Abstract
Background/Objectives
Off-label use of antipsychotics is common in the hospital, most often for delirium management. Antipsychotics have been associated with aspiration pneumonia in community and nursing home settings. However, the association in hospitalized patients is unexplored. We aimed to investigate the association between antipsychotic exposure and aspiration pneumonia during hospitalization.
Design
Retrospective cohort study
Setting
Large academic medical center
Participants
All adult hospitalizations between 1/2007 and 7/2013. We excluded outside hospital transfers, those with a hospitalization < 48 hours, and psychiatric patients.
Measurements
Antipsychotic use defined as any pharmacy charge for an antipsychotic medication. Aspiration pneumonia defined by a discharge diagnosis code for aspiration pneumonia not present on admission, and validated by chart review. A generalized estimating equation was used to control for 43 potential confounders.
Results
Our cohort included 146,552 hospitalizations (median age = 56 years; 39% male). Antipsychotics were used in 10,377 (7.1%) hospitalizations (80% atypical, 35% typical, 15% both). Aspiration pneumonia occurred in 557 (0.4%) hospitalizations. The incidence of aspiration pneumonia was 0.3% in unexposed and 1.2% in those with antipsychotic exposure (OR 3.9, 95% confidence interval [CI] 3.2 to 4.8). After adjustment, antipsychotic exposure was significantly associated with aspiration pneumonia (adjusted OR [aOR] 1.5, 95% CI 1.2 to 1.9). Similar results were demonstrated in a propensity-matched analysis and in an analysis restricted to those with delirium or dementia. The magnitude of the association was similar for typical (aOR 1.4, 95% CI 0.94 to 2.2) and atypical antipsychotics (aOR 1.5, 95% CI 1.1 to 2.0).
Conclusion
Antipsychotics were associated with increased odds of aspiration pneumonia after extensive adjustment for patient characteristics. This risk should be considered when prescribing antipsychotics in the hospital.
Keywords: Antipsychotics, aspiration, pneumonia, hospitalization
INTRODUCTION
Antipsychotic medications are widely used in the hospital setting for non-psychiatric purposes, with recent studies demonstrating use in 6–9% of non-psychiatric hospitalizations, and 9–12% of those age 75 and older, most often for management of delirium.1–3 This practice has recently been questioned based on two systematic reviews, both concluding that current evidence does not support the use of antipsychotics for prevention or treatment of delirium.4–6
Concerns regarding lack of data supporting efficacy for this purpose are compounded by evidence of risk from antipsychotics, including falls7, 8 and death.9, 10 Additionally, concerns have been raised regarding an association between antipsychotics and pneumonia. There are at least two hypothesized mechanisms. First, sedation, a known effect of antipsychotics, can lead to difficulty managing secretions and protecting the airway.11, 12 Second, antipsychotics promote oropharyngeal dysphagia directly.13, 14 Several observational studies have demonstrated an association between antipsychotics and pneumonia, particularly aspiration pneumonia, in older patients in the community.15–18 However, these studies were case-control analyses, and did not focus on hospitalized patients, who have greater degrees of comorbidity and incidence of aspiration, than patients in the community, which could result in an even stronger association between antipsychotics and aspiration pneumonia in this patient population. Understanding the magnitude of any such association is important so that hospital physicians can incorporate this into their risk-to-benefit calculation when considering use of antipsychotics for non-psychiatric, off-label purposes. Given that hospital-acquired pneumonia is common, costly, and morbid, and disproportionately affects older adults, identifying potentially modifiable risk factors could result in improved outcomes for hospitalized older adults.19
In the present study we investigated the association between antipsychotic exposure and aspiration pneumonia developing during hospitalization, hypothesizing that antipsychotic exposure would be associated with increased risk, particularly among older patients.
METHODS
Setting and Data Collection
We conducted a retrospective cohort study of patients admitted to a large academic medical center in Boston, Massachusetts from 1/2007 through 7/2013. The study was approved by the institutional review board at Beth Israel Deaconess Medical Center with a waiver of informed consent. Data were collected from electronic databases maintained at the medical center, collected prospectively for clinical/administrative purposes, and supplemented by chart review where noted.
Inclusion and Exclusion Criteria
All hospitalizations of patients ≥18 years of age were eligible for inclusion. We excluded outside hospital transfers since exposure data could not be obtained in this setting, and those with a length of hospitalization <48 hours to allow sufficient time for development of nosocomial aspiration pneumonia. We also excluded those admitted to a psychiatry service or with a primary or secondary discharge diagnosis of a psychotic disorder, defined by the Elixhauser comorbidity “Psychoses” (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] codes 295.00–298.9, 299.10–299.11 and Diagnosis Related Groups 430 and 885)20 since we were interested in use of antipsychotics for conditions other than primary psychiatric disorders.
Antipsychotic Utilization
In-hospital antipsychotic exposure was defined as presence of any pharmacy charge for antipsychotic medication during the hospitalization. In a secondary analysis,we categorized antipsychotics as typical and atypical based on the classification of the Food and Drug Administration.21, 22 We excluded prochlorperazine from our typical antipsychotic definition, as this medication is used as an antiemetic rather than an antipsychotic.
Aspiration Pneumonia
The primary outcome was aspiration pneumonia acquired during hospitalization (i.e. occurring after the first 48 hours of hospitalization, consistent with the definition of nosocomial pneumonia23). To identify cases, we reviewed the charts of all hospitalizations identified as having a discharge ICD-9-CM code for aspiration pneumonia (507) indicated as not “present-on-admission.” We validated that the treating clinician had made a clinical diagnosis of pneumonia and initiated antibiotics for this purpose. We also reviewed radiographs to confirm the presence of a new infiltrate in conjunction with the clinical diagnosis. Lastly, we reviewed the microbiologic data to determine if there were any associated positive sputum cultures. We defined the date of pneumonia onset as the earliest date among the following (if present): 1) date of initiation of antibiotics, 2) date of the positive radiograph, and 3) date of the positive sputum culture. Uncertain cases (with respect to either presence of pneumonia or timing of diagnosis) were reviewed by a second member of the study team, and in the case of disagreement, adjudicated by a third member. In total, only 15 cases of pneumonia (either aspiration or non-aspiration, further described below) required adjudication by a third reviewer.
For hospitalizations with pneumonia, we censored observation time and medication exposure status on the date of pneumonia diagnosis. For antipsychotic exposure specifically, we performed a chart review to assure that exposures occurring on the same day as pneumonia preceded the pneumonia diagnosis. Receipt of mechanical ventilation and intensive care unit (ICU) stay were censored the day prior to pneumonia diagnosis given the time required to develop infectious complications linked to these risk factors.
Covariates
Our models included variables hypothesized to predict use of antipsychotic medications, and variables thought to increase risk of aspiration pneumonia based on prior literature and clinical grounds, including: 1) demographic variables such as age, gender, and race (self-reported by patients); 2) hospitalization characteristic variables, including admitting department (medicine vs. non-medicine), whether the patient spent time in the ICU, and whether they received mechanical ventilation (including via tracheostomy); 3) comorbidities, identified via ICD-9-CM secondary diagnosis codes and DRGs using Healthcare Cost and Utilization Project (HCUP) Comorbidity Software, version 3.7, based on the work of Elixhauser et al.,20, 24 including paralysis and other neurological disorders; 4) other clinical conditions, including delirium, dementia, insomnia, and acute cerebrovascular disease (see Supplementary Text S1 for ICD-9-CM codes); and 5) use of other medications including opioids, benzodiazepines/barbiturates, steroids, and acid-suppressive medications.
Statistical Analysis
The Chi-square test was used to compare categorical variables, and the independent samples t-test to compare continuous variables.
To determine the adjusted association between antipsychotic exposure (either typical or atypical) and aspiration pneumonia, we used a multivariable generalized estimating equation (GEE) with logit link and first-order auto-regressive correlation structure to control for confounders and to account for within-participant correlated data resulting from patients having multiple hospitalizations. We controlled for all variables listed in Table 1 plus the HCUP comorbidities.
Table 1.
Cohort characteristics overall and by antipsychotic exposure status.
| Characteristic | Overall (n=146,552) |
No Antipsychotic Exposure (n=136,175) |
Antipsychotic Exposure (n=10,377) |
|---|---|---|---|
| Age – median (range) | 56 (18–107) | 56 (18–107) | 67 (18–106) |
| Female – n (%) | 89,818 (61) | 84,624 (62) | 5,194 (50) |
| Race – n (%) | |||
| White | 91,792 (63) | 84,209 (62) | 7,583 (73) |
| Black | 18,286 (12) | 17,159 (13) | 1,127 (11) |
| Other/Unknown | 36,474 (25) | 34,807 (26) | 1,667 (16) |
| Comorbidities – n (%) | |||
| Delirium | 6,976 (5) | 4,636 (3) | 2,340 (23) |
| Dementia | 3,327 (2) | 2,147 (2) | 1,180 (11) |
| Insomnia | 1,505 (1) | 1,311 (1) | 194 (2) |
| Acute cerebrovascular disease | 3,913 (3) | 3,374 (2) | 539 (5) |
| Mechanical Ventilation | 6,770 (5) | 5,064 (4) | 1,710 (16) |
| Intensive Care Unit Stay | 26,821 (18) | 22,774 (17) | 4,051 (39) |
| Medicine Admitting Service | 56,761 (39) | 50,490 (37) | 6,271 (60) |
| Length of observation – median days (range) | 4 (2–245) | 4 (2–194) | 6 (2–245) |
| Other medication exposures | |||
| Opioids | 100,608 (69) | 93,082 (68) | 7,529 (73) |
| Benzodiazepines/barbiturates | 32,973 (23) | 28,409 (21) | 4,564 (44) |
| Steroids | 23,644 (16) | 21,175 (16) | 2,470 (24) |
| Acid-suppressives | 74,524 (51) | 67,073 (49) | 7,452 (72) |
To assess the robustness of our findings, and in an attempt to achieve even more homogenous comparator groups, we performed an additional analysis using propensity score matching. We derived a propensity score25 using a GEE model where antipsychotic exposure was the dependent variable. The same set of covariates was used as in the first approach. The fitted probability from this model was used as the propensity score, and the c-statistic was 0.83.
Hospitalizations were then matched on their propensity score using a greedy matching technique.26 We calculated standardized differences to gauge effectiveness of the match.27 Characteristics with residual imbalance (standardized difference absolute value >0.1)28 were incorporated into a GEE model to obtain the adjusted odds ratio (OR) of aspiration pneumonia.
We evaluated the association between typical and atypical antipsychotic exposure and aspiration pneumonia, using a GEE model controlling for all variables in Table 1 plus the HCUP comorbidities, where the independent variable of interest was a 4-category variable reflecting no antipsychotic exposure (reference group), exposure to typical antipsychotics alone, exposure to atypical antipsychotics alone, and exposure to both.
A 2-sided type-I error of < 0.05 was used to indicate statistical significance. Assuming a rate of 0.5 aspiration pneumonias per 100 hospitalizations and an exposure rate of 10% based on prior literature, a sample size of 150,000 hospitalizations would be necessary to achieve 90% power to detect a relative risk of 1.5. Analyses were carried out using SAS software, version 9.3, Cary, NC.
Sensitivity Analysis
Using methods similar to those of previous investigators,29, 30 we estimated the strength of association (between an unmeasured confounder and antipsychotic use or an unmeasured confounder and aspiration pneumonia) that would be needed to explain the observed risk of aspiration pneumonia from antipsychotic use solely on the basis of confounding.
Specificity Analysis of Non-Aspiration Pneumonia
Because antipsychotics are hypothesized to cause pneumonia through effects on swallowing function, we hypothesized that antipsychotic medication would not be associated with non-aspiration pneumonia. To test this hypothesis, we reviewed the charts of all patients with a discharge ICD-9-CM code for non-aspiration pneumonia (481, 482, 483, 485, 486) indicated as not “present-on-admission,” again validating pneumonia occurrence and timing using methodology described above. We then reran our analysis replacing aspiration with non-aspiration pneumonia as the dependent variable in our models.
Subgroup Analyses: Age and Delirium/Dementia
To assess whether the relationship between antipsychotic exposure and aspiration pneumonia differed by age category, and to determine the attributable risk of aspiration pneumonia among these categories, we performed two additional analyses. First, we assessed for effect modification by age by creating a 3 category age variable (<65, 65–74, >=75) and assessing the significance of the interaction term with antipsychotic exposure in our main model. Second, we ran stratified models of aspiration pneumonia in these predefined age categories. Due to reduced sample size for these analyses, we had to remove covariates with low prevalence from our models to obtain convergence: peptic ulcer disease without bleeding, acquired immune deficiency syndrome (AIDS), solid tumor without metastasis, drug abuse, and insomnia.
Because delirium and dementia are poorly captured in administrative databases,31 and such misclassification could confound our analyses given that patients with these conditions are more likely to be exposed to antipsychotics and more likely to aspirate, we repeated our analysis in the subgroup of hospitalizations with a discharge diagnosis of delirium or dementia. As a result of the reduced sample size, we had to remove covariates with low prevalence from our models to obtain convergence: peptic ulcer disease without bleeding, AIDS, and insomnia.
RESULTS
Cohort Characteristics
There were 230,635 hospitalizations age ≥18 from 1/2007–7/2013. After excluding outside hospital transfers (n = 14,422), hospitalizations <48 hours in duration (n = 59,774), and hospitalizations with psychosis or a psychiatric attending of record (n = 9,887), there were 146,552 hospitalizations in the cohort. The median age was 56 years (range 18–107), and 56,734 (39%) were female. Table 1 shows the cohort characteristics stratified by exposure status (see Supplementary Table S1 for the distribution of HCUP comorbidities).
Exposure to Antipsychotic Medication
Antipsychotic exposure occurred in 10,377 (7.1%) hospitalizations, with a median of 3 (25th–75th percentile 2–5) days of exposure (median length of hospital observation was 4 days; see Table 1). Of the group exposed to antipsychotics, 3,677 (35.4%) received typical and 8,282 (79.8%) received atypical antipsychotics, with 1,582 (15.2%) exposed to both. There were significant differences in baseline characteristics between exposed and unexposed (Table 1).
Antipsychotic Medication and Aspiration Pneumonia
Table 2 shows the unadjusted incidence of aspiration pneumonia relative to antipsychotic exposure. Aspiration pneumonia occurred in 557 hospitalizations (0.4%). Among patients with antipsychotic exposure and aspiration pneumonia, there was a median of 1 (25th–75th percentile 0–2) day between the last dose of antipsychotic medication and the diagnosis of aspiration pneumonia. The unadjusted incidence of aspiration pneumonia was higher in the group exposed to antipsychotics relative to those unexposed (1.2% versus 0.3%; OR 3.9, 95% confidence interval [CI] 3.2–4.8).
Table 2.
Rates of aspiration and non-aspiration pneumonia according to antipsychotic exposure status.
| Outcome | No Antipsychotic Exposure n (%) (n = 136,153) |
Antipsychotic Exposure n (%) (n = 10,399) |
Unadjusted Odds Ratio [95% CI] (n = 146,552) |
Adjusted Odds Ratioa [95% CI] (n = 146,552) |
Propensity Matched Odds Ratiob [95% CI] (n = 20,406) |
|---|---|---|---|---|---|
| Aspiration pneumonia | 430 (0.3) | 127 (1.2) | 3.9 [3.2–4.8] | 1.5 [1.2–1.9] | 1.4 [1.1–1.8] |
| Non-aspiration pneumonia | 956 (0.7) | 175 (1.7) | 2.4 [2.1–2.9] | 1.1 [0.9–1.3] | 1.0 [0.8–1.2] |
Adjusted for all variables listed in Table 1, plus the Healthcare Cost and Utilization Project comorbidities,24 using a multivariable GEE to take into account dependency of the data due to repeated hospitalizations.
Matched on propensity score and analyzed using a multivariable GEE, controlling for all significantly imbalanced baseline characteristics after matching, as demonstrated in Table 3 (using a standardized difference (absolute value) >0.1).
After adjustment, a significant association between antipsychotic exposure and aspiration pneumonia persisted (adjusted OR [aOR] 1.5, 95% CI 1.2–1.9; Table 2).
Propensity-Matched Analysis
We successfully matched 10,203 (98.3%) hospitalizations with antipsychotic exposure to 10,203 unexposed hospitalizations. After matching, the group exposed to antipsychotics was much more similar in baseline characteristics to the unexposed group (Supplementary Table S1), with all standardized differences <0.1 except for age and depression, which we included in our post-match GEE model. A significant association between antipsychotic exposure and aspiration pneumonia persisted (aOR 1.4, 95% CI 1.1–1.8; Table 2).
Exposure Subcategories
Table 3 demonstrates the associations between subcategories of antipsychotics and aspiration pneumonia. The aORs were similar, at 1.4 for typical (95% CI 0.94–2.2), and 1.5 for atypical antipsychotic exposure (95% CI 1.1–2.0).
Table 3.
Associations between subclasses of antipsychotic medication and aspiration pneumonia (n=146,552).
| Exposure Status | Unexposed (n=136,175) |
Typical Exposure (n=2,095) |
Atypical Exposure (n=6,700) |
Both (n=1582) |
|---|---|---|---|---|
| Aspiration pneumonia – n (%) | 430 (0.3) | 31 (1.5) | 64 (1.0) | 32 (2.0) |
| Unadjusted odds ratio [95% CI] | Reference | 4.7 [3.3–6.8] | 3.0 [2.3–4.0] | 6.5 [4.5–9.4] |
| Adjusteda odds ratio [95% CI] | Reference | 1.4 [0.94–2.2] | 1.5 [1.1–2.0] | 1.6 [1.1–2.5] |
Sensitivity Analysis
Assuming prevalence of a confounder of 20% (chosen because it resulted in the most conservative OR estimates), we found that ORs of at least 3–4 would be necessary between confounder and antipsychotic use and between confounder and aspiration pneumonia to explain our observed association solely on the basis of unmeasured confounding.
Specificity Analysis of Non-Aspiration Pneumonia
We found no association between antipsychotic exposure and non-aspiration pneumonia with either our traditional GEE or propensity score approach (aOR 1.1, 95% CI 0.9–1.3 and aOR 1.0, 95% CI 0.8–1.2, respectively; Table 2).
Subgroup Analyses: Age and Delirium/Dementia
Antipsychotic exposure and aspiration pneumonia incidence both increased significantly with age (5.2%, 7.3%, and 12.5% exposure rate and 0.2%, 0.6%, and 0.7% aspiration pneumonia incidence for age <65, 65–74, and ≥75, respectively; p < 0.001 for both). Although terms for effect modification by age were not significant (p = 0.62 and 0.80 for interaction with age 65–74 and ≥75, respectively), both the relative risk of aspiration pneumonia and the absolute incidence of aspiration pneumonia attributable to antipsychotic exposure increased with age (Figure 1).
Figure 1.
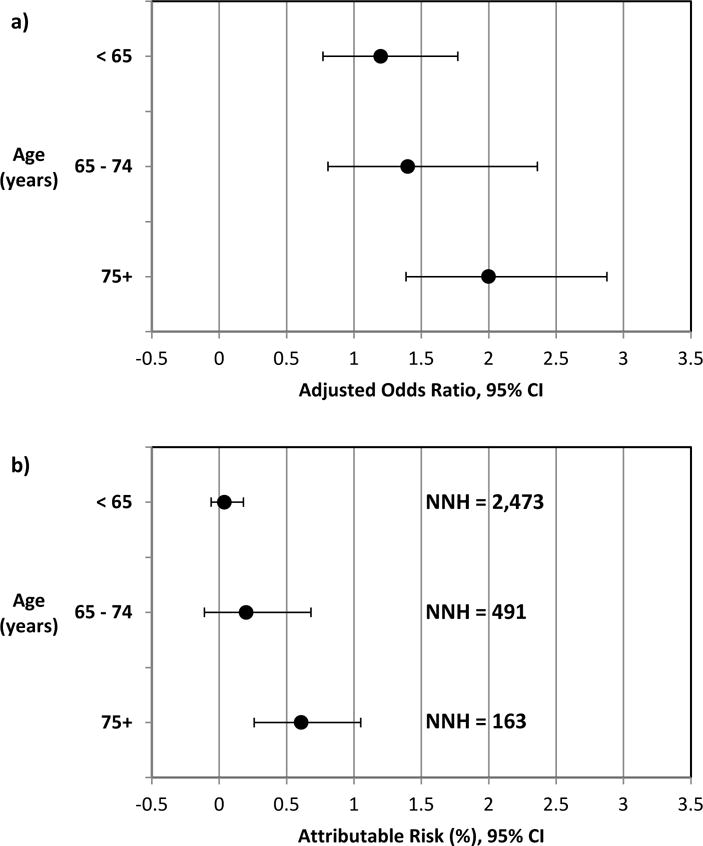
a) Adjusted association between antipsychotic exposure and aspiration pneumonia, by age category. We used a multivariable GEE to adjust for all variables listed in Table 1 except insomnia, plus the Healthcare Cost and Utilization Project comorbidities with the exception of peptic ulcer disease without bleeding, acquired immune deficiency syndrome (AIDS), solid tumor without metastasis, and drug abuse.
b) Adjusted absolute incidence of aspiration pneumonia attributable to antipsychotic exposure (attributable risk), calculated as the difference between the adjusted incidence of aspiration pneumonia among exposed and unexposed, derived using Bayes theorem. Number-needed-to-harm calculated by taking the inverse of the attributable risk. Antipsychotic exposure and aspiration pneumonia incidence both increased with age (5.2%, 7.3%, and 12.5% exposed and 0.2%, 0.6%, and 0.7% aspiration pneumonia incidence for age <65, 65–74, and ≥75, respectively).
After restricting our analysis to those hospitalizations with a discharge diagnosis of delirium or dementia (n = 9,516), the association was again significant for aspiration pneumonia (aOR 1.5, 95% CI 1.1–2.1) but not for non-aspiration pneumonia (aOR 0.8, 95% CI 0.6–1.1).
DISCUSSION
In this cohort of non-psychiatric hospitalizations at a large academic medical center, we found that antipsychotic exposure was associated with increased odds of aspiration pneumonia after extensive adjustment for patient characteristics. This association was robust through multiple analytic approaches, and persisted when focusing on those with discharge diagnoses of delirium and dementia. The specificity of this association, demonstrated through our finding of no association between antipsychotics and non-aspiration pneumonia, lends support to the idea of a causal pathway between exposure and outcome. To our knowledge, this is the first study to evaluate the association between antipsychotic use and development of aspiration pneumonia in hospitalized patients. We believe this risk should be considered when prescribing antipsychotics in the hospital.
Recent systematic reviews have concluded that there is insufficient evidence to justify use of antipsychotics for prevention or treatment of delirium, mostly based on significant methodologic limitations of existing studies and conflicting results.4, 6 Nonetheless, when caring for patients with severe agitation or distress who pose a risk of harm or interruption of medical therapy, hospital physicians are faced with few alternatives, and in this situation, most experts agree that the benefits of antipsychotics are likely to outweigh the risks.5 However, antipsychotics are frequently used outside of this setting in hospitalized patients. Our findings add to the increasingly recognized risks of antipsychotics, providing physicians with additional data to substantiate a higher threshold for use than is commonly employed, and highlighting the importance of additional research to better define any benefits of these medications in delirium management.
Although the relationship between antipsychotic exposure and aspiration pneumonia did not differ significantly by age based on a test for effect modification, the point estimates did increase with increasing age category. Further, it is important to note that patients ≥75 years had more than triple the incidence of aspiration pneumonia compared to patients <65 years of age. Because of this, the absolute risk of aspiration pneumonia attributable to antipsychotic exposure (attributable risk) is much greater for older than younger patients. Accordingly, the number-needed-to-harm is much smaller, dropping from >2000 in those <65 years to 163 in those ≥75 years of age. When coupled with our observation that patients ≥75 years had double the rate of antipsychotic exposure, our findings suggest that targeting older adults for interventions aimed at improving antipsychotic prescribing practices will lead to the greatest absolute reduction in the occurrence of this costly and morbid complication.
Because our study was observational, and thus prone to confounding by severity of illness and indication (wherein factors that make patients more likely to be placed on antipsychotics also make patients more likely to develop aspiration pneumonia, independent of the antipsychotic), we performed subgroup analyses designed to enhance comparability of hospitalizations with and without antipsychotic exposure, including a propensity-matched analysis and an analysis restricted to patients with delirium or dementia. In both of these secondary analyses, the association between antipsychotic exposure and aspiration pneumonia was significant and consistent with our primary analysis. The robustness of this finding through multiple analyses supports the existence of a true association. Additionally, our sensitivity analysis determined that relatively strong associations (ORs of at least 3 to 4) would be necessary between an unmeasured confounder and antipsychotic use and between confounder and aspiration pneumonia to explain the risk observed in this study solely on the basis of unmeasured confounding. Nonetheless, we cannot exclude the possibility that unmeasured confounding (by indication or otherwise) explains our findings.
With an overall aspiration pneumonia rate of 0.4% and an antipsychotic exposure rate of 7%, a relative risk of 1.4 translates to an attributable risk of 0.16% and a number needed to harm of 625. With 40 million discharges from U.S. hospitals each year, and approximately 2.8 million exposed, this suggests potentially >4,000 excess cases of aspiration pneumonia attributable to hospital antipsychotic use each year.
We demonstrated qualitatively similar associations between typical and atypical antipsychotics and aspiration pneumonia. Prior analyses in the community and nursing home settings have yielded conflicted findings in this realm. Some have demonstrated heightened risk in current users of atypical compared to typical antipsychotics,15, 16 while others, including a meta-analysis of observational studies in the outpatient setting, have demonstrated similarly increased risk.32–34 Our results lend support to the idea that pneumonia risk does not vary by antipsychotic subclass.
Strengths of our study include the large sample size, chart-based validation of all cases of pneumonia, and rigorous methods to control for potential confounders. There are also important limitations. First, although we studied almost 150,000 hospitalizations, the single center nature limits generalizability and our findings should be validated at other institutions. Additionally, lack of information on preadmission use of antipsychotic medications precluded our ability to assess for differential effects among new initiators. Two studies in the community-setting found that pneumonia risk was highest during the first week after antipsychotic initiation.15, 16 Since a study conducted at our medical center previously estimated that about half of antipsychotic use in hospitalized patients represents new initiation,2 it is possible that the inclusion of more chronic use in our analysis could have resulted in underestimation of the true association between antipsychotic initiation and aspiration pneumonia.
In conclusion, in this large cohort of non-psychiatric hospitalizations, we found that antipsychotics were associated with 40–50% increased odds of developing aspiration pneumonia during hospitalization. This risk should be considered when prescribing antipsychotics for off-label purposes like delirium and dementia in hospitalized patients, particularly for those age 75 and older. The controversial benefits of use in this setting must be weighed against the growing number of risks.
Supplementary Material
Supplementary Table S1: Cohort characteristics, including HCUP comorbidities, overall and by antipsychotic exposure status, before and after propensity score matching.
Supplementary Text S1: ICD-9-CM codes defining delirium, dementia, insomnia, and acute cerebrovascular disease:
Acknowledgments
Funding Sources: Dr. Herzig was funded by grant number K23AG042459 from the National Institute on Aging. Dr. Marcantonio was funded by grant number K24AG035075 from the National Institute on Aging.
Sponsor’s Role: The funding organizations had no involvement in any aspect of the study, including design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Related paper presentations: An abstract representing an earlier version of the data contained in this manuscript was presented at the Annual Society of General Internal Medicine meeting in San Diego, April 2014.
Author Contributions: Dr. Herzig had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Herzig, LaSalvia, Gurwitz, Rothberg, Marcantonio.
Acquisition of data: Herzig, LaSalvia, Naidus.
Analysis and Interpretation of data: Herzig, LaSalvia, Naidus, Gurwitz, Rothberg, Marcantonio.
Drafting of the manuscript: Herzig.
Critical revision of the manuscript for important intellectual content: LaSalvia, Naidus, Gurwitz, Rothberg, Marcantonio.
Conflicts of Interest and Financial Disclosures: None of the authors have any conflicts of interest to disclose.
References
- 1.Herzig SJ, Rothberg MB, Guess JR, Gurwitz JH, Marcantonio ER. Antipsychotic medication utilization in nonpsychiatric hospitalizations. J Hosp Med. 2016 doi: 10.1002/jhm.2596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Herzig SJ, Rothberg MB, Guess JR, et al. Antipsychotic Use in Hospitalized Adults: Rates, Indications, and Predictors. J Am Geriatr Soc. 2016;64:299–305. doi: 10.1111/jgs.13943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Loh KP, Ramdass S, Garb JL, Brennan MJ, Lindenauer PK, Lagu T. From hospital to community: Use of antipsychotics in hospitalized elders. J Hosp Med. 2014;9:802–804. doi: 10.1002/jhm.2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flaherty JH, Gonzales JP, Dong B. Antipsychotics in the treatment of delirium in older hospitalized adults: a systematic review. J Am Geriatr Soc. 2011;59(Suppl 2):S269–276. doi: 10.1111/j.1532-5415.2011.03675.x. [DOI] [PubMed] [Google Scholar]
- 5.Inouye SK, Marcantonio ER, Metzger ED. Doing Damage in Delirium: The Hazards of Antipsychotic Treatment in Elderly Persons. Lancet Psychiatry. 2014;1:312–315. doi: 10.1016/S2215-0366(14)70263-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Neufeld KJ, Yue J, Robinson TN, Inouye SK, Needham DM. Antipsychotic Medication for Prevention and Treatment of Delirium in Hospitalized Adults: A Systematic Review and Meta-Analysis. J Am Geriatr Soc. 2016;64:705–714. doi: 10.1111/jgs.14076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: I. Psychotropic drugs. J Am Geriatr Soc. 1999;47:30–39. doi: 10.1111/j.1532-5415.1999.tb01898.x. [DOI] [PubMed] [Google Scholar]
- 8.Ray WA, Griffin MR, Schaffner W, Baugh DK, Melton LJ., 3rd Psychotropic drug use and the risk of hip fracture. N Engl J Med. 1987;316:363–369. doi: 10.1056/NEJM198702123160702. [DOI] [PubMed] [Google Scholar]
- 9.Ray WA, Chung CP, Murray KT, Hall K, Stein CM. Atypical antipsychotic drugs and the risk of sudden cardiac death. N Engl J Med. 2009;360:225–235. doi: 10.1056/NEJMoa0806994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang PS, Schneeweiss S, Avorn J, et al. Risk of death in elderly users of conventional vs. atypical antipsychotic medications. N Engl J Med. 2005;353:2335–2341. doi: 10.1056/NEJMoa052827. [DOI] [PubMed] [Google Scholar]
- 11.Harkness GA, Bentley DW, Roghmann KJ. Risk factors for nosocomial pneumonia in the elderly. Am J Med. 1990;89:457–463. doi: 10.1016/0002-9343(90)90376-o. [DOI] [PubMed] [Google Scholar]
- 12.Loeb M, McGeer A, McArthur M, Walter S, Simor AE. Risk factors for pneumonia and other lower respiratory tract infections in elderly residents of long-term care facilities. Arch Intern Med. 1999;159:2058–2064. doi: 10.1001/archinte.159.17.2058. [DOI] [PubMed] [Google Scholar]
- 13.Rudolph JL, Gardner KF, Gramigna GD, McGlinchey RE. Antipsychotics and oropharyngeal dysphagia in hospitalized older patients. J Clin Psychopharmacol. 2008;28:532–535. doi: 10.1097/JCP.0b013e318184c905. [DOI] [PubMed] [Google Scholar]
- 14.Wada H, Nakajoh K, Satoh-Nakagawa T, et al. Risk factors of aspiration pneumonia in Alzheimer’s disease patients. Gerontology. 2001;47:271–276. doi: 10.1159/000052811. [DOI] [PubMed] [Google Scholar]
- 15.Knol W, van Marum RJ, Jansen PA, Souverein PC, Schobben AF, Egberts AC. Antipsychotic drug use and risk of pneumonia in elderly people. J Am Geriatr Soc. 2008;56:661–666. doi: 10.1111/j.1532-5415.2007.01625.x. [DOI] [PubMed] [Google Scholar]
- 16.Trifiro G, Gambassi G, Sen EF, et al. Association of community-acquired pneumonia with antipsychotic drug use in elderly patients: a nested case-control study. Ann Intern Med. 2010;152:418–425. W139–440. doi: 10.7326/0003-4819-152-7-201004060-00006. [DOI] [PubMed] [Google Scholar]
- 17.Gau JT, Acharya U, Khan S, Heh V, Mody L, Kao TC. Pharmacotherapy and the risk for community-acquired pneumonia. BMC Geriatr. 2010;10:45. doi: 10.1186/1471-2318-10-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pratt N, Roughead EE, Ramsay E, Salter A, Ryan P. Risk of hospitalization for hip fracture and pneumonia associated with antipsychotic prescribing in the elderly: a self-controlled case-series analysis in an Australian health care claims database. Drug Saf. 2011;34:567–575. doi: 10.2165/11588470-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 19.Ewan V, Hellyer T, Newton J, Simpson J. New horizons in hospital acquired pneumonia in older people. Age Ageing. 2017:1–7. doi: 10.1093/ageing/afx029. [DOI] [PubMed] [Google Scholar]
- 20.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 21.U.S. Food and Drug Administration. Information on Conventional Antipsychotics. Available at: http://www.fda.gov/drugs/drugsafety/postmarketdrugsafetyinformationforpatientsandproviders/ucm107211.htm. Accessed November 1, 2015.
- 22.U.S. Food and Drug Administration. Atypical Antipsychotic Drugs Information. Available at: http://www.fda.gov/drugs/drugsafety/postmarketdrugsafetyinformationforpatientsandproviders/ucm094303.htm. Accessed November 1, 2015.
- 23.American Thoracic Society; Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388–416. doi: 10.1164/rccm.200405-644ST. [DOI] [PubMed] [Google Scholar]
- 24.HCUP Comorbidity Software. Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality; Rockville, MD: Jan, 2013. Available at: www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp. Accessed March 15, 2016. [PubMed] [Google Scholar]
- 25.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- 26.Parsons LS. Reducing bias in a propensity score matched-pair sample using greedy matching techniques. Proceedings of the Twenty-Sixth Annual SAS (Users Group International Conference); Cary, NC: SAS Institute Inc. 2001. [Google Scholar]
- 27.Yang D, Dalton J. A unified approach to measuring the effect size between two groups using SAS. SAS Global Forum. 2012 Available at: http://support.sas.com/resources/papers/proceedings12/335-2012.pdf. Accessed June 12, 2017.
- 28.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 29.Wang PS, Bohn RL, Glynn RJ, Mogun H, Avorn J. Zolpidem use and hip fractures in older people. J Am Geriatr Soc. 2001;49:1685–1690. doi: 10.1111/j.1532-5415.2001.49280.x. [DOI] [PubMed] [Google Scholar]
- 30.Psaty BM, Koepsell TD, Lin D, et al. Assessment and control for confounding by indication in observational studies. J Am Geriatr Soc. 1999;47:749–754. doi: 10.1111/j.1532-5415.1999.tb01603.x. [DOI] [PubMed] [Google Scholar]
- 31.Inouye SK, Leo-Summers L, Zhang Y, Bogardus ST, Jr, Leslie DL, Agostini JV. A chart-based method for identification of delirium: validation compared with interviewer ratings using the confusion assessment method. J Am Geriatr Soc. 2005;53:312–318. doi: 10.1111/j.1532-5415.2005.53120.x. [DOI] [PubMed] [Google Scholar]
- 32.Nose M, Recla E, Trifiro G, Barbui C. Antipsychotic drug exposure and risk of pneumonia: a systematic review and meta-analysis of observational studies. Pharmacoepidemiol Drug Saf. 2015;24:812–820. doi: 10.1002/pds.3804. [DOI] [PubMed] [Google Scholar]
- 33.Aparasu RR, Chatterjee S, Chen H. Risk of pneumonia in elderly nursing home residents using typical versus atypical antipsychotics. Ann Pharmacother. 2013;47:464–474. doi: 10.1345/aph.1R510. [DOI] [PubMed] [Google Scholar]
- 34.Star K, Bate A, Meyboom RH, Edwards IR. Pneumonia following antipsychotic prescriptions in electronic health records: a patient safety concern? Br J Gen Pract. 2010;60:e385–394. doi: 10.3399/bjgp10X532396. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1: Cohort characteristics, including HCUP comorbidities, overall and by antipsychotic exposure status, before and after propensity score matching.
Supplementary Text S1: ICD-9-CM codes defining delirium, dementia, insomnia, and acute cerebrovascular disease:


