Abstract
Introduction
The use of self-expandable metal stents (SEMS) for the treatment of postoperative leaks of the upper gastrointestinal tract is already established. However, there are discrepancies between the relatively small caliber of the esophageal stents available and the postsurgical luminal size, which may determine an inadequate juxtaposition. As colonic stents have a bigger diameter, they might be more adequate. Additionally, stents with a larger diameter might have a lower risk of migration.
Materials and Methods
The aim of this study was to evaluate the efficacy and complications associated with the use of colonic fully covered SEMS (FSEMS) in the treatment of postoperative leaks in critical patients. All patients with postoperative leaks of the upper gastrointestinal tract treated with colonic stents (Hanarostent® CCI) between 2010 and 2013 were retrospectively included.
Results
Four patients with postoperative leaks were treated with colonic SEMS. The underlying surgeries were a gastric bypass, an esophagogastrectomy for Boerhaave syndrome, a primary repair of esophagopleural fistula due to Boerhaave syndrome, and an esophagectomy due to esophageal cancer. The leaks were detected on average 17 days after the initial surgery. All patients needed admission to a critical care unit after index surgery. Stent placement was technically feasible in all patients. The median residence time of the stents was 7 weeks, and no complications were verified when they were removed. There were no cases of stent migration. The treatment was successful in all patients, with complete healing of the leaks.
Discussion and Conclusions
The placement of colonic FSEMS seems to be successful and safe in the treatment of postoperative leaks of the upper gastrointestinal tract.
Keywords: Anastomotic leak, Gastrointestinal diseases, Postoperative complications, Self-expandable metallic stents
Resumo
Introdução
A utilização de próteses metálicas auto-expansíveis (SEMS) para o tratamento de fístulas e deiscências cirúrgicas do trato gastrointestinal alto está já estabelecida. No entanto, há discrepâncias entre o calibre relativamente pequeno das próteses esofágicas disponíveis e o diâmetro luminal pós-cirúrgico, o que pode determinar uma justaposição inadequada. Visto que as próteses destinadas ao cólon têm um maior calibre, estas poderão ser mais adequadas nestas situações. Adicionalmente, as próteses com maior diâmetro poderão ter um risco mais baixo de migração.
Materiais e Métodos
O objetivo deste estudo foi avaliar a eficácia e complicações associadas ao uso de SEMS do cólon totalmente cobertas (FSEM) no tratamento das fístulas/deiscências cirúrgicas em doentes críticos. Todos os doentes com fístulas/deiscências cirúrgicas do trato digestivo alto tratados com próteses do cólon (Hanarostent® CCI) entre 2010 e 2013 foram incluídos retrospetivamente.
Resultados
Quatro doentes com as caraterísticas referidas foram tratados com próteses do cólon. As cirurgias subjacentes foram um bypass gástrico, uma esogagogastrectomia para síndroma de Boerhaave, uma rafia de uma fístula esofagopleural secundária a síndrome de Boerhaave e uma esofagectomia para cancro esofágico. As fístulas/deiscências foram detetadas em média 17 dias após a cirurgia inicial. Todos os doentes necessitaram de admissão numa unidade de cuidados intensivos após a cirurgia índice. A colocação da prótese foi tecnicamente bem-sucedida em todos os doentes. O tempo mediano de permanência da prótese foi 7 semanas, não se registando complicações na altura da sua remoção. Não ocorreu migração da prótese em nenhum doente. O tratamento foi eficaz em todos os doentes, com cicatrização completa das fístulas/deiscências.
Discussão e Conclusões
A colocação de FSEMS do colon é uma opção terapêutica segura e eficaz nos doentes com fístulas/deiscências cirúrgicas do trato gastrointestinal superior.
Palavras Chave: Fístula anastomótica, Doenças gastrointestinais, Complicações pós-operatórias, Stents metálicos autoexpansíveis
Introduction
Fistula and anastomotic leaks of the upper gastrointestinal tract may occur as a complication of gastrointestinal surgery, with a rate of 4–8% [1, 2, 3]. They can be a major source of mortality and morbidity despite the continuous progress in diagnostic procedures and surgical interventions [4, 5].
There is no consensus on the ideal method for treating patients with these types of conditions, and the chosen treatment method may vary according to the timing after initial surgery, leakage size, and patient condition. Some patients might need surgical reintervention, which is often associated with poor results, especially after delayed diagnosis of the leakage. In selected patients, a conservative approach with parenteral nutrition, broad-spectrum antibiotics, drainage with intercostal drains, or percutaneous drainage guided radiologically might be successful. However, this approach is only indicated for minimal and asymptomatic anastomotic leaks, as it is associated with a high mortality and morbidity when used to treat clinically significant leaks [4, 5, 6, 7].
In the last decade, with the advances of interventional endoscopy, various minimally invasive procedures have been proposed to obtain a nonsurgical repair of anastomotic leaks, such as fibrin glue injection, placement of endoclips, endoscopic vacuum sponge therapy, and stent insertion [4, 5, 6, 8].
Esophageal stent placement is a well-accepted and effective method for palliation of inoperable esophageal malignancies [9]. Recently, temporary placement of fully (FSEMS) or partially (PSEMS) covered self-expanding metal stents (SEMS) or self-expanding plastic stents (SEPS) has emerged as a treatment option for benign esophageal ruptures and leaks, with a favorable outcome [5, 9]. Their use has been proposed for ruptures or leaks that are smaller than 50–70% of the circumference. The stent provides immediate leak occlusion, allowing healing of the wall lesions while providing enteral nutrition. It should be noted that for a successful endoscopic procedure, a complete drainage of fluid collections in the mediastinum or pleural cavity is fundamental [4, 5, 6, 10, 11]. There are 2 major drawbacks associated with stent placement, namely stent migration, which may occur in 13–46% of the patients [10], and tissue in- or overgrowth. This latter complication has been reported to occur more commonly with PSEMS than with FSEMS or SEPS. On the one hand, the reactive tissue growing into the stent meshes may reduce the risk of stent migration and provide a better watertight barrier to luminal contents, favoring fistula healing. On the other hand, severe tissue embedding may cause difficulties in endoscopic stent removal [4, 7, 10].
Esophageal stents were initially designed for the treatment of stenosis and as such have a small diameter. Therefore, there is a discrepancy between the small diameters of commercially available stents and the larger diameter of the upper GI tract after surgery. This may preclude a desired watertight sealing in this particular group of patients and a higher risk of migration [10, 11]. In the absence of stents specifically designed for altered postoperative anatomy, an option to prevent stent migration may be the utilization of a stent with a larger diameter, as is the case with stents designed for the colon. However, the use of these stents may be also associated with a greater risk of adverse events such as perforation and bleeding.
This report describes our results on efficacy and safety of the use of silicone-covered, self-expanding metallic colonic stents for the treatment of postsurgical leakages.
Materials and Methods
Patients
This is a retrospective review of a series of consecutive critically ill patients who underwent placement of colonic FSEMS for the treatment of postsurgical anastomotic leaks/fistulas at the Centro Hospitalar Tondela-Viseu from 2010 to 2013. All patients were admitted to an intensive or intermediate care unit due to their unstable condition secondary to a complication of the index surgical procedure. None of the patients was considered a surgical candidate at the time of stent placement, and the procedure was considered lifesaving.
The following information was collected from their medical record: baseline demographics; type of surgery; time and method of leak diagnosis; leak characteristics; stent placement and stent removal reports; information on concomitant treatment, and follow-up.
Diagnosis of the Anastomotic Leak
The diagnosis of the anastomotic leak was established based on clinical symptoms (fever, respiratory distress, or hemodynamic shock) combined with upper endoscopy, single-contrast fluoroscopy and/or computed tomography examination.
Placement and Removal of the Stent
The Hanarostent® CCI is a SEMS made of a nitinol net that is fully covered with an inner silicone membrane, with flares at both ends as antimigration features. The central and extreme diameters are 24 and 32 mm, respectively. In our center, we have 2 available lengths: 80 and 150 mm. There are radio-opaque markers at both ends and in the middle for fluoroscopic visualization. These stents are generally indicated for application in the palliative treatment of colorectal stricture and/or closure of perforations and postsurgical leaks and fistula by malignant and benign tumors.
All stents were placed under general anesthesia with endotracheal intubation. The same experienced operator performed all endoscopic procedures. An upper endoscopy was performed, and lipiodol, a radio-opaque marker, was injected proximally and distally to the leak in order to guide stent placement. A guidewire was introduced beyond the leak under endoscopic view, after which the endoscope was removed and the stent was placed under fluoroscopic control. After deployment, the position of the stent was checked by endoscopy. A single-contrast fluoroscopy examination was also obtained after placement and removal of the stent to determine if the leak was completely sealed.
The endoscopic removal of the stent was scheduled 4–8 weeks after its placement in agreement with the surgical team and depending on the clinical evolution of the patient. A rat-tooth forceps or a polypectomy snare was used to grasp the loop at the distal end of the stent during upper endoscopy under general anesthesia with propofol or conscious sedation with midazolam, depending on the patient's condition.
Concomitant Treatment
Concomitant drainage of infected areas in the pleural cavity, mediastinum, or abdomen was performed by the placement of intercostal or intraabdominal drains, as well as the administration of antibiotics. All patients were treated in an intensive or intermediate care unit, with concomitant cardiovascular and respiratory support, as needed.
Definitions
We used the following definitions:
time to leak diagnosis: time between the surgical procedure and the diagnosis of the anastomotic leak;
time of stent placement: time between stent placement and removal;
technical success: technically successful stent placement;
clinical success: complete disappearance of the septic symptoms associated with complete healing of the lesion in the gastrointestinal wall confirmed by endoscopy or single-contrast fluoroscopy;
complications: adverse events related to the stent or the stent placement, such as migration, tissue in- or overgrowth, perforation, or hemorrhage;
stent-related mortality: mortality with an evident relationship to stent-placement or removal; and
re-intervention: need of an endoscopic or surgical procedure due to complications or failure of stent placement.
Statistical Analysis
Categorical variables are presented as frequencies and percentages, and continuous variables as means and standard deviations, or medians and interquartile ranges for variables with skewed distributions.
Results
Patient Characteristics and Leak Diagnosis
We identified 4 patients. The majority were males with a mean age of 62.8 ± 10.7 years (range 51–77). Their baseline characteristics are represented in Table 1. All underlying surgeries were different: 2 of them were performed in an urgent context (esophagogastrectomy and suture of the esophagopleural fistula due to Boerhaave syndrome), and the other 2 were elective. The location of the leak was the gastric pouch staple line in patient 1, the esogastric anastomosis in patients 2 and 3 (20 and 35 cm from incisions, respectively), and in the lower third of the esophagus, approximately 39 cm from the incisions, in patient 4.
Table 1.
Baseline characteristics of the patients and clinical information
| Patient | Gender | Age, years | Comorbidities | Underlying surgery | Time to leak diagnosis, days | Size of leak, mm; %a |
|---|---|---|---|---|---|---|
| 1 | Female | 51 | Obesity | Gastric bypass | 12 | 10 |
| 2 | Male | 77 | Auricular fibrillation, arterial hypertension, cerebrovascular disease | Esophagogastrectomy for Boerhaave syndrome | 33 | 20; 40 |
| 3 | Male | 62 | Arterial hypertension | Esophagectomy with gastric tube formation for esophageal cancer | 14 | 25; 60 |
| 4 | Male | 61 | Epilepsy; auricular fibrillation; chronic liver disease | Suture of esophagopleural fistula secondary to Boerhaave syndrome | 7 | 15 |
The percentages are only given in the cases of anastomotic leaks.
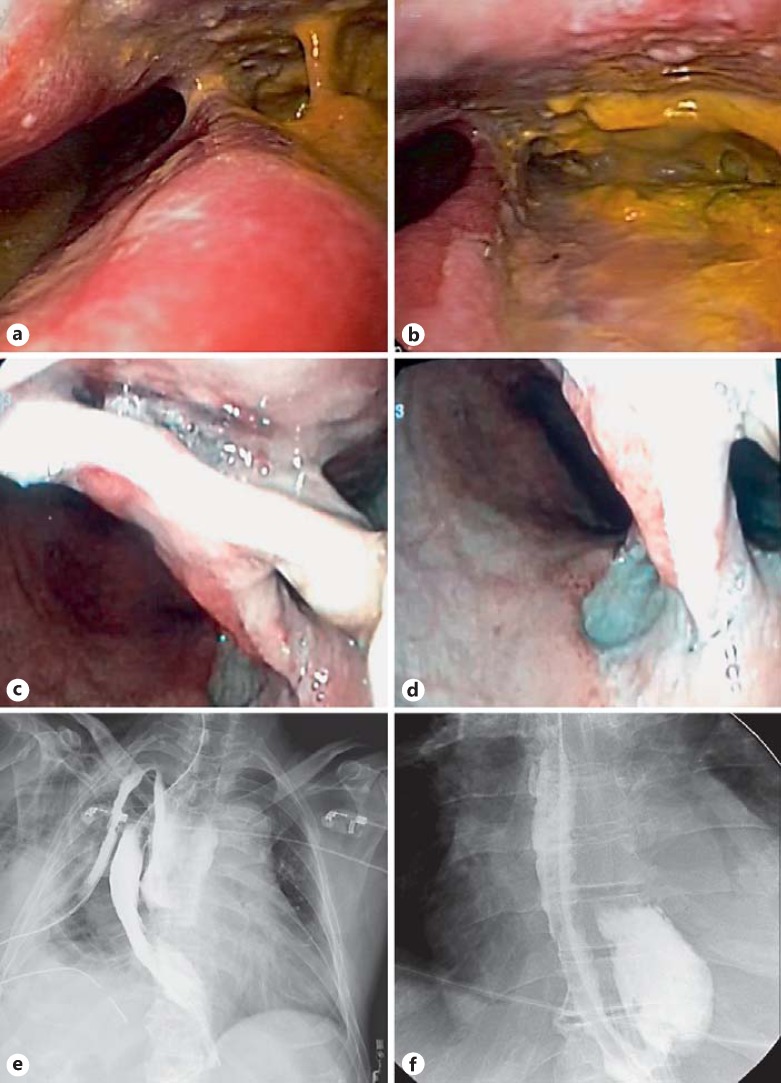
The time to leak diagnosis after surgery was in mean 16.5 ± 11.4 days (range: 7–33) (Fig. 1; Table 2). All patients were symptomatic, presenting with respiratory failure and/or infection signs; 3 of the patients had an empyema, and 1 of them had a perisplenic abscess. At the time of leak suspicion, all patients were submitted to surgical revision with evacuation of the infected fluid and placement of intrathoracic or intraabdominal drains, depending on the case. Appropriate antibiotics were also administered. In none of the cases surgical closure of the leak was achieved.
Fig. 1.
Examples of examinations leading to leak diagnosis. a-d Endoscopic view (a, b Patient 2; c, d Patient 3). e, f Fluoroscopic view demonstrating contrast extravasation (e Patient 3; f Patient 4).
Table 2.
Technical aspects of stent placement and efficacy
| Patient | Interval to stent placement after initial surgery, days | Interval to stent placement after leak detection, days | Stent length, mm | Time of stent placement, weeks | Clinical success |
|---|---|---|---|---|---|
| 1 | 18 | 6 | 80 | 6.43 | Yes |
| 2 | 42 | 9 | 150 | 8.86 | Yes |
| 3 | 17 | 3 | 150 | 6.71 | Yes |
| 4 | 8 | 1 | 150 | 5.57 | Yes |
Technical and Clinical Outcomes
Technical success was achieved in all patients using a single stent. An 8-cm stent was used in 1 patient, and a 15-cm stent in 3 patients. The stents were placed after a mean of 4.75 ± 3.5 days (range 1–9) following leak diagnosis. No anchoring measures were performed.
Stent removal was successful and without adverse events in all patients. The mean time to stent removal was 6.89 ± 1.40 weeks (range 5.57–8.86). Sufficient leak closure was confirmed through clinical signs, endoscopy, and a single-contrast fluoroscopy in all 4 cases (clinical success of 100%).
No minor or major complications were registered during placement or removal of the stent. There were no stent migrations.
Follow-Up
Two patients died during the follow-up period, none of them due to complications related to the stent procedure (Patient 2 died of a respiratory infection 1 year after the procedure, and Patient 4 died 1 month after stent removal due to small-bowel obstruction). A symptomatic stricture developed at the level of the esophagogastric anastomosis in Patient 3, requiring 5 sessions of balloon dilatation with a through-the-scope balloon. Since then, the patient has remained symptom free.
Discussion
Postsurgical leaks and fistula of the upper GI tract still lead to significant morbidity and mortality, and management is challenging. Even though stent placement has emerged as a potential successful treatment for these conditions in recent years, its use was hampered by a relatively high rate of stent migration. In this study, we report our results on safety and efficacy of the utilization of colonic stents for the treatment of postsurgical leaks of the upper GI tract in critically ill patients for whom no other treatment options such as surgery were possible. The rationale for the utilization of colonic stents lies in their bigger diameter, with a potentially lower risk of migration and a better watertight barrier to luminal contents, favoring leak healing. This advantage is of particular importance after upper GI surgery, especially after esophageal resections, where a larger postoperative lumen of the GI tract is found without an obstructive lesion to keep the stent in place. On the other hand, there may also be a greater risk of adverse events [4, 5, 6, 10]. Our study suggests that placement and removal of colonic FSEMS are effective and safe in this particularly difficult group of patients. Remarkably, there was no stent migration or complications in our series.
Recent studies evaluated different types of stents for the management of fistulas or leakages in benign indications. The ideal stent in this context would effectively seal the leak, have a low risk of migration, prevent tissue in- or overgrowth, and be easily removable. A stent with all these characteristics still does not exist. In a systematic review that included 267 patients from 25 studies with a benign esophageal rupture or leak treated with different stents, healing of the rupture or leak was accomplished in 85% of the cases [5]. No differences were noted between PSEMS, FSEMS, and SEPS regarding the efficacy or time of stent placement needed for healing. On the other hand, stent migration with the need of re-intervention occurred in 25% of the patients and was more common with FSEMS (26%) and SEPS (26%) when compared with PSEMS (13%). As for tissue in- or overgrowth, it was more common with PSEMS (12%) compared with SEPS (3%) and FSEMS (7%).
Fischer et al. [12] also addressed the necessity of a stent with a larger diameter after surgery of the upper GI tract due to the lack of watertightness and consequent persistent leak and to the risk of stent migration. They developed a PSEMS with a shaft diameter of 36 mm, a flare diameter of 40 mm, and a noncovered area at the flares of only 5 mm, in order to permit mucosal ingrowth but still facilitating stent extraction. They placed this stent in 11 consecutive patients with postoperative leaks. As in our study, the treatment was successful in all patients; however, their dislocation rate was 36%, which the authors attributed to the stent's strong expansion force, short noncovered flares, and angular positioning. No major complications or harm to the GI wall were noted.
In a multicenter study, van den Berg et al. [10] evaluated the safety and efficacy of the placement of a Hanarostent® CCI for the treatment of upper GI perforations, anastomotic leaks, and fistula; the same stent was used in our series. Of the 34 patients treated, there was technical success in 97% and clinical success in 50% of the patients. The lower clinical success rate as compared to the available studies in the literature was explained by the use of the stent as a last salvation option as previous treatments had been attempted in 16 of the 34 patients. The size of the leak and delay until stent placement may have been factors contributing to worse results, but these data were not provided by the authors. As mentioned, stent placement has been proposed for leaks involving less than 50–70% of the circumference, and surgery is generally recommended for larger leaks [4, 6, 13]. The timing is also a critical factor for healing, as success rates of 50% are reported when the stent placement is performed more than 1 month after perforation as compared to nearly 100% of success on an early approach [4, 5, 14, 15]. In our patients, the maximum time to stent placement after leak detection was 9 days, which might explain the excellent results. Other factors contributing to the poor outcomes in the study by van den Berg et al. [10] may have been the use of concomitant antibiotics and simultaneous drainage of infected areas. As opposed to our series, where all patient were under antibiotic therapy and had a surgically placed intrathoracic or intra-abdominal drain, in their study, only 74 and 65% of the patients, respectively, had these additional measures performed. The early and adequate drainage of fluid collections or abscess cavities in the pleural cavity, mediastinum, or peritoneal cavity, either endoscopically, radiologically, or surgically, is considered an absolute prerequisite for healing [5, 6]. One final factor affecting outcome is the time to stent removal. Even though animal studies suggested 4 weeks as sufficient time for tissue healing, several studies suggest an average of 7 weeks as the optimal time for stent removal [4, 5], which was precisely the mean time observed in our series.
Disappointingly, in the van den Berg study [10], in 21% of the patients, a complete stent migration occurred after a median of 7 days, an additional complete migration occurred with the placement of a second stent in 1 patient, and 6 partial stent migrations were repositioned endoscopically. The overall stent migration was therefore of 41%, and the authors concluded that increasing the stent diameter does not appear to provide better anchoring of SEMS. As in our study, no additional measures were performed to anchor the stent. However, we did not have any case of stent migration, which may be related to differences in the stent placement technique, the postsurgical anatomy, or the small number of cases in our series, which may have not been enough for this complication to occur.
In terms of safety, the use of stents with a larger diameter was not associated with complications such as bleeding, perforation, or tracheal compression, neither in our study, nor in studies in which large diameters were used with this specific indication [10, 12]. In 1 case, an esophageal stricture developed as a long-term complication following stent removal, requiring several balloon dilations. The higher rate of perforations, fistula, fever, or severe bleeding reported in other studies with the use of larger diameters may be related to the use of these stents in patients with esophageal strictures [16].
The present report has some limitations, such as the retrospective design, conditioning the limited availability of data and lack of a common protocol in the treatment of these patients. Nevertheless, the fact that the same operator was responsible for the technical procedure and posterior decisions brings some homogeneity to the management of the cases reported. Furthermore, the number of patients in this series is small. However, it is a very particular population constituted of critically ill patients with no possibility of surgical treatment due to their frail status, and a large patient number can only be obtained by multicenter studies. Remarkably, despite their serious condition, stent placement was clinically successful, avoiding surgical re-intervention in all patients.
Randomized controlled trials are the best way to determine the optimal treatment strategy and to standardize the therapeutic approach, namely in the decision of surgical versus endoscopic treatment and, in case of the latter, the best technique for each situation. However, in this particular situation where there is a small number of patients in critical conditions associated with increasing evidence of efficacy of the use of stents, a randomized controlled trial is difficult to perform. As the efficacy does not appear to be different between FSEMS and PSEMS, other factors such as the risk of migration and easy stent removal should be taken into consideration at the time of stent choice. The diameter of the stent might be a characteristic that influences the risk of migration. New approaches are now emerging, such as covered biodegradable stents.
In conclusion, larger-diameter FSEMS such as the already available colonic stents are an effective and safe treatment for patients with postoperative fistula or anastomotic leaks with a low migration rate and should be considered as an option especially in critically ill patients. However, in order for the treatment to be successful, optimal conditions such as an early stent placement, an adequate concomitant drainage of fluid collections, and stent removal after 7 weeks should be provided.
Statement of Ethics
Protection of human and animal subjects: the authors declare that no experiments were performed on humans or animals for this study. Confidentiality of data: the authors declare that they have followed the protocols of their work center on the publication of patient data. Right to privacy and informed consent: the authors declare that no patient data appear in this article. Full and informed consent for the stent placement was obtained from each patient or from the patient's legal representative.
Disclosure Statement
The authors declare that there are no conflicts of interest to disclose.
References
- 1.Milek T, Ciostek P, Petryka R, Slowik J, Jarosz M. Results of endoscopic and surgical fistula treatment in oesophagointestinal anastomosis after gastrectomy. Wideochir Inne Tec Maloinwazyjne. 2016;10:515–520. doi: 10.5114/wiitm.2015.56478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sauvanet A, Mariette C, Thomas P, Lozac'h P, Segol P, Tiret E, et al. Mortality and morbidity after resection for adenocarcinoma of the gastroesophageal junction: predictive factors. J Am Coll Surg. 2005;201:253–262. doi: 10.1016/j.jamcollsurg.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 3.Meyer L, Meyer F, Dralle H, Ernst M, Lippert H, Gastinger I. Insufficiency risk of esophagojejunal anastomosis after total abdominal gastrectomy for gastric carcinoma. Langenbeck Arch Surg. 2005;390:510–516. doi: 10.1007/s00423-005-0575-2. [DOI] [PubMed] [Google Scholar]
- 4.Manta R, Magno L, Conigliaro R, Caruso A, Bertani H, Manno M, et al. Endoscopic repair of post-surgical gastrointestinal complications. Digest Liver Dis. 2013;45:879–885. doi: 10.1016/j.dld.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 5.van Boeckel PG, Sijbring A, Vleggaar FP, Siersema PD. Systematic review: temporary stent placement for benign rupture or anastomotic leak of the oesophagus. Aliment Pharm Ther. 2011;33:1292–1301. doi: 10.1111/j.1365-2036.2011.04663.x. [DOI] [PubMed] [Google Scholar]
- 6.Schubert D, Scheidbach H, Kuhn R, Wex C, Weiss G, Eder F, et al. Endoscopic treatment of thoracic esophageal anastomotic leaks by using silicone-covered, self-expanding polyester stents. Gastrointest Endosc. 2005;61:891–896. doi: 10.1016/s0016-5107(05)00325-1. [DOI] [PubMed] [Google Scholar]
- 7.van Boeckel PG, Dua KS, Weusten BL, Schmits RJ, Surapaneni N, Timmer R, et al. Fully covered self-expandable metal stents (SEMS), partially covered SEMS and self-expandable plastic stents for the treatment of benign esophageal ruptures and anastomotic leaks. BMC Gastroenterol. 2012;12:19. doi: 10.1186/1471-230X-12-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Loske G, Schorsch T, Muller C. Endoscopic vacuum sponge therapy for esophageal defects. Surg Endosc. 2010;24:2531–2535. doi: 10.1007/s00464-010-0998-x. [DOI] [PubMed] [Google Scholar]
- 9.Hindy P, Hong J, Lam-Tsai Y, Gress F. A comprehensive review of esophageal stents. Gastroenterol Hepatol (NY) 2012;8:526–534. [PMC free article] [PubMed] [Google Scholar]
- 10.van den Berg MW, Kerbert AC, van Soest EJ, Schwartz MP, Bakker CM, Gilissen LP, et al. Safety and efficacy of a fully covered large-diameter self-expanding metal stent for the treatment of upper gastrointestinal perforations, anastomotic leaks, and fistula. Dis Esophagus. 2016;29:572–579. doi: 10.1111/dote.12363. [DOI] [PubMed] [Google Scholar]
- 11.Gonzalez JM, Garces Duran R, Vanbiervliet G, Lestelle V, Gomercic C, Gasmi M, et al. Double-type metallic stents efficacy for the management of post-operative fistulas, leakages, and perforations of the upper gastrointestinal tract. Surg Endosc. 2015;29:2013–2018. doi: 10.1007/s00464-014-3904-0. [DOI] [PubMed] [Google Scholar]
- 12.Fischer A, Bausch D, Richter-Schrag HJ. Use of a specially designed partially covered self-expandable metal stent (PSEMS) with a 40-mm diameter for the treatment of upper gastrointestinal suture or staple line leaks in 11 cases. Surg Endosc. 2013;27:642–647. doi: 10.1007/s00464-012-2507-x. [DOI] [PubMed] [Google Scholar]
- 13.Siersema PD. Treatment of esophageal perforations and anastomotic leaks: the endoscopist is stepping into the arena. Gastrointest Endosc. 2005;61:897–900. doi: 10.1016/s0016-5107(05)01589-0. [DOI] [PubMed] [Google Scholar]
- 14.Swinnen J, Eisendrath P, Rigaux J, Kahegeshe L, Lemmers A, Le Moine O, et al. Self-expandable metal stents for the treatment of benign upper GI leaks and perforations. Gastrointest Endosc. 2011;73:890–899. doi: 10.1016/j.gie.2010.12.019. [DOI] [PubMed] [Google Scholar]
- 15.Siersema PD, Homs MY, Haringsma J, Tilanus HW, Kuipers EJ. Use of large-diameter metallic stents to seal traumatic nonmalignant perforations of the esophagus. Gastrointest Endosc. 2003;58:356–361. doi: 10.1067/s0016-5107(03)00008-7. [DOI] [PubMed] [Google Scholar]
- 16.Verschuur EM, Steyerberg EW, Kuipers EJ, Siersema PD. Effect of stent size on complications and recurrent dysphagia in patients with esophageal or gastric cardia cancer. Gastrointest Endosc. 2007;65:592–601. doi: 10.1016/j.gie.2006.12.018. [DOI] [PubMed] [Google Scholar]