Key Points
There is currently no clear consensus on the best approach to the management of patients with APS and arterial thrombosis.
Combined antiplatelet and anticoagulant therapy may decrease risk of thrombosis recurrence in patients with APS and arterial thrombosis.
Abstract
Management for patients with antiphospholipid syndrome (APS) and arterial thrombosis is controversial. There are no prospective data demonstrating the superiority of high- or moderate-intensity anticoagulation with vitamin K antagonists over antiplatelet agents. Using 2 antiphospholipid antibody databases (single center [New York Presbyterian Hospital] and multicenter [Antiphospholipid Syndrome Alliance for Clinical Trials and International Networking]), we retrospectively collected demographic and clinical data of patients with APS and arterial thrombosis. The primary outcome was recurrent thrombosis rate after initial arterial thrombosis in patients with APS treated with antiplatelet and/or anticoagulant therapy. We identified 139 patients with a median follow-up time of 4.24 years after initial thrombosis. Thirty-seven patients (27.3%) received anticoagulants, 43 (30.9%) antiplatelets, and 58 (41.7%) combined therapy. Sixteen patients (37.2%) in the antiplatelet group, 9 (23.7%) in the anticoagulant group, and 4 (6.9%) in the combined therapy group experienced recurrent thrombosis. We estimate that 20% of patients will experience a recurrence by 3.4, 7.3, and 16.3 years, respectively, depending on assignment to antiplatelet, anticoagulant, or combined therapy. These results suggest that combined therapy decreases the rate of and increases the time to thrombosis recurrence in patients with APS presenting with arterial thrombosis.
Visual Abstract
Introduction
Antiphospholipid syndrome (APS) is characterized by vascular thrombosis and/or pregnancy morbidity in patients with persistently positive antiphospholipid (aPL) antibodies.1,2 Management for patients with APS presenting with arterial thrombosis remains controversial, with no prospective data demonstrating the superiority of high- or moderate-intensity anticoagulation with vitamin K antagonists (VKAs) over antiplatelet agents.3-7 The Antiphospholipid Antibodies and Stroke Study (APASS) showed that a positive lupus anticoagulant (LA) or anticardiolipin antibodies (aCL) antibody among patients with ischemic stroke did not predict either increased risk for subsequent vascular occlusive events over 2 years or a distinct response to aspirin or VKAs.8 Another study evaluated the effect of treatments for secondary thromboprophylaxis in 20 patients presenting with a stroke, suggesting that a combination of antiplatelet and anticoagulant agents may be superior to antiplatelets alone.9 We sought to determine the rate of recurrent thrombosis after initial arterial thrombosis in patients with APS treated with antiplatelet and/or anticoagulant therapy.
Methods
Using 2 aPL antibody databases (single center [New York Presbyterian Hospital (NYPH) from January 2006 to June 2016] and multicenter [Antiphospholipid Syndrome Alliance for Clinical Trials and International Networking (APS ACTION) from August 2012 to June 2016]),10 we retrospectively analyzed demographic and clinical data of patients with APS who presented with arterial thrombosis. Data included sex, age, ethnicity, number of cardiovascular (CV) risk factors (including hypertension, smoking, hyperlipidemia, diabetes, and family history of early CV disease), type of aPL antibody, concomitant autoimmune disorders, and treatment modalities (antiplatelet and/or anticoagulant). Patients were observed until first recurrent thrombosis (arterial, venous, or microvascular) or last clinic or registry visit. Baseline measures across treatment groups were compared using χ2 and Kruskal-Wallis tests for categorical and continuous variables, respectively. Kaplan-Meier curves with log-rank tests as well as Cox proportional hazards regression were used to examine the primary outcomes of this study: rate of and time to recurrent thrombosis. Therapies were determined at the time of start of treatment and may have changed over time. However, we analyzed patients according to intention to treat.
Patients were eligible for the study if they were ≥18 years of age, had a history of arterial thrombosis, and moderate- to high-titer aPL enzyme-linked immunosorbent assay (aCL, anti-β2 glycoprotein-1), immunoglobulin G (IgG), IgM, and IgA isotypes (≥40 U/mL), and/or positive LA test on 2 occasions ≥ 12 weeks apart as per the updated Sapporo APS Classification Criteria.11 Triple positivity was defined as having positive LA, aCL, and anti-β2 glycoprotein-1 antibodies. Arterial thrombosis was defined as cerebrovascular accident (CVA), transient ischemic attack (TIA), myocardial infarction, or other acute arterial thrombosis (renal, splanchnic, peripheral). Additionally, patients had to be treated with antiplatelet agents (aspirin and/or clopidogrel), anticoagulants, or both after initial arterial event. Patients who had presented with venous thrombosis or a combination of arterial and venous thromboses were excluded. Diagnostic criteria for CVA included presence of a sudden onset of neurological deficit, with evidence of new brain injury on computed tomography (CT) or magnetic resonance imaging. Diagnosis of TIA was defined as the sudden onset of neurological deficit lasting <24 hours, without evidence of brain injury by either CT or brain magnetic resonance imaging. The definition of acute arterial thrombosis included new onset of pain or paleness in 1 area of the body, with objective documentation of occlusion of a blood vessel or infarct on CT scan or angiography.
NYPH database
We reviewed the electronic medical records of all patients with APS. We recorded 170 patients, 121 of whom were excluded because they did not meet the inclusion criterion of initial isolated arterial thrombosis. Of the 49 remaining patients, 23 were excluded because of incomplete documentation (resulting from either absence of aPL antibody confirmatory results or lack of follow-up after initial office visit). The target international normalized ratio (INR) for patients receiving VKAs was between 2 and 3. Patient follow-up occurred every 6 to 12 months at NYPH. In the APS ACTION registry, each center generally performs follow-up of its patients every 3 to 12 months. Recurrence included any type of thrombosis (arterial, venous, or microvascular). Documentation of recurrence was based on clinical history and/or objective documentation by imaging study.
APS ACTION
Individual clinicians from 25 centers around the world contribute patients to the APS ACTION clinical database and repository (registry). Retrospective and cross-sectional data are collected at registry entry. Patients are subsequently followed prospectively once a year and/or at the time of new aPL antibody–related thrombosis or pregnancy morbidity. For the purpose of this study, we used only those data collected at registry entry, which were based on retrospective follow-up of patients at different centers every 3 to 12 months. As of December 2016, there were 638 patients enrolled; 138 had presented with arterial thrombosis. Of these, 25 were excluded because they did not fulfill the eligibility criteria; a total of 113 patients were included. The target INR was not recorded in this database. The NYPH institutional review board approved the study.
Results
There were 139 patients identified; 92 (66.2%) were female (Table 1). Median age at first thrombotic event was 43 years (range, 15-84 years). Eighty-five (61.2%) were white, 19 (13.7%) Hispanic, 13 (9.4%) Asian, 6 (4.3%) black, and 1 (0.7%) Middle Eastern; the ethnicities of 15 patients (10.8%) were not recorded. Median follow-up time from initial thrombosis was 4.24 years.
Table 1.
Patient baseline characteristics, recurrence rate, and recurrence by initial site of thrombosis
| Characteristic | Therapy, no. (%) | P | Overall, no. (%) | ||
|---|---|---|---|---|---|
| Anticoagulant | Antiplatelet | Combined therapy | |||
| Overall | 38 (27.3) | 43 (30.9) | 58 (41.7) | 139 | |
| Median (range) age at first thrombosis, y | 37 (22-75) | 46 (15-84) | 42 (15-65) | .011 | 43 (15-84) |
| Sex | .053 | ||||
| Female | 30 (78.9) | 23 (53.5) | 39 (67.2) | 92 (66.2) | |
| Male | 8 (21.1) | 20 (46.5) | 19 (32.8) | 47 (33.8) | |
| Ethnicity | .188 | ||||
| Asian | 3 (7.9) | 8 (18.6) | 2 (3.4) | 13 (9.4) | |
| Black | 2 (5.3) | 1 (2.3) | 3 (5.2) | 6 (4.3) | |
| White | 22 (57.9) | 26 (60.5) | 37 (63.8) | 85 (61.2) | |
| Middle Eastern | 0 (0.0) | 1 (2.3) | 0 (0.0) | 1 (0.7) | |
| Hispanic | 7 (18.4) | 2 (4.7) | 10 (17.2) | 19 (13.7) | |
| Not Reported | 4 (10.5) | 5 (11.6) | 6 (10.3) | 15 (10.8) | |
| Median (IQR) no. of CV risk factors | 2 (1-3.25) | 1 (1-2) | 1.5 (1.25-1.75) | .908 | 1 (1-2.25) |
| Location of initial thrombosis | .003 | ||||
| Cardiac | 2 (5.3) | 9 (20.9) | 5 (8.6) | 16 (11.5) | |
| Cerebral | 25 (65.8) | 33 (76.7) | 43 (74.1) | 100 (71.9) | |
| Other* | 11 (28.9) | 1 (2.3) | 10 (17.2) | 22 (15.8) | |
| Triple-positive aPL antibodies | 12 (31.6) | 17 (39.5) | 21 (36.2) | .757 | 50 (36.0) |
| Recurrence observed | |||||
| Location of initial thrombosis | |||||
| Cardiac (n = 16) | 1 (50) of 2 | 2 (22) of 9 | 0 (0) of 5 | 3 (20) of 16 | |
| Cerebral (n = 101) | 6 (24) of 25 | 13 (39) of 33 | 4 (9) of 43 | 23 (23) of 101 | |
| Other* (n = 22) | 2 (18) of 11 | 1 (100) of 1 | 0 (0) of 10 | 3 (14) of 22 | |
| All, % | 9 | 16 | 4 | 29 | |
IQR, interquartile range.
Describes initial acute arterial location that did not occur at cerebral or cardiac site.
Only 1 patient in the NYPH database had atrial fibrillation. There were 3 patients receiving dual antiplatelet agents in the NYPH database and 8 in the APS ACTION registry. Median age at initial thrombosis significantly differed across treatment groups, at 37, 46, and 42 for the anticoagulant, antiplatelet, and combined therapy groups, respectively (P = .011). Initial thrombosis was observed mainly in the cerebrovascular system, with 15 patients presenting with CVA and 5 with TIA at NYPH and 80 with CVA in the APS ACTION registry. Patients presenting with cardiac events were more likely to be treated with antiplatelet agents rather than anticoagulants or combined therapies (P = .002).
Of 139 patients, 48 (34.5%) had an underlying autoimmune disorder and 50 (36%) had triple-positive aPL antibody. Interestingly, we did not identify any significant differences in outcome when comparing treatment groups in the presence versus absence of autoimmune disorders or triple positivity (log rank P = .90).
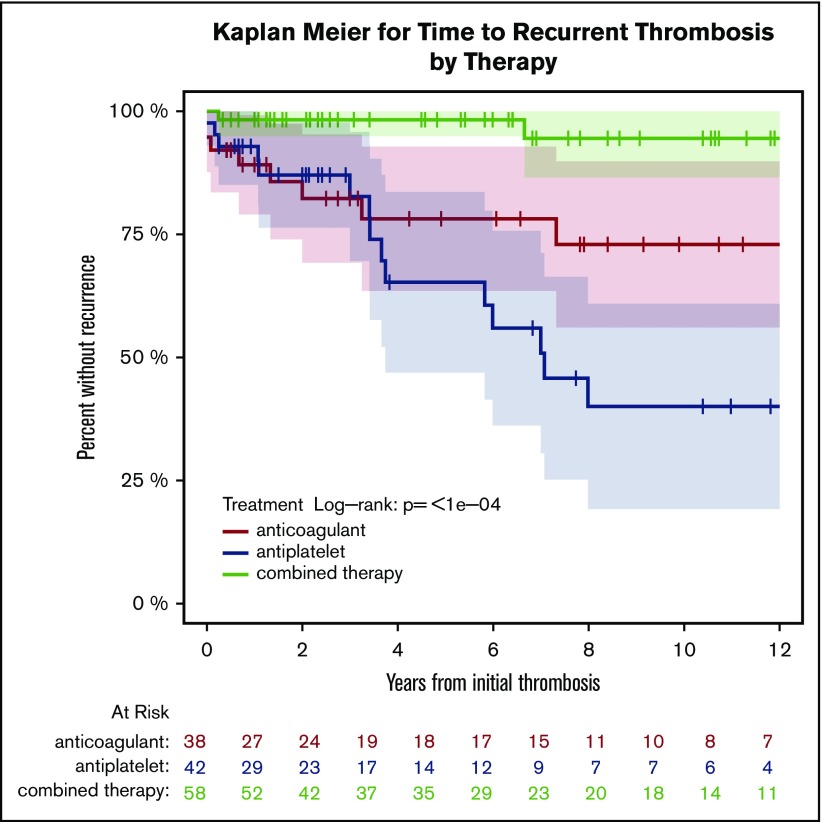
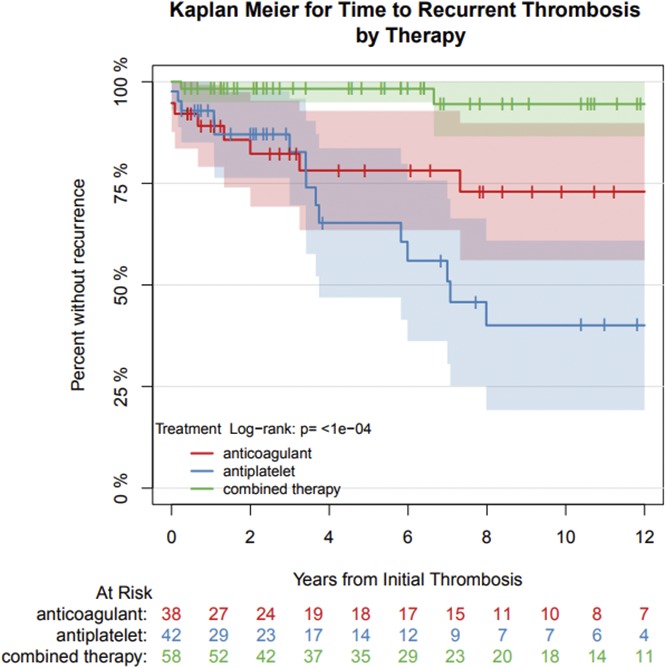
Sixteen patients (37.2%) in the antiplatelet group, 9 (23.7%) in the anticoagulant group, and 4 (6.9%) in the combined therapy group experienced recurrent thrombosis during the study period. Of the 29 recurrences, 18 were arterial, 10 were venous, and 1 was a thrombotic microangiopathy. We estimated that 20% of patients would experience a recurrent thrombotic event within 7.3 years of the initial event. Time to thrombotic recurrence varied according to treatment group (Figure 1; log-rank P < .001), with patients receiving antiplatelet therapy having the highest risk of recurrence. We estimate that 20% of patients will experience recurrence by 3.4, 7.3, and 16.3 years, respectively, depending on assignment to antiplatelet, anticoagulant, or combined therapy. Compared with patients receiving anticoagulants, those receiving antiplatelet agents had a 2.1-fold increase in hazard of recurrence, although because of low power, the difference did not demonstrate a statistically significant trend (95% CI, 0.90-4.7; P = .09). Patients receiving combined therapy had a 70% lower hazard of a recurrent event (hazard ratio, 0.30; 95% CI, 0.08-0.83; P < .025; Figure 1). These results did not differ when accounting for age and sex in multivariable regression. One patient experienced a nonmajor clinically relevant bleeding event in the NYPH database. There were no documented deaths in the NPYH registry. In the APS ACTION registry, death was an exclusion criterion for inclusion in our analysis.
Figure 1.
Kaplan-Meier curve of time to recurrent thrombosis by therapy.
Discussion
Our results differ from those of the APASS trial in that our study patients who received antiplatelet therapy (aspirin and/or clopidogrel) had the highest thrombotic recurrence rate compared with patients in the APASS trial where the thrombotic recurrence rate was similar for patients receiving aspirin or warfarin. Furthermore, our study had a longer median follow-up period of 4.24 years compared with 2 years in the APASS trial.
The 24% recurrence rate of vascular thrombosis in warfarin-treated patients in our study is similar to the reported 26% rate in the Warfarin Aspirin Stroke Study (WARSS).12 However, in the WARSS study, the target INR range was lower (INR, 1.4-2.8) than the INR of 2.0 to 3.0 among patients in the NYPH database. We found a higher rate of thrombotic recurrence (37.2%) in aspirin-treated patients in our study compared with 22% of aPL antibody–negative treated patients in the WARSS trial.
The major strength of our study was the ability to evaluate 3 different therapeutic alternatives (antiplatelet, anticoagulant, or combined therapy) in patients with APS with arterial thrombosis. The superiority of combined therapy in the current study highlights the multifactorial nature of thrombosis in these patients with complex disease. However, even among those receiving combined therapy, a substantial number (7%) developed a recurrent event during the study period, indicating the need for novel therapeutic approaches in this population. The heterogeneity of thrombotic risk factors complicates both study design and treatment decisions for patients with APS.13 This heterogeneity provides a putative explanation for the success of combined therapy in achieving adequate secondary thromboprophylaxis, because coverage of a wider range of thrombotic causes may reduce risk of recurrence. This explanation is 1 of several and requires further evaluation with prospective multicenter studies. An additional strength of our study was the inclusion of patients from the APS ACTION registry, which provides a global representation of patients with APS.
Our study has limitations that may have affected our conclusions. The retrospective design, the relatively small number of patients and recurrent events observed, and the inability to evaluate therapy compliance and INR value at the time of thrombotic events are some of those limitations. Furthermore, bleeding information was not available in the APS ACTION registry during data collection for this study. Additionally, CV risk factors were recorded at the time of enrollment in the APS ACTION registry (not at time of recurrent event). Most importantly, therapy was chosen by the treating physician; thus, different clinical characteristics and recurrence rates across therapy groups may have resulted from selection bias and cannot be attributed to the therapy alone. Moreover, the different recurrence rates in the 3 groups may reflect different pathophysiology rather than treatment effects. Of the confounders analyzed, only sex and age differed significantly across groups, with patients receiving antiplatelet agents more likely to be older and male; multivariable regression accounting for these factors did not change conclusions.
In conclusion, our study suggests that combined antiplatelet and anticoagulant therapy, compared with antiplatelet or anticoagulant therapy alone, decreases the rate of and increases the time to thrombosis recurrence in patients with APS presenting with arterial thrombosis. Randomized controlled trials comparing these regimens will be necessary to confirm our findings.
Acknowledgments
The authors thank the APS ACTION investigators who recruit patients for the APS ACTION registry and Stephen M. Pastores for his insightful input in the revision of the manuscript.
Appendix: study group members
The members of the Antiphospholipid Syndrome Alliance for Clinical Trials and International Networking (APS ACTION) are: Australia: Sydney (Bill Giannakopoulos, Steve Krilis); Brazil: Rio de Janeiro (Guilherme de Jesus, Roger Levy), São Paulo (Renata Rosa, Danieli Andrade); Canada: Quebec (Paul F. Fortin); China: Beijing (Zhouli Zhang); France: Nancy (Stephane Zuily, Denis Wahl); Greece: Athens (Maria Tektonidou); Italy: Brescia (Cecilia Nalli, Laura Andreoli, Angela Tincani), Milan (Cecilia B. Chighizola, Maria Gerosa, Pierluigi Meroni), Padova (Alessandro Banzato, Vittorio Pengo) Turin (Savino Sciascia); Jamaica: Kingston (Karel De Ceulaer, Stacy Davis); Japan: Sapporo (Tatsuya Atsumi); Lebanon: Beirut (Imad Uthman); Netherlands: Utrecht (Ronald Derksen, Philip deGroot); Spain: Barakaldo (Amaia Ugarte, Guillermo Ruiz Irastorza), Barcelona (Ignasi Rodriguez-Pinto, Guillermo Pons-Estel, Ricard Cervera), Madrid (Esther Rodriguez) Cordoba (Maria Angeles Aguirre Zamorano, Rosario Lopez-Pedrera); United Kingdom: London (Ian Mackie, Maria Efthymiou, Hannah Cohen; Maria Laura Bertolaccini, Maria Cuadrado, Munther Khamashta, Giovanni Sanna); United States: Baltimore, MD (Michelle Petri), Chapel Hill, NC (Robert Roubey), Chicago, IL (Jason S. Knight), Durham, NC (Tom Ortel), Galveston, TX (Emilio Gonzalez, Rohan Willis), New York, NY (Steven Levine, Jacob Rand, H. Michael Belmont; Medha Barbhaiya, Doruk Erkan, Jane Salmon, Michael Lockshin), Salt Lake City, UT (Ware Branch).
Footnotes
Presented orally at the 58th annual meeting of the American Society of Hematology, San Diego, CA, 3 December 2016.
Authorship
Contribution: W.G.J. analyzed the data and drafted and wrote the manuscript; C.O. performed statistical analysis and contributed to the writing and review of the manuscript; O.U. partially collected and organized APS ACTION data and reviewed the manuscript; D.E. oversees the APS ACTION registry and contributed to the writing and review of the manuscript; and M.T.D. collected the data for the NYPH cohort, designed the study, analyzed the data, wrote the manuscript, and edited the revised manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
A complete list of the members of the Antiphospholipid Syndrome Alliance for Clinical Trials and International Networking (APS ACTION) appears in “Appendix.”
Correspondence: Maria T. DeSancho, Weill Cornell Medicine, Division of Hematology-Oncology, Department of Medicine, 1305 York Ave, 7th Floor, New York, NY 10021; e-mail: mtd2002@med.cornell.edu.
References
- 1.Gómez-Puerta JA, Cervera R. Diagnosis and classification of the antiphospholipid syndrome. J Autoimmun. 2014;48-49:20-25. [DOI] [PubMed] [Google Scholar]
- 2.Meroni PL, Borghi MO, Raschi E, Tedesco F. Pathogenesis of antiphospholipid syndrome: understanding the antibodies. Nat Rev Rheumatol. 2011;7(6):330-339. [DOI] [PubMed] [Google Scholar]
- 3.Baker WF Jr, Bick RL, Fareed J. Controversies and unresolved issues in antiphospholipid syndrome pathogenesis and management. Hematol Oncol Clin North Am. 2008;22(1):155-174, viii. [DOI] [PubMed] [Google Scholar]
- 4.Ruiz-Irastorza G, Cuadrado MJ, Ruiz-Arruza I, et al. . Evidence-based recommendations for the prevention and long-term management of thrombosis in antiphospholipid antibody-positive patients: report of a task force at the 13th International Congress on antiphospholipid antibodies. Lupus. 2011;20(2):206-218. [DOI] [PubMed] [Google Scholar]
- 5.Lim W, Crowther MA, Eikelboom JW. Management of antiphospholipid antibody syndrome: a systematic review. JAMA. 2006;295(9):1050-1057. [DOI] [PubMed] [Google Scholar]
- 6.Crowther MA, Ginsberg JS, Julian J, et al. . A comparison of two intensities of warfarin for the prevention of recurrent thrombosis in patients with the antiphospholipid antibody syndrome. N Engl J Med. 2003;349(12):1133-1138. [DOI] [PubMed] [Google Scholar]
- 7.Ruiz-Irastorza G, Hunt BJ, Khamashta MA. A systematic review of secondary thromboprophylaxis in patients with antiphospholipid antibodies. Arthritis Rheum. 2007;57(8):1487-1495. [DOI] [PubMed] [Google Scholar]
- 8.Levine SR, Brey RL, Tilley BC, et al. ; APASS Investigators. Antiphospholipid antibodies and subsequent thrombo-occlusive events in patients with ischemic stroke. JAMA. 2004;291(5):576-584. [DOI] [PubMed] [Google Scholar]
- 9.Okuma H, Kitagawa Y, Yasuda T, Tokuoka K, Takagi S. Comparison between single antiplatelet therapy and combination of antiplatelet and anticoagulation therapy for secondary prevention in ischemic stroke patients with antiphospholipid syndrome. Int J Med Sci. 2009;7(1):15-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barbhaiya M, Andrade D, Erkan D; APS ACTION. AntiPhospholipid Syndrome Alliance for Clinical Trials and InternatiOnal Networking (APS ACTION): 5-year update. Curr Rheumatol Rep. 2016;18(10):64. [DOI] [PubMed] [Google Scholar]
- 11.Miyakis S, Lockshin MD, Atsumi T, et al. . International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost. 2006;4(2):295-306. [DOI] [PubMed] [Google Scholar]
- 12.Mohr JP, Thompson JLP, Lazar RM, et al. ; Warfarin-Aspirin Recurrent Stroke Study Group. A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke. N Engl J Med. 2001;345(20):1444-1451. [DOI] [PubMed] [Google Scholar]
- 13.Erkan D, Derksen R, Levy R, et al. . Antiphospholipid Syndrome Clinical Research Task Force report. Lupus. 2011;20(2):219-224. [DOI] [PubMed] [Google Scholar]