Vertebral artery stump syndrome is one of the minor causes (1.4%) of ischemic stroke in posterior circulation region.1, 2
A seventy‐five‐year‐old man repeated ischemic stroke three times for 7 days in posterior circulation area. Head magnetic resonance imaging (MRI) of diffusion‐weighted image (DWI) revealed cerebral infarction at right cerebellum around the posterior inferior cerebellar artery (PICA) area (first time; Figure 1), right posterior cerebral artery (PCA) area (second time; Figure 1), and right lateral medullary (third time; Figure 1), respectively. D dimer in serum was 1.2 μg/mL. Abnormal myocardial motion by echocardiogram and atrial fibrillation (Af) by electrocardiogram were not detected. Cerebral angiography, using 4‐French Simons form catheter, revealed to‐and‐fro stagnated flow in right vertebral artery (Figure 2, arrow). Right VA first segment almost occluded (computed tomography angiography; data not shown). Blood flow came in right VA (Figure 3, arrow) through muscle branch of occipital artery (Figure 3, arrow head). The collateral flow of right VA and reverse flow from left VA formed to‐and‐fro stasis. Intravessel red fibrin thrombus was presumed to cause repeatable and multiple cerebral infarctions. Like this presentation case, VA stump syndrome often brings recurrent ischemic stroke in posterior circulation area.1, 2 Although endovascular intervention on VA origin occlusion is one of surgical therapy,2 wide‐range occlusion or dissection of VA is challenging to treat. Not antiplatelet but anticoagulation therapy is useful to prevent stroke by VA stump syndrome.3 Because of long lesion of right VA, this patient started oral anticoagulant therapy (warfarin) without endovascular intervention.3 Recurrent infarction was not observed.
Figure 1.
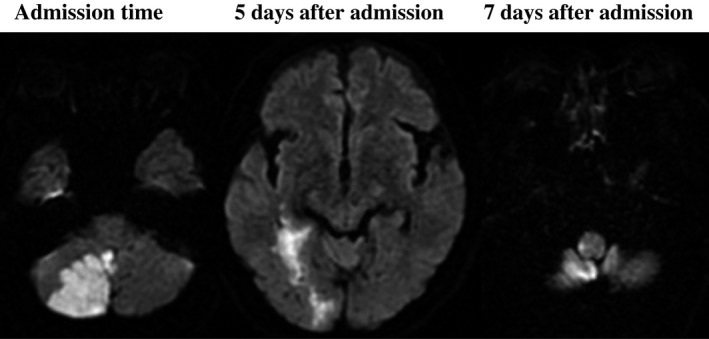
Diffusion‐weighted image (DWI) magnetic resonance imaging (MRI) on head. Cerebral infarction at right cerebellum around the posterior inferior cerebellar artery (PICA) area (first time), right posterior cerebral artery (PCA) area (5 days postadmission), and right lateral medullary (7 days postadmission) was observed, respectively
Figure 2.
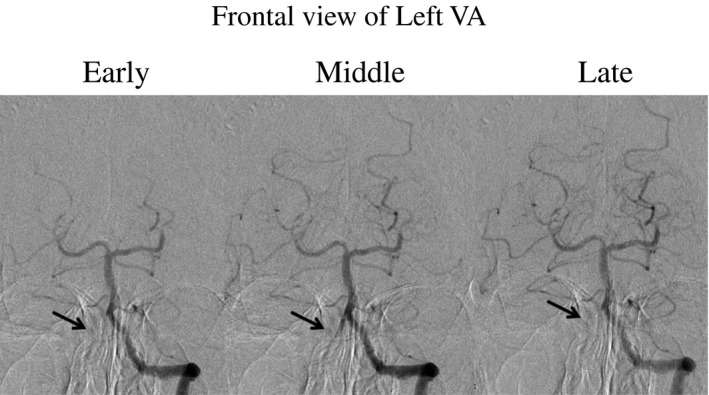
Frontal view of cerebral angiography on left VA. To‐and‐fro stagnated flow in right VA was pointed by arrow
Figure 3.
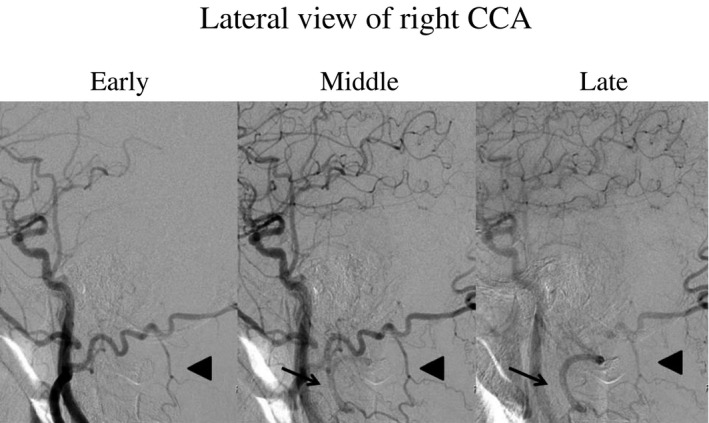
Lateral view of cerebral angiography on left CCA. Blood flow came in right VA (arrow) through muscle branch of occipital artery (arrow head)
Flow stasis with to‐and‐fro stream in VA was directly detected by cerebral angiography. Although angiography is invasive, it is useful to diagnose VA stump syndrome. Clinical symptoms of ischemic stroke by VA stump syndrome and dissection are similar to headache and ataxia. Although Doppler echo can detect blood flow dynamics less invasively,4 it is hard to estimate intracranial impairment. However, VA stump syndrome presents the flow gain at far distal VA to union without proximal signal by MR angiography. Cerebral angiography can directly confirm the flow stasis by VA stump syndrome.
CONFLICT OF INTEREST
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
Tempaku A. Cerebral angiography directly visualizes to‐and‐fro stream of vertebral artery stump syndrome . J Gen Fam Med. 2017;18:462–463. https://doi.org/10.1002/jgf2.114
REFERENCES
- 1. Kawano H, Inatomi Y, Hirano T, Yonehara T. Vertebral artery stump syndrome in acute ischemic stroke. J Neurol Sci 2013;324:74–9. [DOI] [PubMed] [Google Scholar]
- 2. Nguyen TN, Raymond J, Mahmoud M, Weill A, Roy D, Guilbert E. Vertebral artery stump syndrome. J Neurol Neurosurg Psychiatry 2008;79:91–2. [DOI] [PubMed] [Google Scholar]
- 3. Kawano H, Inatomi Y, Hirano T, Yonehara T, Uchino M. Anticoagulant therapy for vertebral artery stump syndrome. J Neurol Sci 2010;295:125–7. [DOI] [PubMed] [Google Scholar]
- 4. Ringelstein EB, Zeumer H. The role of continuous‐wave Doppler sonography in the diagnosis and management of basilar and vertebral artery occlusions, with special reference to its application during local fibrinolysis (“Vertebrobasilar disease. Time for a new strategy”. Louis R. Caplan, 1981). J Neurol 1982;228:161–70. [DOI] [PubMed] [Google Scholar]


