Abstract
Background:
Physical activity is associated with a lower risk of disease recurrence among colon cancer survivors. Excess visceral adipose tissue is associated with a higher risk of disease recurrence among colon cancer survivors. The pathways through which physical activity may alter disease outcomes are unknown, but may be mediated by changes in visceral adipose tissue.
Methods:
Thirty-nine stage I–III colon cancer survivors were randomised to one of three groups: usual-care control, 150 min wk−1 of aerobic exercise (low dose) and 300 min wk−1 of aerobic exercise (high dose) for 6 months. The prespecified key body composition outcome was visceral adipose tissue quantified using dual energy X-ray absorptiometry.
Results:
Exercise reduced visceral adipose tissue in dose–response fashion (Ptrend=0.008). Compared with the control group, the low- and high-dose exercise groups lost 9.5 cm2 (95% CI: –22.4, 3.5) and 13.6 cm2 (95% CI: –27.0, –0.1) in visceral adipose tissue, respectively. Each 60 min wk−1 increase in exercise predicted a 2.7 cm2 (95% CI: –5.4, –0.1) reduction in visceral adipose tissue.
Conclusions:
Aerobic exercise reduces visceral adipose tissue in dose–response fashion among patients with stage I–III colon cancer. Visceral adipose tissue may be a mechanism through which exercise reduces the risk of disease recurrence among colon cancer survivors.
Keywords: physical activity, visceral adipose tissue, waist circumference, recurrence, prevention, obesity
Each year 83 000 people are diagnosed with stage I–III colon cancer in the United States (Siegel et al, 2014). Despite efficacious surgical and chemotherapeutic interventions, 25–40% of patients will experience recurrent and metastatic disease within 3 years of diagnosis (André et al, 2004), and 91% of those who recur within 3 years, die by 5 years (Sargent et al, 2005). Therefore, it is critical to identify additional therapies that may reduce the risk of recurrent disease and promote long-term survival in this population.
Participation in physical activity after diagnosis of colon cancer is associated with a lower risk of recurrence and mortality (Meyerhardt et al, 2006). This observation is independent of various demographic, clinico-pathologic and treatment-related prognostic factors. A consistently reported observation is that post-diagnosis physical activity is associated with disease outcomes in a dose–response fashion, such that larger doses of physical activity or exercise, up to approximately 300 min per week (min wk−1), are associated with more favourable disease outcomes (Schmid and Leitzmann, 2014).
The biologic or biobehavioural pathways through which exercise may favourably alter disease outcomes among colon cancer survivors are unknown. One plausible pathway includes exercise-induced alterations in body composition (Park et al, 2011, 2014). Excess visceral adipose tissue is associated with a higher risk of disease recurrence and mortality among colon cancer survivors (Xiao et al, 2016). In addition, waist circumference (an anthropometric proxy for visceral adipose tissue) is associated with cancer-specific and all-cause mortality among colon cancer survivors (Haydon et al, 2006). These observations are further strengthened by evidence that the visceral adipose tissue of colon cancer survivors exhibits extensive metabolomic activity (Liesenfeld et al, 2015; Del Corno et al, 2016; Donninelli et al, 2017), polymorphisms within adiposity-related genes predict disease recurrence among colon cancer survivors (Sebio et al, 2015) and adipocytes promote the proliferation of colon cancer cells in vivo (Amemori et al, 2007).
Exercise reduces visceral adipose tissue among non-diabetic persons with obesity in a dose–response fashion (Slentz et al, 2009); however, the dose–response effects of exercise on visceral adipose tissue and other body composition measures, such as waist circumference, have not been examined among colon cancer survivors. Understanding how exercise may favourably alter pathways that are hypothesised to influence disease outcomes and the sensitivity of such pathways to respond to different doses of exercise will help to improve the specificity of exercise prescriptions in this population, and provide experimental evidence to support observational studies that document the beneficial effects of exercise among colon cancer survivors.
The COURAGE trial was a randomised controlled trial with the primary aim of examining the safety, feasibility and biological efficacy of 150 and 300 min wk−1 of aerobic exercise vs usual care control over 6 months among men and women with a history of stage I–III colon cancer (Brown et al, 2016). The primary outcomes of this study are published, demonstrating that exercise is feasible, safe and induces reductions in soluble intercellular adhesion molecule-1 (Brown et al, 2017). Here we report body composition outcomes. Visceral adipose tissue quantified using dual-energy X-ray absorptiometry (DXA) was prespecified as the key body composition outcome of this trial. Our hypothesis was that exercise would reduce visceral adipose tissue in a dose–response fashion.
Patients and methods
Participants
Detailed study methods of the COURAGE trial are published (Brown et al, 2016). Potentially eligible participants were recruited throughout the metropolitan Philadelphia region. Participants were eligible if they were diagnosed with histologically proven stage I–III colon cancer; completed surgical resection and adjuvant chemotherapy within 36 months of entering the study; self-reported participating in ⩽150 min wk−1 of moderate or vigorous intensity physical activity using the Paffenbarger Physical Activity Questionnaire (Paffenbarger et al, 1978); were of age ⩾18 years; provided written physician approval; had no additional surgery planned within the 6-month intervention period (including colostomy reversal); and had the ability to walk unaided for 6 min. Participants were ineligible if they had a history of another primary cancer (other than non-melanoma skin cancer); had evidence of distant metastases; were pregnant or breast feeding; were unable to provide a baseline blood sample; had a myocardial infarction or coronary revascularisation procedure within the past 3 months; had uncontrolled hypertension, defined as a systolic blood pressure ⩾180 mm Hg or diastolic blood pressure ⩾100 mm Hg; had high risk or uncontrolled heart arrhythmias (not including atrial fibrillation); had clinically significant heart valve disease; had decompensated heart failure; had a known aortic aneurysm; or had any other condition which, in the opinion of the investigator, may impede testing of study hypotheses or make it unsafe to engage in the exercise program.
Participants were stratified on cancer stage (AJCC 7th Edition: I vs II vs III) and randomised to one of three groups: low-dose aerobic exercise (150 min wk−1), high-dose aerobic exercise (300 min wk−1) or usual care control. This study was approved by the University of Pennsylvania Institutional Review Board and registered on clinicaltrials.gov as NCT02250053. Participants provided written informed consent and written approval from their physician prior to participation.
Intervention
Aerobic exercise was performed over 6 months using study-provided in-home treadmills (LifeSpan Fitness, TR1200i, Salt Lake City, UT, USA). Participants were provided with a heart rate monitor to objectively record heart rate during each exercise session. Participants also used paper logs to record exercise adherence. Participants met with a clinical exercise physiologist to introduce the exercise prescription, and familiarise the participant with use of the treadmill, completion of exercise logs, use of a heart rate monitor, appropriate warm-up and cool-down, stretches, and proper footwear for aerobic exercise. The exercise physiologist provided ongoing behavioural and clinical support and monitored exercise adherence to the study protocol throughout the duration of the study using weekly telephone and email communications. Exercise intensity was prescribed at 50–70% of the age-predicted maximum heart rate (equivalent to 3–6 METs (Ainsworth et al, 2000)). The low-dose and high-dose groups progressed towards of the goal of 150 or 300 min wk−1 of exercise, respectively. Participants were instructed to maintain their pre-study dietary patterns throughout the study. Detailed methods of the intervention are published (Brown et al, 2016).
Participants randomised to the usual-care control group were asked to maintain their pre-study levels of physical activity and/or follow the recommendations provided by their physician. After completing 6-month measures, control group participants were provided with an in-home treadmill and individualised exercise program, like that prescribed to the two exercise groups. Upon study completion, all participants could keep their study-provided treadmills.
Measurements
Baseline and follow-up measurements were obtained by trained staff members who were blinded to treatment assignment. Demographic characteristics including age and sex were self-reported. Daily caloric intake was quantified using 3-day food records that were analysed by a registered dietitian using the Nutrition Data System for Research software (v.2014). Clinical information including cancer stage and treatment were obtained from the state cancer registry, pathology reports or physician records.
Body composition outcomes
The prespecified key body composition outcome was visceral adipose tissue quantified using DXA. All other body composition outcomes were considered exploratory. Participants underwent whole-body DXA (Hologic Horizon, Bedford, MA, USA). Dual-energy X-ray absorptiometry scans were reviewed for quality assurance by a certified DXA technician who was blinded to the study group (Powers et al, 2014). The DXA scanner was calibrated daily using an anthropomorphic spine phantom and thrice weekly using a whole-body phantom. Dual-energy X-ray absorptiometry was used to quantify visceral adipose tissue (cm2), subcutaneous adipose tissue (cm2), fat mass (kg), lean mass (kg) and bone mineral density (g m−2) using Hologic APEX v.13.5 software (Bedford, MA, USA). Dual-energy X-ray absorptiometry-derived visceral adipose tissue has been validated against computed tomography-derived visceral adipose tissue (r=0.93; P<0.001; Micklesfield et al, 2012), and has been used across a large body mass spectrum (Bredella et al, 2013). Other anthropometric outcomes that were measured in duplicate included height (m), body mass (kg), waist and hip circumferences (cm) and sagittal abdominal diameter (cm). Height and body mass were used to calculate body mass index (kg m−2).
Statistical analysis
Descriptive statistics presented for baseline variables include counts and proportions for categorical variables and means±standard deviations for continuous variables. Categorical baseline characteristics were compared among the three groups using Fisher’s exact test, and continuous baseline characteristics were compared among the three study groups using the Kruskal–Wallis test. This study was powered to detect changes in the co-primary study outcomes: soluble intercellular adhesion molecule-1 and soluble vascular cell adhesion molecule-1 (Brown et al, 2017). However, the sample size provided adequate statistical power to examine changes in visceral adipose tissue. Based on prior research (Slentz et al, 2009), over 6 months we hypothesised a change in visceral adipose tissue of +14 cm2 in the control group, +2.9 cm2 in the low-dose group and –11.6 cm2 in the high-dose group with a pooled standard deviation of ±11 cm2. Against the hypothesis of a dose–response relationship, 39 participants provided ⩾80% power with a type I error rate of 5%. All inferential analyses were conducted on an intention-to-treat basis. Normality of continuous variables was examined using graphical techniques. Change in visceral adipose tissue (and other outcomes) was evaluated from baseline to 6 months in the three groups using repeated-measures mixed-effects regression models. This statistical approach includes all available data and accounts for the correlation between repeated measures. The baseline value of the dependent variable and cancer stage (randomisation stratification factor) were included as covariates in the regression models (Fitzmaurice et al, 2012). Group-by-time interaction terms were estimated as fixed-effects in the regression model. Model fit was examined using graphical techniques. Results from the repeated-measures mixed-effects regression models are presented as least-squares mean (LS Mean)±standard error (s.e.). To evaluate the presence of a dose–response relationship across randomised groups, a test of trend was conducted by examining linear contrasts.
Results
Between January 2015 and August 2015, 39 colon cancer survivors were recruited and randomised with data collection ending in February 2016. Baseline characteristics of study participants are presented in Table 1. One participant did not provide endpoint data (97% follow-up rate).
Table 1. Baseline characteristics of the participants.
| Characteristic | Total (n=39) | Control (n=13) | Low dose (n=14) | High dose (n=12) | P |
|---|---|---|---|---|---|
|
Age, % | |||||
| <60 years | 25 (64%) | 9 (69%) | 8 (57%) | 8 (67%) | 0.840 |
| ⩾60 years | 14 (36%) | 4 (31%) | 6 (43%) | 4 (33%) | |
|
Sex, % | |||||
| Male | 15 (38%) | 4 (31%) | 7 (50%) | 4 (33%) | 0.601 |
| Female | 24 (62%) | 9 (69%) | 7 (50%) | 8 (67%) | |
|
Body mass index, % | |||||
| <25.0 kg m−2 | 7 (18%) | 3 (23%) | 2 (14%) | 2 (17%) | 0.884 |
| 25.0–29.9 kg m−2 | 12 (31%) | 5 (38%) | 4 (29%) | 3 (25%) | |
| ⩾30.0 kg m−2 | 20 (51%) | 5 (38%) | 8 (57%) | 7 (58%) | |
| Energy intake, kcal day−1 | 1735 (1270–1962) | 1800 (1233–2110) | 1776 (1483–2111) | 1632 (1196–1739) | 0.725 |
|
Cancer stage, % | |||||
| I | 5 (13%) | 1 (8%) | 2 (14%) | 2 (17%) | 0.999 |
| II | 14 (36%) | 5 (38%) | 5 (36%) | 4 (33%) | |
| III | 20 (51%) | 7 (54%) | 7 (50%) | 6 (50%) | |
| Chemotherapy, % | 28 (72%) | 10 (77%) | 10 (71%) | 8 (67%) | 0.906 |
|
Time since treatment, % | |||||
| ⩽12 months | 25 (64%) | 8 (62%) | 10 (71%) | 7 (58%) | 0.770 |
| >12 months | 14 (36%) | 5 (38%) | 4 (26%) | 5 (42%) | |
P-values are from the overall test of group differences. Data are median (interquartile range), or counts with percentages.
Exercise prescription program variables have been described in detail (Brown et al, 2017). Briefly, over 6 months, adherence to the prescribed volumes of exercise in the low- and high-dose groups were 92.8±2.4% and 89.0±2.6%, respectively (P=0.287). Average exercise volume in the low- and high-dose groups were 141.5±9.9 and 247.2±10.7 min wk−1, respectively (Δ between groups: 105.7±14.6; P<0.001). Exercise intensity was 70.7±0.8% of the age-predicted maximal heart rate and the proportion of exercise sessions validated with objective heart rate data was 96.8±0.6%, both of which did not differ between the two exercise groups. There were no significant changes in self-reported caloric consumption (P=0.743).
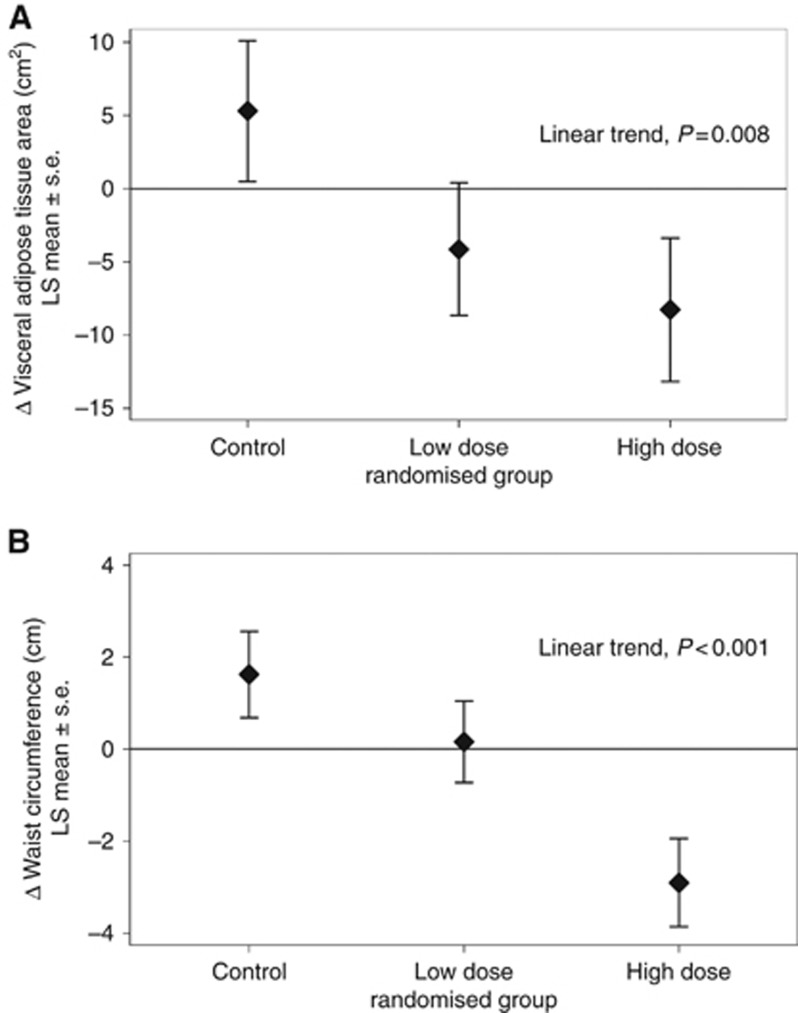
Body composition outcomes using DXA are presented in Table 2. Exercise reduced visceral adipose tissue, the prespecified key body composition outcome, in dose–response fashion (Ptrend=0.008; Figure 1A). Compared with the control group, the low- and high-dose exercise groups lost 9.5 cm2 (95% CI: –22.4, 3.5) and 13.6 cm2 (95% CI: –27.0, –0.1) in visceral adipose tissue, respectively. Each 60 min wk−1 increase in exercise predicted a 2.7 cm2 (95% CI: –5.4, –0.1) reduction in visceral adipose tissue. Exercise improved bone mineral density in dose–response fashion (Ptrend=0.015). Compared with the control group, the low- and high-dose exercise groups gained 0.015 g m−2 (95% CI: 0.001, 0.029) and 0.013 g m−2 (95% CI: -0.001, 0.028) in bone mineral density, respectively. Post hoc sex-stratified body composition outcomes using DXA are presented for hypothesis generating purposes (Supplementary Table S1).
Table 2. Body composition outcomes using DXA at baseline and change during 6 months.
| Outcome | Baseline (mean±s.d.) | Δ baseline to month 6 (LS mean±s.e.) | Δ from control (LS mean±s.e.) |
|---|---|---|---|
|
Visceral adipose tissue, cm2 | |||
| Control | 112.6±55.2 | 5.31±4.80 | — |
| Low dose | 131.3±45.6 | −4.13±4.53 | −9.45±6.60 |
| High dose | 154.2±60.5 | −8.27±4.89 | −13.58±6.86b |
| Test for trend | P=0.008 | ||
|
Subcutaneous adipose tissue, cm2 | |||
| Control | 388.4±142.6 | −3.87±8.64 | — |
| Low dose | 381.1±138.6 | 1.70±8.15 | 5.57±11.88 |
| High dose | 461.9±110.9 | −17.86±8.81a | −14.00±12.34 |
| Test for trend | P=0.222 | ||
|
Fat mass, kg | |||
| Control | 32.8±10.0 | −0.01±0.49 | — |
| Low dose | 32.6±7.6 | −0.13±0.47 | −0.12±0.68 |
| High dose | 38.1±11.9 | −0.71±0.50 | −0.70±0.71 |
| Test for trend | P=0.238 | ||
|
Lean mass, kg | |||
| Control | 49.9±13.1 | 0.30±0.35 | — |
| Low dose | 52.6±11.1 | −0.06±0.33 | −0.36±0.48 |
| High dose | 53.4±13.8 | 0.01±0.36 | −0.29±0.50 |
| Test for trend | P=0.450 | ||
|
Bone mineral density, g cm−2 | |||
| Control | 1.08±0.10 | 0.006±0.005 | — |
| Low dose | 1.03±0.12 | 0.021±0.005a | 0.015±0.007b |
| High dose | 1.02±0.09 | 0.020±0.005a | 0.013±0.007 |
| Test for trend | P=0.015 | ||
Abbreviations: DXA=dual-energy X-ray absorptiometry; LS mean=least-squares mean; s.d.=standard deviation; s.e., standard error.
Changes in outcomes are estimated using a linear mixed-effects regression model that adjusted for the baseline value of the dependent variable and cancer stage (randomisation stratification factor).
Significantly different from baseline (within-group), P⩽0.05.
Significantly different from control, P⩽0.05.
Figure 1.
Dose-response effects of exercise on body composition. Between group changes in (A) visceral adipose tissue and (B) waist circumference from baseline to 6 months. Note: LS mean, least squares mean; s.e., standard error.
Anthropometric outcomes are presented in Table 3. The finding that exercise reduced visceral adipose tissue was reinforced by the observation that exercise reduced waist circumference (an anthropometric proxy for visceral adipose tissue) in dose–response fashion (Ptrend<0.001; Figure 1B). Compared with the control group, the low- and high-dose exercise groups lost 1.5 cm (95% CI: –4.0, 1.1) and 4.5 cm (95% CI: –7.1, –1.9) in waist circumference, respectively. Each 60 min wk−1 increase in exercise predicted a 0.9 cm (95% CI: –1.4, –0.4) reduction in waist circumference. Changes in visceral adipose tissue were correlated with changes in waist circumference (r=0.42; P=0.009). Improvements in the waist-to-hip ratio did not reach statistical significance (Ptrend=0.054). No significant change in body mass was observed (Ptrend=0.280). Post hoc sex-stratified anthropometric outcomes are presented for hypothesis generating purposes (Supplementary Table S2).
Table 3. Anthropometric outcomes at baseline and change during 6 months.
| Outcome | Baseline (mean±s.d.) | Δ baseline to month 6 (LS mean±s.e.) | Δ from control (LS mean±s.e.) |
|---|---|---|---|
|
Body mass, kg | |||
| Control | 83.7±22.1 | 0.43±0.61 | — |
| Low dose | 86.2±13.1 | −0.51±0.57 | −0.95±0.84 |
| High dose | 92.2±24.3 | −0.32±0.62 | −0.76±0.87 |
| Test for trend | P=0.280 | ||
|
BMI, kg m-2 | |||
| Control | 29.2±6.0 | 0.14±0.22 | — |
| Low dose | 29.5±4.3 | −0.17±0.21 | −0.31±0.30 |
| High dose | 32.5±6.9 | −0.11±0.23 | −0.25±0.32 |
| Test for trend | P=0.354 | ||
|
Waist circumference, cm | |||
| Control | 98.0±17.1 | 1.62±0.94 | — |
| Low dose | 98.7±11.9 | 0.16±0.89 | −1.46±1.29 |
| High dose | 106.9±14.6 | −2.90±0.96a | −4.52±1.34b |
| Test for trend | P<0.001 | ||
|
Hip circumference, cm | |||
| Control | 103.4±13.5 | 1.85±1.42 | — |
| Low dose | 104.5±10.3 | 0.18±1.34 | −1.67±1.95 |
| High dose | 110.6±15.0 | 0.02±1.45 | −1.84±2.03 |
| Test for trend | P=0.518 | ||
|
Waist to hip ratio | |||
| Control | 0.94±0.09 | −0.005±0.011 | — |
| Low dose | 0.94±0.07 | 0.001±0.011 | 0.005±0.016 |
| High dose | 0.97±0.09 | −0.029±0.012a | −0.023±0.016 |
| Test for trend | P=0.054 | ||
|
Sagittal abdominal diameter, cm | |||
| Control | 22.6±4.0 | 0.45±0.32 | — |
| Low Dose | 22.4±3.6 | 0.01±0.30 | −0.43±0.44 |
| High Dose | 23.9±4.0 | 0.01±0.32 | −0.45±0.46 |
| Test for trend | P=0.200 | ||
Abbreviations: BMI=body mass index; LS mean=least-squares mean; s.d.=standard deviation; s.e.=standard error.
Changes in outcomes are estimated using a linear mixed-effects regression model that adjusted for the baseline value of the dependent variable and cancer stage (randomisation stratification factor).
Significantly different from baseline (within-group), P⩽0.05.
Significantly different from control, P⩽0.05.
No serious (grade ⩾3) adverse events occurred. Non-serious (grade 1−2) adverse events have been reported in detail (Brown et al, 2017).
Discussion
A 6-month moderate-intensity aerobic exercise program among stage I–III colon cancer survivors resulted in significant linear dose–response reductions in visceral adipose tissue measured by DXA and waist circumference. The findings from this randomised trial provide mechanistic data to support observational evidence that suggests physical activity may lower the risk of recurrence and mortality among colon cancer survivors.
The linear dose–response reductions in visceral adipose tissue and waist circumference with increasing exercise volume are similar to prior dose–response exercise interventions in other populations (Kay and Fiatarone Singh, 2006). For example, among overweight and obese men and women with dyslipidaemia, increasing exercise volume produced larger reductions in visceral adipose tissue and waist circumference (Slentz et al, 2009). Excess visceral adipose tissue is associated with a higher risk of disease recurrence and mortality among colon cancer survivors (Xiao et al, 2016). Prior epidemiologic studies have often quantified visceral adipose tissue using quartiles or quintiles (Xiao et al, 2016), which challenges direct comparison of our results to these prior studies. In the general population, each 10 cm2 increase in visceral adipose tissue is associated with an 8–10% increase in the risk of death (Kuk et al, 2006; Katzmarzyk et al, 2012). In our study, the low- and high-dose exercise groups lost 9.5 and 13.6 cm2 in visceral adipose tissue, respectively, over 6 months compared with the control group. In a cohort of 536 colon cancer survivors, each 5 cm increase in waist circumference was associated with an 8–10% increase in the risk of colon cancer-specific and all-cause mortality (Haydon et al, 2006). In our study, the low- and high-dose exercise groups lost 1.5 and 4.5 cm in waist circumference, respectively, over 6 months compared with the control group. Collectively, these data suggest that the observed exercise-induced changes in body composition may hold clinical importance for colon cancer survivors.
In our study, we observed a modest, though not statistically significant, increase in visceral adipose tissue and waist circumference over 6 months among usual-care control group participants. This observation has been reported in the control groups of prior exercise trials (Slentz et al, 2009), and underscores the deleterious effect of continued sedentary behaviour. Excess energy intake is preferentially stored as visceral adipose tissue during extended periods of inactivity (Belavý et al, 2014). It is important to note that we did not observe significant changes in body mass. Exercise preferentially utilises visceral adipose tissue as an energetic substrate, often without altering total body mass (Lee et al, 2005; Johnson et al, 2009). Health-care providers who prescribe exercise to colon cancer survivors should inform patients that exercise may not significantly reduce body mass, and that body mass alone should not be used as an indicator of exercise efficacy, as important physiologic changes are likely to occur in the absence of weight loss.
The biologic or biobehavioural pathways through which exercise may favourably alter disease outcomes among colon cancer survivors are unknown. Excess visceral adipose tissue and waist circumference are associated with an increased risk of disease recurrence and mortality among colon cancer survivors (Xiao et al, 2016). Visceral adipose tissue is an active endocrine organ that secretes various bioactive compounds such as adipokines, cytokines, hormone-like factors and other metabolites (Ahima and Flier, 2000), that have been hypothesised to influence disease recurrence and progression (Park et al, 2011, 2014). Excess visceral adipose tissue and other states associated with adiposity such as hyperinsulinaemia activate the PI3K–Akt–mTOR pathway (McCurdy and Klemm, 2013). Activation of the PI3K–Akt–mTOR pathway is associated with the growth and progression of colon cancer metastases (Gulhati et al, 2011), and silencing of this pathway inhibits the growth of metastases by inducing cell-cycle arrest and apoptosis (Zhang et al, 2009).
Several polymorphisms within adiposity-related genes predict disease recurrence among colon cancer survivors (Sebio et al, 2015). For example, PPAR-γ rs1801282 regulates transcription factors for several genes that influence colon cancer growth (Sarraf et al, 1998). Furthermore, PPAR-γ rs1801282 predicts the progression from impaired glucose tolerance to type 2 diabetes (Kilpelainen et al, 2008; Brito et al, 2009). Physical activity reduces the risk of progression from impaired glucose tolerance to type 2 diabetes that is attributed to this polymorphism (Kilpelainen et al, 2008; Brito et al, 2009). Type 2 diabetes is associated with an inferior prognosis in colon cancer (Meyerhardt et al, 2003). Future research will be needed to discern if the disease-specific benefits of physical activity for colon cancer survivors are achieved through similar pathways as that of type 2 diabetes prevention.
There are several limitations to this trial. The primary limitation to this trial is the small sample size, which limited our statistical power to examine other body composition outcomes. The small sample size allowed for numeric differences in baseline body composition and anthropometric measures. Our analyses plan prespecified that the baseline value of the dependent variable would be included in the model to account for baseline differences; however, we cannot rule out that the observed differences may be partly due to regression to the mean. The small sample size also reduces the generalisability of our findings. As we have previously described (Brown et al, 2016), trial participants were younger than the population from which they were recruited. This has important implications for the generalisability of our findings to the broader population of colon cancer survivors. The duration of the exercise intervention was 6 months, and it is not known if the dose–response effects of exercise on visceral adipose tissue would be maximised or sustained over a longer time horizon. Trial participants were not recruited based on having excess visceral adipose tissue at baseline. It is not known if the exercise-induced reductions in visceral adipose tissue would be similar or larger in magnitude among a sample who all had excess visceral adipose tissue at baseline.
There are several strengths to this trial. The use of two intervention groups, each prescribed a distinct dose of exercise, allowed us to examine how visceral adipose tissue changed along the exercise dose curve. The exercise program was flexible, emphasising a home-based program, blended with ongoing behavioural and clinical support from an exercise physiologist. The provision of home-based treadmills succeeded in providing a reasonable incentive for participation, as recruitment was completed ahead of schedule and succeeded in promoting favourable adherence to the exercise prescription over 6 months. Completion of the prescribed exercise dose was objectively quantified using heart-rate monitors with long-term (⩾3 month) memory. Data collection was completed by staff blinded to study group who followed standardised protocols. Participants in this trial had later stage of disease than the population from which they were recruited (Brown et al, 2016), which represents colon cancer survivors at highest risk for disease recurrence. Participants had a variety of comorbid conditions that are common among colon cancer survivors including hypertension, hyperlipidaemia, diabetes and cardiovascular disease. Endpoint data collection was satisfactory (97% complete).
In conclusion, the findings from this randomised trial demonstrate the dose–response effects of moderate intensity aerobic exercise to favourably reduce visceral adipose tissue among selected patients recently treated for stage I–III colon cancer. The findings from this randomised trial may be useful to health-care providers to improve the specificity of exercise prescriptions for colon cancer survivors. The findings from this randomised trial are also useful for investigators to begin to understand the mechanistic pathways that are hypothesised to mediate the relationship between exercise and disease outcomes in this population. Visceral adipose tissue may be a mechanism through which exercise reduces the risk of disease recurrence among colon cancer survivors.
Acknowledgments
We gratefully thank the Pennsylvania Cancer Registry for their role in recruitment activities for this study. This research was supported by R21-CA182767, F31-CA192560 and U54-CA155850 from the National Cancer Institute, P30-DK019525 from the National Institute of Diabetes and Digestive and Kidney Diseases, and UL1-TR000003 from the National Center for Research Resources and the National Center for Advancing Translation Science. This research was supported by discounts for treadmills from LifeSpan Fitness, LLC (Salt Lake City, UT, USA).
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Supplementary Information accompanies this paper on British Journal of Cancer website (http://www.nature.com/bjc)
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
The authors declare no conflicts of interest.
Supplementary Material
References
- Ahima RS, Flier JS (2000) Adipose tissue as an endocrine organ. Trends Endocrinol Metab 11(8): 327–332. [DOI] [PubMed] [Google Scholar]
- Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, O'Brien WL, Bassett DR Jr, Schmitz KH, Emplaincourt PO, Jacobs DR Jr, Leon AS (2000) Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 32(9 Suppl): S498–S504. [DOI] [PubMed] [Google Scholar]
- Amemori S, Ootani A, Aoki S, Fujise T, Shimoda R, Kakimoto T, Shiraishi R, Sakata Y, Tsunada S, Iwakiri R, Fujimoto K (2007) Adipocytes and preadipocytes promote the proliferation of colon cancer cells in vitro. Am J Physiol Gastrointest Liver Physiol 292(3): G923–G929. [DOI] [PubMed] [Google Scholar]
- André T, Boni C, Mounedji-Boudiaf L, Navarro M, Tabernero J, Hickish T, Topham C, Zaninelli M, Clingan P, Bridgewater J (2004) Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med 350(23): 2343–2351. [DOI] [PubMed] [Google Scholar]
- Belavý D, Möhlig M, Pfeiffer A, Felsenberg D, Armbrecht G (2014) Preferential deposition of visceral adipose tissue occurs due to physical inactivity. Int J Obes 38(11): 1478–1480. [DOI] [PubMed] [Google Scholar]
- Bredella MA, Gill CM, Keating LK, Torriani M, Anderson EJ, Punyanitya M, Wilson KE, Kelly TL, Miller KK (2013) Assessment of abdominal fat compartments using DXA in premenopausal women from anorexia nervosa to morbid obesity. Obesity 21(12): 2458–2464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brito EC, Lyssenko V, Renström F, Berglund G, Nilsson PM, Groop L, Franks PW (2009) Previously associated type 2 diabetes variants may interact with physical activity to modify the risk of impaired glucose regulation and type 2 diabetes. Diabetes 58(6): 1411–1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown JC, Troxel AB, Ky B, Damjanov N, Zemel BS, Rickels MR, Rhim AD, Rustgi AK, Courneya KS, Schmitz KH (2016) A randomized phase II dose–response exercise trial among colon cancer survivors: purpose, study design, methods, and recruitment results. Contemp Clin Trials 47: 366–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown JC, Troxel AB, Ky B, Damjanov N, Zemel BS, Rickels MR, Rhim AD, Rustgi AK, Courneya KS, Schmitz KH (2017) Dose-response effects of aerobic exercise among colon cancer survivors: a randomized phase II trial. Clin Colorectal Cancer e-pub ahead of print 17 June 2017; doi:10.1016/j.clcc.2017.06.001. [DOI] [PMC free article] [PubMed]
- Del Corno M, D'Archivio M, Conti L, Scazzocchio B, Vari R, Donninelli G, Varano B, Giammarioli S, De Meo S, Silecchia G, Pennestri F, Persiani R, Masella R, Gessani S (2016) Visceral fat adipocytes from obese and colorectal cancer subjects exhibit distinct secretory and omega6 polyunsaturated fatty acid profiles and deliver immunosuppressive signals to innate immunity cells. Oncotarget 7(39): 63093–63105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donninelli G, Del Corno M, Pierdominici M, Scazzocchio B, Vari R, Varano B, Pacella I, Piconese S, Barnaba V, D'Archivio M, Masella R, Conti L, Gessani S (2017) Distinct blood and visceral adipose tissue regulatory T cell and innate lymphocyte profiles characterize obesity and colorectal cancer. Front Immunol 8: 643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzmaurice GM, Laird NM, Ware JH (2012) Applied Longitudinal Analysis Vol. 998. John Wiley & Sons: Hoboken, NJ, USA. [Google Scholar]
- Gulhati P, Bowen KA, Liu J, Stevens PD, Rychahou PG, Chen M, Lee EY, Weiss HL, O'Connor KL, Gao T, Evers BM (2011) mTORC1 and mTORC2 regulate EMT, motility, and metastasis of colorectal cancer via RhoA and Rac1 signaling pathways. Cancer Res 71(9): 3246–3256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haydon AM, Macinnis RJ, English DR, Giles GG (2006) Effect of physical activity and body size on survival after diagnosis with colorectal cancer. Gut 55(1): 62–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson NA, Sachinwalla T, Walton DW, Smith K, Armstrong A, Thompson MW, George J (2009) Aerobic exercise training reduces hepatic and visceral lipids in obese individuals without weight loss. Hepatology 50(4): 1105–1112. [DOI] [PubMed] [Google Scholar]
- Katzmarzyk PT, Mire E, Bouchard C (2012) Abdominal obesity and mortality: The Pennington Center Longitudinal Study. Nutr Diabetes 2(8): e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kay SJ, Fiatarone Singh MA (2006) The influence of physical activity on abdominal fat: a systematic review of the literature. Obes Rev 7(2): 183–200. [DOI] [PubMed] [Google Scholar]
- Kilpelainen TO, Lakka TA, Laaksonen DE, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, Keinanen-Kiukaanniemi S, Lindi V, Tuomilehto J, Uusitupa M, Laakso M (2008) SNPs in PPARG associate with type 2 diabetes and interact with physical activity. Med Sci Sports Exerc 40(1): 25–33. [DOI] [PubMed] [Google Scholar]
- Kuk JL, Katzmarzyk PT, Nichaman MZ, Church TS, Blair SN, Ross R (2006) Visceral fat is an independent predictor of all-cause mortality in men. Obesity 14(2): 336–341. [DOI] [PubMed] [Google Scholar]
- Lee S, Kuk JL, Davidson LE, Hudson R, Kilpatrick K, Graham TE, Ross R (2005) Exercise without weight loss is an effective strategy for obesity reduction in obese individuals with and without type 2 diabetes. J Appl Physiol 99(3): 1220–1225. [DOI] [PubMed] [Google Scholar]
- Liesenfeld DB, Grapov D, Fahrmann JF, Salou M, Scherer D, Toth R, Habermann N, Böhm J, Schrotz-King P, Gigic B (2015) Metabolomics and transcriptomics identify pathway differences between visceral and subcutaneous adipose tissue in colorectal cancer patients: the ColoCare study. Am J Clin Nutr 102(2): 433–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCurdy CE, Klemm DJ (2013) Adipose tissue insulin sensitivity and macrophage recruitment: does PI3K pick the pathway? Adipocyte 2(3): 135–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyerhardt JA, Catalano PJ, Haller DG, Mayer RJ, Macdonald JS, Benson AB 3rd, Fuchs CS (2003) Impact of diabetes mellitus on outcomes in patients with colon cancer. J Clin Oncol 21(3): 433–440. [DOI] [PubMed] [Google Scholar]
- Meyerhardt JA, Heseltine D, Niedzwiecki D, Hollis D, Saltz LB, Mayer RJ, Thomas J, Nelson H, Whittom R, Hantel A, Schilsky RL, Fuchs CS (2006) Impact of physical activity on cancer recurrence and survival in patients with stage III colon cancer: findings from CALGB 89803. J Clin Oncol 24(22): 3535–3541. [DOI] [PubMed] [Google Scholar]
- Micklesfield LK, Goedecke JH, Punyanitya M, Wilson KE, Kelly TL (2012) Dual-energy X-ray performs as well as clinical computed tomography for the measurement of visceral fat. Obesity 20(5): 1109–1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paffenbarger R, Wing A, Hyde R (1978) Paffenbarger physical activity questionnaire. Am J Epidemiol 108: 161–175. [DOI] [PubMed] [Google Scholar]
- Park J, Euhus DM, Scherer PE (2011) Paracrine and endocrine effects of adipose tissue on cancer development and progression. Endocr Rev 32(4): 550–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park J, Morley TS, Kim M, Clegg DJ, Scherer PE (2014) Obesity and cancer [mdash] mechanisms underlying tumour progression and recurrence. Nat Rev Endocrinol 10(8): 455–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers C, Fan B, Shepherd J (2014) Importance of image review for accurate reporting of hologic DXA visceral adipose tissue. J Clin Densitom 17(3): 399. [Google Scholar]
- Sargent DJ, Wieand HS, Haller DG, Gray R, Benedetti JK, Buyse M, Labianca R, Seitz JF, O'Callaghan CJ, Francini G (2005) Disease-free survival versus overall survival as a primary end point for adjuvant colon cancer studies: individual patient data from 20,898 patients on 18 randomized trials. J Clin Oncol 23(34): 8664–8670. [DOI] [PubMed] [Google Scholar]
- Sarraf P, Mueller E, Jones D, King FJ, DeAngelo DJ, Partridge JB, Holden SA, Chen LB, Singer S, Fletcher C (1998) Differentiation and reversal of malignant changes in colon cancer through PPARγ. Nat Med 4(9): 1046–1052. [DOI] [PubMed] [Google Scholar]
- Schmid D, Leitzmann M (2014) Association between physical activity and mortality among breast cancer and colorectal cancer survivors: a systematic review and meta-analysis. Ann Oncol 25(7): 1293–1311. [DOI] [PubMed] [Google Scholar]
- Sebio A, Gerger A, Matsusaka S, Yang D, Zhang W, Stremitzer S, Stintizing S, Sunakawa Y, Yamauchi S, Ning Y (2015) Genetic variants within obesity-related genes are associated with tumor recurrence in patients with stages II/III colon cancer. Pharmacogenet Genomics 25(1): 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel R, Desantis C, Jemal A (2014) Colorectal cancer statistics, 2014. CA Cancer J Clin 64(2): 104–117. [DOI] [PubMed] [Google Scholar]
- Slentz CA, Houmard JA, Kraus WE (2009) Exercise, abdominal obesity, skeletal muscle, and metabolic risk: evidence for a dose response. Obesity (Silver Spring) 17(Suppl 3(S3): S27–S33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao J, Mazurak VC, Olobatuyi TA, Caan BJ, Prado CM (2016) Visceral adiposity and cancer survival: a review of imaging studies. Eur J Cancer Care (Engl) e-pub ahead of print 6 December 2017; doi:10.1111/ecc.12611. [DOI] [PubMed]
- Zhang Y-J, Dai Q, Sun D-F, Xiong H, Tian X-Q, Gao F-H, Xu M-H, Chen G-Q, Han Z-G, Fang J-Y (2009) mTOR signaling pathway is a target for the treatment of colorectal cancer. Ann Surg Oncol 16(9): 2617–2628. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.