Abstract
Objectives
Glucocorticoid (GC) use is widespread and associated with many adverse effects. Thus, it is important to ascertain GC utilisation patterns. In this study, we examined the annual prevalence of prescription users and amount of use of systemic GCs.
Design
Population-wide prevalence study.
Setting
The primary healthcare and hospital sectors in Denmark from 1999 to 2015.
Results
Approximately 3% of the Danish population redeemed at least one prescription for a systemic GC annually between 1999 and 2015, with annual prevalence remaining constant over the period. However, after adjusting for age and sex, we observed a decrease in annual prevalence from 1999 to 2015, with a prevalence ratio of 0.92 (95% CI 0.91 to 0.92). Annual prevalence was highest among the elderly (7.0%–8.2% among persons 65–79 years of age and 8.4%–10% among persons 80+ years of age). Prednisolone was the most frequently redeemed systemic GC, with annual prevalence increasing from 1.4% to 2.1% during the 1999–2015 period. The amount of systemic GCs provided to the hospital sector increased from 2.3 defined daily doses (DDD)/1000 inhabitants/day in 1999 to 3.5 DDD/1000 inhabitants/day in 2015, while the amount provided to the primary healthcare sector remained constant in the range of 10–11 DDD/1000 inhabitants/day.
Conclusion
We found a high prevalence of systemic GC use of 3% with a remarkably high prevalence in elderly of up to 10%, wherefore continued awareness of its effects is mandated.
Keywords: Glucocorticoids, Denmark, Prevalence, Drug utilisation
Strengths and limitations of this study.
Current knowledge of glucocorticoid (GC) utilisation patterns is in need of updating and expansion.
A strength of our study is the population-based design that enables us to assess utilisation of systemic GCs in the entire Danish nation from 1999 to 2015.
An additional advantage was the ability to assess GC use in the hospital sector as well as the primary healthcare sector, which is normally not captured when using Danish prescription registries for research.
The results of this study apply only to redeemed prescriptions and sales of systemic GCs and not necessarily to actual adherence and use.
As we used aggregated data, we were not able to address number of prescriptions at an individual level, to separate oral and injectable formulations, to obtain incidence use and to assess use of comedication.
Background
Glucocorticoids (GCs) are potent anti-inflammatory drugs used widely since the 1950s to treat common conditions such as asthma, chronic obstructive pulmonary disease, chronic inflammatory bowel diseases, rheumatic diseases and malignancies.1 Besides their beneficial effects in treating inflammatory diseases, GCs are associated with increased risk of a number of adverse outcomes, including iatrogenic adrenocortical insufficiency,2 venous thromboembolism3 and cardiac disease.4–6 In addition, GCs can cause metabolic diseases such as hyperglycaemia, diabetes7 and dyslipidaemia.8 They also are associated with increased risk of osteoporosis9 and neuropsychiatric disorders.10
Current knowledge of GC utilisation patterns is in need of updating and expansion. Earlier studies estimated that the prevalence of oral GC use is approximately 1% in the UK and the US adult populations.11–13 In the current population-based study, we examined the annual prevalence of systemic GC prescription users (one or more redeemed prescriptions in a year) in the primary healthcare sector and ascertained the amount of GC used within the primary healthcare and hospital sectors in Denmark during 1999–2015.
Methods
Setting
Our study population included the entire Danish population from 1 January 1999 to 31 December 2015. Denmark provides its entire population (5.6 million) with universal tax-supported healthcare, guaranteeing free and equal access to general practitioners and hospitals and partial reimbursement for prescribed medications, including GCs. A unique central personal registration number (civil registration number) is assigned to all Danish residents at birth or on immigration, enabling accurate and unambiguous linkage of relevant registries at the individual level.14
Utilisation of systemic glucocorticoids in Denmark
In Denmark, all systemic GCs (ATC code H02AB) are available by prescription only. We used Medstat (http://www.medstat.dk) to retrieve data on systemic GC amount and prevalence of prescription users in Denmark.15 The publicly available Medstat website hosted by the Danish Serum Institute provides aggregate statistics on the sale of pharmaceutical preparations in Denmark since 1995, based on data reported to the Register of Medicinal Product Statistics.16 Aggregated Medstat statistics are complete from 1999 onwards and allow for extraction of both amount (in primary healthcare and hospital sector) and number of users (in primary healthcare) each year.15 Amount is expressed in defined daily doses (DDD)/1000 inhabitants/24 hours and can be assessed in primary healthcare sector, hospital sector and in total. DDD is developed by WHO and defined as the assumed average maintenance dose per day for a drug used for its main indication in adults.17 However, it should be emphasised that the DDD is a unit of measurement and does not necessarily reflect the recommended prescribed dose. As an example, the DDD for prednisolone is 10 mg per day. Medicines to the hospital sector are distributed to departments, and the people who are treated with the medicines are not reported; hence, only amount and not prevalence of users can be assessed in this sector. Use in primary healthcare includes individual dispensing of medicines in pharmacies. As the civil registration number is registered at each prescription redemption at pharmacies in Denmark, we were able to retrieve number of prescription users in primary care in addition to amount and stratify on age and sex.
Statistical analysis
First, we focused on prescriptions for systemic GCs in the primary healthcare sector. The annual prevalence of systemic GC prescription users was defined as the number of people who redeemed at least one prescription for a systemic GC each year divided by the number of people in the population each year (as of 1 January). We calculated overall annual prevalence and then stratified by sex and age group (0–4 years, 5–9 years, 10–14 years, 15–19 years, 20–39 years, 40–64 years, 65–79 years and ≥80 years). Age was defined as the age at which the first prescription was redeemed each year. We further stratified on generic type of systemic GC. In our computation of the annual prevalence of GC use, the entire Danish population served as the reference group. When we computed the prevalence in subgroups (age and sex), the subgroup of interest served as the reference population. To examine changes in prevalence, we used a Poisson regression model to estimate adjusted prevalence ratios according to age, sex and calendar year. When comparing age groups, we adjusted for sex and calendar year; when comparing sex, we adjusted for age group and calendar year and when comparing calendar years, we adjusted for sex and age group. Finally, we calculated the amount (DDD/1000 inhabitants/24 hours) of systemic GC used in total and according to healthcare sector (primary healthcare sector and hospital sector). We conducted our statistical analyses using Stata 12 for Windows (Stata Corp, College Station, TX, USA).
Results
In any given year between 1999 and 2015, 3% (range: 3.0%–3.4%) of the total Danish population redeemed at least one prescription for a systemic GC (table 1). Overall, prevalence of systemic GC prescription users during this period, adjusted for age and sex, was fairly stable with a slight decrease towards the end of the period (table 2).
Table 1.
Annual prevalence of systemic glucocorticoid (GC) prescription users in Denmark, 1999–2015, overall and stratified by sex and age group
| Prevalence of prescription users (% of the national population) | |||||||||||
| All | Sex | Age groups (years) | |||||||||
| Women | Men | 0–4 | 5–9 | 10–14 | 15–19 | 20–39 | 40–64 | 65–79 | 80+ | ||
| 1999 | 3.2 | 3.4 | 2.9 | 0.06 | 0.1 | 0.2 | 0.9 | 2.2 | 3.8 | 8.1 | 8.4 |
| 2000 | 3.3 | 3.6 | 3.0 | 0.06 | 0.1 | 0.2 | 1.0 | 2.4 | 3.9 | 8.1 | 8.7 |
| 2001 | 3.3 | 3.6 | 3.0 | 0.09 | 0.1 | 0.2 | 1.0 | 2.4 | 3.9 | 8.2 | 8.8 |
| 2002 | 3.3 | 3.6 | 3.0 | 0.06 | 0.1 | 0.3 | 1.1 | 2.6 | 3.9 | 8.1 | 8.9 |
| 2003 | 3.2 | 3.5 | 2.9 | 0.07 | 0.1 | 0.2 | 1.0 | 2.3 | 3.8 | 8.0 | 8.9 |
| 2004 | 3.2 | 3.5 | 2.9 | 0.06 | 0.1 | 0.2 | 0.9 | 2.3 | 3.8 | 8.0 | 8.9 |
| 2005 | 3.3 | 3.6 | 3.0 | 0.06 | 0.1 | 0.2 | 1.0 | 2.5 | 3.8 | 8.0 | 9.2 |
| 2006 | 3.4 | 3.7 | 3.0 | 0.07 | 0.1 | 0.3 | 1.1 | 2.5 | 4.0 | 8.0 | 9.3 |
| 2007 | 3.4 | 3.7 | 3.1 | 0.07 | 0.1 | 0.3 | 1.2 | 2.6 | 4.0 | 8.0 | 9.4 |
| 2008 | 3.4 | 3.7 | 3.1 | 0.07 | 0.1 | 0.3 | 1.2 | 2.6 | 3.9 | 7.7 | 9.5 |
| 2009 | 3.3 | 3.6 | 3.0 | 0.08 | 0.1 | 0.3 | 1.1 | 2.4 | 3.9 | 7.7 | 9.5 |
| 2010 | 3.3 | 3.6 | 2.9 | 0.07 | 0.1 | 0.2 | 1.0 | 2.2 | 3.8 | 7.6 | 9.7 |
| 2011 | 3.2 | 3.5 | 2.9 | 0.08 | 0.1 | 0.2 | 1.0 | 2.1 | 3.7 | 7.4 | 9.7 |
| 2012 | 3.1 | 3.4 | 2.8 | 0.07 | 0.1 | 0.2 | 0.9 | 2.0 | 3.6 | 7.2 | 9.7 |
| 2013 | 3.1 | 3.4 | 2.8 | 0.08 | 0.1 | 0.2 | 0.8 | 1.9 | 3.5 | 7.1 | 10 |
| 2014 | 3.1 | 3.4 | 2.8 | 0.07 | 0.1 | 0.2 | 0.8 | 1.9 | 3.5 | 7.0 | 9.8 |
| 2015 | 3.0 | 3.3 | 2.7 | 0.07 | 0.1 | 0.2 | 0.7 | 1.7 | 3.3 | 7.0 | 9.9 |
Reference group for all systemic GCs is all members of the Danish population as of 1 January in the year of interest. Reference groups for the stratified results are all members in the subpopulation of interest as of 1 January of each year.
Table 2.
Prevalence ratios of redemption of systemic glucocorticoid prescriptions according to sex, age and calendar year, modelled using a multivariable Poisson regression
| Prevalence ratios (95% CI) | |
| Sex* | |
| Men | 1 (ref) |
| Women | 1.11 (1.11 to 1.11) |
| Age groups (years)† | |
| 0–19 | 1 (ref) |
| 20–39 | 6.84 (6.79 to 6.89) |
| 40–64 | 10.7 (10.7 to 10.8) |
| 65–79 | 21.3 (21.1 to 21.4) |
| 80+ | 25.3 (25.1 to 25.5) |
| Calendar year‡ | |
| 1999 | 1 (ref) |
| 2000 | 1.03 (1.03 to 1.04) |
| 2001 | 1.03 (1.03 to 1.04) |
| 2002 | 1.05 (1.05 to 1.06) |
| 2003 | 1.01 (1.00 to 1.02) |
| 2004 | 1.02 (1.01 to 1.03) |
| 2005 | 1.04 (1.03 to 1.04) |
| 2006 | 1.06 (1.05 to 1.07) |
| 2007 | 1.06 (1.06 to 1.07) |
| 2008 | 1.06 (1.05 to 1.07) |
| 2009 | 1.05 (1.04 to 1.06) |
| 2010 | 1.02 (1.01 to 1.03) |
| 2011 | 1.00 (1.00 to 1.01) |
| 2012 | 0.97 (0.96 to 0.98) |
| 2013 | 0.95 (0.94 to 0.96) |
| 2014 | 0.95 (0.94 to 0.96) |
| 2015 | 0.92 (0.91 to 0.92) |
*Prevalence ratios adjusted for age group and calendar year.
†Prevalence ratios adjusted for sex and calendar year.‡Prevalence ratios adjusted for sex and age group.
The annual prevalence of systemic GC prescription users was higher among women than among men with a prevalence ratio of 1.11 (95% CI 1.11 to 1.11) (table 2) and prevalence ranging from 3.3% to 3.7% in women and 2.7% to 3.1% in men (table 1). The prevalence of prescription users increased substantially with age. Thus, persons aged 40–64 were more than 10 times as likely and persons aged 80+ were more than 25 times as likely to receive GC treatment than those aged below 19 (table 2). While prevalence was relatively constant between 1999 and 2015, the prevalence fell from 8.2% to 7.0% among persons aged 65–79 years and increased from 8.4% to 10% among those aged 80 or above (table 1).
The most frequently redeemed systemic GC was prednisolone. Its annual prevalence of redemption in the Danish population increased from 1.4% to 2.1% during 1999 and 2015. In 2015, prednisolone accounted for 50% of all GC prescriptions redeemed in the period (taking into account only the first prescription each year). There was a decrease in redemptions of prednisone and betamethasone, from 0.4% to 0.1% and from 1.0% to 0.4% of the Danish population, respectively, from 1999 to 2015 (figure 1).
Figure 1.
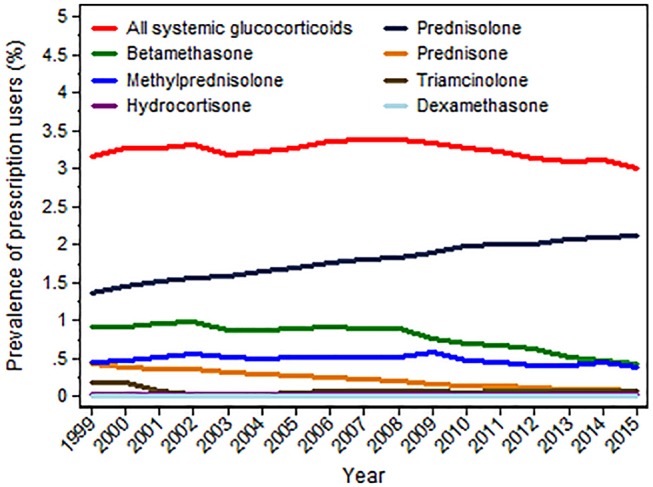
Annual prevalence of systemic glucocorticoid (GC) prescription users in Denmark, 1999–2015, overall and stratified by generic type. All systemic GCs (red line), prednisolone (dark blue line), betamethasone (green line), prednisone (orange line), methylprednisolone (blue line), triamcinolone (dark green line), hydrocortisone (purple line), dexamethasone (light blue line).
The amount of systemic GC used in the primary healthcare sector consistently remained at 10 DDD/1000 inhabitants/24 hours (range: 10.0–10.8 DDD/1000 inhabitants/24 hours) from 1999 to 2015. The amount of systemic GCs used in the hospital sector increased from 2.3 DDD/1000 inhabitants/24 hours in 1999 to 3.5 DDD/1000 inhabitants/24 hours in 2015 (table 3).
Table 3.
Amount of systemic glucocorticoids sold to the primary healthcare sector, hospital sector and in total, Denmark, 1999–2015
| Defined daily dose/1000 inhabitants/24 hours | |||
| Primary sector healthcare sector | Hospital sector | Total | |
| 1999 | 10.4 | 2.3 | 12.7 |
| 2000 | 10.5 | 2.3 | 12.8 |
| 2001 | 10.8 | 2.3 | 13.1 |
| 2002 | 11.0 | 2.6 | 13.5 |
| 2003 | 10.8 | 2.5 | 13.3 |
| 2004 | 10.8 | 2.4 | 13.2 |
| 2005 | 10.8 | 2.5 | 13.3 |
| 2006 | 10.8 | 2.6 | 13.4 |
| 2007 | 10.7 | 2.7 | 13.4 |
| 2008 | 10.7 | 2.7 | 13.4 |
| 2009 | 10.6 | 3.0 | 13.6 |
| 2010 | 10.5 | 3.1 | 13.6 |
| 2011 | 10.3 | 3.1 | 13.5 |
| 2012 | 10.2 | 3.3 | 13.5 |
| 2013 | 10.1 | 3.4 | 13.5 |
| 2014 | 10.1 | 3.6 | 13.7 |
| 2015 | 10.0 | 3.5 | 13.5 |
Discussion
This population-based nationwide study found a high prevalence (3%) of systemic GC users from 1999 to 2015 in Denmark, especially among the elderly (10%). This underscores the importance of clinical awareness of the adverse effects of GC treatment. Still, when changes in the age structure of the population were taken into consideration, a minor decrease in prevalence of GC prescriptions users was observed during the study period. When assessing amount of systemic GC use, we observed a slight increase from 1999 to 2015, mainly due to inclined use in the hospital sector.
Previous studies conducted in UK and USA reported a lower prevalence of approximately 1%.11–13 However, UK and USA estimates were limited to the use of oral GCs. Our inclusion of all systemic GCs—both oral and injectable formulations—might explain in part the higher estimates of prevalence of use in the Danish population. Also, the UK study covered only long-term (≥1 year) GC use,11 while our study included all use. Still, the results from our study most likely reflect a higher use of systemic GCs in Denmark compared with UK and USA.
The UK study reported an increase in prescriptions for long-term oral GCs of nearly 34% between 1989 and 2008.11 Our study found that overall annual prevalence did not vary substantially between 1999 and 2015. Taking into account changes in age and sex distribution of the population, we found a decrease in the annual prevalence of systemic GC prescription users towards the end of our study period. Due to use of aggregated data, we were not able to investigate long-term use.
Our finding that prednisolone was the most frequent subtype of redeemed GC prescription (50%) is consistent with the UK and US studies, which reported that 92.3% and 76.6% of total GC prescriptions were for prednisolone.11 13
The UK study found the highest prevalence of use of oral GCs among women aged 80–90 years (3.05% (95% CI 3.01% to 3.09%)) and the lowest prevalence among men aged 18–29 years (0.08% (95% CI 0.07% to 0.09%)).11 In the US population, the highest prevalence of use was found among men aged ≥80 years (3.5% (95% CI 2.3% to 4.7%)) and among women aged 70–79 years (2.7% (95% CI 1.7% to 3.7%)).13 The high prevalence of GC use observed among the elderly in our study is noteworthy, as it is well established that persons in the highest age groups are particularly prone to adverse outcomes due to higher levels of comorbidity, senescent changes in the body composition and polypharmacy.18
When assessing amount of systemic GC use, we observed an increase of use in the hospital sector. A possible explanation for this can be a higher frequency of elderly admitted to the Danish hospitals from 1999 to 2015.19 When patients are hospitalised, treatment with medicine is not registered at an individual level in our national registries; hence, we were not able to examine use according to age; neither could we include GC use in the hospital sector in our prevalence analyses.
The pattern of disease has changed from 1999 to 201411 20–22 with increasing prevalence of many inflammatory diseases. Despite this, we have observed a minor decrease in prevalence of systemic GC users when taking changes in age structure into account. An explanation for this can be an increased clinical awareness of the adverse effects of GC treatment as well as increased use of alternative immunomodulatory treatments. The use of methotrexate, azathioprine and anti-tumour necrosis factor alpha therapy has increased and newer biological agents have been approved for treatment in Denmark during our study period.15
The strength of our study includes its large nationwide study population making use capable of assessing utilisation of GCs in the entire Danish nation. In addition, we had the ability to assess GC use in the hospital sector. Many drug utilisation studies do not have available information on prescribing in the hospital section. Hence, our study helps to inform which proportion of prescribing may be missing from such studies. However, this study also has limitations. First, the results of this study apply only to redeemed prescriptions and sales of systemic GCs and not necessarily to actual use or dose, as we were not able to estimate adherence to the medication. Second, as we used aggregated data, we were not able to address number of redeemed prescriptions at an individual level, to separate oral and injectable formulations, to obtain incidence use and to assess use of comedication, which is all relevant when describing utilisation patterns. Third, our study did not aim to describe utilisation of inhaled and topical GCs; however, these formulations should also be considered important when addressing adverse effects.
In conclusion, this population-based nationwide study found a high prevalence of systemic GC use of 3% with remarkably high prevalence in the elderly of up to 10%, wherefore continued awareness of its adverse effects is mandated.
Supplementary Material
Footnotes
Contributors: KL, IP, JOLJ and HTS made primary contributions to the study conception and wrote the manuscript. KL extracted results from Medstat (http://www.medstat.dk/en) and performed statistical analyses. KL, IP, JOLJ and HTS contributed to the interpretation of results and revised the manuscript critically. All authors approved the final manuscript. KL is the guarantor for this study.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Rasmussen Å. Pro.medicin.dk. Information on glucocorticoid package sizes and indications in Denmark [in Danish]. 2016;2015. [Google Scholar]
- 2.Broersen LH, Pereira AM, Jørgensen JO, et al. Adrenal insufficiency in corticosteroids use: systematic review and meta-analysis. J Clin Endocrinol Metab 2015;100:2171–80. 10.1210/jc.2015-1218 [DOI] [PubMed] [Google Scholar]
- 3.Johannesdottir SA, Horváth-Puhó E, Dekkers OM, et al. Use of glucocorticoids and risk of venous thromboembolism: a nationwide population-based case-control study. JAMA Intern Med 2013;173:743–52. 10.1001/jamainternmed.2013.122 [DOI] [PubMed] [Google Scholar]
- 4.Fardet L, Petersen I, Nazareth I. Risk of cardiovascular events in people prescribed glucocorticoids with iatrogenic Cushing's syndrome: cohort study. BMJ 2012;345:e4928 10.1136/bmj.e4928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davis JM, Maradit Kremers H, Crowson CS, et al. Glucocorticoids and cardiovascular events in rheumatoid arthritis: a population-based cohort study. Arthritis Rheum 2007;56:820–30. 10.1002/art.22418 [DOI] [PubMed] [Google Scholar]
- 6.Christiansen CF, Christensen S, Mehnert F, et al. Glucocorticoid use and risk of atrial fibrillation or flutter: a population-based, case-control study. Arch Intern Med 2009;169:1677–83. 10.1001/archinternmed.2009.297 [DOI] [PubMed] [Google Scholar]
- 7.Clore JN, Thurby-Hay L. Glucocorticoid-induced hyperglycemia. Endocr Pract 2009;15:469–74. 10.4158/EP08331.RAR [DOI] [PubMed] [Google Scholar]
- 8.Zimmerman J, Fainaru M, Eisenberg S. The effects of prednisone therapy on plasma lipoproteins and apolipoproteins: a prospective study. Metabolism 1984;33:521–6. 10.1016/0026-0495(84)90006-4 [DOI] [PubMed] [Google Scholar]
- 9.van Staa TP, Leufkens HG, Cooper C. The epidemiology of corticosteroid-induced osteoporosis: a meta-analysis. Osteoporos Int 2002;13:777–87. 10.1007/s001980200108 [DOI] [PubMed] [Google Scholar]
- 10.Fardet L, Petersen I, Nazareth I. Suicidal behavior and severe neuropsychiatric disorders following glucocorticoid therapy in primary care. Am J Psychiatry 2012;169:491–7. 10.1176/appi.ajp.2011.11071009 [DOI] [PubMed] [Google Scholar]
- 11.Fardet L, Petersen I, Nazareth I. Prevalence of long-term oral glucocorticoid prescriptions in the UK over the past 20 years. Rheumatology 2011;50:1982–90. 10.1093/rheumatology/ker017 [DOI] [PubMed] [Google Scholar]
- 12.van Staa TP, et al. Use of oral corticosteroids in the United Kingdom. QJM 2000;93:105–11. 10.1093/qjmed/93.2.105 [DOI] [PubMed] [Google Scholar]
- 13.Overman RA, Yeh J-Y, Deal CL. Prevalence of oral glucocorticoid usage in the United States: a general population perspective. Arthritis Care Res 2013;65:294–8. 10.1002/acr.21796 [DOI] [PubMed] [Google Scholar]
- 14.Pedersen CB. The Danish Civil Registration System. Scand J Public Health 2011;39:22–5. 10.1177/1403494810387965 [DOI] [PubMed] [Google Scholar]
- 15.Anonymous, Danish Serum Institute. Statistics on the annual sale of medicines in Denmark based on the data from the Register of Medicinal Product Statistics. 2016;2016. [Google Scholar]
- 16.Kildemoes HW, Sørensen HT, Hallas J. The Danish National prescription registry. Scand J Public Health 2011;39:38–41. 10.1177/1403494810394717 [DOI] [PubMed] [Google Scholar]
- 17.WHO collaborating Centre for Drug Statistics Methodology. Definition and general considerations. 2016;2017. [Google Scholar]
- 18.Bressler R, Bahl JJ. Principles of drug therapy for the elderly patient. Mayo Clin Proc 2003;78:1564–77. 10.4065/78.12.1564 [DOI] [PubMed] [Google Scholar]
- 19.Sundheds- og ældreministeriet. Healthcare in Denmark- an overview. 2016;2016. [Google Scholar]
- 20.Hammer T, Nielsen KR, Munkholm P, et al. The Faroese IBD study: incidence of inflammatory bowel diseases across 54 years of population-based data. Journal of Crohn's and Colitis 201610:934–42. 10.1093/ecco-jcc/jjw050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Minichiello E, Semerano L, Boissier M-C. Time trends in the incidence, prevalence, and severity of rheumatoid arthritis: a systematic literature review. Joint Bone Spine 2016;83:625–30. 10.1016/j.jbspin.2016.07.007 [DOI] [PubMed] [Google Scholar]
- 22.Simpson CR, Hippisley-Cox J, Sheikh A. Trends in the epidemiology of chronic obstructive pulmonary disease in England: a national study of 51 804 patients. Br J Gen Pract 2010;60:277–84. 10.3399/bjgp10X514729 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


