Abstract
Background
Malnutrition is associated with many adverse clinical outcomes. The present study aimed to identify the prevalence of malnutrition in hospitalized patients in Korea, evaluate the association between malnutrition and clinical outcomes, and ascertain the risk factors of malnutrition.
Methods
A multicenter cross-sectional study was performed with 300 patients recruited from among the patients admitted in 25 hospitals on January 6, 2014. Nutritional status was assessed by using the Subjective Global Assessment (SGA). Demographic characteristics and underlying diseases were compared according to nutritional status. Logistic regression analysis was performed to identify the risk factors of malnutrition. Clinical outcomes such as rate of admission in intensive care units, length of hospital stay, and survival rate were evaluated.
Results
The prevalence of malnutrition in the hospitalized patients was 22.0%. Old age (≥ 70 years), admission for medical treatment or diagnostic work-up, and underlying pulmonary or oncological disease were associated with malnutrition. Old age and admission for medical treatment or diagnostic work-up were identified to be risk factors of malnutrition in the multivariate analysis. Patients with malnutrition had longer hospital stay (SGA A = 7.63 ± 6.03 days, B = 9.02 ± 9.96 days, and C = 12.18 ± 7.24 days, P = 0.018) and lower 90-day survival rate (SGA A = 97.9%, B = 90.7%, and C = 58.3%, P < 0.001).
Conclusion
Malnutrition was common in hospitalized patients, and resulted in longer hospitalization and associated lower survival rate. The rate of malnutrition tended to be higher when the patient was older than 70 years old or hospitalized for medical treatment or diagnostic work-up compared to elective surgery.
Keywords: Malnutrition, Nutrition Assessment, Hospitalization, Prevalence, Subjective Global Assessment
Graphical Abstract
INTRODUCTION
Malnutrition is associated with many adverse clinical outcomes, including longer length of stay, increased morbidity and mortality, and increased hospital costs.1,2,3,4,5 Although measurement of malnutrition varied depending on the hospital setting and method of nutritional assessment, its prevalence in hospitals was reported to range from 20% to 50%.1,4,5,6,7,8 Therefore, the recognition of malnutrition and early nutritional therapy in hospitalized patients is important along with the treatment of underlying diseases. However, although malnutrition among hospitalized patients is not rare, it is occasionally overlooked1,4,8,9 either because medical resources, such as the availability of nutritional specialists or hospital systematic and financial support, are insufficient, or because clinicians do not consider malnutrition to be a vital issue.
The nationwide prevalence of malnutrition in hospitalized patients is not well studied in Korea, and nutritional therapy planning for patients with malnutrition is difficult without information regarding the present situation. This nationwide multicenter cross-sectional study was conducted to determine the prevalence of malnutrition and associated clinical factors, and to evaluate the association with clinical outcomes in Korea.
METHODS
Participants
Clinical research groups of the Korean Society for Parenteral and Enteral Nutrition (KSPEN) recruited a total of 25 hospitals (19 tertiary hospitals and 6 secondary hospitals). The size of the participating hospitals ranged from 400 to 2,700 beds. All hospitals had their own nutritional support team. The study participants were recruited from among the patients hospitalized on January 6, 2014, regardless of the departments of admission. The exclusion criteria were as follows: patients who were pregnant, aged < 18 years, and planned to be discharged within 72 hours. The number of recruiting participants from each hospital was determined by considering the average number of admitting patients for 1 day. Based on the sample size calculation, we planned to enroll 337 patients. The included participants were investigated for the following characteristics: age, sex, height, weight, department of admission, major diagnosis at the time of admission, and underlying diseases. All the participating hospitals acquired approval from the Institutional Review Board, and informed consent was obtained from all the patients.
Nutritional status and clinical outcome assessment
The nutritional support team of each hospital investigated the demographic characteristics and evaluated the nutritional status of the study subjects using the Subjective Global Assessment (SGA) on the day of admission and categorized them into SGA A, B, or C (Appendix 1).10,11 The worst two groups in terms of nutrition, SGA B and C, were defined as patients with malnutrition. Subsequently, clinical outcomes, such as length of stay, intensive care unit admission rate, survival rate, and type of discharge were evaluated after 90 days.
Statistical analysis
In the preliminary study conducted with 99 patients from six hospitals in Korea 2013,12 the malnutrition rate in the hospitalized patients was 20.2% (20/99). By using this rate, we initially calculated the sample size to be 218 patients, with an α of 0.05 and a statistical power of 0.8. The refusal rate of the enrolled study subjects from our preliminary study was 0%–35%; therefore, we applied the highest rate in a conservative manner. Thus, the total number of participants was calculated to be 335 (218 × ).
In addition, we classified the 25 participating hospitals into five groups according to rank for the number of admitting patients a day (range: 20–350). The hospitals in the same group were allocated with the same number of study subjects. We allotted the required number of study participants to each group in proportion to the average number of admitted patients. As a result, each hospital in the five groups was allotted 6, 11, 12, 15, and 25 patients, respectively. Finally, the total number of participants was determined to be 337.
Categorical variables were compared by using the χ2 or Fisher exact test; and continuous variables, by using the Student t-test or one-way analysis of variance (ANOVA). To determine the risk factors of malnutrition in hospitalized patients, we used logistic regression models in the univariate and multivariate analyses with the backward method. A two-sided significance level of 0.05 was used for all statistical analyses. Statistical analyses were performed by using the Statistical Package for Social Sciences version 22.0 software (SPSS Inc., Chicago, IL, USA).
Ethics statement
The Institutional Review Board of Asan Medical Center approved this study (approval number: 2013-1120) and informed consent was obtained from all patients.
RESULTS
Among the 337 planned participants, 300 (79.0%) were finally recruited. No significant differences in enrollment rate were found between the five groups of hospitals (P = 0.701). The most common reason for admission was medical treatment (50.7%), followed by elective surgery (38.7%) and diagnostic work-up (10.6%).
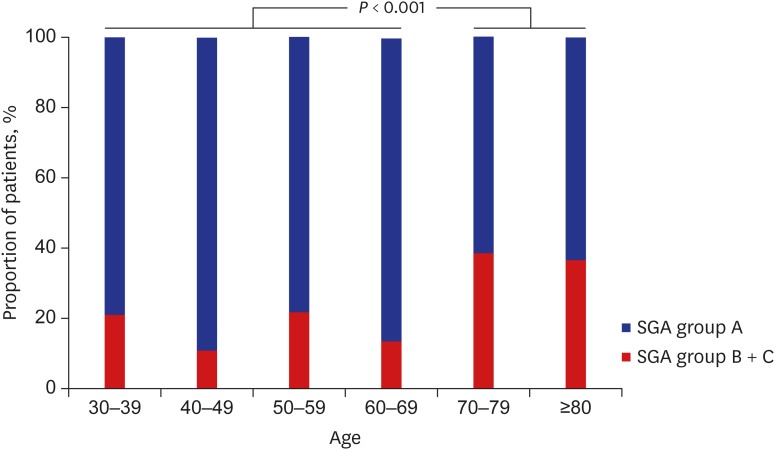
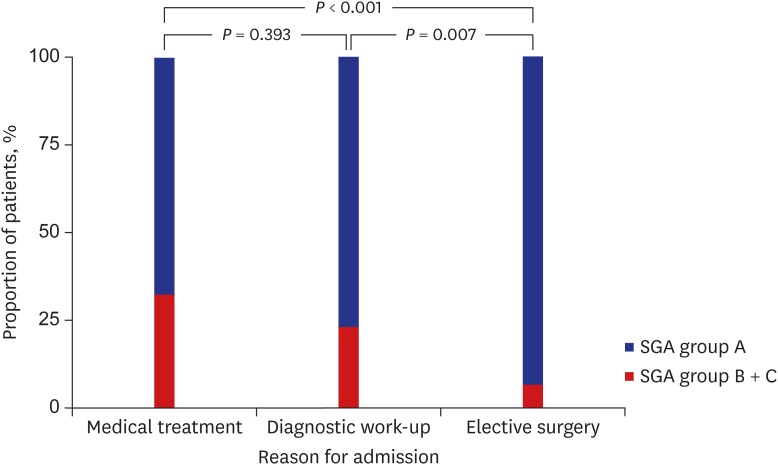
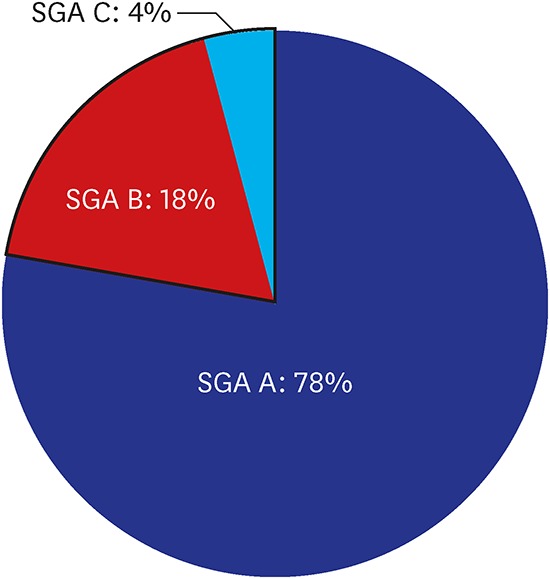
The malnutrition rate in the hospitalized patients was found to be 22.0% (66/300). Among the patients with malnutrition (SGA B + C), 81.8% (n = 54) had moderate malnutrition (SGA B) and 18.2% (n = 12) had severe malnutrition (SGA C). The malnutrition rate was not different according to the size (number of admitting patients a day, divided into five groups) or the referral level (secondary or tertiary) of the participating hospital (P = 0.851 and P = 0.769). A difference in malnutrition rate was found between the different age groups, and the elderly (aged ≥ 70 years) had a significantly higher malnutrition rate than the younger age group (38.2% vs. 17.2%, P < 0.001; Fig. 1). A significant difference in malnutrition rate was observed among the reasons for admission. The malnutrition rate was highest in the patients admitted for medical treatment (32.5%), followed by those admitted for diagnostic work-up (23.3%) and elective surgery (7.0%; Fig. 2).
Fig. 1.
Patients aged ≥ 70 years exhibited higher malnutrition rates than the younger patients.
SGA = Subjective Global Assessment.
Fig. 2.
Malnutrition rates according to the reason for admission.
SGA = Subjective Global Assessment.
The demographic characteristics of the enrolled patients according to nutritional status are presented in Table 1. The patients with malnutrition had significantly lower body mass index (24.2 ± 3.3 kg/m2 vs. 21.9 ± 3.9 kg/m2, P < 0.001), and more patients were admitted for medical treatment in the malnourished group (41.6% vs. 69.7%, P < 0.001). In terms of underlying disease, more patients had underlying pulmonary and oncological diseases in the malnourished group, with a statistically significant difference (4.3% vs. 12.1%, P = 0.034; 15.0% vs. 25.8%, P = 0.041). The prevalence rates of renal, gastrointestinal, and psychological diseases were also elevated in this group (6.8% vs. 13.6%, 5.6% vs. 12.1%, and 1.7% vs. 6.1%), but these were not statistically significant (Table 1).
Table 1. Demographic characteristics of the hospitalized patients (n = 300) according to SGA rank.
| Items of demography or clinical condition | SGA A (n = 234) | SGA B (n = 54) and C (n = 12) (n = 66) | P value | |
|---|---|---|---|---|
| Sex (male) | 125 (53.4) | 37 (56.1) | 0.704 | |
| Age, yr | 54.5 ± 15.6 | 59.6 ± 16.9 | 0.024 | |
| BMI, kg/m2 | 24.2 ± 3.3 | 21.9 ± 3.9 | < 0.001 | |
| Admission for medical treatment or diagnostic work-up | 126 (53.8) | 58 (87.9) | < 0.001 | |
| Underlying diseases (yes) | ||||
| Cardiological disease | 20 (8.5) | 6 (9.0) | 0.897 | |
| Vascular disease | 73 (31.1) | 23 (34.8) | 0.574 | |
| Pulmonary disease | 10 (4.3) | 8 (12.1) | 0.034 | |
| Neurological disease | 4 (1.7) | 2 (3.0) | 0.616 | |
| Endocrine disease | 49 (20.9) | 19 (28.8) | 0.179 | |
| Renal disease | 16 (6.8) | 9 (13.6) | 0.078 | |
| Gastrointestinal disease | 13 (5.6) | 8 (12.1) | 0.065 | |
| Oncological disease | 35 (15.0) | 17 (25.8) | 0.041 | |
| Psychological disease | 4 (1.7) | 4 (6.1) | 0.074 | |
| Musculoskeletal disease | 12 (5.1) | 3 (4.5) | > 0.999 | |
| Othersa | 8 (3.4) | 4 (6.1) | 0.306 | |
Data are shown as number (%) or mean ± standard deviation.
SGA = Subjective Global Assessment, BMI = body mass index.
aFor example, benign prostatic hypertrophy and cataract.
In the univariate analysis, malnourishment was the dependent variable, and age ≥ 70 years (odds ratio [OR], 2.97; 95% confidence interval [CI], 1.64–5.39), underlying pulmonary and oncological diseases (OR, 3.09; 95% CI, 1.17–8.18 and OR, 1.97; 95% CI, 1.02–3.81, respectively), and admission for medical treatment or diagnostic work-up (OR, 6.11; 95% CI, 2.79–13.36) were associated with a significantly higher rate of malnutrition (Table 2). Factors that were statistically significant in the univariate analysis (P < 0.100) and sex were included in the multivariate analysis. The patients aged ≥ 70 years were found to have 2.4 times higher risk of malnutrition (95% CI, 1.01–4.56; P = 0.005). The patients admitted for medical treatment or diagnostic work-up had an increased risk of malnutrition (OR, 5.48; 95% CI, 2.47–12.14, P < 0.001; Table 2).
Table 2. Logistic binary regression with malnutrition (SGA B + C) as a dependent variable.
| Variables | Univariate analysisa | Multivariate analysisb | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | |
| Male | 1.113 | 0.642–1.928 | 0.704 | |||
| Age ≥ 70 yr | 2.971 | 1.637–5.393 | < 0.001 | 2.439 | 1.307–4.553 | 0.005 |
| Admission for medical treatment or diagnostic work-up | 6.108 | 2.793–13.360 | < 0.001 | 5.479 | 2.473–12.140 | < 0.001 |
| Pulmonary disease | 3.090 | 1.167–8.179 | 0.023 | |||
| Renal disease | 2.151 | 0.904–5.120 | 0.083 | |||
| Gastrointestinal disease | 2.345 | 0.928–5.925 | 0.072 | |||
| Oncological disease | 1.973 | 1.021–3.810 | 0.043 | |||
| Psychological disease | 3.710 | 0.902–15.250 | 0.069 | |||
SGA = Subjective Global Assessment, OR = odds ratio, CI = confidence interval.
aOnly underlying diseases with a P value of < 0.100 are listed; bAll the listed variables are adjusted in the multivariate analysis.
Malnutrition was closely related to the clinical outcomes (Table 3). As malnutrition worsen, the length of hospital stay was increased and the survival rate decreased, with statistically significant differences across the three SGA groups (7.63 ± 6.03 vs. 9.02 ± 9.96 vs. 12.18 ± 7.24 days, P = 0.018 and 97.9% vs. 90.7% vs. 58.3%, P < 0.001). In the post hoc study, length of hospital stay was significantly different between groups A and C only (P = 0.024 with Bonferroni correction), and survival rate was significantly different among all the groups (SGA A and B, P = 0.030; B and C, P = 0.015; A and C, P < 0.001, with Bonferroni correction).
Table 3. Clinical outcomes of the hospitalized patients according to SGA rank.
| Outcomes | SGA A (n = 234) | SGA B (n = 54) | SGA C (n = 12) | P value |
|---|---|---|---|---|
| ICU admission | 9 (3.8) | 1 (1.9) | 1 (8.3) | 0.531 |
| Length of hospital staya | 7.63 ± 6.03 | 9.02 ± 9.96 | 12.18 ± 7.24 | 0.018 |
| Survival rateb | 229 (97.9) | 49 (90.7) | 7 (58.3) | < 0.001 |
Data are shown as number (%) or mean ± standard deviation.
SGA = Subjective Global Assessment, ICU = intensive care unit, ANOVA = analysis of variance.
aStatistically significant only between SGA A and C by ANOVA with Bonferroni correction (P = 0.024); bSGA A and B, P = 0.030; B and C, P = 0.015; A and C, P < 0.001, using the χ2 test with Bonferroni correction.
DISCUSSION
In this nationwide multicenter cross-sectional study in Korea, 22% of the hospitalized patients had malnutrition at the point of admission according to SGA rank. This rate corresponds with those in other studies that evaluated the hospital malnutrition rate according to SGA rank. An Australian study performed in 2008 by Gout et al.4 reported a 23% malnutrition rate in tertiary hospitals using the SGA rank, and a German study performed by Pirlich et al.7 reported a malnutrition rate of 27.4% in 13 hospitals. Like our study, these studies only evaluated nutritional status at the point of admission. If our study included already hospitalized patients, the malnutrition rate may have been higher. For instance, in the Brazilian National Survey on Hospital Nutritional Assessment survey conducted in Brazil, the malnutrition rate was determined to be 48.1% by using the SGA rank.8 This relatively high rate may have resulted from including both newly admitted and already hospitalized patients.
Age was a major risk factor of malnutrition. Of the patients aged ≥ 70 years, 38.2% had a significantly higher malnutrition rate than the younger patients (17.2% vs. 38.2%, P < 0.001). The aforementioned German study7 also reported a high prevalence of malnutrition in elderly patients (43%). Many physiological, social, and psychological changes ensue as patients get older, which makes the elderly particularly vulnerable to malnutrition.13,14 Considering the high prevalence of malnutrition in this group, routine and periodic nutritional assessment of hospitalized elderly patients is mandatory as an initiating step of appropriate nutritional therapy. The Mini Nutrition Assessment, which is encouraged for use in the elderly, can be applied for a more detailed evaluation.15,16,17
Having specific underlying comorbidities was associated with malnutrition, and this was especially apparent in the patients with pulmonary and oncological diseases in this study. Resting energy expenditure increased to as high as 15%–20% of the expected value among chronic obstructive pulmonary disease patients, which could have resulted from the increased energy of the respiratory muscles.18,19 In addition, inflammation, hypoxia, hypercapnia, and various medications are known to cause malnutrition in patients with pulmonary disease. Weight loss is a common symptom in patients with oncological diseases, due to the tumor itself, the physiological reaction to the tumor, and treatment complications from treatment, all of which can promote malnutrition.20,21,22 Oncological disease was also identified as an independent risk factor of malnutrition in other studies.7,23
The patients admitted for medical treatment or diagnostic work-up exhibited a higher malnutrition rate than those admitted for elective surgery. This may be explained by the fact that the latter group of patients were unlikely to have acute medical diseases at the time of admission. A relatively low malnutrition rate in patients admitted for elective surgical treatment was also observed in other studies.7,8 The analysis was done only for the type of care, not departments such as general surgery or cardiovascular department, because each hospital has a unique structure of departments, even patients with the same condition can be admitted to different departments. In addition, since the purpose of hospitalization differs for each patient even within a single department, it is difficult to correlate the general health condition of a patient with the departments where the patient was hospitalized.
Malnutrition is known to worsen many clinical outcomes.1,2,3,4,5 In the present study, a poor nutritional status was associated with longer length of hospital stay and lower 90-day survival rate. Fortunately, several studies demonstrated that adequate nutritional therapy for patients with malnutrition reduces length of hospital stay, infectious or non-infectious complications, and mortality.24,25,26,27,28 Considering 22% of malnutrition rate and its adverse effect on clinical outcomes, clinician should make effort to identify and manage malnutrition in hospitalized patients. Therefore, all hospitals should implement a nutritional screening program to identify patients with or at risk of malnutrition.29,30 In addition, having a multidisciplinary nutritional support team that can assess high-risk patients and provide appropriate nutritional therapy is important.28 Foremost, clinicians should recognize that malnutrition is not an inevitable result of the aging process or underlying diseases but should be considered as a specific disease entity that requires active management.
The present study has some limitations. First, nutritional status was only evaluated on the day of admission and patients who were already hospitalized were not included in this study; therefore, this study may have underestimated the malnutrition rate of all the hospitalized patients. Second, clinical outcomes according to the nutritional status were not adjusted for the severity of underlying diseases, which may have biased the results. Third, previous admission history within some period was not considered in the analysis of the comparison between SGA A or SGA B or the association with the likelihood of malnutrition (SGA B + C), which could have been an important factor. However, the sample size for each hospital was calculated from the number of admitted patients at each hospital to reduce the selection bias. To the best of our knowledge, this study is the first nationwide prospective study to identify the malnutrition rate of hospital inpatients in Korea, and our findings will help promote the hospital nutritional support programs in Korea.
In conclusion, malnutrition was common in hospitalized patients, and the rate of malnutrition tended to be high when the patient was older than 70 years old or hospitalized for medical treatment or diagnostic work-up. Malnourished patients needed longer hospitalization and showed lower survival rate in the present study.
Appendix 1
SGA questionnaire
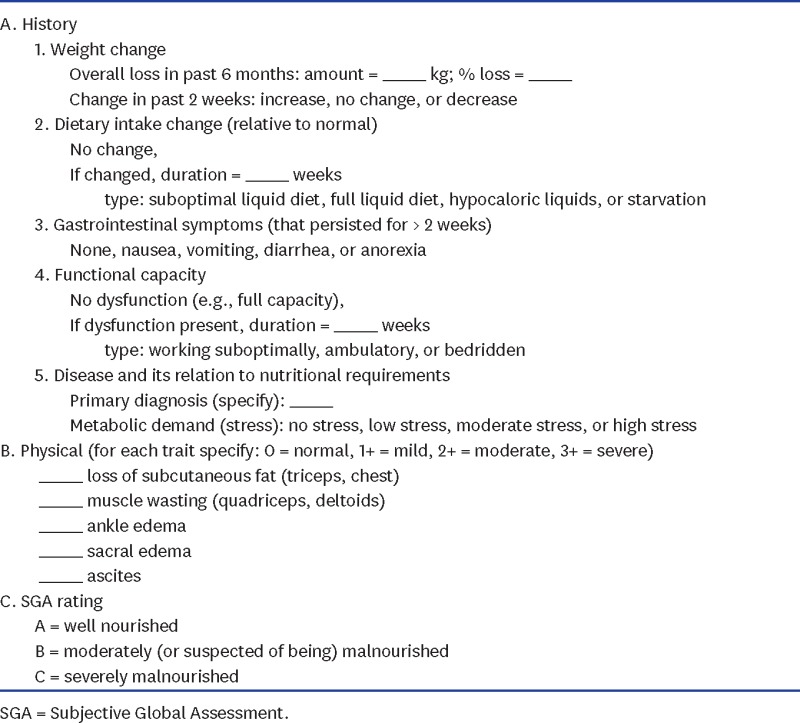
SGA = Subjective Global Assessment.
Footnotes
Funding: This study was funded by the Korean Society for Parenteral and Enteral Nutrition (KSPEN).
Disclosure: The authors have no potential conflicts of interest to disclose.
Author Contributions: Conceptualization: Kang MC, Kim JH, Ryu SW, Moon JY, Park JH, Park JK, Park JH, Baik HW, Seo JM, Son MW, Song GA, Shin DW, Shin YM, Ahn HY, Yang HK, Yu HC, Yun IJ, Lee JG, Lee JM, Lee JH, Lee TH, Yim H, Jeon HJ, Jung K, Jung MR, Jeong CY, Lim HS, Hong SK. Formal analysis: Ahn HY. Writing - original draft: Kang MC, Hong SK. Writing - review & editing: Kang MC, Kim JH, Ryu SW, Moon JY, Park JH, Park JK, Park JH, Baik HW, Seo JM, Son MW, Song GA, Shin DW, Shin YM, Ahn HY, Yang HK, Yu HC, Yun IJ, Lee JG, Lee JM, Lee JH, Lee TH, Yim H, Jeon HJ, Jung K, Jung MR, Jeong CY, Lim HS, Hong SK.
References
- 1.Barker LA, Gout BS, Crowe TC. Hospital malnutrition: prevalence, identification and impact on patients and the healthcare system. Int J Environ Res Public Health. 2011;8(2):514–527. doi: 10.3390/ijerph8020514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu GH, Liu ZH, Wu ZH, Wu ZG. Perioperative artificial nutrition in malnourished gastrointestinal cancer patients. World J Gastroenterol. 2006;12(15):2441–2444. doi: 10.3748/wjg.v12.i15.2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Allard JP, Keller H, Jeejeebhoy KN, Laporte M, Duerksen DR, Gramlich L, et al. Decline in nutritional status is associated with prolonged length of stay in hospitalized patients admitted for 7 days or more: a prospective cohort study. Clin Nutr. 2016;35(1):144–152. doi: 10.1016/j.clnu.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 4.Gout BS, Barker LA, Crowe TC. Malnutrition identification, diagnosis and dietetic referrals: are we doing a good enough job? Nutr Diet. 2009;66(4):206–211. [Google Scholar]
- 5.Norman K, Pichard C, Lochs H, Pirlich M. Prognostic impact of disease-related malnutrition. Clin Nutr. 2008;27(1):5–15. doi: 10.1016/j.clnu.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 6.Correia MI, Campos AC, ELAN Cooperative Study Prevalence of hospital malnutrition in Latin America: the multicenter ELAN study. Nutrition. 2003;19(10):823–825. doi: 10.1016/s0899-9007(03)00168-0. [DOI] [PubMed] [Google Scholar]
- 7.Pirlich M, Schütz T, Norman K, Gastell S, Lübke HJ, Bischoff SC, et al. The German hospital malnutrition study. Clin Nutr. 2006;25(4):563–572. doi: 10.1016/j.clnu.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 8.Waitzberg DL, Caiaffa WT, Correia MI. Hospital malnutrition: the Brazilian national survey (IBRANUTRI): a study of 4000 patients. Nutrition. 2001;17(7-8):573–580. doi: 10.1016/s0899-9007(01)00573-1. [DOI] [PubMed] [Google Scholar]
- 9.Adams NE, Bowie AJ, Simmance N, Murray M, Crowe TC. Recognition by medical and nursing professionals of malnutrition and risk of malnutrition in elderly hospitalised patients. Nutr Diet. 2008;65(2):144–150. [Google Scholar]
- 10.Detsky AS, McLaughlin JR, Baker JP, Johnston N, Whittaker S, Mendelson RA, et al. What is subjective global assessment of nutritional status? JPEN J Parenter Enteral Nutr. 1987;11(1):8–13. doi: 10.1177/014860718701100108. [DOI] [PubMed] [Google Scholar]
- 11.Kim SE. Nutritional screening and assessment in hospitalized patients. Korean J Gastroenterol. 2015;65(6):336–341. doi: 10.4166/kjg.2015.65.6.336. [DOI] [PubMed] [Google Scholar]
- 12.Lee YM, Kim SH, Kim YS, Kim EM, Kim JY, Keum MA, et al. Nutritional status of Korean hospitalized patients: a multi-center preliminary survey. J Clin Nutr. 2014;6(2):71–78. [Google Scholar]
- 13.Hickson M. Malnutrition and ageing. Postgrad Med J. 2006;82(963):2–8. doi: 10.1136/pgmj.2005.037564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vanderwee K, Clays E, Bocquaert I, Gobert M, Folens B, Defloor T. Malnutrition and associated factors in elderly hospital patients: a Belgian cross-sectional, multi-centre study. Clin Nutr. 2010;29(4):469–476. doi: 10.1016/j.clnu.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 15.Kondrup J, Allison SP, Elia M, Vellas B, Plauth M, Educational and Clinical Practice Committee, European Society of Parenteral and Enteral Nutrition (ESPEN) ESPEN guidelines for nutrition screening 2002. Clin Nutr. 2003;22(4):415–421. doi: 10.1016/s0261-5614(03)00098-0. [DOI] [PubMed] [Google Scholar]
- 16.Beck AM, Ovesen L, Osler M. The ‘Mini Nutritional Assessment’ (MNA) and the ‘Determine Your Nutritional Health’ Checklist (NSI Checklist) as predictors of morbidity and mortality in an elderly Danish population. Br J Nutr. 1999;81(1):31–36. [PubMed] [Google Scholar]
- 17.Lee H, Kang JH, Kim E, Kim WG. Prevalence of malnutrition in hospitalized elderly Korean patients based on mini nutritional assessment-short form. J Clin Nutr. 2014;6(1):24–29. [Google Scholar]
- 18.Ezzell L, Jensen GL. Malnutrition in chronic obstructive pulmonary disease. Am J Clin Nutr. 2000;72(6):1415–1416. doi: 10.1093/ajcn/72.6.1415. [DOI] [PubMed] [Google Scholar]
- 19.Engelen MP, Schols AM, Baken WC, Wesseling GJ, Wouters EF. Nutritional depletion in relation to respiratory and peripheral skeletal muscle function in out-patients with COPD. Eur Respir J. 1994;7(10):1793–1797. doi: 10.1183/09031936.94.07101793. [DOI] [PubMed] [Google Scholar]
- 20.Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F, et al. ESPEN guidelines on nutrition in cancer patients. Clin Nutr. 2017;36(1):11–48. doi: 10.1016/j.clnu.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 21.Argilés JM. Cancer-associated malnutrition. Eur J Oncol Nurs. 2005;9(Suppl 2):S39–S50. doi: 10.1016/j.ejon.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 22.Van Cutsem E, Arends J. The causes and consequences of cancer-associated malnutrition. Eur J Oncol Nurs. 2005;9(Suppl 2):S51–S63. doi: 10.1016/j.ejon.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 23.Meijers JM, Schols JM. van Bokhorst-de van der Schueren MA, Dassen T, Janssen MA, Halfens RJ. Malnutrition prevalence in The Netherlands: results of the annual dutch national prevalence measurement of care problems. Br J Nutr. 2009;101(3):417–423. doi: 10.1017/S0007114508998317. [DOI] [PubMed] [Google Scholar]
- 24.Fukuda Y, Yamamoto K, Hirao M, Nishikawa K, Maeda S, Haraguchi N, et al. Prevalence of malnutrition among gastric cancer patients undergoing gastrectomy and optimal preoperative nutritional support for preventing surgical site infections. Ann Surg Oncol. 2015;22(Suppl 3):S778–S785. doi: 10.1245/s10434-015-4820-9. [DOI] [PubMed] [Google Scholar]
- 25.O’Flynn J, Peake H, Hickson M, Foster D, Frost G. The prevalence of malnutrition in hospitals can be reduced: results from three consecutive cross-sectional studies. Clin Nutr. 2005;24(6):1078–1088. doi: 10.1016/j.clnu.2005.08.012. [DOI] [PubMed] [Google Scholar]
- 26.Zhong JX, Kang K, Shu XL. Effect of nutritional support on clinical outcomes in perioperative malnourished patients: a meta-analysis. Asia Pac J Clin Nutr. 2015;24(3):367–378. doi: 10.6133/apjcn.2015.24.3.20. [DOI] [PubMed] [Google Scholar]
- 27.Johansen N, Kondrup J, Plum LM, Bak L, Nørregaard P, Bunch E, et al. Effect of nutritional support on clinical outcome in patients at nutritional risk. Clin Nutr. 2004;23(4):539–550. doi: 10.1016/j.clnu.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 28.Tappenden KA, Quatrara B, Parkhurst ML, Malone AM, Fanjiang G, Ziegler TR. Critical role of nutrition in improving quality of care: an interdisciplinary call to action to address adult hospital malnutrition. J Acad Nutr Diet. 2013;113(9):1219–1237. doi: 10.1016/j.jand.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 29.Khalatbari-Soltani S, Marques-Vidal P. Impact of nutritional risk screening in hospitalized patients on management, outcome and costs: a retrospective study. Clin Nutr. 2016;35(6):1340–1346. doi: 10.1016/j.clnu.2016.02.012. [DOI] [PubMed] [Google Scholar]
- 30.Omidvari AH, Vali Y, Murray SM, Wonderling D, Rashidian A. Nutritional screening for improving professional practice for patient outcomes in hospital and primary care settings. Cochrane Database Syst Rev. 2013;(6):CD005539. doi: 10.1002/14651858.CD005539.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]