Abstract
The effect of aspirin in primary stroke prevention is controversial in Western population, and no evidence is available in Asian population. We performed stroke subanalysis of the Japanese Primary Prevention Project (JPPP), which was a randomized controlled trial of aspirin vs no aspirin for primary prevention of vascular events in 14 464 patients aged over 60 years with hypertension, diabetes, and/or dyslipidemia. We evaluated the effects of aspirin on the risk of stroke and intracranial hemorrhage. Aspirin did not show any net benefit for primary stroke prevention during median follow‐up for 5 years, because nonsignificant reduction in ischemic stroke was offset by nonsignificant increase in hemorrhagic stroke. Aspirin is not recommended for primary stroke prevention in elderly Japanese patients with vascular risk factors in general. Asymptomatic large artery atherosclerosis appears to be a new target for primary prevention of stroke.
Keywords: aspirin, intracranial hemorrhage, Japanese, primary prevention, stroke
1. INTRODUCTION
Aspirin has been proven to have a larger benefit than risk in secondary stroke prevention,1 although clinical trials of aspirin conducted in Western countries have reported conflicting results regarding the efficacy for primary stroke prevention,2, 3, 4 and there is no evidence available for Asian population, which might have a different risk‐benefit profile from that in Western population. However, hemorrhagic stroke is more likely to occur in Asian population than in Western population.5, 6 Based on these backgrounds, we performed stroke subanalysis of the Japanese Primary Prevention Project (JPPP), which was a randomized controlled trial of aspirin in elderly patients with vascular risk factors.7
2. SUBJECTS AND METHODS
JPPP was an investigator‐driven, nationwide, multicenter, open‐label, randomized controlled trial of aspirin for primary prevention of vascular events.7 Patients aged over 60 years with hypertension, diabetes, and/or dyslipidemia were randomized to receive either 100 mg of aspirin or no aspirin and were followed for up to 6.5 years. A total of 14 464 patients were recruited, and the median follow‐up period was 5.02 years. We evaluated the effects of aspirin on fatal and nonfatal stroke, ischemic stroke plus transient ischemic attack (TIA), ischemic stroke, and intracranial hemorrhage (ICH) using exploratory Cox regression analyses.8
3. RESULTS
Fatal and nonfatal strokes occurred in 128 patients in both the aspirin and no aspirin groups. No significant difference in the rate of any stroke or TIA at 5 years was observed between the two groups (2.068% in the aspirin group and 2.299% in the no aspirin group, adjusted hazard ratio [HR] 0.927, 95% confidence interval [CI] 0.741‐1.160, P = .509) (Figure 1A). There was also no significant difference in any stroke at 5 years between both groups (1.809% in the aspirin group and 1.828% in the no aspirin group, adjusted HR 1.011, 95% CI 0.791‐1.291, P = .932) (Figure 1B). Fewer ischemic strokes occurred in the aspirin group than in the no aspirin group, but the difference was not significant (1.199% in the aspirin group and 1.451% in the no aspirin group, adjusted HR 0.842%, 95% CI 0.631‐1.123, P = .240) (Figure 1C). Cumulative rate of ICH at 5 years was nonsignificantly higher in the aspirin group than in the no aspirin group (0.748% in the aspirin group and 0.511% in the no aspirin group, adjusted HR 1.463, 95% CI 0.956‐2.237, P = .078) (Figure 1D). The details of ICH are shown in Table 1. Cerebral hemorrhage occurred more frequently in the aspirin group than in the no aspirin group, whereas the rates of subarachnoid hemorrhage and subdural hematoma were comparable between the two groups.
Figure 1.
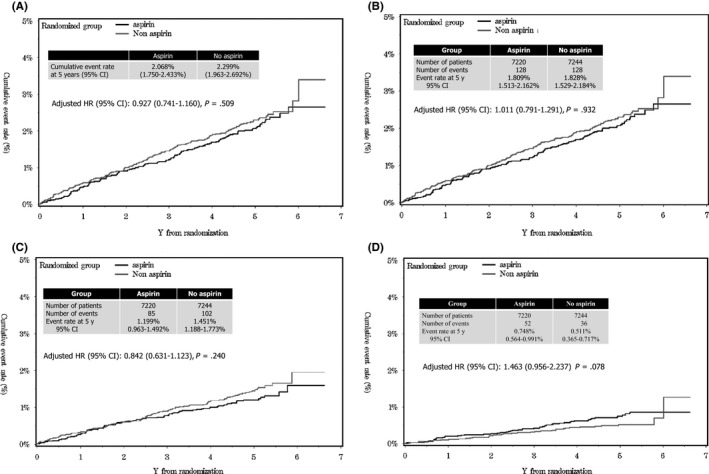
(A) Cumulative rates of any stroke or transient ischemic attack (TIA) in aspirin and no aspirin groups. There was no difference in the rates of stroke or TIA between the two groups. (B) Cumulative rate of any stroke in aspirin and no aspirin groups. There was no difference in the rate of stroke between the two groups. (C) Cumulative rate of ischemic stroke in aspirin and no aspirin groups. Ischemic stroke was nonsignificantly fewer in the aspirin group than in the no aspirin group. (D) Cumulative rate of intracranial hemorrhage (ICH) in aspirin and no aspirin groups. Rate of ICH was nonsignificantly higher in the aspirin than in the no aspirin group (Quoted from reference 8)
Table 1.
Cerebrovascular events and intracranial hemorrhage8
| Events | Aspirin | No aspirin |
|---|---|---|
| Cerebrovascular events | 147 | 128 |
| Fatal or nonfatal stroke | 128 | 102 |
| Ischemic stroke | 85 | 102 |
| Hemorrhagic stroke | 38 | 23 |
| Unclassified | 5 | 3 |
| Transient ischemic attack | 19 | 34 |
| Intracranial hemorrhage | 52 | 36 |
| Cerebral hemorrhage | 28 | 15 |
| Subarachnoid hemorrhage | 10 | 8 |
| Subdural hematoma | 13 | 12 |
| Other hemorrhage | 1 | 1 |
Factors affecting stroke and TIA were evaluated using a Cox regression analysis in all patients recruited (Table 2). Aspirin was not one of the factors affecting cerebrovascular events. Age over 70 years, cigarette smoking and diabetes mellitus were independent risk factors for cerebrovascular events. According to the estimated parameters, the risk score was calculated as a total of two for age over 70 years, one for smoking, and one for diabetes. A score of 0 or 1 was classified as low risk, and a score of two or more was classified as high risk. The cumulative rate of cerebrovascular events at 5 years was not different between the aspirin group and no aspirin group not only for the low‐risk patients but also for the high‐risk patients (Figure 2).
Table 2.
Cox regression to calculate risk score for cerebrovascular events8
| Factor | Parameter estimate | P value | Hazard ratio (95% CI) |
|---|---|---|---|
| Aspirin | −0.07906 | .489 | 0.924 (0.379‐1.156) |
| Female | −0.21015 | .085 | 0.810 (0.638‐1.029) |
| Age ≧70 years | 0.79179 | <.001 | 2.207 (1.718‐2.836) |
| Smoking | 0.41.26 | .009 | 1.513 (1.111‐2.061) |
| Diabetes | 0.44123 | <.001 | 1.555 (1.237‐1.954) |
Figure 2.
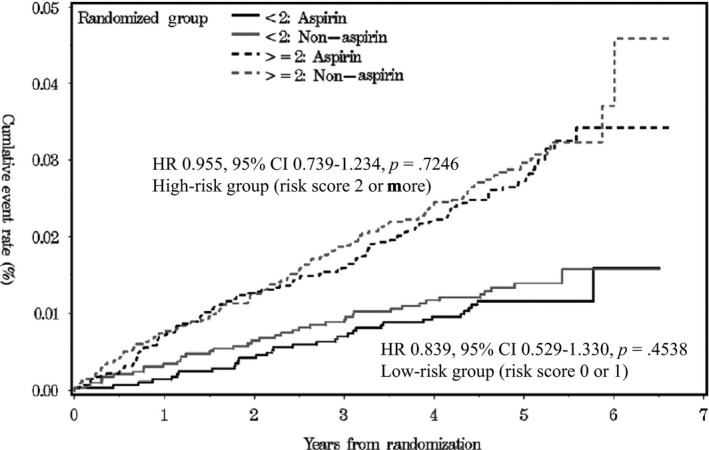
Cumulative rate of any stroke or transient ischemic attack (TIA) in low‐ and high‐risk groups. Risk factors for cerebrovascular events were estimated by Cox regression analysis. Age over 70 years, smoking, and diabetes were significant risk factors for cerebrovascular events. According to these results, risk score was calculated by the sum of two for age over 70 years, one for smoking, and one for diabetes (quoted from reference 8)
4. DISCUSSION
Clinical trials conducted in Western countries have reported conflicting results regarding the benefit of aspirin for primary stroke prevention.2, 3, 4 According to a meta‐analysis reported by the Antithrombotic Trialists’ Collaboration (ATT), aspirin did not reduce the risk of stroke for primary prevention 1 (Table 3). However, the risk ratio of aspirin vs control was 0.95% (95% CI 0.85‐1.06). Aspirin nonsignificantly reduced the risk of ischemic stroke (rate ratio 0.86, 95% CI 0.74‐1.00) but nonsignificantly increased the risk of hemorrhagic stroke (risk ratio 1.32, 95% CI 1.00‐1.75).
Table 3.
Effects of aspirin in primary and secondary prevention trials (meta‐analysis by Antithrombotic Trialists’ Collaboration)1
| Number of events (aspirin vs control) | Rate ratio (95% CI) (aspirin vs control) | |||
|---|---|---|---|---|
| Primary prevention (660 000 person‐years) | Secondary prevention (43 000 person‐years) | Primary Prevention | Secondary prevention | |
| Stroke | 655 vs 683 | 480 vs 580 | 0.95 (0.85‐1.06) | 0.81 (0.71‐0.92) |
| Ischemic | 317 vs 367 | 140 vs 176 | 0.86 (0.74‐1.00) | 0.78 (0.61‐0.99) |
| Hemorrhagic | 116 vs 89 | 36 vs 19 | 1.32 (1.00‐1.75) | 1.67 (0.97‐2.90) |
| Unknown cause | 222 vs 226 | 304 vs 385 | 0.97 (0.80‐1.18) | 0.77 (0.66‐0.91) |
We suspected that the risk‐benefit profile of aspirin for primary stroke prevention might be different between Japanese and Western populations. In reality, the rate of ischemic stroke was lower in the JPPP population than in the ATT population for primary prevention (0.26%/y vs 1.04%/y), whereas the rate of hemorrhagic stroke was higher in the JPPP population than in the ATT population (0.08%/y vs 0.03%/y).1, 8 However, the results of our subanalysis of stroke in the JPPP were similar to the results of the meta‐analysis reported by ATT regarding the net benefit for primary stroke prevention. Therefore, we can conclude that aspirin does not reduce the risk of total stroke because the nonsignificant reduction of ischemic stroke is offset by the nonsignificant increase in hemorrhagic stroke regardless ethnicities including Japanese.
The presently ongoing Study to Assess the Efficacy and Safety of Enteric‐Coated Acetylsalicylic Acid in Patients at Moderate Risk of Cardiovascular Disease (ARRIVE), A Study of Cardiovascular Events in Diabetes (ASCEND), Aspirin in Reducing Events in the Elderly (ASPREE), and International Standard Randomised Controlled Trial Number (ISRCTN) trials, in which the majority of recruited patients are from Western populations, may provide additional information regarding ethnic differences in the efficacy and safety of aspirin for the primary prevention of stroke.
The relatively low rate of ischemic stroke may be attributable to well‐controlled risk factors, as demonstrated in the baseline data.7, 8 However, despite the sufficient management of risk factors, hemorrhagic stroke was more common in the JPPP population than in the ATT population.1, 8 Among ICH, cerebral hemorrhage was more common in the aspirin group than in the no aspirin group, whereas subarachnoid hemorrhage and subdural hematoma were comparable between the two groups.8
The strongest risk factor for cerebral hemorrhage is widely recognized to be hypertension.9, 10, 11, 12, 13 In the Secondary Prevention of Small Subcortical Strokes (SPS3) trial, the rate of hemorrhagic stroke was significantly reduced by a systolic blood pressure target of <130 mm Hg, compared with a systolic blood pressure target of 130 to 149 mm Hg in patients receiving aspirin alone or aspirin plus clopidogrel.14 In the Bleeding with Antithrombotic Therapy (BAT) study, which was an observational cohort study in patients receiving antithrombotic drugs for cerebrovascular or cardiovascular diseases, the optimal cutoff blood pressure level to predict ICH was 130/81 mm Hg.15
Based on these results, the Guidelines of the Japanese Society of Hypertension 2014 recommended a target blood pressure of <130/80 mm Hg for stroke patients receiving antithrombotics.16 Also, in the Japanese Guidelines for the Management of Stroke 2015, a blood pressure <130/80 mm Hg is recommended for stroke patients receiving antithrombotics.17
However, there is no recommendation for blood pressure control in patients receiving antiplatelet drugs for primary stroke prevention because there is no convincing evidence in this population. A stricter control of blood pressure, compared with the conventional blood pressure control level, may be required to reduce the risk of cerebral hemorrhage in patients treated with aspirin for the primary prevention of strokes, especially among populations with a high risk of ICH, such as Japanese or other Asian populations.5, 6
A Cox regression analysis to calculate the risk score for all the patients recruited in the JPPP showed that the risk factors for cerebrovascular events were age >70 years, smoking, and diabetes mellitus. The present results suggest that smoking cessation and the management of diabetes mellitus are important as modifiable risk factors to reduce the residual risk of cerebrovascular events, regardless of treatment with aspirin in elderly Japanese patients with vascular risk factors.
Aspirin significantly reduced myocardial infarction (MI) and TIA as demonstrated in the main results of JPPP.7 Majority of MI and TIA is categorized into atherothrombosis, which is a platelet‐dependent disease state in large arteries.18 Therefore, aspirin might be able to reduce not only TIA but also atherothrombotic stroke. Unfortunately, it was difficult to differentiate atherothrombotic stroke from lacunar stroke in JPPP, because which was a collaborative study mainly not by vascular neurologists but by general physicians, and vascular imaging was not required for the diagnosis of stroke subtype.
In conclusion, aspirin did not have any net benefit for the primary prevention of strokes in elderly Japanese patients with risk factors. Because, nonsignificant reduction in ischemic stroke was offset by nonsignificant increase in hemorrhagic stroke. Aspirin should be used for patients in whom a net clinical benefit, which is estimated by the total incidence of major ischemic and hemorrhagic events, can be expected19 (Figure 3). Therefore, aspirin is not recommended for primary stroke prevention in elderly Japanese patients with vascular risk factors based on the results of this subanalysis of JPPP. It is interesting to study whether or not aspirin is beneficial for the prevention of atherothrombotic stroke or TIA in patients with asymptomatic large artery atherosclerosis.
Figure 3.
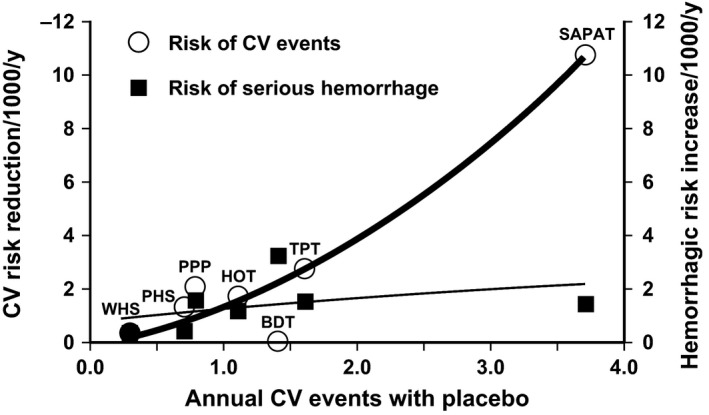
Benefits and risks of low‐dose aspirin in primary prevention trials. The numbers of vascular events avoided and episodes of major bleeding caused by per 1000 patients treated with aspirin per year re plotted from the results of individual placebo‐controlled trials of aspirin in different patient populations characterized by various degrees of cardiovascular risk. WHS denotes Women's Health Study, PHS Physicians’ Health Study, PPP Primary Prevention Project, HOT Hypertension Optimal Treatment Study, BDT British Doctors Trial, TPT Thrombosis Prevention Trial, and SAPAT Swedish Angina Pectoris Aspirin Trial (quoted from reference 18)
CONFLICT OF INTEREST
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
Uchiyama S. Aspirin for primary stroke prevention in elderly patients with vascular risk factors. J Gen Fam Med. 2017;18:331–335. https://doi.org/10.1002/jgf2.102
REFERENCES
- 1. Antithrombotic Trialists’ (ATT) Collaboration . Aspirin in the primary and secondary prevention of vascular disease: collaborative meta‐analysis individual participant data from randomised trials. Lancet. 2009;373:1849–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Steering Committee of the Physicians’ Health Study Research . Group: final report on the aspirin component of the ongoing Physicians’ Health Study. N Engl J Med. 1989;321:129–35. [DOI] [PubMed] [Google Scholar]
- 3. de Gaetano G; Collaborative Group of the Primary Prevention Project . Low‐dose aspirin and vitamin E in people at cardiovascular risk: a randomised trial in general practice. Collaborative Group of the Primary Prevention Project. Lancet. 2001;357:89–95. [DOI] [PubMed] [Google Scholar]
- 4. Ridker PM, Cook NR, Lee IM, et al. A randomized trial of low‐dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med. 2005;352:1293–304. [DOI] [PubMed] [Google Scholar]
- 5. Krishnamurthi RV, Feigin VL, Forouzanfar MH, et al. Global and regional burden of first‐ever ischaemic and haemorrhagic stroke during 1990‐2010: findings from the Global Burden of Disease Study 2010. Lancet Glob Health. 2013;1:e259–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ueshima H, Sekikawa A, Miura K, et al. Cardiovascular disease and risk factors in Asia: a selected review. Circulation. 2008;118:2702–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ikeda Y, Shimada K, Teramoto T, et al. Low‐dose aspirin for primary prevention of cardiovascular events in Japanese patients 60 years or older with atherosclerotic risk factors: a randomized clinical trial. JAMA. 2014;312:2510–20. [DOI] [PubMed] [Google Scholar]
- 8. Uchiyama S, Ishizuka N, Shimada K, et al. Aspirin for stroke prevention in elderly patients with vascular risk factors. Japanese Primary Prevention Project. Stroke. 2016;47:1605–11. [DOI] [PubMed] [Google Scholar]
- 9. Hata J, Ninomiya T, Hirakawa Y, et al. Secular trends in cardiovascular disease and its risk factors in Japanese: half‐century data from the Hisayama Study (1961‐2009). Circulation. 2013;128:1198–205. [DOI] [PubMed] [Google Scholar]
- 10. Arima H, Tanizaki Y, Yonemoto K, et al. Impact of blood pressure levels on different types of stroke: the Hisayama study. J Hypertens. 2009;27:2437–43. [DOI] [PubMed] [Google Scholar]
- 11. Ariesen MJ, Claus SP, Rinkel GJ, Algra A. Risk factors for intracerebral hemorrhage in the general population: a systematic review. Stroke. 2003;34:2060–5. [DOI] [PubMed] [Google Scholar]
- 12. ODo'nnell MJ, Xavier D, Liu L, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case‐control study. Lancet. 2010;376:112–23. [DOI] [PubMed] [Google Scholar]
- 13. Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life‐years lost, and age‐specific associations in 1.25 million people. Lancet. 2014;383:1899–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. SPS Study Group . Blood pressure targets in patients with recent lacunar stroke: the SPS3 randomized trial. Lancet. 2013;382:507–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Toyoda K, Yasaka M, Uchiyama S, et al. ;Bleeding With Antithrombotic Therapy (BAT) Study Group . Blood pressure levels and bleeding events during antithrombotic therapy: the Bleeding with Antithrombotic Therapy (BAT) Study. Stroke. 2010;41:1440–4. [DOI] [PubMed] [Google Scholar]
- 16. Shimamoto K, Ando K, Fujita T, et al. ;Japanese Society of Hypertension Committee for Guidelines for the Management of Hypertension . The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res. 2014;37:253–390. [DOI] [PubMed] [Google Scholar]
- 17. Stroke Guideline Committee of the Japan Stroke Society . Japanese guidelines for the management of stroke. Tokyo: Kyowa Kikaku; 2015. [Google Scholar]
- 18. Bhatt DL, Steg PG, Ohman EM, et al. International prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA. 2006;295:180–9. [DOI] [PubMed] [Google Scholar]
- 19. Patrono CP, Rodriguez LAG, Landolfi R, Baigent C. Low‐dose aspirin for the prevention of atherothrombosis. N Engl J Med. 2005;353:2373–83. [DOI] [PubMed] [Google Scholar]


