Abstract
In response to the epidemic of falls and serious falls-related injuries among older persons, in 2014, the Patient Centered Outcomes Research Institute (PCORI) and the National Institute on Aging funded a pragmatic trial, Strategies to Reduce Injuries and Develop confidence in Elders (STRIDE) to compare the effects of a multifactorial intervention and an enhanced usual care intervention.
The STRIDE multifactorial intervention consists of 5 major components delivered by registered nurses in the role of Falls Care Managers (FCM), who co-manage fall risk in partnership with patients and their primary care providers (PCP). The components include: 1) standardized assessment of 8 modifiable risk factors (medications, postural hypotension, feet and footwear, vision, vitamin D, osteoporosis, home safety, and strength, gait, and balance impairment) and the use of protocols and algorithms to generate recommended management of risk factors; 2) explanation of assessment results to the patient (and caregiver when appropriate) using basic motivational interviewing techniques to elicit patient priorities, preferences, and readiness to participate in treatments; 3) co-creation of individualized Falls Care Plans that are reviewed, modified, and approved by patients’ PCPs; 4) implementation of the Falls Care Plan; and 5) ongoing monitoring of response, regularly scheduled re-assessments of fall risk, and revisions of the Falls Care Plan. Custom-designed falls care management software facilitates risk factor assessment, the identification of recommended interventions, clinic note generation, and longitudinal care management.
The trial testing the effectiveness of the STRIDE intervention is in progress with results expected in late 2019.
Keywords: falls, injuries, prevention, cluster-randomized clinical trial
INTRODUCTION
More than one in four of older Americans fall each year, 20% of whom sustain serious injuries (e.g., hip fractures, head trauma),1 making falls the leading cause of fatal2 and nonfatal3 injuries. Despite evidence that falls can be prevented, fewer than 50% of persons discuss their falls with their primary care providers (PCP).4
STRIDE is a multi-site cluster randomized clinical trial (cRCT) comparing the effectiveness of an evidence-based, multifactorial, individually-tailored intervention versus enhanced usual care in reducing serious fall injuries among 5451 at-risk, non-institutionalized, older persons. People eligible to participate (hereafter referred to as “patients”) were at least 70 years of age and had failed a screen for elevated risk of injurious falls in the future (i.e., reported two or more falls or an injurious fall during the past year – or a fear of falling because of balance or gait problems.)5 In this paper, we describe the STRIDE intervention. Note that this differs from the STRIDE program of supervised walking for older adults for older adults to the hospital with medical illnesses.6
THE STRIDE INTERVENTION
Overview
The STRIDE intervention consists of specific care processes designed to reduce patients’ fall risks, as well as two methods of ensuring that these processes are followed for each at-risk patient. The care processes include an assessment of the patient’s specific risks of falling, followed by evidence-based7 interventions steps that are tailored to the patient’s individual risk factors and preferences. The two methods used to ensure implementation are: 1) “practice redesign,” based on the ACOVE-2 approach8 and 2) risk factor assessments and interventions to engage patients and caregivers, based on the Connecticut Collaboration for Fall Prevention.9,10
The STRIDE processes are:
Risk assessment and generation of recommendations by a Falls Care Manager (FCM) using standardized, structured assessment procedures and algorithms.
Explanation of identified risks by the FCM to the patient (and caregiver, when appropriate) and suggested interventions, using motivational interviewing to elicit patient preferences and readiness to participate in treatments.
Co-creation (FCM and patient) of an individualized Falls Care Plan that considers risk-specific treatment algorithms, personal preferences, and available resources.
- Implementation of the Falls Care Plan by the patient, FCM, PCP, and other providers.
- Interventions within a RN’s scope of practice (e.g., recommendations for safe footwear and instruction on simple home exercises) are managed by FCMs and patients.
- Interventions outside a RN’s scope of practice (e.g., treatment of osteoporosis) are communicated to relevant providers using the Situation, Background, Assessment and Recommendation (SBAR) template.
- Interventions requiring specialized skills or programs are referred (e.g., to outpatient physical therapy or community-based exercise programs).
Longitudinal follow-up includes in-person visits (at least annually) and phone calls (at least once during the first year) to reassess the patient’s falls risk factors and to evaluate the implementation and the effects of the Falls Care Plan. These calls and visits determine whether the patient had difficulty implementing the specific prioritized actions in the Care Plan and, if so, what assistance could be provided or modifications could be made. The FCMs also inquired about whether the patients’ goals and expectations were met, as outlined in the Care Plan (eg, better balance, improved function) but did not ask obtain the research outcomes, which were collected by the Data Coordination Center.
Intervention development and implementation were guided by a Patient and Stakeholder Council that reviewed and revised procedures, algorithms and patient education materials. The Council is composed of 21 members including 4 patients and 1 caregiver as well as community stakeholder representatives, and national fall prevention experts.
Falls care management software was created to facilitate risk calculation, note generation, tracking of care, and implementation of recommendations.
Falls Care Manager’s Qualifications and Role
FCMs are Bachelor of Science in Nursing (BSN)-prepared Registered Nurses (RNs) who completed a comprehensive STRIDE training course, which includes 26 online modules (with narrated presentations, formative assessments, and written resources) and supplemented with a face-to-face group session designed to facilitate simulation and practice delivering all intervention components. Continuing education is offered throughout the study via annual face-to-face group sessions and monthly conference calls.
FCMs practice within a co-management model with PCPs and their health care teams. FCMs are supervised by a site clinical director (SCD), who is a physician, nurse practitioner, or pharmacist with expertise in falls and knowledge regarding the local healthcare system. To ensure cross-site standardization, FCMs participate in weekly conference calls with a nurse scientist who has expertise in advanced practice nursing in gerontology.
Work Flow for the STRIDE Intervention
Before contacting each high-risk patient, the FCM reviews the patient’s electronic medical record for information related to falls risk factors, including prior bone mineral density testing, cognitive function and medications related to falling and osteoporosis.11
In the initial contact with the patient, which occurs via telephone, the FCM introduces the clinical aspects of the STRIDE intervention and begins to develop a therapeutic relationship. The FCM reviews the circumstances of any falls and data that will be needed to calculate the patient’s risk of future fractures (FRAX score).11 The FCM also informs the patient of documents that will soon arrive by mail (a pre-visit questionnaire [PVQ], a CDC Home Safety Checklist, and a travel safety checklist) and encourages the patient to bring to the first STRIDE visit the completed PVQ and all current medications, and wear usual footwear to the visit.
The FCM’s goal for the patient’s initial visit is to complete a comprehensive falls risk assessment and to draft with the patient (and caregiver, when appropriate) a Falls Care Plan. The history clarifies or expands on PVQ topics and current medications, and the physical exam includes postural vital signs, a Snellen vision screen (when indicated), a modified short physical performance battery (mSPPB)12 that was modified for this study (http:/www.stride-study.org) to accommodate the time constraints of clinical practice, cognitive screening using the Mini-Cog,13 and inspection of the patient’s feet and footwear.
The FCM then summarizes the patient’s modifiable risk factors and begins the process of care planning. Techniques of motivational interviewing and self-management14,15,16,17,18 are used to explore the patient’s perspectives regarding the identified risk factors and which of these are the patient’s priorities for modification. The FCM then describes the evidence-based interventions that could reduce each of these risk factors, including how the patient might help implement them. Based on the patient’s preferences, the FCM drafts an initial Falls Care Plan (Figures 1 and 2) and gives the patient written information about each of their prioritized risks (in English or Spanish). Finally, the patient (and the caregiver, when appropriate) is instructed on how to get up from a fall, either by video or by reviewing an illustrated handout.
Figure 1.
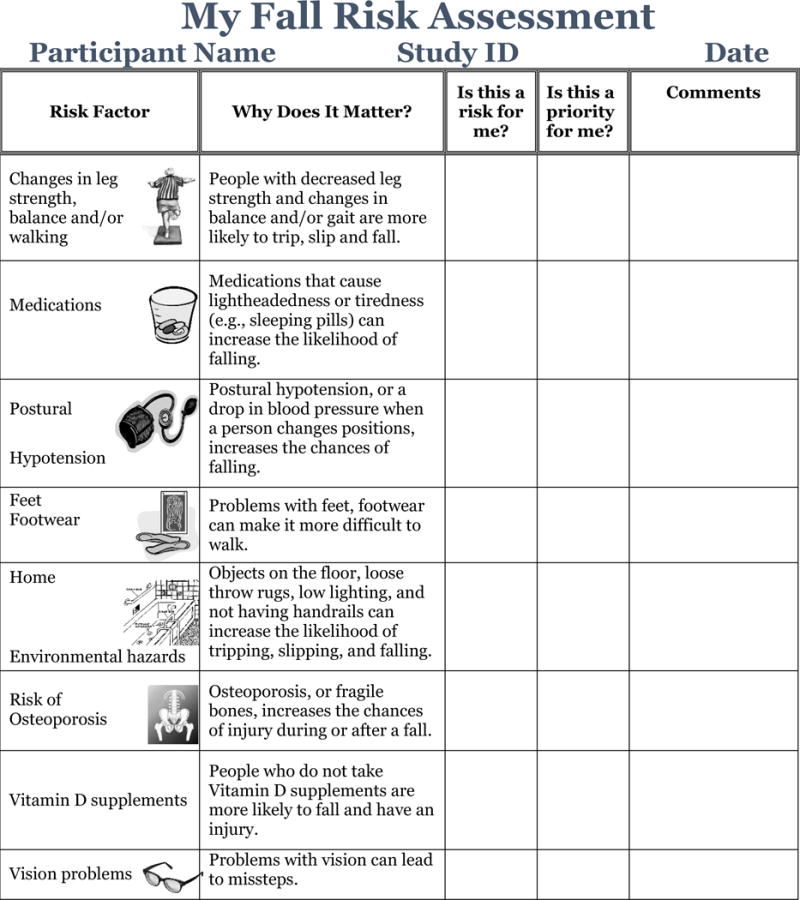
Falls Care Plan Page 1: Summary of Risk Assessment
Figure 2.
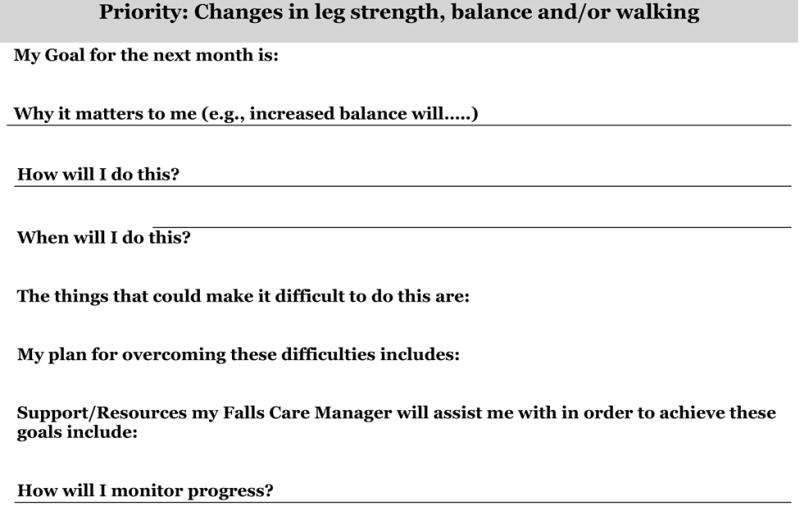
Falls Care Plan Pages 2–7 Example Template: Risk factor-specific goals and plans*
*A separate page is completed for each risk factor that the patient prioritizes.
After the initial visit, the FCM completes a comprehensive note and communicates the initial Falls Care Plan electronically to the PCP and other health care team members including the pharmacist, if fall risk increasing drugs (FRIDs) are identified. STRIDE recommended interventions are communicated using standardized SBAR templates through the EHR. Within several days, the PCP sends edits to and/or approval of the Falls Care Plan to the FCM – and the FCM telephones the patient to discuss these recommendations and plan appropriate follow-up.
Risk Factor Assessment and Recommendations
Through this evaluation and planning process, the FCM addresses eight risk factors for falling including generating specific recommendations (http:/www.stride-study.org/. An example is provided as Figure 3. Sites have leeway to modify the protocols to fit local cultures as long as the risk assessment and recommendation process lead to the same outcomes of the protocols. For example, one site prefers to have bone mineral testing performed on all patients.
Figure 3.
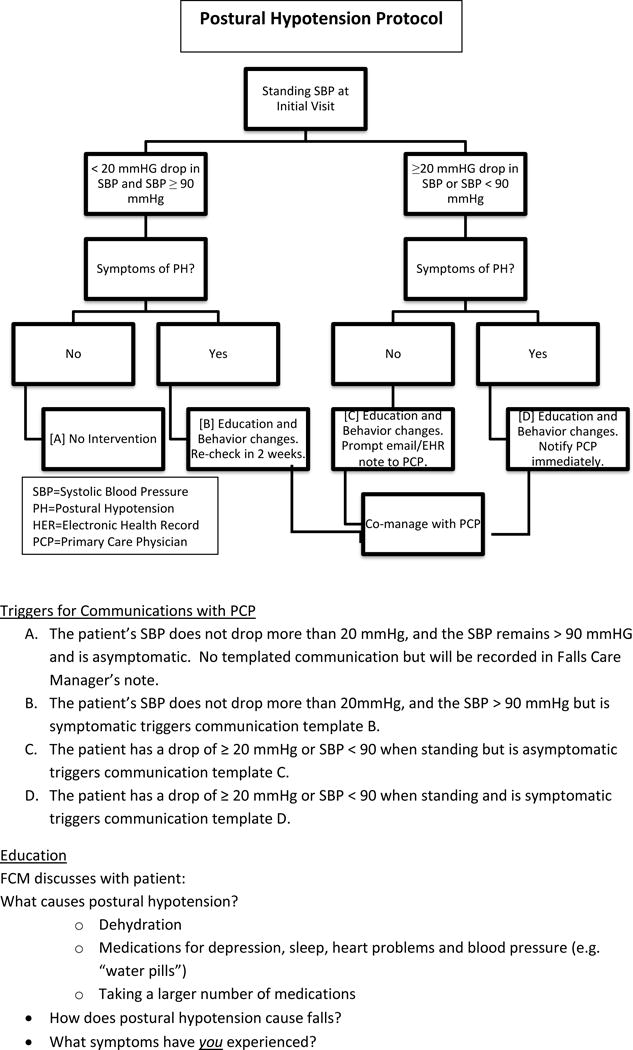
Protocol for one fall risk factor addressed in STRIDE: Postural Hypotension
Medications
The FCM reviews the patient’s medications to detect:
Fall risk increasing drugs (FRIDs) – including benzodiazepines, first generation antihistamines, skeletal muscle relaxants, long acting hypoglycemic agents, and tertiary tricyclic antidepressants
Drug-related side effects that may increase the risk falling – including feeling unsteady, dizzy, drowsy, foggy or sleepy
Medications without a clear indication
Medication adherence problems
Increased fall risk due to the patient’s use of alcohol
If any are present, the FCM reports concerns about these medication issues to the site Pharmacist or the SCD who then communicates any recommendations to the PCP, who, in turn, communicates any medication changes back to the FCM.
Strength, Gait and Balance impairment
Based on the patient’s SPPB results, cognitive function, pain level and preferences, the FCM recommends a course of evidence-based exercise:19 outpatient or home health physical therapy, community-based exercise programs, or home-exercises based on the Otago exercise program.20
Postural Hypotension
Any of the following abnormalities associated with changing from lying to standing position indicate a need for further investigation and treatment:
A drop in systolic blood pressure of more than 20 mmHg
A systolic blood pressure of less than 90 mmHg when standing
No compensatory rise in heart rate when BP drops 20 mmHg or more
Symptoms of lightheadedness or dizziness and 1 or 2 is present.
Feet and Footwear
Foot-related risk factors include foot pain, reduced range of motion, numbness, weakness of toes and/or ankles and deformities such as bunions, hammertoes and long toenails. Footwear-related risks include walking barefoot, in slippers, or in shoes that have inadequate fixation, high and/or narrow heels, or smooth, thick and/or soft soles. The FCM may initiate referrals to podiatry for nail and foot care and to other specialists for shoe and orthotic interventions.
Home Safety
Based on the completed PVQ and home safety checklist, the FCM evaluates the need for and makes a referral, when appropriate, to an occupational therapist for a home safety assessment – or recommends needed home safety modifications, such as nightlights or bathroom grab bars.
Osteoporosis and Vitamin D
The assessment determines whether patients are currently receiving treatment for osteoporosis and, if so, for how long. Consistent with the National Osteoporosis Foundation guidelines,21 if not currently receiving treatment, the FCM determines whether the patient has osteoporosis as determined by a bone mineral density (BMD) test or a history of a “minimal trauma” fracture. If the patient has osteopenia or there is no BMD, then the FRAX risk calculator6 is used to determine recommendations for treatment.22 Supplementation with calcium and vitamin D is recommended for all patients per Institute of Medicine recommendations.23
Visual impairment
The FCM reviews the patient’s history to identify any history of cataracts, macular degeneration, glaucoma or visual loss – and to determine whether a visit with an eye doctor has occurred during in the past year. Recommendations are made accordingly.
Fidelity
Standardized training, implementation and monitoring ensure that the STRIDE intervention is delivered consistently across all sites. Each FCM has been observed performing patient assessments and their clinical notes have been reviewed periodically for accuracy and comprehensiveness. In addition, each FCM was monitored making follow-up calls to patients (acted by a member of the study’s Patient and Stakeholder Council) and received standardized feedback on her motivational interviewing techniques. FCMs from all sites participate in weekly conference calls to discuss protocol or implementation issues. All FCMs use the same software for recording fall risks, recommendations and interventions, further ensuring that the STRIDE protocols are implemented consistently. Similarly, on-site training was provided to the physical therapists and community partners who provide exercise interventions at each practice site, and community-based exercise programs were vetted to ensure that they provide evidence-based care.
Follow-up and Study Outcomes
Follow-up is conducted according to patients’ individualized Care Plans, but at a minimum includes formal visits six months following the initial assessment and then annually. The six-month follow-up visit focuses on Care Plan evaluation during a scheduled telephone visit unless patients have had challenges implementing their Care Plan; had falls; or had changes in their medical, functional, or mobility status. Annual visits also include re-assessments of all fall risks, as well as Care Plan evaluations and revisions, as needed. Collection of study outcomes is not part of the STRIDE intervention. The primary study outcome is time to first serious fall-related injury, defined as falls leading to medical attention, including non-vertebral fractures, joint dislocation, head injury, lacerations, and other major sequelae (e.g., rhabdomyolysis, internal injuries, hypothermia). Secondary outcomes include all fall injuries and all falls, defined as an event in which a person unintentionally comes to rest on the ground or other lower level not as a result of a major intrinsic event or an overwhelming external hazard.
DISCUSSION
Despite the importance of preventing falls in the older population and evidence to support the efficacy of interventions to reduce the risk of falling,6 efforts to integrate fall-preventive interventions into the routine care of older patients have lagged.24 National strategies, such as the Centers for Disease Control’s “Stopping Elderly Accidents, Deaths & Injuries” (STEADI) initiative,25 have assembled educational materials for patients and health care providers but their integration into practice on a system level has been inconsistent. The STRIDE intervention, embedded in the context of a pragmatic trial, is an attempt to engage health care systems in evaluating and modifying risk factors for serious falls-related injuries by changing the care of older persons who are at risk of these injuries. It utilizes principles of co-management, in this instance by registered nurses and PCPs, that have been demonstrated to be effective in improving the quality of care and the clinical outcomes of chronic conditions.7, 26, 27, 28 STRIDE also partners with community-based fall prevention programs that have been found to reduce falls. Moreover, the intervention actively engages patients in their care through motivational interviewing and attention to risk factors that are their initial and subsequent highest priorities.
Most trials of multifactorial interventions to reduce serious falls-related injuries (the focus of STRIDE) have been conducted in settings where research staff have administered the interventions without integrating them into patients’ routine clinical care.29 In contrast, the STRIDE intervention is embedded in clinical practice, including PCPs and other clinical professionals (e.g., pharmacists and physical therapists). All STRIDE components are standard components of clinical care that have been protocolized to provide guidance for the FCMs and to ensure that the intervention is delivered uniformly across clinical sites. The intervention also requires the training and supervision of FCMs. For the purposes of this trial, supervision has been provided nationally, as well as locally. However, this supervision has been designed so that it can be provided at local sites. The STRIDE intervention is also consistent with recommendations for optimizing the role of registered nurses as partners in primary care.30
Whether the STRIDE intervention will reduce serious-falls related injuries remains to be determined. The STRIDE pragmatic trial began enrolling patients in in July 2015 and completed enrollment in March 2017. Although the results of the study will not be available until late 2019, the design and implementation of a standardized intervention that systematically assesses and modifies eight major risk factors for falling suggests that the intervention is feasible in different health systems serving diverse populations.
Supplementary Material
Supplementary Acknowledgments S1: The STRIDE Study Team and Funding Support
Acknowledgments
Funding:
PCORI, National Institute on Aging
Rosanne M. Leipzig: Receiving salary support from grant for this study
Lisa Quintiliani: Lisa Quintiliani is employed by Boston University and has grant funding from the NIH and foundations. She has also served as a Consultant to the STRIDE study.
Sponsor’s Role:
A representative of the sponsor is one of the authors of the paper and was involved in design and preparation of the paper.
Footnotes
Conflict of Interest:
David B. Reuben: NONE
Priscilla K. Gazarian: none
Neil Alexander: none
Katy LB Araujo: none
Dorothy Baker: none
Jonathan F. Bean: none
Chad E Boult: none
Peter A Charpentier: none
Pamela W Duncan: NONE
Nancy Latham: none
Thomas Storer: none
Siobhan McMahon: none
Author Contributions:
David B. Reuben: concept design, acquisition of data, analysis and interpretation. Preparation of manuscript.
Priscilla K. Gazarian: Preparation of the manual of procedures to guide FCMs in implementation and fidelity of intervention.
Neil Alexander: concept design, acquisition of data, analysis and interpretation. Preparation of manuscript.
Katy LB Araujo: Software development, electronic data capture and risk profile generate modules
Dorothy Baker: concept design, acquisition of data, analysis and interpretation. Preparation of manuscript.
Jonathan F. Bean: concept design, acquisition of data, analysis and interpretation. Preparation of manuscript.
Chad Boult: Developed original concept and general design, consulted on definition of intervention, edited the manuscript
Peter A Charpentier: Software Developer, electronic data capture and risk profile generator modules.
Pamela W Duncan: study design, intervention design and training.
Nancy Latham: I was involved in the concept and design, acquisition of subjects and preparation of the manuscript.
Rosanne M. Leipzig: concept design, acquisition of data, analysis and interpretation. Preparation of manuscript.
Lisa Quintiliani: contributed to the design and implementation of the intervention and preparation of the manuscript.
Thomas Storer: concept design, analysis and interpretation. Preparation of manuscript.
Siobhan McMahon: assisted with the design and preparation of the manuscript.
References
- 1.https://www.cdc.gov/homeandrecreationalsafety/Falls/adultfalls.html accessed 12/30/2016
- 2.Kramarow E, Chen LH, Hedegaard H, Warner M. NCHS data brief. 199. Hyattsville, MD: National Center for Health Statistics; 2015. Deaths from unintentional injury among adults aged 65 and over: United States, 2000–2013. [PubMed] [Google Scholar]
- 3.https://ihis.ipums.org/ihis/resources/IHIS_Data_Brief_No_3.pdf accessed 1230/2016
- 4.Stevens JA, Ballesteros MF, Mack KA, Rudd RA, DeCaro E, Adler G. Gender differences in seeking care for falls in the aged Medicare Population. Am J Prev Med. 2012;43:59–62. doi: 10.1016/j.amepre.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 5.Jennings LA, Reuben DB, Kim SB, Keeler E, Roth CP, Zingmond DS, Wenger NS, Ganz DA. Targeting a high-risk group for fall prevention: strategies for health plans. Am J Manag Care. 2015 Sep 1;21(9):e519–26. [PMC free article] [PubMed] [Google Scholar]
- 6.Hastings SN, Sloane R, Morey MC, Pavon JM, Hoenig H. Assisted early mobility for hospitalized older veterans: preliminary data from the STRIDE program. J Am Geriatr Soc. 2014 Nov;62(11):2180–4. doi: 10.1111/jgs.13095. Epub 2014 Oct 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stevens JA, Burns ER. A CDC Compendium of Effective Fall Interventions: What Works for Community-Dwelling Older Adults. 3rd. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2015. [Google Scholar]
- 8.Ganz DA, Koretz BK, McCreath HE, et al. Nurse Practitioner Co-Management for Patients in an Academic Geriatric Practice. Am J Manag Care. 2010;16(12):e343–e355. [PMC free article] [PubMed] [Google Scholar]
- 9.Baker DI, King MB, Fortinsky R, Graff LG, Gottschalk M, Acampora D, Preston J, Brown CJ, Tinetti ME. Dissemination of an Evidence-based Multi-component Fall Risk Assessment and Management Strategy throughout a Geographic Area. J Am Geriatr Soc. 2005;53:675–680. doi: 10.1111/j.1532-5415.2005.53218.x. [DOI] [PubMed] [Google Scholar]
- 10.Tinetti M, Baker DI, King M, Gottschalk M, Murphy TE, Acampora D, Carlin BP, Leo-Summers L, Allore H. Effect of Dissemination of Evidence in Reducing Injuries from Falls. New England Journal of Medicine. 2008;359:252–61. doi: 10.1056/NEJMoa0801748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beckett CD, Kipnis G. Collaborative communication: integrating SBAR to improve quality/patient safety outcomes. J Healthc Qual. 31(5):19–28. doi: 10.1111/j.1945-1474.2009.00043.x. http://www.ncbi.nlm.nih.gov/pubmed/19813557. Accessed January 24, 2017. [DOI] [PubMed] [Google Scholar]
- 12.https://www.shef.ac.uk/FRAX/ accessed 12/30/2016
- 13.Guralnik JM, Ferrucci L, Pieper CF, et al. Lower Extremity Function and Subsequent Disability: Consistency Across Studies, Predictive Models, and Value of Gait Speed Alone Compared with the Short Physical Performance Battery. J Gerontol Med Sci. 2000;55A:M221–M231. doi: 10.1093/gerona/55.4.m221. [DOI] [PubMed] [Google Scholar]
- 14.Borson S, Scanlan J, Brush M, Vitaliano P, Dokmak A. The mini-cog: a cognitive ‘vital signs’ measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry. 2000 Nov;15(11):1021–7. doi: 10.1002/1099-1166(200011)15:11<1021::aid-gps234>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 15.McMahon SK, Wyman JF, Belyea MJ, Shearer N, Hekler EB, Fleury J. Combining Motivational and Physical Intervention Components to Promote Fall-Reducing Physical Activity Among Community-Dwelling Older Adults: A Feasibility Study. Am J Health Promot. 2016 Nov;30(8):638–644. doi: 10.4278/ajhp.130522-ARB-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moore SM, Schiffman R, Waldrop-Valverde D, et al. Recommendations of Common Data Elements to Advance the Science of Self-Management of Chronic Conditions. Journal of Nursing Scholarship. 2016;48(5):437–447. doi: 10.1111/jnu.12233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O’Halloran PD, Blackstock F, Shields N, et al. Motivational interviewing to increase physical activity in people with chronic health conditions: a systematic review and meta-analysis. Clinical Rehabilitation. 2014;28(12):1159–1171. doi: 10.1177/0269215514536210. [DOI] [PubMed] [Google Scholar]
- 18.Purath J, Keck A, Fitzgerald CE. Motivational interviewing for older adults in primary care: a systematic review. Geriatric Nursing (New York, NY) 2014;35(3):219–224. doi: 10.1016/j.gerinurse.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 19.Conn VS, Ruppar TM, Chase JA, Enriquez M, Cooper PS. Interventions to Improve Medication Adherence in Hypertensive Patients: Systematic Review and Meta-analysis. Current hypertension reports. 2015;17(12):94. doi: 10.1007/s11906-015-0606-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brown LG, Ni M, Schmidt CT, Bean JF. Evaluation of an Outpatient Rehabilitative Program to Address Mobility Limitations Among Older Adults. Am J Phys Med Rehabil. 2017 Jan 11; doi: 10.1097/PHM.0000000000000682. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Campbell AJ, Robertson MC. Otago exercise programme to prevent falls in older adults. http://www.acc.co.nz/PRD_EXT_CSMP/groups/external_providers/documents/publications_promotion/prd_ctrb118334.pdf.
- 22.Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, Lindsay R, National Osteoporosis Foundation Clinician’s Guide to Prevention and Treatment of Osteoporosis. Osteoporos Int. 2014 Oct;25(10):2359–81. doi: 10.1007/s00198-014-2794-2. Erratum in: Osteoporos Int. 2015 Jul;26(7):2045–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, Lindsay R, National Osteoporosis Foundation Clinician’s Guide to Prevention and Treatment of Osteoporosis. Osteoporos Int. 2014 Oct;25(10):2359–81. doi: 10.1007/s00198-014-2794-2. Erratum in: Osteoporos Int. 2015 Jul;26(7):2045–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and CalciumRoss AC, Taylor CL, Yaktine AL, et al., editors. Dietary Reference Intakes for Calcium and Vitamin D. Washington (DC): National Academies Press; US: 2011. Available from: https://www.ncbi.nlm.nih.gov/books/NBK56070/ [DOI] [PubMed] [Google Scholar]
- 25.Phelan EA, Aerts S, Dowler D, Eckstrom E, Casey CM. Adoption of Evidence-Based Fall Prevention Practices in Primary Care for Older Adults with a History of Falls. Frontiers in Public Health. 2016;4:190. doi: 10.3389/fpubh.2016.00190.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.https://www.cdc.gov/steadi/ accessed 12/30/2016
- 27.Shaw RJ, McDuffie JR, Hendrix CC, Edie A, Lindsey-Davis L, Nagi A, et al. Effects of Nurse-Managed Protocols in the Outpatient Management of Adults With Chronic Conditions: A Systematic Review and Meta-analysis. Ann Intern Med. 2014;161:113–121. doi: 10.7326/M13. [DOI] [PubMed] [Google Scholar]
- 28.Reuben DB, Ganz DA, Roth CP, McCreath HE, Ramirez KD, Wenger NS. Effect of nurse practitioner comanagement on the care of geriatric conditions. J Am Geriatr Soc. 2013 Jun;61(6):857–67. doi: 10.1111/jgs.12268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Archer J, Bower P, Gilbody S, Lovell K, Richards D, Gask L, Dickens C, Coventry P. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev. 2012 Oct 17;10:CD006525. doi: 10.1002/14651858.CD006525.pub2. [DOI] [PubMed] [Google Scholar]
- 30.Guirguis-Blake JM, Michael YL, Perdue LA, Thompson JH, Coppola EL. Interventions to Prevent Falls in Older Adults: A Systematic Review for the US Preventive Services Task Force. Rockville, MD: Agency for Healthcare Research and Quality; 2016. (Evidence Synthesis No. XXX. AHRQ Publication No. XXX). [PubMed] [Google Scholar]
- 31.Josiah Macy Jr. Foundation, editor. Recommendations from the Macy Foundation Conference on Preparing Registered Nurses for Enhanced Roles in Primary Care. Atlanta: 2016. Registered Nurses: Partners in Transforming Primary Care; pp. 1–15. http://www.macyfoundation.org/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Acknowledgments S1: The STRIDE Study Team and Funding Support


