Abstract
Higher rates of obesity and obesity-related chronic disease are prevalent in communities where there is limited access to affordable, healthy food. The B’More Healthy Communities for Kids (BHCK) trial worked at multiple levels of the food environment including food wholesalers and corner stores to improve the surrounding community’s access to healthy food. The objective of this article is to describe the development and implementation of BHCK’s corner store and wholesaler interventions through formal process evaluation. Researchers evaluated each level of the intervention to assess reach, dose delivered, and fidelity. Corner store and wholesaler reach, dose delivered, and fidelity were measured by number of interactions, promotional materials distributed, and maintenance of study materials, respectively. Overall, the corner store implementation showed moderate reach, dose delivered, and high fidelity. The wholesaler intervention was implemented with high reach, dose, and fidelity. The program held 355 corner store interactive sessions and had 9,347 community member interactions, 21% of which were with children between the ages of 10 and 14 years. There was a 15% increase in corner store promoted food stocking during Wave 1 and a 17% increase during Wave 2. These findings demonstrate a successfully implemented food retailer intervention in a low-income urban setting.
Keywords: process evaluation, program planning and evaluation, health education, nutrition, community intervention, obesity, chronic disease, health promotion
INTRODUCTION
The global supply of inexpensive and calorie-dense foods has increased over the past four decades (Swinburn et al., 2011). This has contributed to the rise in obesity in the United States over the past decades, with a prevalence of 35% of adults and 17% of children (≤18 years) currently classified as obese, respectively (Flegal et al., 2016; Ogden, Carroll, Kit, & Flegal, 2014). Obesity during childhood can lead to metabolic syndrome, type 2 diabetes, an increased risk for obesity in adulthood, as well as other comorbidities (Biro & Wien, 2010; Estrada et al., 2014). Among food insecure households in Baltimore City who experience hunger, 73% of adults and 19% of children are obese (Vedovato et al., 2016). African American residents have disproportionately poor access to healthy foods, compared to Caucasian residents and a corresponding high rate of obesity (Baltimore City Health Department, 2014; Buczynski, Freishtat, & Buzogany, 2015; Franco, Roux, Glass, Caballero, & Brancati, 2008).
In Baltimore City, approximately 25% of residents live in a food desert, defined as an area where the median household income is 185% below the poverty line, over 30% of residents do not have a vehicle, low average score of Healthy Food Availability Index (Díez et al., 2016; Glanz, Sallis, Saelens, & Frank, 2007), and the closest supermarket is more than quarter mile away (Baltimore City Health Department, 2014; Buczynski et al., 2015; Mui et al., 2015). Healthy Food Availability Index scores were created using an abbreviated version of the Nutrition Environment Measures Survey in Stores, a standardized retail food store observational tool (Glanz et al., 2007). In these areas, corner stores are the primary food source available, where the most frequent purchases are sugar sweetened beverages and foods high in fat, sodium, and sugar (Borradaile et al., 2009; D’Angelo, Suratkar, Song, Stauffer, & Gittelsohn, 2011; Mui et al., 2015). Consequently, greater access to corner stores and convenience stores is associated with higher rates of obesity (Borradaile et al., 2009; Kiszko et al., 2015). In low-income communities, fresh produce is often overpriced or of poor quality when available, and small food store owners report that unhealthy food is easier to stock due to its low price and convenient delivery options (Evans, Banks, & Jennings, 2015; Martin et al., 2014; Powell, Slater, Mirtcheva, Bao, & Chaloupka, 2007; Walker, Keane, & Burke, 2010).
Small store owners face multiple barriers when it comes to stocking healthy foods, including few healthy food suppliers, inability to purchase healthy foods in small quantities, lack of proper infrastructure (i.e., fridge, freezer, limited shelf space), and a perceived low demand from customers (Andreyeva, Middleton, Long, Luedicke, & Schwartz, 2011; Caspi, Pelletier, Harnack, Erickson, & Laska, 2016; Gittelsohn et al., 2008; O’Malley, Gustat, Rice, & Johnson, 2013). Wholesalers require a consistent demand from corner stores to maintain stock of healthier foods (Mui et al., 2015). Wholesalers are a key point of intervention in the corner store food supply chain because they are centrally connected to both unhealthy and healthy suppliers and serve as a primary supplier for corner stores (Mui et al., 2015).
Recent corner store trials found point of purchase labeling increased sales of promoted items in low-income areas with a low-literacy population (Escaron, Meinen, Nitzke, & Martinez-Donate, 2013; Gittelsohn, Rowan, & Gadhoke, 2012; Moore, Pinard, & Yaroch, 2016). Other strategies include involvement of stakeholders, community forums, cooking demonstrations, and taste tests (Bodor, Ulmer, Dunaway, Farley, & Rose, 2010; Budd et al., 2015; Gittelsohn et al., 2013; Gittelsohn et al., 2012). Previous corner store trials in Baltimore have improved store owner stocking of healthy foods and significantly decreased the weight of female adolescent participants through the utilization of point of purchase labeling, taste testing, and supplemental nutrition education in recreation centers (Gittelsohn et al., 2010; Gittelsohn et al., 2013). The B’More Healthy Communities for Kids (BHCK) trial intervened at multiple levels of the food environment in collaboration with city officials, local wholesalers, corner stores, carryouts, and recreation centers (Gittelsohn et al., 2014).
Little published literature exists on the relationship between small food stores (corner stores & carryouts) and the wholesalers that supply them (Budd et al., 2015; Centers for Disease Control and Prevention, 2014; The Food Trust, 2015; New York City Department of Health and Mental Hygiene, 2013; O’Malley et al., 2013), and only one previous study has sought to intervene in this relationship (Budd et al., 2015). Furthermore, process evaluation data of environmental interventions is rarely reported. However, more emphasis should be placed on understanding opportunities for quality improvement of the study and reasons for success or failure of trials. Therefore, the primary aim of this article is to report on process evaluation measures and standards used to evaluate the reach, dose, and fidelity of the corner store and wholesale-level intervention implementation of the BHCK trial to ensure quality of the study.
MATERIALS AND METHOD
Setting
Baltimore City has approximately 435 corner stores, 300 convenience stores, and 45 supermarkets (Buczynski et al., 2015). Approximately 24.2% of residents live below the poverty line and those in the lowest income bracket (<$25,000) are 5 times more likely than higher income residents (>$50,000) to live 15 minutes or more from a supermarket (Baltimore City Health Department, 2014; U.S. Census Bureau, 2015).
Study Design
The BHCK trial used a group randomized study design, and assigned 28 low-income, predominantly African American, geographic zones to intervention or comparison. A 1-mile radius around a Baltimore City recreation center served as the zone perimeter; intervention neighborhoods were located more than 1 mile from comparison zones to prevent contamination. The intervention’s priority population were low-income African American, youth (10–14 years old) and their caregivers (>18 years; Gittelsohn et al., 2014). BHCK implementation occurred in two waves. Each wave consisted of seven intervention and seven comparison zones (14 total neighborhoods per wave). Wave 1 was implemented from July 2014 to February 2015; Wave 2 occurred from November 2015 to July 2016. BHCK intervened in a minimum of three food sources/zone, including a combination of corner stores and carryouts in each zone (Gittelsohn et al., 2014). Social cognitive theory, social ecology and systems theory guided the BHCK intervention (Gittelsohn et al., 2014). The store-level component used social modeling and observational learning to improve knowledge, self-efficacy, and intentions to healthy eating of consumers and create demand for healthy foods at corner stores (Bandura, 1977; Kremers et al., 2006; Rimal, 2001, 2003; Stokols & Daniel, 1992). As individuals and the environment have a reciprocal relationship, BHCK worked with corner store owners to implement environmental changes where the healthy food could be the preferred choice for the community (McLeroy, Bibeau, Steckler, & Glanz, 1988). Finally, a systems approach was implemented to connect each level of the food supply chain and included wholesalers to ensure stocking of the promoted foods at stores. The study was reviewed and approved by the Johns Hopkins Bloomberg School of Public Health’s Institutional Review Board. Further information regarding study design can be found elsewhere (Gittelsohn et al., 2014).
Corner Store and Wholesaler Recruitment
The Johns Hopkins Center for a Livable Future GIS maps in addition to ground truthing techniques aided in identifying corner stores for recruitment (Coakley et al., 2014; Haering & Franco, 2010). Recruited stores were those that agreed to participate and met the following criteria: (1) located within a 1-mile radius of a recreation center, (2) reported being frequently visited by the priority population (10–14-yearold children), (3) independently owned and operated (Buczynski et al., 2015; Gittelsohn et al., 2014). Across the 28 group-randomized neighborhoods, a total of 29 intervention stores and 24 comparison stores, and 2 English-speaking wholesalers (one with two locations) agreed to participate. Stores were classified intervention or comparison, depending on the randomization allocation of the neighborhood in which they were located.
Description of Intervention
Three themed phases, each roughly 2 months in length (1- to 2-week-long breaks were taken between each phase), were used to organize intervention activities throughout the 6-month intervention: smart drinks, smart snacks, and smarter cooking (Table 1; Gittelsohn et al., 2014). Each phase had four subphases that focused on a specific behavioral message and healthy alternative foods (<10% of the daily value for fat, <10% of the daily value for sodium, <10 g sugar in drinks and snacks per serving) to frequently consumed “junk” foods and sugary drinks (Table 1). During Wave 2 of the intervention, three subphases with low initial reach were repeated to increase reach, adding a month to the duration of the intervention (Phase 4). This article will report on all Wave 1 and Phases 1 through 4 of Wave 2 of the intervention.
TABLE 1.
BHCK Intervention Corner Store and Wholesale Promoted Products
| Phase | Theme | Taste Test | Promoted Foods |
|---|---|---|---|
| Smart drinks | |||
| Week 1–2 | Step up your water | Fruit flavored water | Bottled water and zero-calorie flavored water |
| Week 3–4 | Sugar-free drink mixes | Crystal light | Sugar free fruit drink mixes and sugar free tea mixes |
| Week 5–6 | Low-sugar/diet soda | 10 Series | Low sugar and diet soda |
| Week 7–8 | Lower sugar fruit drinks | Big burst | Low sugar fruit drinks and low calorie sports drinks |
| Smart snacks | |||
| Week 9–10 | Sugar substitutions | Chewy granola bars | Low fat yogurt, fruit cups in 100% fruit juice, chewy granola bars |
| Week 10–12 | Salty substitutions | Baked chips | Baked chips, pretzels, low-fat popcorn |
| Week 13–14 | Fruit as a snack | Mandarin oranges | Fresh fruit, fruit cups in 100% fruit juice, unsweetened applesauce |
| Week 15–16 | Nuts seeds and vegetables | Trail-mix without chocolate | Trail-mix without chocolate, sunflower seeds, fresh vegetables, string cheese |
| Smart cooking | |||
| Week 17–18 | Breakfast | Kix cereal and dried fruit | Low-sugar cereal, 1% or skim milk, high fiber cereal |
| Week 19–20 | Wholegrains | Mini whole wheat bagels with peanut butter | 100% wholegrain bread, 100% whole wheat tortillas, brown rice, 100% whole wheat pasta |
| Week 21–22 | Vegetables | Ants on a log | Fresh vegetables, frozen vegetables, low-sodium canned vegetables (<10% DV sodium) |
| Week 23–24 | Cooking methods | Quesadillas or fresh tomato salsa | Cooking spray, low-fat margarine, low-fat/low-sodium condiments |
| Review phasea | |||
| Week 25–26 | Sugar substitutions | 1 chewy granola bar | Low fat yogurt, fruit cups in 100% fruit juice, chewy granola bars |
| Week 27–28 | Vegetables | 1 small baby carrots bag with low-fat dip | Fresh vegetables, frozen vegetables, low-sodium canned vegetables |
| Week 29–30 | Nuts, seeds, and vegetables | Trail mix without chocolate (chex cereal, raisins, almonds, sunflower seeds, and craisins) 1oz | Trail mix without chocolate and small fresh vegetable bags |
NOTE: BHCK = B’More Healthy Communities for Kids; DV = daily value.
Review phase promoted sweet and salty snacks from Phases 1 and 2 and occurred only during BHCK Wave 2 (June–July, 2016).
Wholesale Level
BHCK collaborated with one local wholesale supplier (with two locations) and one national chain store. The wholesalers agreed to ensure stock of three promoted items per subphase, some of which were already in stock, provide discounts and labels containing the program logo on BHCK items on shelves as appropriate, and position the BHCK logo next to promoted products in the circular. Store circulars have been considered as an environmental factor that can shape health-related behaviors and have been described as an effective tool to promote healthful foods (Ethan, Basch, Rajan, Samuel, & Hammond, 2014). The wholesale-level evaluation included seven standards, developed based on previous experience working with wholesalers in Baltimore, related to reach, dose, and fidelity (Table 2; Budd et al., 2015).
TABLE 2.
Process Evaluation of Corner Store and Wholesale Intervention: Percent of High Standard Met
| Process Standard | Percent of High Process Evaluation Standard Meta
|
Overall Process Percenta
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| W1P1b | W1P2b | W1P3b | W2P1b | W2P2b | W2P3b | W2P4b | W1c | W2c | Overalld | |
| Corner store reach | 78 | 81 | 80 | |||||||
| No. of stores participating in BHCK program throughout intervention | 107 | 107 | 100 | 100 | 93 | 86 | 93 | |||
| No. of child (ages 10–14 years) interactions during interactive session | 52 | 76 | 66 | 44 | 56 | 77 | 68 | |||
| No. of adult (ages >18 years) interactions during interactive session | 72 | 68 | 56 | 80 | 77 | 75 | 130 | |||
| Corner store dose delivered | 85 | 101 | 94 | |||||||
| No. of times BHCK team meets with a store owner per phase | 123 | 64 | 89 | 104 | 50 | 43 | 100 | |||
| Length of interactive session | 137 | 115 | 119 | 125 | 127 | 135 | 131 | |||
| Average length of time spent with store owner per meeting | 102 | 84 | 69 | 99 | 77 | 61 | 58 | |||
| No. of food samples distributed per interactive sessions | 132 | 111 | 86 | 114 | 105 | 109 | 108 | |||
| No. of handouts distributed per interactive session | 56 | 62 | 66 | 107 | 107 | 106 | 112 | |||
| No. of giveaways distributed per interactive session | 67 | 78 | 66 | 102 | 109 | 111 | 114 | |||
| No. of times educational display boards are used per phase | 74 | 110 | 104 | 129 | 172 | 177 | 123 | |||
| Total number of promoted food posters positioned by BHCK team per phase | 127 | 129 | 117 | 131 | 121 | 118 | 79 | |||
| No. of shelf labels on promoted foods positioned by BHCK team per visit | 1 | 10 | 10 | 37 | 42 | 43 | 48 | |||
| Corner store fidelity | 85 | 112 | 105 | |||||||
| Percentage of correctly positioned shelf labels by the end of each phase | 67 | 86 | 83 | 81 | 110 | 114 | 147 | |||
| No. of promoted foods stocked per phasee | 104 | 127 | 120 | 131 | 147 | 157 | 143 | |||
| No. of NEW promoted foods introduced per phase | n/af | n/af | n/af | 88 | 169 | 167 | 40 | |||
| No. of (in-person) training videos watched by the end of the interventiong | n/af | n/af | 57 | 74 | 91 | 110 | 117 | |||
| No. of structural incentives earned per store by the end of the intervention | n/af | n/af | 38 | 12 | 76 | 100 | 167 | |||
| Wholesale reach | 150 | 100 | 125 | |||||||
| No. of wholesaler locations participating in program | 150 | 150 | 150 | 100 | 100 | 100 | 100 | |||
| Wholesale dose delivered | n/af | 219 | 219 | |||||||
| No. of times speak per phase | n/af | n/af | n/af | 83 | 33 | 50 | 133 | |||
| No. of e-mails send per phase | n/af | n/af | n/af | 413 | 725 | 263 | 235 | |||
| Average length of time spent with wholesaler per visit | n/af | n/af | n/af | 200 | 83 | 67 | 333 | |||
| Wholesale fidelity | 74 | 124 | 107 | |||||||
| Percent shelf labels correctly placed | n/af | n/af | n/af | 133 | 133 | 133 | 161 | |||
| No. of food items available at wholesaler that meet the BHCK promoted food nutrition guidelines for each phase | 120 | 122 | 122 | 161 | 139 | 150 | 387 | |||
| No. of promoted food items included in wholesaler circular per phasee | 38 | 20 | 21 | 27 | 7 | 30 | 21 | |||
NOTE: BHCK = B’More Healthy Communities for Kids; W = Wave; P = Phase.
Percent reflects the high process evaluation standard. See Supplemental Tables S1 and S2 (available online with this article), respectively, for complete set of wholesale and corner store process standards.
Wave 1, Phase 1, Wave 1, Phase 2, and so on.
Overall percent of the high standard met for each process measure for Wave 1 and Wave 2.
Overall average percentage of the high standard met for each process measure for whole intervention.
Out of a total of 21 promoted products.
Data were not gathered on forms or standard did not exist.
Additional videos may have been viewed online by store owners, but only in-person views are reported.
Corner Store Level
The intervention mirrored previous store trials, but included new innovative components, such as store owner training with an incentive structure to improve knowledge and self-efficacy (Budd et al., 2015; Gittelsohn et al., 2010; Gittelsohn et al., 2013). The tiered incentive structure rewarded owners with structural incentives to address stocking barriers (e.g., produce bins, small refrigerator/freezers, and banana holders) for completing training videos and stocking promoted items. Videos were recorded in English and Korean, with additional translation occurring in-person by a staff person for Mandarin- and Spanish-speaking owners. In addition to training videos, the store interventionist met with owners in person at least once per subphase to provide technical support and troubleshoot challenges. BHCK staff conducted biweekly educational interactive sessions in each store, which included discussions with store customers about key health messages for that subphase (e.g., lower sugar fruit drinks), healthy taste tests, educational displays (e.g., amount of sugar in sugar-sweetened beverage display), handouts containing recipes and nutrition tips, and free giveaways (e.g., water bottles, portion plates). Posters advertised new products and brightly colored shelf labels were positioned under BHCK promoted products, which contained the product name, a photo of the product, and a health message related to each phase (e.g., refuel with a smart snack). An example of these is provided in the Supplemental Figure S1 (available online with this article).
Additional Components
BHCK also provided youth mentor-led nutrition education in recreation centers, worked with local policy makers to develop a sustainability plan for each component, and used social media to increase the project’s reach. Text messaging, Facebook, and Instagram posts advertised store sessions and encouraged the purchase of promoted products. BHCK worked with owners of carryouts, here, defined as an independently owned limited-service prepared food source with few or no seating area, where patron orders and pays before eating (Lee et al., 2010), to design and hang new menus, to advertise healthier sides, drinks, and entrees with a “fresh” logo. Process findings for these components will be reported elsewhere, but are part of the context of intervention implementation reported in this article.
Process Evaluation Instruments
Due to the complex nature of the intervention, it is important to measure and keep track of all components to make sure the intervention was being implemented as planned, and this was also a helpful tool to follow progress and areas needing improvement. Three instruments were modified from previous store trials conducted in Baltimore to assess implementation of corner stores and wholesale components (1) corner store and wholesale environmental assessment, (2) store owner visit form, and (3) the interventionist process evaluation form (Budd et al., 2015; Gittelsohn et al., 2010; Gittelsohn et al., 2013; Shin et al., 2015). Each intervention component and interaction with community partners and study participants were documented and evaluated in detail through multiple process evaluation measures to ensure adequate reach, dose delivered, fidelity to plan (quality), and reproducibility of the intervention (Linnan & Steckler, 2002).
Corner Store and Wholesale Environmental Assessment
Trained data collectors conducted monthly structured observations at both the corner store and wholesale level to assess (1) maintenance of communication materials (e.g., BHCK shelf labels, posters), (2) healthy food availability, and (3) state of the store environment (Budd et al., 2015; Gittelsohn et al., 2010; Gittelsohn et al., 2013; Shin et al., 2015). At the wholesale level, the environmental assessment monitored price changes (e.g., discounts) on promoted items.
Visit Form
Study staff completed visit forms at both the wholesale and corner store level to assess the number and length of meetings with the store owner or wholesale representatives (Gittelsohn et al., 2010).
Interventionist Process Evaluation Form
The interventionist process evaluation form measured (1) the number of communication materials distributed during interactive sessions, (2) taste test acceptance, (3) interactions with community members and their duration (10–60 seconds or >1 minute), and (4) session overall outcome during the biweekly interactive sessions (Gittelsohn et al., 2010).
Data Collector Training
The principal investigator, project coordinator, and study interventionist developed a manual of procedures to standardize the delivery of the program and train data collectors and interventionists. The certification process included an hour-long training, role-play, and supervised practice. Korean, Mandarin, and Spanish translators conducted store owner interviews, reviewed stocking sheets, and maintained regular communication with store owners whose first language was not English. All forms were in English, and the translators transcribed data in English.
Process Evaluation Measures
Based on previous store trials (Budd et al., 2015; Gittelsohn et al., 2010; Gittelsohn et al., 2013), process evaluation standards were developed at the corner store and wholesaler levels, prior to implementation of the intervention, to assess reach, dose delivered, and fidelity (Supplemental Tables S1 and S2, available online with this article). At the wholesale level, reach was calculated based on how many locations participated throughout the program. Dose delivered was defined as the duration and number of meetings between BHCK members and wholesale representatives. Fidelity was assessed based on the number of promoted foods stocked and percent of shelf labels in the correct location. For a complete list of wholesale standards, please see Supplemental Table S1 (available online with this article).
At the corner store level, reach was calculated based on the average number of youth (10–14 years old) and adults (18 years or older) who attended the corner store sessions and the number of stores participating in the program. Dose delivered was determined based on the number of intervention materials (e.g., taste tests, educational handouts) distributed at the interactive session, number of visits, and time spent with store owners. Fidelity was determined based on the number of new products stocked, correct label percentage, and store owner training compliance. For a complete list of corner store standards, see Supplemental Table S2 (available online with this article).
Optimal intervention delivery was defined as meeting a high standard, meaning that the process evaluation indicator met ≥100% of the ideal or high standard set. A medium standard was considered marginally acceptable implementation (50% to <100% of high standard) and low (<50% of high standard) was considered unacceptable intervention delivery. Study staff met regularly throughout the intervention and made changes to optimize program delivery. Implementing the program in two waves eased staff burden and allowed for minor improvements to be made between waves based on best practices and lessons learned.
Data Analysis
Data were entered in Microsoft Access®, 2010, Microsoft® Excel, 2010, and Stata® Version 13.1 were used to calculate descriptive statistics for quantitative data. An average was calculated for each process indicator and reported as a percentage.
RESULTS
Corner Store Owner Demographics
Of the 29 BHCK intervention store owners, 24% (n = 7) were Korean speaking, 3% were Spanish speaking (n = 1), 3% were Mandarin speaking (n = 1), and the remainder were English speaking (n = 20).
Wholesale Level
Reach at the wholesale level remained high during Waves 1 and 2 (150% vs. 100%; Figure 1). The large wholesale chain location experienced change in management during Wave 2 and was unable to contribute adequate time to the program in order to bring in new products, thus decreasing overall reach (Table 2). There was not a dose delivered standard developed during Wave 1, but overall the high standard was met during Wave 2 of the intervention due to improved communication (219%; Table 2). Fidelity at the wholesale level improved from low to high from Wave 1 to Wave 2, due to an overall increase in total promoted foods stocked and high correct label placement (74% vs. 124%; Figure 1).
FIGURE 1. Wholesale Process Evaluation Results.
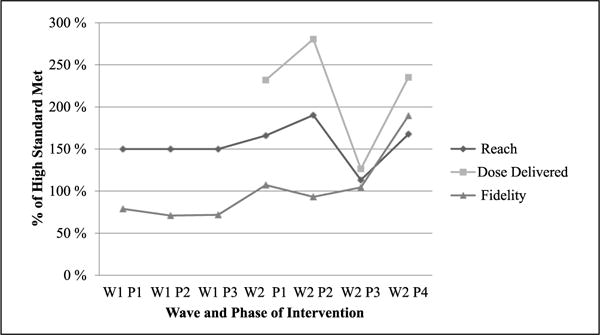
NOTE: W = Wave; P = Phase.
aPercentage of high process evaluation standard achieved. See Supplemental Table S2 (available online with this article) for standards. No dose delivered standards were collected in Wave 1. There were two fidelity process standards evaluated in Wave 1, and three standards were evaluated in Wave 2.
There were a variety of improvements made during Wave 2 to improve program implementation at the wholesale level. During Wave 2, BHCK staff improved communication with more frequent in-person visits, phone calls, and e-mails. To track correspondence, interventionists developed a monitoring form and process evaluation standard to track these interactions in Wave 2. There was not only an increase in e-mail communication during Wave 2, due to its efficiency and effectiveness for both parties, but also a corresponding decrease in in-person visits, especially during Phases 2 and 3 of Wave 2. BHCK successfully provided training through in-person meetings, working with the purchasing manager and the marketing team at the local wholesale supplier to ensure products could be ordered, stocked, and advertised with the BHCK logo both on the shelves and in the circular (e.g., sales catalog). In addition, BHCK was able to provide the wholesalers with ongoing feedback and data from the storeowners that the team interacted with on a regular basis, further incentivizing them to make healthy stocking changes.
Corner Store Level
The intervention had moderate reach during Waves 1 and 2 (78% vs. 81%; Figure 2). BHCK consistently struggled with attracting youth to the store sessions, especially during the winter months, decreasing overall reach during both waves. Corner store dose delivered increased from moderate in Wave 1 to high in Wave 2 (85% vs. 101%; Table 2). A total of 7,784 food samples, 6,121 educational handouts, and 6,402 giveaways were distributed at the corner store level over the course of the intervention. Overall fidelity in Wave 1 was moderate, but improved during Wave 2, meeting the high standard (85% vs. 112%; Figure 2). An increase in participation in store owner training, promoted food stocking, correct label placement, and a corresponding increase in incentive distribution led to an increase in overall fidelity.
FIGURE 2. Corner Store Process Evaluation Results.
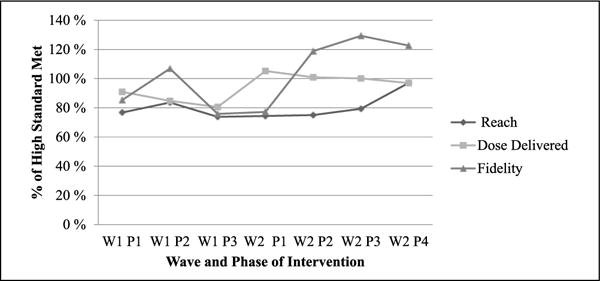
NOTE: W = Wave; P = Phase.
aPercentage of high process evaluation standard achieved. See Supplemental Tables S1 and S2 (available online with this article) for standards. Four fidelity measures were evaluated for Wave 1, and five standards for Wave 2.
Improvements were also made at the corner store level prior to the start of Wave 2. During Wave 1, store owners were asked to watch training videos in order to receive a structural incentive. During Wave 2, BHCK redesigned the store owner incentive structure to encourage owners to watch all six training videos, stock at least two new items per phase, and maintain at least 50% of their shelf labels in the right location. The team also provided store owners with more frequent reminders regarding upcoming promoted products, resulting in an average of 3.4 new products stocked per phase. Staff also distributed one gift-card per subphase, instead of all at the beginning of the phase, to encourage the purchase of one promoted product at a time. Finally, BHCK staff provided store owners with a “store owner binder,” which contained an intervention calendar, promoted product sheets with images, and brands of promoted products that could be found at the wholesaler, and an incentive chart and contact information. Store owners used the binder to track upcoming promoted products, interactive session dates, and incentive progress.
DISCUSSION
This is the first article to report on process evaluation measures at both the corner store and wholesale level. BHCK implementation took place in two distinct waves, which allowed for improvements to be made prior to Wave 2 implementation. The program had a 56% increase in community members interactions throughout the duration of the program than previous corner store trials in Baltimore (Gittelsohn et al., 2013). BHCK also maintained a higher percent of label placement than Baltimore Healthy Eating Zones, a previous Baltimore corner store trial, (73.9% vs. 36% correct label placement, respectively; Gittelsohn et al., 2013). Point of purchase labeling alone has been found to influence customers’ decisions to purchase healthier alternatives and is a cost-effective mode of education (Escaron et al., 2013).
Our study was able to test a theory-based multilevel multicomponent obesity prevention trial implemented in collaboration with city stakeholders to improve the healthy food supply chain for low-income communities. Emphasis was placed on the interaction and influence between the institutional and intrapersonal levels (retailer discounts, point of purchase promotions, and health education), based on the socioecological model. In addition, over the course of the intervention, we built strong rapport with different components of the BHCK project across all levels of the intervention— including Baltimore officials, local wholesalers, and retail food stores/carryouts—which may help explain the increase seen in terms of process evaluation outcomes over time (Wave 1 vs. Wave 2). However, it is worth mentioning that this temporal improvement in intervention implementation due to rapport built with the community is rarely addressed in social and behavioral theories.
BHCK used a model that did not involve a financial incentive for wholesalers as in previous trials, but rather used direct demand from corner stores as an incentive for stocking new items (Budd et al., 2015). Many store owners indicate that suppliers are the limiting step for stocking healthier food (New York City Department of Health and Mental Hygiene, 2013). Wholesale representatives were most interested in how they could increase their sales and decrease their financial risk for stocking a new product. The wholesale locations that participated in BHCK followed both an “operator driven logistic” and a “specialized distribution company” model, which made corner store owner needs a priority (The Food Trust, 2015).
BHCK staff also sent biweekly e-mails to participating wholesale locations. The e-mails included total dollar amount in wholesale gift cards distributed to store owners, number of posts made on social media promoting their business, and upcoming promoted product needs, including total number of each item, brand, and unit size. These e-mails not only served as a program update but also informed wholesalers of what healthy products store owners were interested in purchasing. BHCK staff also communicated the number of likes or impressions on wholesale-related social media posts to further inform wholesalers of the community’s response to their participation in the program. Future work with wholesalers can encourage group bulk-purchasing to lower the cost of healthy products for small store owners. In the network model by Mui et al. (2015), the wholesaler supplier category was central to the healthy and unhealthy food supply networks for corner stores.
In addition to fluid communication, full-time Korean interventionists played an important role in program implementation. Korean store owners reported feeling more comfortable participating in the program with an interventionist who spoke their native language (Song et al., 2011). To increase rapport and communication, a full-time English-speaking store interventionist provided all other owners with a consistent point of contact throughout both Wave 1 and Wave 2 of the program. The relationship between the store owners, wholesale representatives, and interventionist were key for successful program implementation.
The study had the following barriers to implementation. During the Wave 1, frequent store renovation at two out of the three wholesalers may have interfered the fidelity of the study implementation, with incorrect label placement and irregular stocking patterns. In addition, only two local wholesale locations (out of three locations) actively stocked new BHCK promoted items on request for the entire duration of the intervention. The two local wholesale stores were more willing and able to stock new items, brands, and shift stock with short notice than the national chain wholesale supplier. Similar to The Food Trust’s (2015) findings, the national chain wholesale location struggled to stock items in small enough quantities for small store owners to afford and have room for in their small stores. The incentive methods to the wholesaler could be revised and improved to address the supply chain needs.
The study had several limitations. New standards for both the wholesale and corner store level of the intervention were developed to more closely evaluate program implementation, but made comparability difficult between waves. Significant staff turnover from Wave 1 to Wave 2 may have affected consistency of implementation between waves. However, a manual of procedures was used during both waves to document standards and best practices for implementation at all intervention levels. BHCK only worked with two wholesaler companies (three locations total) and approximately 4% of all corner stores/convenience stores in Baltimore City due to limited funding and staff (Haering & Franco, 2010). It is important to note that BHCK worked with one wholesaler who was already central to the corner store supply network in Baltimore. Consequently, results may not be generalizable to other cities.
Findings revealed that wholesale suppliers require a direct demand from store owners (i.e., specific type and number of product to be purchased) to decrease the perceived financial risk of stocking a new product. BHCK program staff found that local wholesalers were more readily able to bring in new products in small enough quantities for corner store owners than national wholesaler chains. Persistent communication at both the store and wholesale level were vital to achieve a moderate to high level of implementation and to increase stocking at the corner store level.
Current literature lacks standardized process evaluation guidelines for corner store trials, which limits comparison and establishment of best practices (Gittelsohn et al., 2008). This study serves as a resource for best practices as well as a framework for process evaluation standard development for future corner store and wholesale-level interventions. Future studies can choose the measures that are most appropriate for their setting. While work in small urban corner stores is increasingly common, almost none of this work has sought to involve wholesalers and other suppliers of these stores. This is one of the first intervention trials to do so, and therefore, the implementation data provided are essential for developing and implementing sustainable interventions in small urban food stores and supporting policies. Recommendations for future trials include (1) integrating suppliers into the planning, product selection, and implementation of corner store trials; (2) updating wholesalers on the financial benefits to their organization throughout the program; and (3) using and reporting process evaluation measures in interventions to determine areas for improvement of intervention quality.
Supplementary Material
Acknowledgments
Authors’ Note: Research reported in this publication was supported by the Global Obesity Prevention Center at Johns Hopkins, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, and the Office of the Director, National Institutes of Health (Award No. U54HD070725). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
SUPPLEMENTAL MATERIAL
The Supplemental Material is available online with this article.
References
- Andreyeva T, Middleton AE, Long MW, Luedicke J, Schwartz MB. Food retailer practices, attitudes and beliefs about the supply of healthy foods. Public Health Nutrition. 2011;14:1024–1031. doi: 10.1017/S1368980011000061. [DOI] [PubMed] [Google Scholar]
- Baltimore City Health Department. Baltimore Community Health Survey 2014: Summary results report. 2014 Retrieved from http://health.baltimorecity.gov/sites/default/files/BCHD%20CHS%20Report%20Sept%2016%202015.pdf.
- Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review. 1977;84:191–215. doi: 10.1037/0033-295X.84.2.191. [DOI] [PubMed] [Google Scholar]
- Biro FM, Wien M. Childhood obesity and adult morbidities. American Journal of Clinical Nutrition. 2010;91(5):1499S–1505S. doi: 10.3945/ajcn.2010.28701B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodor JN, Ulmer VM, Dunaway LF, Farley TA, Rose D. The rationale behind small food store interventions in low-income urban neighborhoods: Insights from New Orleans. Journal of Nutrition. 2010;140:1185–1188. doi: 10.3945/jn.109.113266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borradaile KE, Sherman S, Vander Veur SS, McCoy T, Sandoval B, Nachmani J, Foster GD. Snacking in children: The role of urban corner stores. Pediatrics. 2009;124:1293–1298. doi: 10.1542/peds.2009-0964. [DOI] [PubMed] [Google Scholar]
- Buczynski A, Freishtat H, Buzogany S. Mapping Baltimore city’s food environment 2015 report. 2015 Retrieved from http://mdfoodsystemmap.org/wp-content/uploads/2015/06/Baltimore-Food-Environment-Report-2015-1.pdf.
- Budd N, Cuccia A, Jeffries JK, Prasad D, Frick KD, Powell L, Gittelsohn J. B’More healthy: Retail rewards-design of a multi-level communications and pricing intervention to improve the food environment in Baltimore City. BMC Public Health. 2015;15(1):283. doi: 10.1186/s12889-015-1616-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi CE, Pelletier JE, Harnack L, Erickson DJ, Laska MN. Differences in healthy food supply and stocking practices between small grocery stores, gas-marts, pharmacies and dollar stores. Public Health Nutrition. 2016;19:540–507. doi: 10.1017/S1368980015002724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Healthier food retail: An action guide for public health practitioners. 2014 Retrieved from https://www.cdc.gov/nccdphp/dnpao/state-local-programs/pdf/healthier-food-retail-guide-full.pdf.
- Coakley HL, Steeves EA, Jones-Smith JC, Hopkins L, Braunstein N, Mui Y, Gittelsohn J. Combining ground-truthing and technology to improve accuracy in establishing children’s food purchasing behaviors. Journal of Hunger & Environmental Nutrition. 2014;9:418–430. doi: 10.1080/19320248.2014.898173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Angelo H, Suratkar S, Song HJ, Stauffer E, Gittelsohn J. Access to food source and food source use are associated with healthy and unhealthy food-purchasing behaviours among low-income African-American adults in Baltimore city. Public Health Nutrition. 2011;14:1632–1639. doi: 10.1017/S1368980011000498. [DOI] [PubMed] [Google Scholar]
- Díez J, Bilal U, Cebrecos A, Buczynski A, Lawrence RS, Glass T, Franco M. Understanding differences in the local food environment across countries: A case study in Madrid (Spain) and Baltimore (USA) Preventive Medicine. 2016;89:237–244. doi: 10.1016/j.ypmed.2016.06.013. [DOI] [PubMed] [Google Scholar]
- Escaron AL, Meinen AM, Nitzke SA, Martinez-Donate AP. Supermarket and grocery store-based interventions to promote healthful food choices and eating practices: A systematic review. Preventing Chronic Disease. 2013;10:E50. doi: 10.5888/pcd10.120156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estrada E, Eneli I, Hampl S, Mietus-Snyder M, Mirza N, Rhodes E, … Children’s Hospital Association. Children’s Hospital Association consensus statements for comorbidities of childhood obesity. Childhood Obesity. 2014;10:304–317. doi: 10.1089/chi.2013.0120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ethan D, Basch CH, Rajan S, Samuel L, Hammond RN. A comparison of the nutritional quality of food products advertised in grocery store circulars of high versus low-income New York city zip codes. International Journal of Environmental Research and Public Health. 2014;11:537–547. doi: 10.3390/ijerph110100537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans A, Banks K, Jennings MR. Increasing access to healthful foods: A qualitative study with residents of low-income communities. International Journal of Behavioral Nutrition and Physical Activity. 2015;12:1–27. doi: 10.1186/1479-5868-12-S1-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. JAMA Journal of the American Medical Association. 2016;315:2284–2291. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Food Trust. Healthy food supply in small stores : Exploring the distribution gap existing distribution models for small stores. 2015 Retrieved from http://thefoodtrust.org/uploads/media_items/healthy-food-and-small-stores.original.pdf.
- Franco M, Diez Roux AV, Glass TA, Caballero B, Brancati FL. Neighborhood characteristics and availability of healthy foods in Baltimore. American Journal of Preventive Medicine. 2008;35:561–567. doi: 10.1016/j.amepre.2008.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gittelsohn J, Anderson Steeves E, Mui Y, Kharmats AY, Hopkins LC, Dennis D. B’More Healthy Communities for Kids: Design of a multi-level intervention for obesity prevention for low-income African American children. BMC Public Health. 2014;14:942. doi: 10.1186/1471-2458-14-942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gittelsohn J, Dennisuk LA, Christiansen K, Bhimani R, Johnson A, Alexander E, Coutinho AJ. Development and implementation of Baltimore Healthy Eating Zones: A youth-targeted intervention to improve the urban food environment. Health Education Research. 2013;28:732–744. doi: 10.1093/her/cyt066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gittelsohn J, Franceschini MCT, Rasooly IR, Ries AV, Lara SHo, Pavlovich W, Frick KD. Understanding the Food Environment in a low-income urban setting: Implications for food store interventions. Journal of Hunger & Environmental Nutrition. 2008;2:33–50. doi: 10.1080/19320240801891438. [DOI] [Google Scholar]
- Gittelsohn J, Rowan M, Gadhoke P. Interventions in small food stores to change the food environment, improve diet, and reduce risk of chronic disease. Preventing Chronic Disease. 2012;9:E59. Retrieved from http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3359101&tool=pmcentrez&rendertype=abstract. [PMC free article] [PubMed] [Google Scholar]
- Gittelsohn J, Steeves E, Mui Y, Kharmats A, Hopkins L, Dennis D. B’More Healthy Communities for Kids: Design of a multi-level intervention for obesity prevention for low-income African American children. BMC Public Health. 2014;14:942. doi: 10.1186/1471-2458-14-942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gittelsohn J, Suratkar S, Song HJ, Sacher S, Rajan R, Rasooly IR, Anliker JA. Process evaluation of Baltimore healthy stores: A pilot health intervention program with supermarkets and corner stores in Baltimore city. Health Promotion Practice. 2010;11:723–732. doi: 10.1177/1524839908329118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K, Sallis JF, Saelens BE, Frank LD. Nutrition Environment Measures Survey in Stores (NEMS-S): Development and evaluation. American Journal of Preventive Medicine. 2007;32:282–289. doi: 10.1016/j.amepre.2006.12.019. [DOI] [PubMed] [Google Scholar]
- Haering SA, Franco M. The Baltimore city food environment. The Johns Hopkins Center for a Livable Future; 2010. Retrieved from http://www.jhsph.edu/clf/PDF_Files/BaltimoreCityFoodEnvironment.pdf. [Google Scholar]
- Kiszko K, Cantor J, Abrams C, Ruddock C, Moltzen K, Devia C, Elbel B. Corner store purchases in a low-income urban community in NYC. Journal of Community Health. 2015;40:1084–1090. doi: 10.1007/s10900-015-0033-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kremers SPJ, de Bruijn GJ, Visscher TLS, van Mechelen W, de Vries NK, Brug J. Environmental influences on energy balance-related behaviors: A dual-process view. International Journal of Behavioral Nutrition and Physical Activity. 2006;3:9. doi: 10.1186/1479-5868-3-9. http://doi.org/10.1186/1479-5868-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SH, Rowan MT, Powell LM, Newman S, Klassen AC, Frick KD, Gittelsohn J. Characteristics of prepared food sources in low-income neighborhoods of Baltimore city. Ecology of Food and Nutrition. 2010;49:409–430. doi: 10.1080/03670244.2010.524102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linnan L, Steckler A. Process evaluation in public health interventions and research: An overview. In: Steckler A, Linnan L, editors. Process evaluation in public health interventions and research. San Francisco, CA: Jossey-Bass; 2002. pp. 1–23. [Google Scholar]
- Martin KS, Ghosh D, Page M, Wolff M, McMinimee K, Zhang M. What role do local grocery stores play in urban food environments? A case study of Hartford-Connecticut. PLoS ONE. 2014;9(4):e94033. doi: 10.1371/journal.pone.0094033. Retrieved from http://www.scopus.com/inward/record.url?eid=2-s2.0-84899499410&partnerID=40&md5=18c36c234aa79bc655b12289334ca5c4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Education Quarterly. 1988;15:351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- Moore LV, Pinard CA, Yaroch AL. Features in grocery stores that motivate shoppers to buy healthier foods, consumer styles 2014. Journal of Community Health. 2016;41:812–817. doi: 10.1007/s10900-016-0158-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mui Y, Lee BY, Adam A, Kharmats AY, Budd N, Nau C, Gittelsohn J. Healthy versus unhealthy suppliers in food desert neighborhoods: A network analysis of corner stores’ food supplier networks. International Journal of Environmental Research and Public Health. 2015;12:15058–15074. doi: 10.3390/ijerph121214965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New York City Department of Health and Mental Hygiene. Shop Healthy NYC 2013 [Google Scholar]
- O’Malley K, Gustat J, Rice J, Johnson C. Feasibility of increasing access to healthy foods in neighborhood corner stores. Journal of Community Health. 2013;38:741–749. doi: 10.1007/s10900-013-9673-1. [DOI] [PubMed] [Google Scholar]
- Ogden C, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA Journal of the American Medical Association. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell LM, Slater S, Mirtcheva D, Bao Y, Chaloupka FJ. Food store availability and neighborhood characteristics in the United States. Preventive Medicine. 2007;44:189–195. doi: 10.1016/j.ypmed.2006.08.008. [DOI] [PubMed] [Google Scholar]
- Rimal RN. Longitudinal influences of knowledge and self-efficacy on exercise behavior: Tests of a mutual reinforcement model. Journal of Health Psychology. 2001;6:31–46. doi: 10.1177/135910530100600103. [DOI] [PubMed] [Google Scholar]
- Rimal RN. Intergenerational transmission of health: The role of intrapersonal, interpersonal, and communicative factors. Health Education & Behavior. 2003;30:10–28. doi: 10.1177/1090198102239256. [DOI] [PubMed] [Google Scholar]
- Shin A, Surkan PJ, Coutinho AJ, Suratkar SR, Campbell RK, Rowan M, Gittelsohn J. Impact of Baltimore Healthy Eating Zones: An environmental intervention to improve diet among African American youth. Health Education & Behavior. 2015;42(1 Suppl):97S–105S. doi: 10.1177/1090198115571362. [DOI] [PubMed] [Google Scholar]
- Song HJ, Gittelsohn J, Kim M, Suratkar S, Sharma S, Anliker J. Korean American storeowners’ perceived barriers and motivators for implementing a corner store-based program. Health Promotion Practice. 2011;12:472–482. doi: 10.1177/1524839910364369. [DOI] [PubMed] [Google Scholar]
- Stokols D, Daniel Establishing and maintaining healthy environments: Toward a social ecology of health promotion. American Psychologist. 1992;47:6–22. doi: 10.1037/0003-066X.47.1.6. [DOI] [PubMed] [Google Scholar]
- Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, Gortmaker SL. The global obesity pandemic: Shaped by global drivers and local environments. The Lancet. 2011;378:804–814. doi: 10.1016/S0140-6736(11)60813-1. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Quick facts: Baltimore City, Maryland. 2015 Retrieved from https://www.census.gov/quickfacts/table/PST045214/24510/embed/accessible.
- Vedovato GM, Surkan PJ, Jones-Smith J, Steeves EA, Han E, Trude AC, Gittelsohn J. Food insecurity, overweight and obesity among low-income African-American families in Baltimore City: Associations with food-related perceptions. Public Health Nutrition. 2016;19:1405–1416. doi: 10.1017/S1368980015002888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker RE, Keane CR, Burke JG. Disparities and access to healthy food in the United States: A review of food deserts literature. Health & Place. 2010;16:876–884. doi: 10.1016/j.healthplace.2010.04.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


