Abstract
The importance of telomere length to human health, aging, and cancer continues to be underappreciated. This review examines some basics of telomere biology and relates how telomere function, telomerase activity, and mutations in TERC or TERT are involved in bone marrow failure, leukemias, and other cancers. Given the challenge to obtain accurate data on telomerase activity and telomere length in specific cell types, the situation in acute myeloid leukemia (AML) remains puzzling. In most cancers, telomerase levels are increased after cells have encountered a “telomere crisis,” which is typically associated with poor prognosis. Cells emerging from “telomere crisis” have defective DNA damage responses, resulting, for example, from loss of p53. Such cells often express elevated telomerase levels as a result of point mutations in the TERT promoter or amplification of the TERT gene. While telomeres in AML blasts are typically shorter than expected for normal leukocytes, most AML cells do not show evidence of having gone through a “telomere crisis.” In chronic myeloid leukemia (CML), the difference between the telomere length in nonmalignant T cells and malignant blasts from the same patient was found to correlate with the remaining duration of the chronic phase. This observation supports that a mitotic clock is ticking in CML stem cells and that disease progression in CML heralds the onset of a “telomere crisis.” The presence of very short telomeres in tumor cells was found to predict disease progression in chronic lymphocytic leukemia, myeloma, and various solid tumors. In view of these findings longitudinal studies of telomere length in AML appear worthwhile.
Introduction
Based in part on pioneering Canadian research, it is now firmly established that all blood cells are derived from rare blood-forming, or hematopoietic, stem cells.1-3 Each individual adult produces billions of red blood cells, granulocytes, and platelets daily. This enormous production of cells is driven by the proliferation of progenitor cells, which in turn are derived from hematopoietic stem cells (HSCs). The stem cells can self-renew and produce more stem cells in addition to various lineage-committed progenitors.4 Interestingly, most stem cells are normally not dividing and are only called into action when the committed progenitor cells need to be replaced. It is this “cell division on demand” property of stem cells that is exploited in cancer chemotherapy that primarily targets dividing cells.
The thinking in the 1980s was that if HSCs could be purified and their self-renewal mechanisms figured out, major advances could be made in bone marrow transplantation, gene therapy, and other areas. Investigators, including myself, placed much emphasis on developing reagents, monoclonal antibodies, cell separation techniques, cell culture techniques, and novel assays to understand the stem-cell compartment.
Two observations made in the early 1990s provided some insight into stem cell self-renewal. The first observation compared CD34+ cells from cultures initiated with stem cell candidates from fetal liver, adult bone marrow, and cord blood.5 The CD34+ cells started with fetal liver increased over a thousand-fold, whereas the CD34+ cells started with cord blood increased significantly less. In adult bone marrow, the CD34+ cells never increased >10 times the starting number. Clearly, at the level of stem cells, self-renewal properties are developmentally controlled. HSCs should therefore be considered a moving target: HSCs in the fetus are not the same as HSCs in an adult. The second observation was that telomeres, the repetitive DNA sequences at the ends of chromosomes, got shorter with age and with cell divisions.6 In bone marrow, telomeres were on average shorter than those in cord blood. In cord blood, they were on average shorter than in fetal liver. Therefore, not only are there developmentally related changes in stem cells but there also seems to be a temporal change at the level of DNA: with each cell division telomeres in HSCs apparently get shorter.
Telomere function
Telomeres have very specific TTAGGG repeat sequences along their length that allow association with specific “shelterin” proteins7 (Figure 1). In the absence of telomerase, at least 12 repeats and their associated proteins are required for the telomere to execute its primary function, defined as ensuring that a normal end of a chromosome is not recognized as a double-strand break.8 Telomere repeats are lost with each round of DNA replication,9 and the number of repeats required on 1 or more chromosomes ends in different cell types is a major question in the telomere field. If there are insufficient repeats, an insufficient number of proteins can bind and the telomere will resemble a double-strand break.8 Such an “uncapped” telomere will activate a DNA damage response. The evolutionary solution to the distinction between a normal chromosome end and a double-strand break as well as the “end replication problem”10 is a specialized reverse transcriptase called telomerase (Figure 2). This complex enzyme uses RNA to synthesize DNA rather than the other way around. The minimal components of telomerase are a reverse transcriptase polymerase protein called TERT, an RNA template that encodes the G-rich repeats, and dyskerin, a protein required for proper folding and stability of the telomerase RNA.11 Telomeres always end with a single-stranded 3′ overhang, assumed to be “tucked away” by invading duplex telomeric DNA.12 Conservation of the telomerase RNA template sequence in the telomerase RNA genes explains why exactly the same telomere repeat sequences are found at the ends of chromosomes in highly divergent species.13
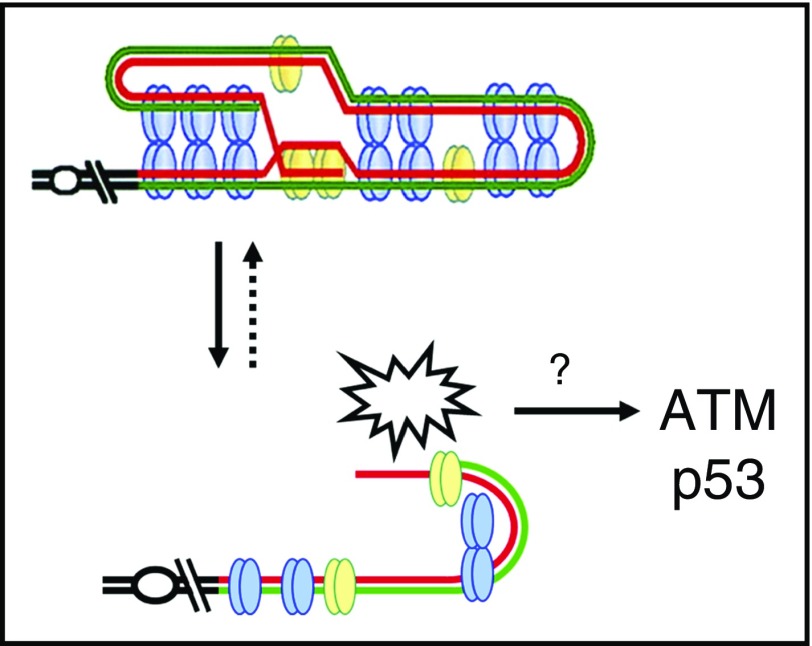
Figure 1.
Telomere repeats and the DNA damage response. Telomeres have very specific sequences of repeats along their length, and at least 12 TTAGGG repeats and their associated proteins are required for the telomere to execute its primary function. If there are insufficient repeats, the telomere looks like a double-strand break. Such an “uncapped” telomere will activate a DNA damage response involving the Ataxia-Telangiectasia mutated (ATM) kinase and p53.
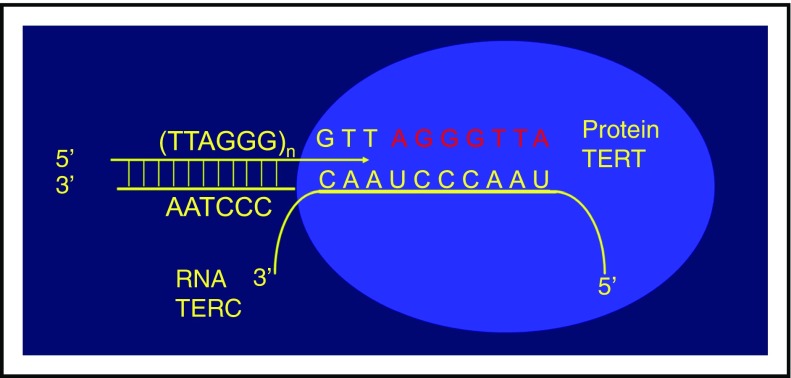
Figure 2.
The telomerase enzyme complex. Telomerase contains a polymerase protein called TERT and an RNA template, TERC, which encodes the G-rich repeats. Chromosomes always end with a single-stranded 3′ DNA overhang believed to invade into telomere duplex DNA if sufficient repeats are available.
How shelterin proteins protect chromosome ends is not entirely clear. Apart from the possibility that the very end of a chromosome is hidden by invasion into duplex telomere repeats,12 it was suggested that interactions between shelterin proteins and telomeric DNA could result in a compact globular structure at telomeres that effectively prevent interactions between chromosome ends and DNA damage response proteins.14 No doubt the questions about the nature of “end protection” will be answered in the near future.
Measuring telomeres
Several methods have been proposed to measure the length of telomere repeats in cells and chromosomes. All methods have advantages as well as shortcomings.15 Polymerase chain reaction–based assays are popular but inaccurate. The average length of telomeres in specific cell types can be accurately measured using fluorescence in situ hybridization (FISH) and flow cytometry, a technique called Flow FISH.16,17 Key in this method is the use of peptide nucleic acid (PNA) probes that allow quantitative hybridization. Following lysis of red blood cells, leukocytes are mixed with bovine thymocytes for telomere length measurements. Bovine thymocytes have long telomeres and provide an internal control for each measurement. Telomere length in cell populations can be gauged by the number of bound PNA probes, their DNA content, or bound antibodies, and reproducible measurements are obtained.
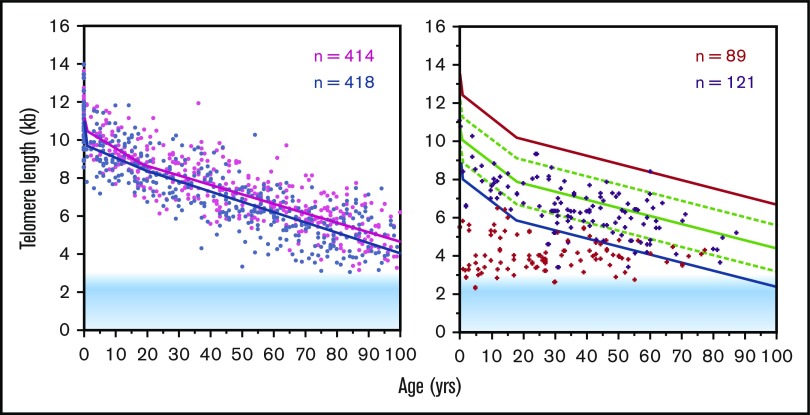
In a normal population, the most dramatic decline in telomere repeats with age is in the first few years of life, for both lymphocytes and granulocytes (Figure 3). At any given age, there is much variation in telomere length; it is not hard to find a 70 year old who has longer telomeres than a teenager. Nevertheless, there is, at the population level, a highly significant decline with age that is more pronounced for lymphocytes than for granulocytes.18 The relative proportion of memory T cells increases with age, and with each T-cell division, as in stem cells, telomeres get shorter. Interestingly, B cells do not show a similar pattern of telomere loss with age as granulocytes and T cells.19,20 For example, some B cells in 90 year olds are longer than one typically sees in newborns. Perhaps telomerase levels in some B cells are upregulated to enable the large number of cell divisions required for clonal selection of cells that secrete antibodies with increased affinity for selected antigens. The flip side of such an evolutionary advantage could be that such B cells are more susceptible to malignant transformation as was previously suggested.21 The finding that B-cell tumors are much more common than T-cell tumors supports this possibility.
Figure 3.
Telomere length declines with age in human lymphocytes measured using flow FISH. The left panel shows that the average difference in telomere length between females (pink) and males (blue) persist throughout life. The right panel shows the telomere length in individuals with “telomeropathies,” in this case, heterozygous carriers of a mutation in either the TERC or the TERT gene (red) and their unaffected siblings (purple). Figure adapted from data shown in Aubert et al.18
The initial decline in telomere length is intriguing. A longitudinal study in baboons showed that just like in humans, the absolute, average telomere length at a given age can vary considerably.22 In the first 100 weeks, there is a dramatic decline in telomere length in newborn baboons, which is most pronounced in T cells, which are presumably actively dividing to set up the T-cell repertoire of the immune system. The telomere length in granulocytes, which is used as a surrogate for the telomere length in stem cells, also shows a rapid decline.21 Interestingly, the absolute decline in telomere length in animals with longer telomeres is more pronounced than in animals with shorter telomeres. Telomere shortening slows down dramatically at ∼1 year of age in baboons. In humans, a similar drop in telomere attrition rate is seen ∼2 to 4 years of age.18 Most likely, these observations point to a drop in the stem cell turnover rate, perhaps reflecting the developmental switch that was inferred from the limited expansion of adult vs cord blood and fetal stem cells.5 Interestingly, at birth there are already differences in leukocyte telomere length between male and female leukocytes, which are maintained throughout life (Figure 3 left panel).18 It has been reported that female embryos grow more slowly,23 and it is tempting to speculate that, on average, males have at birth already consumed more of a finite replicative lifespan than females.
Telomerase in human biology
The crucial role of telomerase in normal human biology was first underscored by studies of patients with dyskeratosis congenita.24 Subsequently, it was found that haploinsufficiency for TERT also can give rise to bone marrow failure.25 Many studies since have confirmed that patients with telomeropathies, defined as diseases caused by genetic defects in telomere length regulation, typically have very short telomeres.26 The dramatic effect of haploinsufficiency for TERT or TERC on telomere length is shown in Figure 3 (right panel).18 Apparently, a modest twofold reduction in telomerase levels can give rise to very short telomeres and dyskeratosis congenita and primary bone marrow failure. With the exception of some dominant negative mutations, lethal genetic disorders are rarely caused by haploinsufficiency for any given gene. Mutations in TERC or TERT are spread out over these genes, implicating loss of function as the disease mechanism. That 2 genes implicated in the same pathway cannot tolerate loss of 1 allele and can both give rise to fatal disease highlights the enormous importance of telomeres and telomerase levels in normal human biology. One possibility is that normal telomerase levels are required to repair critically short telomeres and that this repair capacity is limiting. This scenario is illustrated in the cartoon shown in Figure 4.
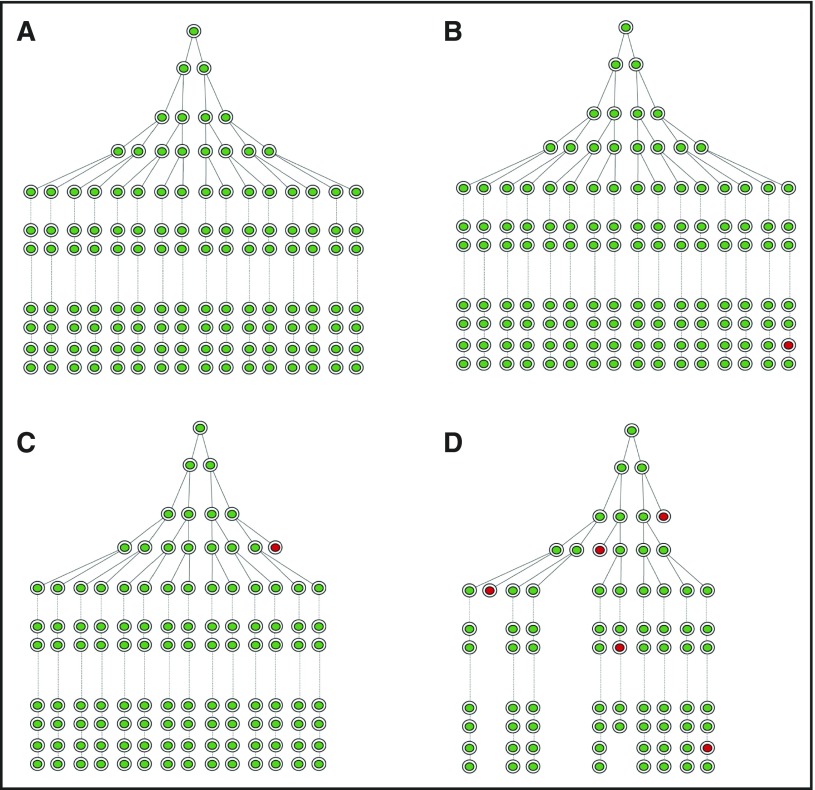
Figure 4.
Normal telomerase levels are needed to maintain telomeres and prevent bone marrow failure. Each stem cell division results in loss of telomere repeats explaining why the average telomere length in various cell types including granulocytes and lymphocytes declines with age (Figure 3). (A) Illustrative representation of the hematopoietic stem cell hierarchy. (B-C) In normal individuals, an occasional stem cell drops out of the stem cell pool (B, red circle) when too many short telomeres relative to the limited repair capacity provided by telomerase accumulate. In patients with reduced telomerase levels, for example, as a result of mutations in telomerase genes, stem cells start dropping out during development (C), putting a strain on remaining stem cells, which have to undergo more divisions to make up the pool (hence, shorter telomeres) as illustrated in panel D. The net result of this negative feed-forward loop is (1) very short telomeres in patients with telomerase deficiency and (2) eventual loss of stem cells resulting in bone marrow failure.
Telomeres and telomerase in leukemias
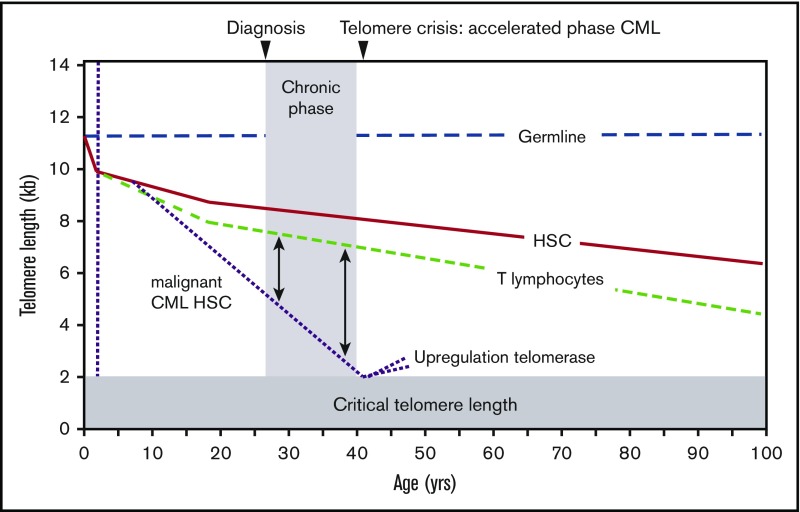
Telomere loss is believed to limit the growth of many somatic stem cells and thereby act as a tumor suppressor mechanism.27 Perhaps occasional short telomeres can be extended by the low telomerase levels in normal stem cells, but when the number of critically short telomeres exceeds repair pathways, DNA damage responses will be activated and cells will either die or become senescent. This provides strong selective pressure for cells that do not respond to DNA damage signals (loss of p53!)28 or cells that have upregulated telomerase levels, for example, as a result of point mutations in the telomerase promoter.29 Defective telomeres in cells with defective DNA damage responses will result in end-to-end fusions and aneuploidy and, eventually, selection of cells with improved telomere maintenance, for example, by higher telomerase levels resulting from further mutations such as amplification of the hTERT gene.30 In patients with chronic myeloid leukemia (CML), there is a difference in telomere length between normal T cells and malignant cells.31 Patients in the accelerated phase or blast phase of the disease showed significantly shorter average telomere length compared with patients in chronic phase. Patients in chronic phase who went into blast phase within 2 years furthermore had significantly shorter telomeres relative to their T lymphocytes than those who did not develop blast phase for at least 2 years. These data suggest that telomere shortening can serve as a surrogate marker of disease progression for patients in chronic phase CML. The data in CML are compatible with the diagram shown in Figure 5. The telomere fusion threshold is also applicable to other cancer types. In patients with chronic lymphoblastic leukemia,32 multiple myeloma,33 and breast cancer,34 the presence of very short, fusogenic telomeres is correlated with “telomere crisis,” poor prognosis, and rapid disease progression.
Figure 5.
Telomere length in CML. The difference in telomere length between CML blast cells relative to T lymphocytes in the same patient correlates with disease progression. See also Figure 3. Most likely cells with defective DNA damage responses are selected when telomeres get critically short, allowing for rapid selection of more malignant, chromosomally unstable cells with additional genetic abnormalities, such as mutations in TERT promoter, amplification of the TERT gene, etc. Figure adapted from Brümmendorf et al.31
Telomere length and maintenance in AML
The situation in acute myeloid leukemia (AML) is less clear. A study of 167 children with AML found that telomere length in leukemic cells was very short compared with healthy control peripheral blood mononuclear cells.35 Patient age at diagnosis was not associated with telomere length. However, cells with an FLT3/internal tandem duplication or a WT1 mutation and FLT3/internal tandem duplication had significantly shorter telomeres than did CEBPA double mutants (P = .0064 and P = .051, respectively) and NPM1 mutants (P = .0012 and P = .0176, respectively). Although telomeres in AML blasts are typically shorter than expected for normal leukocytes, in most cases AML cells do not show evidence of having gone through a “telomere crisis.” Whether this reflects upregulation of telomerase activity in AML stem cells36,37 prior to such a “telomere crisis” or the extensive replicative potential of normal blood-forming stem cells is currently not clear. An important caveat for telomere length measurements in AML is that leukemic cells tend to be heterogeneous with regards to DNA content. Measurement calculations based on diploid genomes in G0 or G1 of the cell cycle could result in erroneous results in AML. Some studies have shown that short telomeres appear to predict the risk of AML development38,39 and is possible that in some cases AML stem cells upregulate telomerase activity by specific mutations in telomerase genes and thereby prevent telomere crisis all together39 (reviewed in Savage and Dufour40). The role of telomere shortening, and, for example, the development of treatment-associated myelodysplastic syndrome and AML after autologous stem cell transplantation,41 is another topic of interest. Telomerase levels could be upregulated in AML cells following abnormalities in the Wnt/b-catenin pathway.42 Before or after telomere crisis, telomerase levels can be elevated by mutations in the promoter hTERT,29 amplification of the hTERT gene, and overexpression of genes that increase telomerase activity, such as c-Myc, HIF-1-α,43 sex hormones, and potentially many others. Upregulation of telomerase levels may prevent telomere loss, or telomeres could be extended. Both possibilities will result in an extension of the proliferative potential of the AML cells. The latter may also occur because of abnormal compaction of telomeres, for example, by increased levels of TRF1 that could occur via various pathways, including defects in proteasome function.44 Therefore, there are many different ways that cells can bypass or postpone a telomere crisis. In view of these possibilities and the observations in CML (Figure 5), longitudinal studies of telomere length in AML appear worthwhile. Unfortunately, convenient and cheap polymerase chain reaction–based studies are too inaccurate to be suitable for such studies.15 Depending on the research question, either the flow FISH or the single telomere length analysis method8,45 is the more useful tool to address questions about telomere dynamics in AML.
Authorship
Contribution: P.M.L. wrote the paper.
Conflict-of-interest disclosure: P.M.L. is a founding shareholder of Repeat Diagnostics, a biotech company providing clinical telomere length measurements.
Correspondence: Peter M. Lansdorp, Terry Fox Laboratory, 675 West 10th Ave, Vancouver, BC V5Z1L3, Canada; e-mail: plansdor@bccrc.ca.
References
- 1.Metcalf D. Blood Lines. Durham, NC: AlphaMed Press; 2005. [Google Scholar]
- 2.Siminovitch L, McCulloch EA, Till JE. The distribution of colony-forming cells among spleen colonies. J Cell Comp Physiol. 1963;62:327-336. [DOI] [PubMed] [Google Scholar]
- 3.Till JE, McCulloch EA, Siminovitch L. A stochastic model of stem cell proliferation, based on the growth of spleen colony-forming cells. Proc Natl Acad Sci USA. 1964;51:29-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pang WW, Schrier SL, Weissman IL. Age-associated changes in human hematopoietic stem cells. Semin Hematol. 2017;54(1):39-42. [DOI] [PubMed] [Google Scholar]
- 5.Lansdorp PM, Dragowska W, Mayani H. Ontogeny-related changes in proliferative potential of human hematopoietic cells. J Exp Med. 1993;178(3):787-791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vaziri H, Dragowska W, Allsopp RC, Thomas TE, Harley CB, Lansdorp PM. Evidence for a mitotic clock in human hematopoietic stem cells: loss of telomeric DNA with age. Proc Natl Acad Sci USA. 1994;91(21):9857-9860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Lange T. Shelterin: the protein complex that shapes and safeguards human telomeres. Genes Dev. 2005;19(18):2100-2110. [DOI] [PubMed] [Google Scholar]
- 8.Capper R, Britt-Compton B, Tankimanova M, et al. . The nature of telomere fusion and a definition of the critical telomere length in human cells. Genes Dev. 2007;21(19):2495-2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Verdun RE, Karlseder J. Replication and protection of telomeres. Nature. 2007;447(7147):924-931. [DOI] [PubMed] [Google Scholar]
- 10.Lingner J, Cooper JP, Cech TR. Telomerase and DNA end replication: no longer a lagging strand problem? Science. 1995;269(5230):1533-1534. [DOI] [PubMed] [Google Scholar]
- 11.Cohen SB, Graham ME, Lovrecz GO, Bache N, Robinson PJ, Reddel RR. Protein composition of catalytically active human telomerase from immortal cells. Science. 2007;315(5820):1850-1853. [DOI] [PubMed] [Google Scholar]
- 12.de Lange T. How telomeres solve the end-protection problem. Science. 2009;326(5955):948-952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang Y, Yesselman JD, Zhang Q, Kang M, Feigon J. Structural conservation in the template/pseudoknot domain of vertebrate telomerase RNA from teleost fish to human. Proc Natl Acad Sci USA. 2016;113(35):E5125-E5134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bandaria JN, Qin P, Berk V, Chu S, Yildiz A. Shelterin protects chromosome ends by compacting telomeric chromatin. Cell. 2016;164(4):735-746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aubert G, Hills M, Lansdorp PM. Telomere length measurement-caveats and a critical assessment of the available technologies and tools. Mutat Res. 2012;730(1-2):59-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baerlocher GM, Lansdorp PM. Telomere length measurements using fluorescence in situ hybridization and flow cytometry. Methods Cell Biol. 2004;75:719-750. [DOI] [PubMed] [Google Scholar]
- 17.Baerlocher GM, Vulto I, de Jong G, Lansdorp PM. Flow cytometry and FISH to measure the average length of telomeres (flow FISH). Nat Protoc. 2006;1(5):2365-2376. [DOI] [PubMed] [Google Scholar]
- 18.Aubert G, Baerlocher GM, Vulto I, Poon SS, Lansdorp PM. Collapse of telomere homeostasis in hematopoietic cells caused by heterozygous mutations in telomerase genes. PLoS Genet. 2012;8(5):e1002696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martens UM, Brass V, Sedlacek L, et al. . Telomere maintenance in human B lymphocytes. Br J Haematol. 2002;119(3):810-818. [DOI] [PubMed] [Google Scholar]
- 20.Weng NP, Granger L, Hodes RJ. Telomere lengthening and telomerase activation during human B cell differentiation. Proc Natl Acad Sci USA. 1997;94(20):10827-10832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lansdorp PM. Telomeres, stem cells, and hematology. Blood. 2008;111(4):1759-1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baerlocher GM, Rice K, Vulto I, Lansdorp PM. Longitudinal data on telomere length in leukocytes from newborn baboons support a marked drop in stem cell turnover around 1 year of age. Aging Cell. 2007;6(1):121-123. [DOI] [PubMed] [Google Scholar]
- 23.Mittwoch U. Blastocysts prepare for the race to be male. Hum Reprod. 1993;8(10):1550-1555. [DOI] [PubMed] [Google Scholar]
- 24.Dokal I, Vulliamy T. Dyskeratosis congenita: its link to telomerase and aplastic anaemia. Blood Rev. 2003;17(4):217-225. [DOI] [PubMed] [Google Scholar]
- 25.Yamaguchi H, Calado RT, Ly H, et al. . Mutations in TERT, the gene for telomerase reverse transcriptase, in aplastic anemia. N Engl J Med. 2005;352(14):1413-1424. [DOI] [PubMed] [Google Scholar]
- 26.Townsley DM, Dumitriu B, Young NS. Bone marrow failure and the telomeropathies. Blood. 2014;124(18):2775-2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aubert G, Lansdorp PM. Telomeres and aging. Physiol Rev. 2008;88(2):557-579. [DOI] [PubMed] [Google Scholar]
- 28.Brassat U, Balabanov S, Bali D, et al. . Functional p53 is required for effective execution of telomerase inhibition in BCR-ABL-positive CML cells. Exp Hematol. 2011;39(1):66-76.e61-62. [DOI] [PubMed] [Google Scholar]
- 29.Chiba K, Lorbeer FK, Shain AH, et al. . Mutations in the promoter of the telomerase gene TERT contribute to tumorigenesis by a two-step mechanism. Science. 2017;357(6358):1416-1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weir BA, Woo MS, Getz G, et al. . Characterizing the cancer genome in lung adenocarcinoma. Nature. 2007;450(7171):893-898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brümmendorf TH, Holyoake TL, Rufer N, et al. . Prognostic implications of differences in telomere length between normal and malignant cells from patients with chronic myeloid leukemia measured by flow cytometry. Blood. 2000;95(6):1883-1890. [PubMed] [Google Scholar]
- 32.Lin TT, Norris K, Heppel NH, et al. . Telomere dysfunction accurately predicts clinical outcome in chronic lymphocytic leukaemia, even in patients with early stage disease. Br J Haematol. 2014;167(2):214-223. [DOI] [PubMed] [Google Scholar]
- 33.Hyatt S, Jones RE, Heppel NH, et al. . Telomere length is a critical determinant for survival in multiple myeloma. Br J Haematol. 2017;178(1):94-98. [DOI] [PubMed] [Google Scholar]
- 34.Simpson K, Jones RE, Grimstead JW, Hills R, Pepper C, Baird DM. Telomere fusion threshold identifies a poor prognostic subset of breast cancer patients. Mol Oncol. 2015;9(6):1186-1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Aalbers AM, Calado RT, Young NS, et al. . Telomere length and telomerase complex mutations in pediatric acute myeloid leukemia. Leukemia. 2013;27(8):1786-1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Röth A, Vercauteren S, Sutherland HJ, Lansdorp PM. Telomerase is limiting the growth of acute myeloid leukemia cells. Leukemia. 2003;17(12):2410-2417. [DOI] [PubMed] [Google Scholar]
- 37.Hartmann U, Brümmendorf TH, Balabanov S, Thiede C, Illme T, Schaich M. Telomere length and hTERT expression in patients with acute myeloid leukemia correlates with chromosomal abnormalities. Haematologica. 2005;90(3):307-316. [PubMed] [Google Scholar]
- 38.Gerbing RB, Alonzo TA, Sung L, et al. . Shorter remission telomere length predicts delayed neutrophil recovery after acute myeloid leukemia therapy: a report from the Children’s Oncology Group. J Clin Oncol. 2016;34(31):3766-3772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ventura Ferreira MS, Crysandt M, Ziegler P, et al. . Evidence for a pre-existing telomere deficit in non-clonal hematopoietic stem cells in patients with acute myeloid leukemia. Ann Hematol. 2017;96(9):1457-1461. [DOI] [PubMed] [Google Scholar]
- 40.Savage SA, Dufour C. Classical inherited bone marrow failure syndromes with high risk for myelodysplastic syndrome and acute myelogenous leukemia. Semin Hematol. 2017;54(2):105-114. [DOI] [PubMed] [Google Scholar]
- 41.Chakraborty S, Sun CL, Francisco L, et al. . Accelerated telomere shortening precedes development of therapy-related myelodysplasia or acute myelogenous leukemia after autologous transplantation for lymphoma. J Clin Oncol. 2009;27(5):791-798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hoffmeyer K, Raggioli A, Rudloff S, et al. . Wnt/β-catenin signaling regulates telomerase in stem cells and cancer cells. Science. 2012;336(6088):1549-1554. [DOI] [PubMed] [Google Scholar]
- 43.Coussens M, Davy P, Brown L, et al. . RNAi screen for telomerase reverse transcriptase transcriptional regulators identifies HIF1alpha as critical for telomerase function in murine embryonic stem cells. Proc Natl Acad Sci USA. 2010;107(31):13842-13847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zeng Z, Wang W, Yang Y, et al. . Structural basis of selective ubiquitination of TRF1 by SCFFbx4. Dev Cell. 2010;18(2):214-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Williams J, Heppel NH, Britt-Compton B, et al. . Telomere length is an independent prognostic marker in MDS but not in de novo AML. Br J Haematol. 2017;178(2):240-249. [DOI] [PubMed] [Google Scholar]