting was 3.1 percentage points greater. Next, we evaluated the influence of prior adoption by distant system affiliates outside the HRR. We found no relationship between distant affiliates’ prior adoption and the likelihood of a given system hospital adopting, unless a critical mass of distant affiliates (at least 5%) had previously become Magnets.
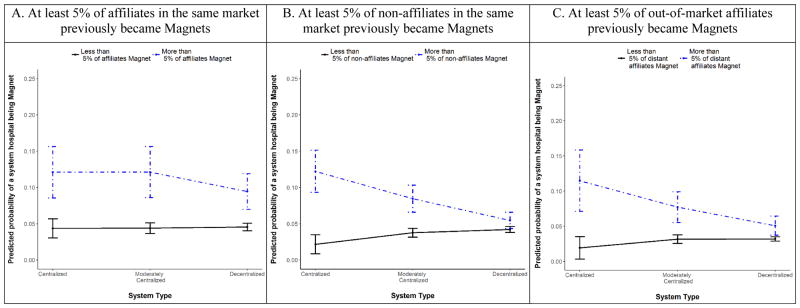
We also estimated our models with an interaction term to examine whether our findings were conditional upon the type of system (centralized, moderately centralized, or decentralized). Figure 2A shows the different predicted probabilities of a given system hospital, by system type (centralized, moderately centralized, or decentralized), becoming a Magnet if at least 5% of affiliates in the same market (i.e., within the hospital’s HRR) were Magnets. We can see that hospitals in centralized and moderately centralized systems located in HRRs where at least 5% of affiliates previously adopted Magnet, had the highest likelihood of adopting Magnet themselves (12%).
Figure 2.
Probability of a system hospital adopting Magnet by system type if:
A. At least 5% of affiliates in the same market previously became Magnets
B. At least 5% of non-affiliates in the same market previously became Magnets
C. At least 5% of out-of-market affiliates previously became Magnets
Note: Predicted probabilities based on model that includes dummy variables for year and hospital covariates for number of competitors within the HRR, the HRR’s Herfindahl-Hirschman Index (HHI), a binary indicator for the hospital being the “market leader”), teaching status, high technology status, and non-profit ownership status.
Figure 2B shows the predicted probability of a given hospital becoming a Magnet if at least 5% of non-affiliates in the same market were Magnets, by system type. Again, the results suggest that local concentration of Magnet recognition is likely to prompt Magnet adoption most among hospitals that are part of centralized systems. Figure 2C shows the predicted probability of a given hospital becoming a Magnet if at least 5% of affiliates outside its market previously became Magnets, by system type. The results suggest that a hospital is more likely to be prompted to become a Magnet by prior adoption among out-of-market affiliates if that hospital belongs to a more centralized system.
Figure 3 presents a final descriptive exploration of the relative size of a hospital that has achieved Magnet recognition. Clearly, the largest hospitals within a system tend to be Magnets, and the likelihood of being a Magnet declined with a hospital’s within-system size ranking. The pattern was nearly constant over our study period.
Figure 3.
Within-system hospital size among existing Magnets in three cross-sectional survey years
Source: AHA data, restricting to adult acute care facilities that are not government owned. Figure only includes Magnet hospitals present in a given year. Note: Ranking of hospitals is done by total number of beds. The ranking spans all affiliate hospitals in the given year. There are 29, 148, and 254 Magnet hospitals within integrated hospital systems for the respective AHA survey years
DISCUSSION
Abraham, Jerome-D’Emilia, and Begun (2011) found that system affiliation appeared unrelated to Magnet adoption and concluded that hospital systems have a weaker affinity toward the Magnet program. Yet, our results offer a more nuanced view. Consistent with Hypothesis 1, there is evidence for hierarchical effects in local markets: the presence of other local affiliates with Magnet status promotes Magnet adoption among members of the same hospital system. Consistent with Hypothesis 2, these hierarchical effects are more pronounced in more centralized systems. Third, consistent with Hypothesis 3, the local market is important—prior adoption activity by non-affiliates within the market significantly influenced the likelihood of Magnet adoption. However, system member (hierarchy) effects at the local level appear stronger than competitive (non-system) effects; i.e., the influence of prior adoption by local non-affiliates was not as large as the effect of prior adoption by local affiliates. We observed greater adoption by the dominant market leader in the face of prior adoption by non-affiliates, suggesting both a “fast follower” phenomenon and a local periphery-to-center diffusion model (Becker, 1970). Consistent with Hypothesis 4, effects were more pronounced in local rather than more distant markets. This supports the adage that all healthcare is local. Geographic proximity and less geographic dispersion magnifies both hierarchical and normative influences on the diffusion process.
Our findings highlight the importance of system structure and organizational ties. The prior adoption patterns of both local affiliates and non-affiliates, as well as the distant affiliates, did not influence all system hospitals equally. Centralized systems were more sensitive to prior Magnet adoption among affiliates (local and distant) and non-affiliates, compared to decentralized systems. This is consistent with evidence that inter-organizational linkage is associated with innovation (Goes & Park, 1997), particularly the implementation of known innovations, as is the case with Magnet.
Our results suggest that growing organizational momentum around Magnet adoption within a system leads to an expansion of Magnets over time; however, the underlying motivation is not immediately clear. For example, as we noted, such behavior could reflect increased institutional and cultural buy-in. In a similar way, concurrent adoption behavior among local peers could be consistent with integrated systems seeking a uniform high-quality nursing work environment across all affiliated hospitals or an effort to bolster their local professional reputation. Lastly, the propensity for systems’ largest hospitals to achieve Magnet recognition could reflect these hospitals being more “Magnet-ready” or, alternatively, serving as the “flagship” facility in the effort to improve the professional environment and attract and retain highly qualified clinical staff. Economic market forces could also plausibly feed into the decision-making for system hospitals as well. Additional research is needed to parse out these competing — but not mutually exclusive — motivations for seeking Magnet recognition.
Our study is descriptive in nature since the hospital fixed-effects models are sensitive to any time varying omitted factors. And, as previously discussed, our data cannot speak to the specific thought process driving these organizational decisions. Instead, our contribution is a novel and longitudinal look at the organizational behavior of hospital systems in relation to Magnet adoption. Providing these empirical patterns represents the first steps in understanding the role of hospital systems in the spread of Magnet hospitals throughout the U.S. health care system. We also note that there are many ways to define hospital markets (Garnick, Luft, Robinson, & Tetreault, 1987). We use HRRs that are based on patient referral patterns, but also look at state boundaries. It is possible that there are other market area constructions that would lead to alternative findings.
PRACTICE IMPLICATIONS
Our findings highlight the importance of hospital system structure, hierarchy within the system, and environmental influences on diffusion of an organizational innovation — Magnet recognition. The results are useful to hospital nurse leaders, executives, and policymakers interested in the diffusion of organizational innovations targeting the work environment and care quality. In light of the trends towards hospital consolidation (Brown et al., 2012; Dafny, 2014) and a growing climate of quality incentives, these findings articulate several implications related to Magnet adoption and the downstream implications for system affiliates.
We find the likelihood of Magnet adoption is related to hospital system structure such that centralized hospital systems are more reactive to the adoption behavior of their affiliates compared with hospitals in moderately centralized or decentralized systems. Given uncertainty about whether centralized systems are more or less efficient than decentralized systems (Rosko et al., 2007), our results are limited in their ability to suggest the adoption of a more centralized hospital system structure. Rather, our results imply that centralized hospitals are better able to respond to their affiliates, likely as strong nursing leaders across the system coalescence around shared values regarding the centrality of a good work environment as the foundation for quality. The system may also secondarily achieve branding economies within the system (Besanko et al., 2009), particularly signaling a high quality professional work environment.
Additionally, there is some evidence that Magnet is more than a recognition of pre-existing quality, but that it transforms the work environment and in doing so, leads to better care and patient outcomes (Kutney-Lee et al., 2015; McHugh et al., 2013). Our study suggests that
Magnet adoption is associated with adoption by affiliate hospitals, suggesting a hierarchy effect of common governance. In other words, hospitals respond to the adoption behavior of their affiliates. Although to a lesser extent, hospitals also respond to adoption behavior of non-affiliate hospitals within their local market reflecting normative pressures, and to a lesser extent competitive pressure.
Dominant market leaders within a hospital system are most reactive to Magnet adoption among competitors, suggesting they are “fast followers” (Jarousse, 2012; Zaltman et al., 1973). This is consistent with hypotheses of Hage and Aiken (1967) suggesting that, in complex institutions (as hospitals no doubt are), centralized systems may be slow to initiate an innovation, but once they do, they are able to implement more efficiently.
Our results support the adage that all healthcare is local. Magnet adoption is more likely when competitor hospitals are in the local market as compared to more distant markets. This relationship exists whether or not prior adoption is by affiliates or non-affiliates. When a hospital in a local market adopts, administrators and especially nursing leaders in local competitor hospitals should consider the implications of further adoption that is likely to come to that local environment in the future.
Lastly, the findings are relevant to ongoing efforts to improve clinical quality across the U.S., especially as policymakers and health care administrators consider the downstream implications from growing hospital consolidation and system expansion. A key finding of the Institute of Medicine’s Quality Chasm series including the report, To Err is Human, is that the biggest potential for gains in patient safety comes through the ability of organizations to create the conditions for good quality care. Magnet is not the only means of improving the work environment. It does, however, provide a proven blueprint for improving the work environment, setting the stage for highy qualified clinicians to exert their expertise, execute best practices, and work with interdisciplinary colleagues as an effective high-functioning team. Focusing on the work environment may facilitate achieving the elusive gains in quality that has been the pursuit of hospital systems.
Acknowledgments
The authors wish to thank the American Nurses Foundation Nursing Research Grants Program for partially supporting this research and the National Institute of Nursing Research (T32NR0714). All views and remaining errors belong solely to the authors.
Footnotes
Conflicts: None to declare.
References
- Abraham J, Jerome-D’Emilia B, Begun JW. The diffusion of Magnet hospital recognition. Health Care Management Review. 2011;36(4):306–314. doi: 10.1097/HMR.0b013e318219cd27. [DOI] [PubMed] [Google Scholar]
- Alexander JA, Lee SD, Bazzoli GJ. Governance forms in health systems and health networks. Health Care Management Review. 2003;28(3):228–242. doi: 10.1097/00004010-200307000-00004. [DOI] [PubMed] [Google Scholar]
- Bazzoli GJ, Shortell SM, Dubbs N, Chan C, Kralovec P. A taxonomy of health networks and systems: bringing order out of chaos. Health Services Research. 1999;33(6):1683. [PMC free article] [PubMed] [Google Scholar]
- Becker MH. Factors affecting diffusion of innovations among health professionals. American Journal of Public Health and the Nations Health. 1970;60(2):294–304. doi: 10.2105/ajph.60.2.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood) 2008;27(3):759–769. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- Besanko D, Dranove D, Shanley M, Schaefer S. Economics of strategy. New York: John Wiley & Sons; 2009. [Google Scholar]
- Brown TC, Jr, Werling KA, Walker BC, Burgdorfer RJ, Shields JJ. Current trends in hospital mergers and acquisitions: Healthcare reform will result in more consolidation and integration among hospitals, reversing a recent trend in which hospitals tended to stay away from such transactions. Healthcare Financial Management. 2012;66(3):114–120. [PubMed] [Google Scholar]
- Burns LR, McCullough JS, Wholey DR, Kruse G, Kralovec P, Muller R. Is the system really the solution? Operating costs in hospital systems. Medical Care Research and Review. 2015;72(3):247–272. doi: 10.1177/1077558715583789. [DOI] [PubMed] [Google Scholar]
- Burns LR, Wholey DR, McCullough JS, Kralovec P, Muller R. Annual Review of Health Care Management: Strategy and Policy Perspectives on Reforming Health Systems. Emerald Group Publishing Limited; 2012. The changing configuration of hospital systems: centralization, federalization, or fragmentation? pp. 189–232. [DOI] [PubMed] [Google Scholar]
- Dafny L. Hospital industry consolidation—still more to come? New England Journal of Medicine. 2014;370(3):198–199. doi: 10.1056/NEJMp1313948. [DOI] [PubMed] [Google Scholar]
- DiMaggio P, Powell WW. The iron cage revisited: Collective rationality and institutional isomorphism in organizational fields. American Sociological Review. 1983;48(2):147–160. [Google Scholar]
- Furukawa MF, Raghu TS, Spaulding TJ, Vinze A. Adoption of health information technology for medication safety in US hospitals, 2006. Health Affairs. 2008;27(3):865–875. doi: 10.1377/hlthaff.27.3.865. [DOI] [PubMed] [Google Scholar]
- Garnick DW, Luft HS, Robinson JC, Tetreault J. Appropriate measures of hospital market areas. Health Services Research. 1987;22(1):69–89. [PMC free article] [PubMed] [Google Scholar]
- Gaynor MS, Kleiner SA, Vogt WB. Analysis of hospital production: An output index approach. Journal of Applied Econometrics. 2015;30(3):398–421. [Google Scholar]
- Goes JB, Park SH. Interorganizational links and innovation: The case of hospital services. Academy of Management Journal. 1997;40(3):673–696. [Google Scholar]
- Hage J, Aiken M. Relationship of Centralization to Other Structural Properties. Administrative Science Quarterly. 1967;12(1):72–92. [Google Scholar]
- Henke RM, Karaca Z, Moore B, Cutler E, Liu H, Marder WD, Wong HS. Impact of health system affiliation on hospital resource use intensity and quality of care. Health Services Research. 2016 doi: 10.1111/1475-6773.12631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hines S, Joshi MS. Variation in quality of care within health systems. The Joint Commission Journal on Quality and Patient Safety. 2008;34(6):326–332. doi: 10.1016/s1553-7250(08)34041-0. [DOI] [PubMed] [Google Scholar]
- Jarousse LA. Innovation – your new core competency. [Accessed on February 25, 2017];Hospitals and Health Networks. 2012 Available online at: http://www.hhnmag.com/articles/6025-innovation-your-new-core-competency.
- Jayawardhana J, Welton JM, Lindrooth RC. Is there a business case for Magnet hospitals? Estimates of the cost and revenue implications of becoming a Magnet. Medical Care. 2014;52(5):400–406. doi: 10.1097/MLR.0000000000000092. [DOI] [PubMed] [Google Scholar]
- Kutney-Lee A, Quinn L, Witkoski Stimpfel A, Sloane DM, Cimiotti J, Aiken LH. Changes in patient and nurse outcomes associated with Magnet hospital recognition. Medical Care. 2015;53(6):550–557. doi: 10.1097/MLR.0000000000000355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ladapo JA, Horwitz JR, Weinstein MC, Gazelle GS, Cutler DM. Adoption and spread of new imaging technology: a case study. Health Aff (Millwood) 2009;28(6):w1122–1132. doi: 10.1377/hlthaff.28.6.w1122. hlthaff.28.6.w1122 [pii] [DOI] [PubMed] [Google Scholar]
- Lasater KB, Germack HD, Small DS, McHugh MD. Hospitals known for nursing excellence perform better on Value Based Purchasing measures. Policy, Politics, & Nursing Practice. 2017 doi: 10.1177/1527154417698144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makary MA, Daniel M. Medical error—the third leading cause of death in the US. Brisit Medical Journal. 2016;353:i2139. doi: 10.1136/bmj.i2139. [DOI] [PubMed] [Google Scholar]
- McHugh MD, Kelly LA, Smith HL, Wu ES, Vanak J, Aiken LH. Lower mortality in Magnet hospitals. Medical Care. 2013;51(5):382–388. doi: 10.1097/MLR.0b013e3182726cc5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller RW, Kruse GB. Commentary on “Is the System Really the Solution? Operating Costs in Hospital Systems” Limits to System Efficiency in Centralized Hospital Systems: Illustration From the University of Pennsylvania Health System. Medical Care Research and Review. 2015;72(3):273–276. doi: 10.1177/1077558715584224. [DOI] [PubMed] [Google Scholar]
- Richards MR, Lasater KB, McHugh MD. A race to the top? Competitive pressure and Magnet adoption among US hospitals 1997 – 2012. Medical Care. doi: 10.1097/MLR.0000000000000650. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosko MD, Proenca J, Zinn JS, Bazzoli GJ. Hospital inefficiency: What is the impact of membership in different types of systems? INQUIRY: The Journal of Health Care Organization, Provision, and Financing. 2007;44(3):335–349. doi: 10.5034/inquiryjrnl_44.3.335. [DOI] [PubMed] [Google Scholar]
- Rye CB, Kimberly JR. The adoption of innovations by provider organizations in health care. Medical Care Research and Review. 2007;64(3):235–278. doi: 10.1177/1077558707299865. [DOI] [PubMed] [Google Scholar]
- Shortell SM, Bazzoli GJ, Dubbs NL, Kralovec P. Classifying health networks and systems: managerial and policy implications. Health Care Management Review. 2000;25(4):9–17. doi: 10.1097/00004010-200010000-00002. [DOI] [PubMed] [Google Scholar]
- Sweetland SR. Human capital theory: Foundations of a field of inquiry. Review of Educational Research. 1996;66(3):341–359. [Google Scholar]
- Tsai TC, Jha AK. Hospital consolidation, competition, and quality: is bigger necessarily better? Journal of the American Medical Association. 2014;312(1):29–30. doi: 10.1001/jama.2014.4692. [DOI] [PubMed] [Google Scholar]
- Wang BB, Wan TTH, Burke DE, Bazzoli GJ, Lin BYJ. Factors influencing health information system adoption in American hospitals. Health Care Management Review. 2005;30(1):44–51. doi: 10.1097/00004010-200501000-00007. [DOI] [PubMed] [Google Scholar]
- Zaltman G, Duncan R, Holbek J. Innovations and organizations. Vol. 1973. Wiley; New York: 1973. [Google Scholar]