Abstract
Purpose
A basicervical femoral fracture is defined as a fracture of base of neck of femur that occurs medially from intertrochanteric line above lesser trochanter. In this study, we intended to evaluate radiological and clinical results of basicervical femoral fractures treated by intramedullary nailing.
Materials and Methods
Fifteen patients, who underwent intramedullary nailing among 50 patients, out of 50 who were diagnosed with basicervical femoral fractures from July 2012 to May 2015 were studied. All of 15 patients' fracture were two-part basicervical fractures. Using radiography, we characterized the: i) state of reduction, ii) location of the lag screw, iii) tip apex distance (TAD), and iv) sliding distance of lag screw and bone union. Additionally, we performed clinical assessment before injury and at final follow-up.
Results
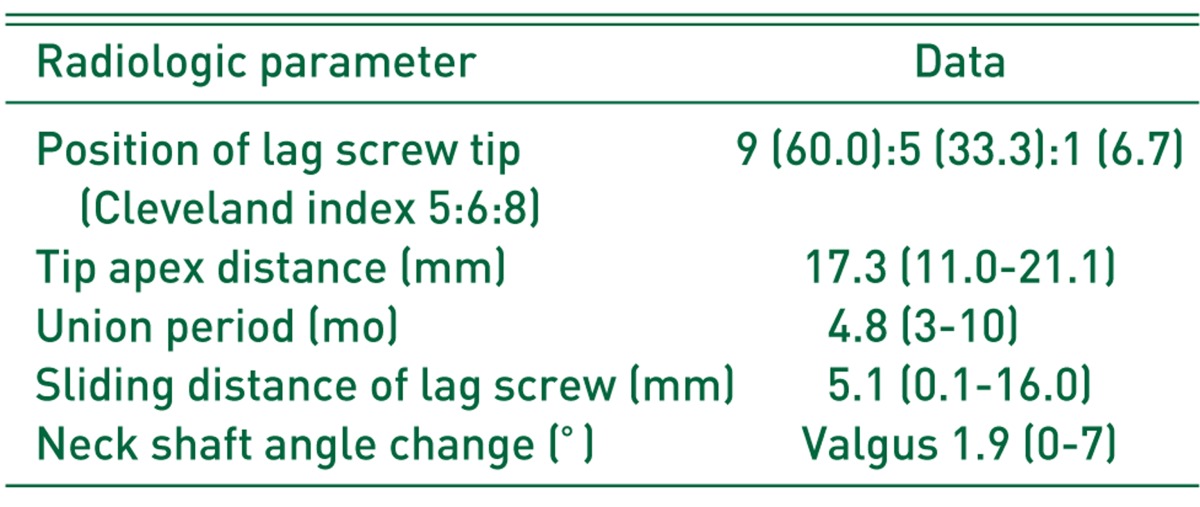
In radiological assessment, we achieved acceptable reduction state in all patients. All lag screws were fixated on appropriate locations. Mean TAD was 17.3 mm (11.0–21.1 mm), which showed insertion point of <25 mm in all cases. The mean sliding distance of the lag screw was 5.1 mm (0.1–16.0 mm) at the final follow-up. The mean bone union period was 4.8 months (3–10 months) with achieving in all cases. In clinical assessment, Harris hip score, visual analogue scale score and Western Ontario and McMaster Universities Arthritis Index score, all of them significantly improved postoperatively compared with preoperative scores (P<0.05).
Conclusion
In elderly patients with basicervical femoral fractures, treatment with intramedullary nailing showed satisfactory results, considered to be a useful method if performed with skilled technique.
Keywords: Femur, Basicervical fractures, Intramedullary fracture fixation
INTRODUCTION
Proximal femoral fractures include intertrochanteric fractures, femoral neck fractures1), and basicervical fractures2). Basicervical fractures, due to their anatomical nature (i.e., occurring between the base of the femoral neck and the intertrochanteric region) remains a controversial fracture type which can be regarded as either extracapsular or intracapsular one3,4,5). Parker et al.6) defined it as a fracture in which the fracture line runs along the line of the anterior/inferior attachment of the joint capsule. Blair et al.3) described it as a fracture in which the fracture line moves through the base of the femoral neck at its junction with the intertrochanteric region. A variety of options for fixation may be considered because the classification of basicervical fracture is unclear.
Internal fixation using a compression hip screw and an intramedullary nail may be considered as a treatment option for basicervical femoral fractures7,8). It has been suggested that basicervical fractures are more unstable than intertrochanteric ones3,9,10), and may manifest insufficient functional outcomes when fixed with dynamic sliding hip screws4,11,12,13). With the recent development of a variety of intramedullary devices, intramedullary nails are less invasive than dynamic hip screws (DHS), which may result in shorter operation time and smaller transfusion volume, and have shown favorable clinical results14).
The aim of this study was to retrospectively evaluate clinical and radiological outcomes of basicervical femoral fractures treated with intramedullary nailing.
MATERIALS AND METHODS
1. Subjects
We reviewed 50 patients (6.2%) diagnosed with basicervical femoral fractures among 810 patients diagnosed with proximal femoral fractures in our institution from July 2012 to May 2015. Of these 50 patients, 15 were treated with intramedullary nailing and followed up for at least 2 years (Fig. 1). This study retrospectively reviewed these patients after acheiving approval of institutional review board from our institution (No. WKUH2017-05-003-002).
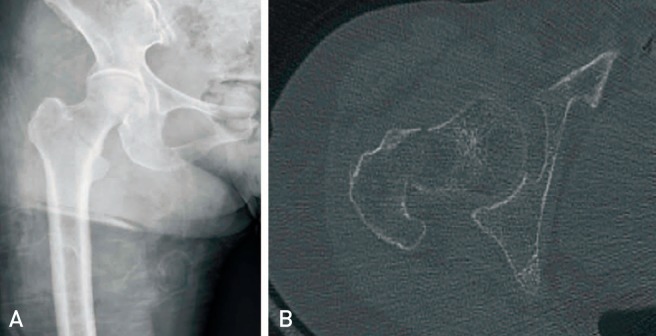
Fig. 1. Images of an female patient aged 90 years old. (A) Anteroposterior X-ray shows a basicervical fracture in the right hip that had occurred after a simple fall. (B) Computed tomography shows the axial section of fracture level.
Basicervical femoral fractures were defined as two-part fractures between the base of the femoral neck and the intertrochanteric region on computed tomography scans. Intramedullary nailing was performed in patients satisfying this definition with a minimum follow-up of 2 years, excluding 35 patients with ipsilateral fractures, extension of the fracture lines into the inferior lesser trochanter and arthroplasty after being diagnosed with basicervical fractures. The mean age of the subjects was 78.14 years old (range, 39–92 years). Six were males and 9 were females. The average follow-up period was 25.2 months (range, 24–31 months). Since the subjects were mostly over 65 years old, 10 of 15 cases had underlying medical conditions including heart failure, arrhythmia, pneumonia, chronic renal failure, cardiovascular disease and others. Four patients were diagnosed with dementia. Ambulation status was normal in 13 cases and 2 patients used a cane walker for ambulation. Based on American Society of Anesthesiologists (ASA) scores for the preoperative risk assessment of anesthesia, 9 cases were classified as ASA II, 5 as ASA III, and 1 as ASA IV. The cause of injury was slip down (n=11), fall down (n=3) and traffic accident (n=1). Dual energy X-ray absorptiometry was performed preoperatively in all cases. The average T-score of the femoral trochanteric area was −2.52 (range, −4.4 to −1.8). Nine cases had T-score of −2.5 or less indicating the presence of osteoporosis (Table 1).
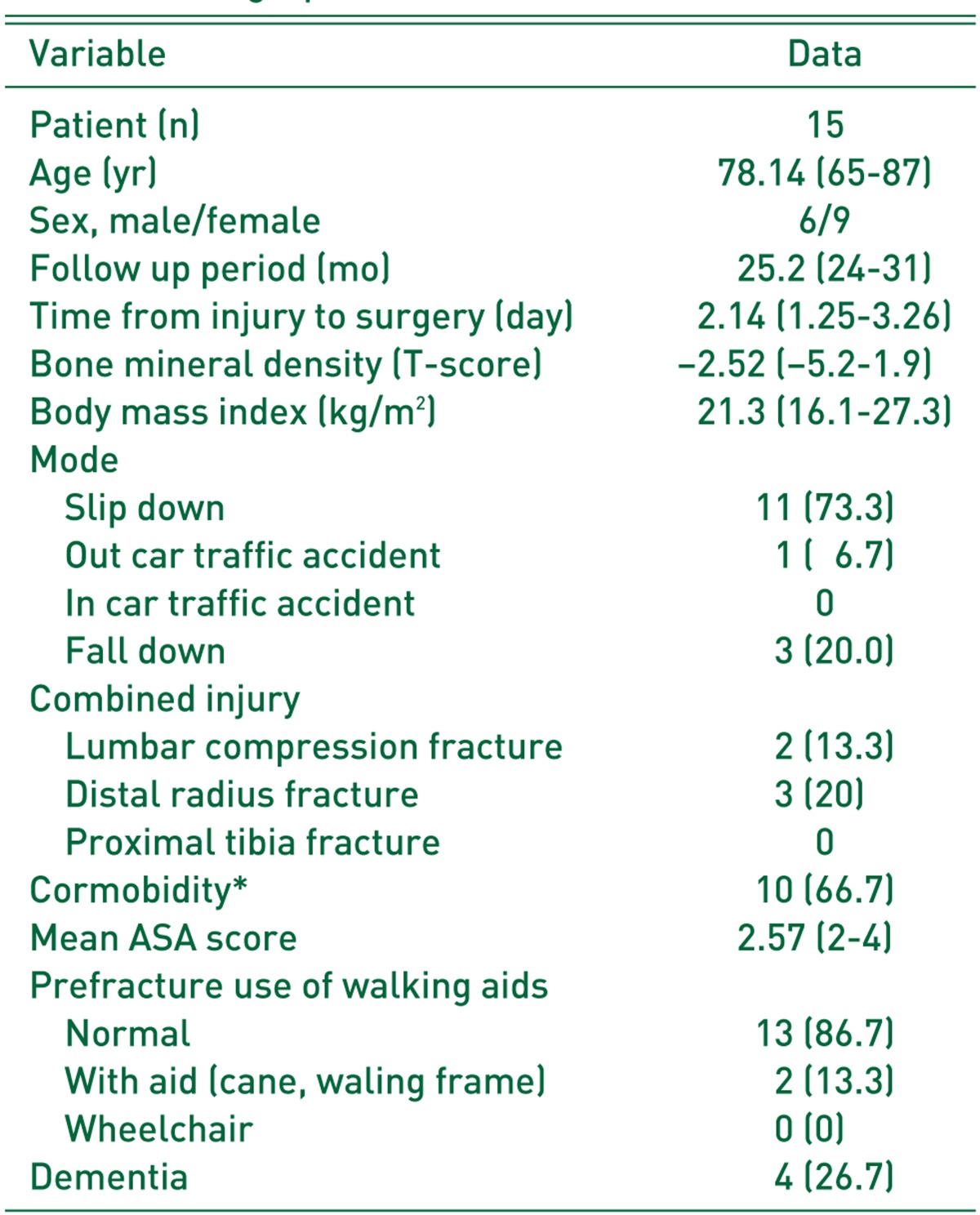
Table 1. Demographic Data of Patients.
Values are presented as number only, mean (range), or number (%).
ASA, American Society of Anesthesiologists.
* Heart failure, arrhythmia, pneumonia, chronic kidney disease, cardiovascular disease.
2. Surgical Methods and Rehabilitation
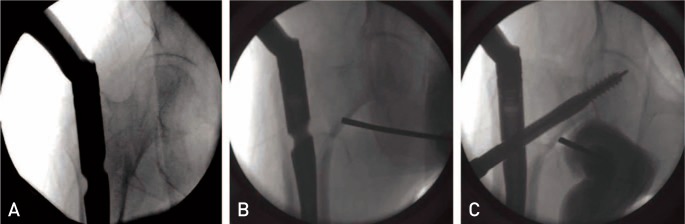
Reduction was attempted on an operating table after spinal anesthesia, and reduction status was examined using the C-arm image intensifier. The position of the femoral head was confirmed with anteroposterior views using the C-arm and then a line was marked on the skin. After making a small incision at the 3 to 5 cm inferior to the distal end of the line, a Steinmann pin with handle was inserted at 45° and placed above the lesser trochanter to the medial side of the fracture line on anteroposterior views, and the placement of the pin at the anterior femoral head was confirmed on lateral views. After obtaining anatomical reduction of the fracture site by moving the Steinmann pin as a joystick, an intramedullary nail (Gamma3 CMN; Stryker, Kalamazoo, MI, USA) was inserted by preventing rotation or medial or lateral displacement of the femoral head to the distal fragment. The Steinmann pin was used at the end to prevent rotational deformity of the femoral head during reaming and lag screw fixation. Distal lag screws were inserted in all cases. Lag screw insertion was placed into the center-center or central-inferior position on the femoral head (Fig. 2).
Fig. 2. During insertion of an intramedullary nail's massive empennage, there is a distraction effect (V effect) on the trochanteric fragments, which increases the incidence of hip varus deformity or nonunion (A). With the assistant holding the proximal-medial part of basicervical fracture line in position (B), a reamer with high rotation speed can be used to enlarge the proximal femur; this diminishes the V effect and lag screw malposition (C).
Sitting was allowed from the first postoperative day, and wheelchair usage and partial weight bearing was instructed between the 3rd and the 7th postoperative days depending on the degree of reduction, systemic condition and pain. Partial weight bearing with a walker was allowed from the 2nd postoperative week and full weight bearing from the 6th postoperative week.
3. Radiological and Clinical Assessment
Upon radiological assessment, reduction status was categorized into good, acceptable and poor by determining the degree of recovery of the fracture immediately after the surgery based on the classification criteria of Fogagnolo et al15). Using the Cleveland index16), the location of the lag screw within the head was divided into nine sections by dividing the femoral head into three parts on the anteroposterior and lateral X-ray images. Tip apex distance (TAD)17) was the sum of the distance from the tip of the lag screw to the apex of the femoral head on the postoperative anteroposterior and lateral radiographs. The migration distance of the lag screw was calculated by measuring the difference in the distance between the tip of the lag screw and the lateral cortex on the final follow-up radiographs after bone union. Since the degree of hip rotation and image ratio may differ upon measurement, the difference was calculated by taking the ratio of screw length measured on radiographs taken immediately after the surgery and at the last follow-up as a correction factor. Furthermore, union time was confirmed through additional radiographic examination. The femoral neck shaft angles were measured immediately after the surgery and at the last follow-up, and were compared, and the difference in the actual anatomical neck shaft angles of the healed femur was assessed. The degree of postoperative reduction was evaluated as an indirect index; greater than 10° angular deformation was classified as “poor”.
Upon clinical assessment, the modified Harris hip score and Western Ontario and McMaster Universities Arthritis Index (WOMAC) scores were measured at the final follow-up, and the Koval classification18) was used to evaluate pre- and postoperative mobility. In addition, recovery of activities of daily living (ADL) was determined using the Functional Recovery Scale (Koval and Zuckerman)19). The operation time and the amount of blood loss were collected and analyzed based on medical records.
4. Statistical Analysis
Statistical analysis was performed using IBM SPSS Statistics ver. 23.0 for Windows Release (IBM Co., Armonk, NY, USA) with the Wilcoxon test to compare pre- and postoperative changes. P-values of less than 0.05 were considered statistically significant.
RESULTS
1. Radiological Outcomes
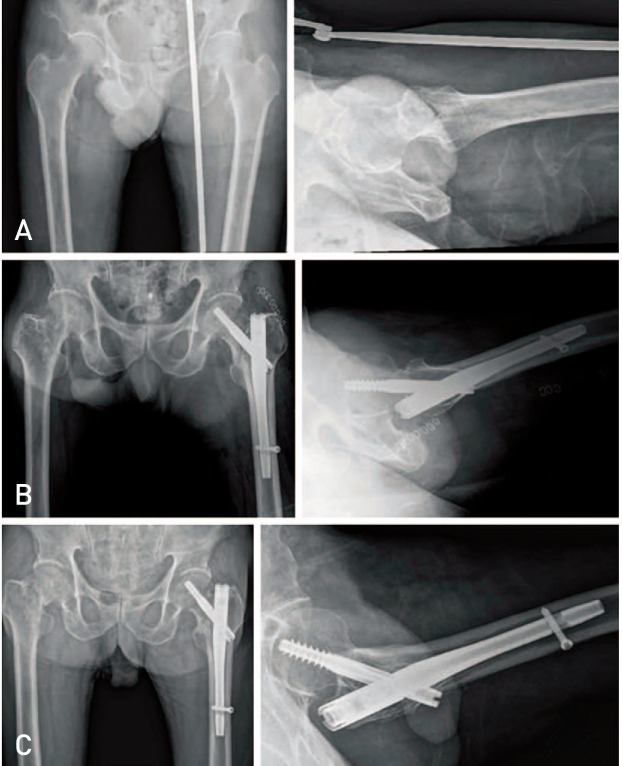
Based on the classification developed by Fogagnolo et al.15), reduction state as determined by radiological assessment immediately after surgery was satisfactory in all cases (good, 12; acceptable, 3). The position of the lag screw was located at Cleveland index16) 5, 6 and 8 regions in 9, 5, and 1 cases, respectively, and a lag screw was properly placed in one case (Fig. 3). TAD was measured from the tip of the lag screw to the apex of the femoral head on the postoperative anteroposterior and lateral radiographs. The mean TAD was 17.3 mm (range, 11–21.1 mm) and the TAD was less than 25 mm in all cases. The average sliding distance of the lag screws was 5.1 mm (range, 0.1–16 mm) at the final follow-up. The mean bone union period was 4.8 months (range, 3–10 months), and complete bone union was achieved (Fig. 4). The change in the mean neck shaft angle on postoperative and bone union radiographs was 1.9° (range, 0°–7°), and neck-shaft angle difference was less than 10° (Table 2). No postoperative mechanical complications occurred (e.g., perforation of the femoral head by the screw, excessive sliding of the lag screw, varus deformity, intraoperative lateral wall fracture, or avascular necrosis of the femoral head).
Fig. 3. For the Cleveland index, the femur head is divided into nine zones in the axial view to classify the position of the cervical screw.
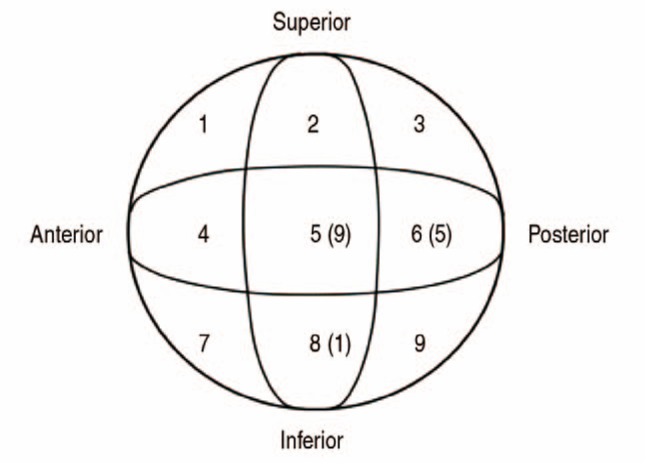
Fig. 4. (A) Initial radiograph in 77-year-old female patient show a basicervical fracture in the left hip. (B) Immediate postoperative radiograph shows that fixation was done with Gamma. (C) Radiograph at 12 months shows the bone union at the fracture site.
Table 2. Radiologic Results of Cephalomedullary Nailing.
Values are presented as number (%) or mean (range).
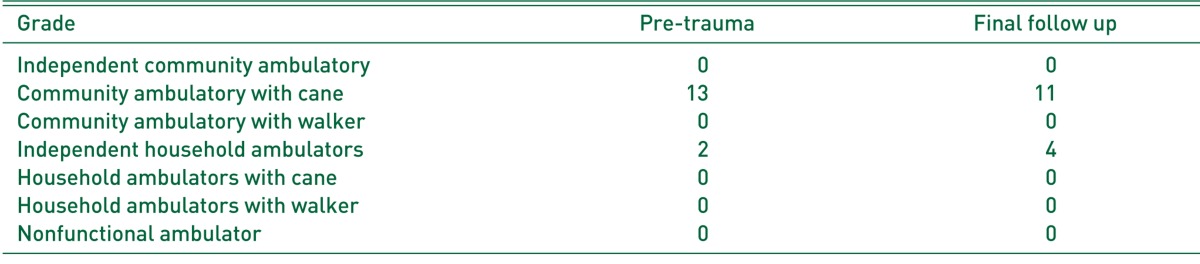
2. Clinical Outcomes
The mean duration of operation from skin incision to wound suturing was 35 minutes (range, 25–55 minutes), and the average blood loss was 204.28 mL (range, 50–350 mL). Both the modified Harris hip and WOMAC scores improved postoperatively compared with pre-injury status, and 13 (86.7%) patients were community ambulators who were able to perform independent outdoor ambulation, excluding 2 patients who were able to ambulate independently indoor or using a cane or walker. In walking ability evaluation at the final follow-up, 11 (73.3%) cases were community ambulators with independent outdoor ambulation, 4 (26.7%) were household ambulators with limited walking ability, and 2 became household ambulators who were initially community ambulators before the surgery (Table 3). During the pre-injury assessment, all patients were able to perform ADL, but only 13 patients had the ability to perform instrumental ADL (IADL). Postoperatively, all 15 patients were able to perform ADL, while 13 of 15 had no difference in IADL compared to preoperative status.
Table 3. The Changes of Walking Ability at Preoperative and Final Follow Up (by Koval).
DISCUSSION
The definition and optimal treatment approach of basicervical fractures remain controversial. Basicervical fractures are described as the ones occurring along the lines between the proximal femoral neck and the intertrochanteric region and regarded as an intermediate form between femoral neck and intertrochanteric fractures due to its anatomical location1). Internal fixation using multiple cancellous screws or sliding screw devices2,3) or bipolar hemiarthroplasty are considered as treatment options. Although bipolar hemiarthroplasty may result in faster time to ambulation, no fracture-related complication and avoidance of reoperation, this modality also has greater risk in surgical procedures compared to intramedullary nailing (e.g., greater blood loss, loosening, erosion of acetabular cartilage, infection dislocation and others)7,8).
Su et al.20) recommended that basicervical fractures should be treated as unstable femoral trochanteric fractures since collapses occur more commonly in basicervical fractures than in intertrochanteric fractures when treated with DHS with antirotational screw. According to various reports in the literature, favorable surgical outcomes were achieved when treating basicervical fractures as intertrochanteric fractures using a compression hip screw or a cephalomedullary nail. Upon careful examination of 1,624 cases diagnosed with basicervical fractures on plain X-rays in a study by Saarenpää et al.2), 51 were transcervical fractures, 30 were basicervical fractures and 27 were trochanteric fractures. Of the 30 basicervical fracture cases, 14 were treated as extracapsular fractures and led to better results than the 16 treated as intracapsular fractures. Deneka et al.4) suggested that good outcomes were obtained when a basicervical fracture occurring at the intracapsular femoral neck and extracapsular trochanteric region was treated as a trochanteric fracture using dynamic compression screws or cephalomedullary nails. Watson et al.21) yielded bone union without any complication in 5 of 11 hips with double segmental fracture and cut-out of the femoral head in 5 and non-union in one among 6 hips with anatomical reduction, and recommended that the use of intramedullary nailing is inappropriate for treating basicervical fractures. They hypothesized that the cause of a fracture non-union was the contact of the nail at the superior and inferior aspects of the basicervical fracture line leading to interference with the sliding of lag screw in case of nail insertion at the tip of the greater trochanter. In most patients, the common cause of failure was cut-out due to excessive sliding of the lag screw rather than non-union. Even though their radiographic assessment revealed anatomical reduction in double segmental basicervical fractures considered unstable, distal screw fixation was neither performed nor addressed. The authors of this study carried out anatomical reduction and screw fixation in the distal femur like in the study of Watson et al21).
Skála-Rosenbaum et al.22) suggested that when performing intramedullary nailing, distal screw fixation is unnecessary in stable fractures, but needed in unstable proximal femoral fractures to prevent rotational deformity of the distal fragment and shortening of the fracture area due to compression force. Moreover, several reports addressed that fixation using dynamic compression screws is more difficult to maintain reduction since basicervical fractures are more unstable than intertrochanteric fractures, and intramedullary nailing may achieve better clinical results11,12,13,14).
In the present study, in order to promote bone union when performing intramedullary nailing for basicervical fractures, the authors did the following: i) in cases of underlying diseases for surgical delay, blood loss was minimized by shortening the time spent on soft tissue contracture and reduction through bone traction at supracondylar area of the femur for the initial 3 days after injury; ii) for displacement of the fracture fragments and accurate positioning of the lag screws, the distal fragment was displaced laterally using a Hohmann retractor or bone hook after traction of the fractured bone during insertion using guide pins and reamers, and fixation was done without the rotation and displacement of the fractured bone while maintaining the reduction by inserting Steinmann pins in the proximal and distal fragments; and iii) we attempted to reduce the TAD to be less than 25 mm. These surgical techniques appear to produce satisfactory clinical results when treating basicervical fracture with no complications.
This study is limited by the retrospective nature of the analysis including the risk of selection bias and may have less statistical significance due to the relatively small sample size. Further studies with a larger sample size are needed to compare radiological and clinical results between the intramedullary nail and DHS.
CONCLUSION
In elderly patients with basicervical femoral fractures, treatment with intramedullary nailing showed satisfactory radiological and clinical results in fracture union at the 2-year follow-up when performed with skilled technique.
ACKNOWLEDGEMENTS
This study was supported by 2017 research fund of Wonkwang University.
Footnotes
CONFLICT OF INTEREST: The authors declare that there is no potential conflict of interest relevant to this article.
References
- 1.Lieberman JR. AAOS comprehensive orthopaedic review. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2009. pp. 597–598. [Google Scholar]
- 2.Saarenpää I, Partanen J, Jalovaara P. Basicervical fracture--a rare type of hip fracture. Arch Orthop Trauma Surg. 2002;122:69–72. doi: 10.1007/s004020100306. [DOI] [PubMed] [Google Scholar]
- 3.Blair B, Koval KJ, Kummer F, Zuckerman JD. Basicervical fractures of the proximal femur. A biomechanical study of 3 internal fixation techniques. Clin Orthop Relat Res. 1994;(306):256–263. [PubMed] [Google Scholar]
- 4.Deneka DA, Simonian PT, Stankewich CJ, Eckert D, Chapman JR, Tencer AF. Biomechanical comparison of internal fixation techniques for the treatment of unstable basicervical femoral neck fractures. J Orthop Trauma. 1997;11:337–343. doi: 10.1097/00005131-199707000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Dossick PH, Dorr LD, Gruen T, Saberi MT. Techniques for preoperative planning and postoperative evaluation of noncemented hip arthroplasty. Tech Orthop. 1991;6(3):1–6. [Google Scholar]
- 6.Parker MJ, Pryor GA, Thorngren KG. Extramedullary fixation of extracapsular fractures. In: Parker MJ, Pryor GA, Thorngren KG, editors. Handbook of hip fracture surgery. Oxford: Butterworth-Heinemann; 1997. pp. 63–90. [Google Scholar]
- 7.Kim KW, Ahn SH. Elderly trochanteric fractures: principles of treatment. J Korean Soc Fract. 1994;7:227–234. [Google Scholar]
- 8.Yoon ES, Min HJ, Suh JS, et al. Comparison of clinical results between bipolar hemiarthroplasty and compression hip screw on unstable intertrochanteric fractures of the femur in elderly patients. J Korean Fract Soc. 2004;17:214–220. [Google Scholar]
- 9.Gill JM, Johnson GR, Sher JL, Kornjaca NA. Biomechanical aspects of the repair of intertrochanteric fractures. J Biomed Eng. 1989;11:235–239. doi: 10.1016/0141-5425(89)90149-0. [DOI] [PubMed] [Google Scholar]
- 10.Ly TV, Swiontkowski MF. Management of femoral neck fractures in young adults. Indian J Orthop. 2008;42:3–12. doi: 10.4103/0019-5413.38574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jones HW, Johnston P, Parker M. Are short femoral nails superior to the sliding hip screw? A meta-analysis of 24 studies involving 3,279 fractures. Int Orthop. 2006;30:69–78. doi: 10.1007/s00264-005-0028-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parker MJ, Handoll HH. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst Rev. 2008;(3):CD000093. doi: 10.1002/14651858.CD000093.pub4. [DOI] [PubMed] [Google Scholar]
- 13.Hu SJ, Yu GR, Zhang SM. Surgical treatment of basicervical intertrochanteric fractures of the proximal femur with cephalomeduallary hip nails. Orthop Surg. 2013;5:124–129. doi: 10.1111/os.12038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tasyikan L, Ugutmen E, Sanel S, Soylemez MS, Ozkan K, Solakoglu C. Short-term results of surgical treatment with cephalomedullary nails for basicervical proximal femoral fractures. Acta Orthop Belg. 2015;81:427–434. [PubMed] [Google Scholar]
- 15.Fogagnolo F, Kfuri M, Jr, Paccola CA. Intramedullary fixation of pertrochanteric hip fractures with the short AO-ASIF proximal femoral nail. Arch Orthop Trauma Surg. 2004;124:31–37. doi: 10.1007/s00402-003-0586-9. [DOI] [PubMed] [Google Scholar]
- 16.Cleveland M, Bosworth DM, Thompson FR, Wilson HJ, Jr, Ishizuka T. A ten-year analysis of intertrochanteric fractures of the femur. J Bone Joint Surg Am. 1959;41-A:1399–1408. [PubMed] [Google Scholar]
- 17.Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77:1058–1064. doi: 10.2106/00004623-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Koval KJ, Skovron ML, Aharonoff GB, Meadows SE, Zuckerman JD. Ambulatory ability after hip fracture. A prospective study in geriatric patients. Clin Orthop Relat Res. 1995;(310):150–159. [PubMed] [Google Scholar]
- 19.Koval KJ, Zuckerman JD. Functional recovery after fracture of the hip. J Bone Joint Surg Am. 1994;76:751–758. doi: 10.2106/00004623-199405000-00018. [DOI] [PubMed] [Google Scholar]
- 20.Su BW, Heyworth BE, Protopsaltis TS, et al. Basicervical versus intertrochanteric fractures: an analysis of radiographic and functional outcomes. Orthopedics. 2006;29:919–925. doi: 10.3928/01477447-20061001-04. [DOI] [PubMed] [Google Scholar]
- 21.Watson ST, Schaller TM, Tanner SL, Adams JD, Jeray KJ. Outcomes of low-energy basicervical proximal femoral fractures treated with cephalomedullary fixation. J Bone Joint Surg Am. 2016;98:1097–1102. doi: 10.2106/JBJS.15.01093. [DOI] [PubMed] [Google Scholar]
- 22.Skála-Rosenbaum J, Bartonícek J, Bartoska R. Is distal locking with IMHN necessary in every pertrochanteric fracture? Int Orthop. 2010;34:1041–1047. doi: 10.1007/s00264-009-0874-2. [DOI] [PMC free article] [PubMed] [Google Scholar]