Abstract
Objective
To investigate knowledge of and attitudes to human papillomavirus (HPV) infection, HPV vaccination, cervical cancer, related sources of information and factors associated with willingness to vaccinate one’s own daughter among primary health care (PHC) personnel.
Design
Cross-sectional study.
Setting
PHC.
Subjects
All public health nurses (PHNs) and general practitioners (GPs) in Northern Norway were invited to answer a structured electronic questionnaire; 31% participated (N = 220).
Main outcome measures
Self-reported and actual knowledge, information sources, attitudes and willingness to vaccinate their (tentative) daughter.
Results
47% of respondents knew that HPV infection is a necessary cause of cervical cancer. PHNs had higher self-reported and actual knowledge about HPV vaccination and cervical cancer than GPs. PHNs used the Norwegian Institute of Public Health’s numerous information sources on HPV, while GPs had a low user rate. 88% of PHNs and 50% of GPs acquired information from the pharmaceutical industry. 93% PHNs and 68% of GPs would vaccinate their 12-year-old daughter. In a multivariate logistic regression analysis, willingness to vaccinate one’s daughter was positively associated with younger age, being PHN (OR = 5.26, 95%CI 1.74–15.94), little concern about vaccine side effects (OR = 3.61, 95%CI 1.10–11.81) and disagreement among experts (OR = 7.31, 95%CI 2.73–19.60).
Conclusions
Increased knowledge about HPV infection and vaccination is needed, particularly among GPs. Those least concerned about side effects and disagreements among experts were most likely to vaccinate their daughter. These findings are of interest for public health authorities responsible for the Norwegian vaccination and cervix cancer screening programmes, and providers of training of PHC personnel.
Key points
One year after introduction of HPV vaccination among 12-year-old schoolgirls in Norway, a cross-sectional study in Northern Norway among general practitioners (GPs) and public health nurses (PHNs) showed that
• barely half of PHC professionals knew the causal relationship between HPV infection and cervical cancer
• PHNs and GPs had higher self-reported than actual knowledge about HPV vaccination and cervical cancer
nearly all PHNs and two thirds of GPs wanted to vaccinate their 12-year-old daughter. Those most concerned about side effects and disagreement among experts were less likely to vaccinate.
Keywords: HPV vaccine, GP, public health nurses, knowledge and attitudes, school-based, vaccination programme, Norway
Introduction
In 2012, 330 women in Norway got a cervical cancer diagnosis, and 68 women died from the disease. Annually, about 3000 women in Norway undergo surgical treatment due to pre-cancerous cervical lesions [1]. Such uterus-saving procedures can increase the risk of late miscarriage and preterm delivery in subsequent pregnancies [2,3], thus adding to the disease burden among women infected with the human papillomavirus (HPV). The incidence of cervical cancer varies across the Nordic countries, with the highest incidence in Greenland, followed by Denmark, Norway, Iceland, Sweden and Finland [4]. A persistent infection with oncogenic genotypes of HPV is a prerequisite for cervical cancer [4]. The HPV genotypes 16 and 18 account for approximately 75% of cases of cervical cancer [5]. There were two commercially available HPV vaccines against these genotypes. The quadrivalent vaccine was chosen for the Norwegian programme. This vaccine also counteracts genotypes 6 and 11, causing 86% of cases of anogenital warts [4,5].
Long-term follow-up studies of the commercially available vaccines demonstrate their effectiveness in reducing the incidence of HPV infection with a corresponding reduction in cervical intraepithelial neoplasia (CIN, grades 2 and 3), and adenocarcinoma in situ associated with HPV, which are well-documented predictors of cervical cancer [6–8]. Few serious side effects have been detected in follow-up studies of the vaccine [6,8]. Already in 2006 the inclusion of HPV-vaccine in childhood immunisation programmes was recommended [9]. In 2007, the Norwegian Institute of Public Health (NIPH) recommended this, and vaccination started in 2009 for 12-year-old girls [10,11]. In 2008 the European Centre for Disease Prevention and Control (ECDC) also recommended inclusion of the HPV vaccine in vaccination programmes [12].
In most Nordic countries, health professionals who were active in the debate concerning HPV vaccination were mostly in favour of the vaccine. In Norway, there has been disagreement among leading health professionals, including the editor of the Journal of the Norwegian Medical Association, about the safety, efficacy and duration of the HPV vaccine [4]. In several editorials in 2007/2008 the editor responded to the health authorities proposals and the support from an independent governmental council [13–18], followed by editorials in leading international medical journals in 2008–09 [19,20]. Her position was that more long-term studies were needed to collect more data on long-term effects, side effects and efficacy, since the endpoints in the trials were precancerous lesions only. She also argued that replacement by other oncogenic HPV genotypes could occur when the vaccine reduced the genotypes 16 and 18 in the population. While the Norwegian Council for Priority Setting in Health Care endorsed HPV-vaccination inclusion in the vaccination programme [18], the Norwegian College of General Practice called for a postponement, as did the Norwegian Biotechnology Advisory Board [21,22].
In January 2009, the NIPH conducted a nationwide telephone survey on knowledge and attitudes among PHNs and GPs on topics related to HPV vaccination to explore the need for updating among key vaccination personnel in order to provide proper training before the HPV-vaccination programme commenced. The respondents generally held a positive view on HPV vaccination, but the survey revealed that the PHC professionals needed more knowledge about the vaccine, HPV infection and cervical cancer [23]. During spring 2009, the NIPH in collaboration with the county chief medical officers arranged courses nationwide on these topics, mostly relevant for PHNs, and GPs working in the school-based health service and as municipal public health officers. Vaccinations started with girls born in 1997, and 70% of these girls have received the first dose, and 67% all three doses, but vaccination coverage has steadily increased up to approximately 80% [24,25]. Other vaccines in the school-based programme show coverage >90% [4].
In the light of professional controversy and lower HPV vaccination rates among schoolgirls, the aim of this study was to identify the extent of knowledge about and the attitudes towards the HPV vaccine among PHNs and GPs in order to identify related information sources and barriers to uptake; and to stimulate further education of the professions on this issue.
Materials and methods
The eligible group consisted of 307 PHNs and 448 GPs in Nordland, Troms and Finnmark counties, i.e. all public health nurses and GPs in Northern Norway. The membership list of the Norwegian Medical Association provided the email addresses of all the GPs, while the northern counties representatives of the Association of Public Health Nurses provided the email addresses of the PHNs.
Electronic questionnaires (Questback) were sent by email in December 2010, with four reminders. Both PHNs and GPs got the same questions concerning knowledge and attitudes to HPV infection, vaccination, and cervical cancer, derived from the NIPH pre-vaccination survey of PHC professionals [23] New questions on information sources and willingness to vaccinate one’s own 12-year-old daughter were added. GPs were also asked on willingness to vaccinate an older daughter aged 13–17 years and same-age patients on request.
Responses on self-reported knowledge and attitudes questions (Tables 1 and 3) were originally given on a five-point scale from very low/strongly disagree (value 1) to very high/strongly agree (value 5) or ‘don’t know’. The Questback form did not allow participants to continue, unless they had answered the questions presented in Tables 1–4. The self-reported knowledge and attitude responses were dichotomized into high/clearly agreement responses (values 4 and 5) coded as 'yes' (1), versus all other responses (i.e. values 1–3 and ‘don't know’) coded as zero (0), Actual knowledge questions were assessed with pre-coded response alternatives (Table 2) and were coded as ‘true’ (1) versus ‘false/don’t know’ (0). ‘Don’t know’ responses were few on the self-reported knowledge questions (2–5 on each) and on attitude questions (mostly in the range 0–3). The actual knowledge response had several ‘don’t know responses’, mostly two-digit responses on each question (range 10–36).
Table 1.
Proportion (%) of GPs and public health nurses in Northern Norway with self-reported high knowledge of HPV infection, vaccine and cervical cancer (95% CI).a
| GPs (n = 121) % | Public health nurses (n = 99) % | pb | |
|---|---|---|---|
| How much knowledge do you think you have about HPV and cervical cancer?c | 84 (77–91) | 97 (93–100) | <0.001 |
| How much knowledge do you think you have about the extent of cervical cancer?c | 61 (51–70) | 81 (73–89) | <0.001 |
| How much knowledge do you think you have about the HPV vaccine?c | 64 (55–73) | 99 (97–101) | <0.001 |
One year after the introduction of the HPV vaccine in the vaccination programme.
Significant differences between GPs and PHN in bold, p value based on the Chi square test.
Used as independent variables in logistic regression model(s).
Table 3.
Attitudes towards HPV infection, vaccine and cervical cancer among GPs and public health nurses in Northern Norway: Proportion (%) agreeing with the following statements (95% CI).a
| GPs (n = 121) % | Public healthnurses (n = 99) % | pb | |
|---|---|---|---|
| I am very concerned about possible side effects in the long termd | 13 (7–19) | 9 (3–15) | 0.337 |
| I am very unsure about whether the vaccine is effective enough against cancerd | 21 (14–28) | 17 (10–24) | 0.512 |
| I am worried that the vaccine may make the screening programme less populard | 22 (15–29) | 14 (7–21) | 0.160 |
| I am concerned because there is much disagreement among experts about the vaccined | 24 (16–32) | 15 (8–22) | 0.104 |
| I do not believe the effect of the vaccine lasts long enough | 9 (4–14) | 6 (1–11) | 0.402 |
| The vaccine is important to prevent women needing operations to avoid cervical cancer | 58 (49–67) | 72 (63–81) | 0.033 |
| I do not think HPV or cervical cancer is such a big problem that we need the HPV vaccine | 11 (5–17) | 6 (1–11) | 0.219 |
| The vaccine is important to prevent the development of cervical cancer | 79 (72–86) | 96 (92–100) | <0.000 |
| The screening programme for cervical cancer is so good that the HPV vaccine is unnecessary | 12 (6–18) | 2 (0–5) | 0.008c |
| Cervical cancer is a public health problem | 40 (31–49) | 56 (46–66) | 0.019 |
| Precancerous lesions is a public health problem | 50 (41–59) | 67 (58–76) | 0.015 |
| The vaccine is important for preventing genital warts | 31 (23–39) | 75 (66–84) | <0.000 |
One year after the inclusion of the HPV vaccine in the childhood vaccination programme.
Significant differences between GPs and PHN in bold, p value based on Chi square test and.
Fisher’s Exact Test.
Used as independent variables in logistic regression model(s).
Table 2.
Knowledge of HPV infection, vaccine and cervical cancer among GPs and public health nurses in Northern Norway: Proportions (%) giving correct answer to each question (95% CI).a
| GPs (n = 121) % | Public healthnurses (n= 99) % | pb | Correct answer | |
|---|---|---|---|---|
| What percentage of cervical cancer is caused by HPV?d | 55 (45–65) | 37 (28–46) | 0.008 | 100%c |
| What is the lifetime risk of a sexually active person getting HPV infectiond | 26 (17–35) | 35 (27–44) | 0.117 | 70% |
| What percentage of cervical cancer do the genotypes HPV16 and 18 cause?d | 44 (35–53) | 58 (48–68) | 0.042 | 70% |
| How many cases of cervical cancer do you think we have in Norway per year? | 43 (33–53) | 64 (56–73) | 0.002 | 300 |
| How many operations for precancerous lesions are performed in Norway per year? | 32 (23–39) | 56 (46–66) | <0.000 | 3000 |
| Which vaccine was chosen for the programme in Norway? | 33 (25–41) | 86 (79–93) | <0.000 | 4-valent, against genotypes 6, 11, 16 and 18 |
| What is the price of one dose of this vaccine? | 41 (32–50) | 68 (59–77) | <0.000 | NOK 1200 |
One year after the introduction of the HPV vaccine in the vaccination programme.
Significant differences between GPs and PHN in bold, p value based on the Chi square test.
90–100% accepted as correct answer.
Used as independent variables in logistic regression model(s).
Table 4.
Information sources on the HPV-vaccine used by public health nurses (PHN) and GPs in Northern Norway in proportions (%) and 95% CI.a
| GPs (n = 121) % | Public health nurses (n = 99) % | pb | |
|---|---|---|---|
| NIPH Booklet (ref. [26]) | 30 (22–38) | 98 (95–100) | 0.000 |
| NIPH Rapport (ref. [10)) | 30 (22–38) | 85 (79–91) | 0.000 |
| NIPH webside | 33 (25–41) | 90 (84–96) | 0.000 |
| Nationwide courses before initiation of vaccination programme | 3 (0–6) | 63 (53–73) | 0.000c |
| Pharmaceutical Industry, information brochuresd | 50 (41–59) | 88 (82–94) | 0.000 |
| Pharma courses | 6 (2–10) | 19 (11–27) | 0.002 |
| Pharma evening meetings | 22 (15–29) | 22 (14–30) | 0.896 |
One year after the inclusion of the HPV vaccine in the childhood vaccination programme.
Significant differences between GPs and PHN in bold, p value based on Chi square test.
Fisher’s Exact Test.
Information brochures on HPV vaccine sent by post to all public health nurses and GPs from pharmaceutical industry.
We were primarily interested in identifying associations between a positive attitude towards the HPV vaccine and possible correlates. A willingness to vaccinate your own (tentative) 12-year-old daughter, interpreted as a positive attitude to HPV-vaccination, was selected as the dependent variable in the logistic regression analyses. The pre-coded responses were coded as ‘yes’ (1) and ‘no/don’t know’ as zero (0): 12.7% answered ‘don’t know’, 18.2% of GPs and 6.1% of PHNs. In the logistic regression analyses, the GPs and PHNs were collapsed into one group of PHC personnel.
Three items on self-reported knowledge (Table 1) were included as independent variables. The selection of other independent variables was done ‘a priori’, based on what the team considered the most relevant knowledge, and the most important attitudes reflecting the public debate, i.e. the three first questions in Table 2, and the four first questions in Table 3. All the four independent attitude variables were based on ‘negative statements’, i.e. ‘concerned/unsure/worried’ regarding the HPV vaccine. Responses agreeing with the negative statements (values 4–5) and ‘don’t know’ responses were coded as zero (0), while responses that disagreed/were indifferent with the negative attitudes towards the vaccine (values 1–3) were coded as one (1). The other independent variables on self-reported knowledge (Table 1) were coded in the same way; low self-reported knowledge (values 1–2) and ‘don’t know’ as zero (0), and high/middle self-reported knowledge (values 3–5) as one (1) . The exact knowledge answers (Table 2) kept the same coding as before, i.e. ‘true’ vs. ‘false/don’t know’.
Differences between GPs and PHNs were tested by the chi-square test and Fishers Exact Test (when applicable), and 95% confidence intervals (CI) for proportions are provided. All variables with a bivariate significant correlation with the dependent variable were included in the multivariate analysis (Table 4).
SPSS version 19 was used for data processing and analyses.
Results
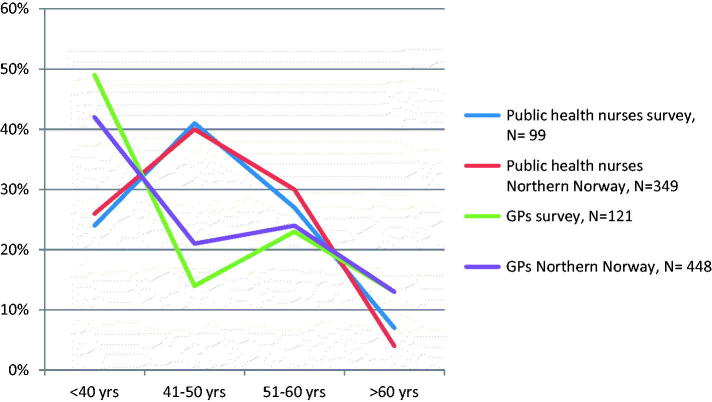
The overall response rate was 31% (220/709): 33% (99/299) for PHNs and 30% (121/410) for GPs. Eight nurses and 38 doctors replied that they could not access the form, had left their job or were on leave and therefore unavailable. No significant differences were found in age distribution between the respondents and all GPs and PHNs in Northern Norway (Figure 1). 55(46–64)% of the doctors were GP specialists, compared to 49(44–54)% of all GPs in Northern Norway, while 49(42–58)% were women, compared to 42(37–47)% of the GPs in the region .
Figure 1.
Age distribution of respondents (%) compared with all the nurses and GPs in Northern Norway.
Knowledge and attitudes among GPs and PHNs
PHNs had higher self-reported knowledge of the HPV infection, the extent of cervical cancer and HPV vaccination than GPs (Table 1). GPs were more knowledgeable of the causal relationship between HPV and cervical cancer than PHN, however, in both groups the knowledge was relatively low. PHNs knew more about HPV infection, cervical cancer and the vaccine than GPs on five of seven knowledge questions (Table 2). Self-reported knowledge was considerably higher than actual knowledge among both professionals (Tables 1 and 2). Attitudes among GPs and PHNs concerning HPV infection, cervical cancer and the HPV vaccine are presented in Table 3. More PHNs than GPs believed that the HPV vaccine was important in preventing genital warts and the development of cervical cancer. However, on all the 12 attitude questions, GPs were more worried than PHNs about the HPV vaccine’s possible negative effects, and less optimistic about its potential benefits, although only significantly on half of the questions.
None PHNs and 2(0–5)% GPs worried that HPV-vaccination would cause earlier sex debut, while 3(0–6)% PHNs and 4(1–8)% GPs worried about more unprotected sex (data not shown).
Information sources used by PHC personnel
PHNs and GPs used available information sources on HPV vaccine differently (Table 4). PHNs overwhelmingly acquired knowledge about the HPV vaccine from the NIPH [26, 10], compared to one third or less of GPs. GPs acquired knowledge mainly from the magazine Dagens Medisin, 80 (73–87) %, the Journal of the Norwegian Medical Association, 79 (72–86) % and the Norwegian Electronic Medical Handbook NEL, 50 (41–59) %. While nearly two thirds of PHNs attended the nationwide courses before initiation of vaccination programme, few GPs did so. Nearly nine of ten PHNs compared to half of the GP used information material provided by the pharmaceutical industry. Few GPs compared to one fifth of PHCN attended courses, while one fifth of both groups participated in evening meetings arranged by the pharmaceutical industry
If you had a daughter, would you vaccinate her?
If they had a 12-year-old daughter, 92(87–97) % of PHNs and 68(60–79) % of GPs would vaccinate her (p = 0.000). The relationship between willingness to vaccinate one’s daughter and selected knowledge and attitude questions was examined by logistic regression modelling (Table 5). Both univariate and multivariate analyses show that PHNs were more positive than GPs towards vaccination, as were younger compared with older respondents. Those reporting precise knowledge on the percentage of cervical cancer caused by the genotypes HPV 16 and 18, and those least concerned about side effects and disagreement among experts were most likely to vaccinate their daughter.
Table 5.
Knowledge and attitudesa associated with willingness to HPV vaccinate their own 12-year-old daughter among 220 Northern Norwegian GPs and public health nurses.b
| Crude OR (95% CI) | Multivariate OR (95% CI) | |
|---|---|---|
| Age (in 10-year age groups) | 0.73 (0.53–0.99) | 0.62 (0.40–0.95) |
| Profession (nurses vs. GPs) | 5.40 (2.39–12.25) | 5.26 (1.74–15.94) |
| High self-reported knowledge of HPV vaccine | 2.23 (1.08–4.63) | 2.23 (0.78–6.33) |
| Correct, lifetime risk of HPV infection | 2.46 (1.08–5.60) | 2.24 (0.78–6.45) |
| Correct, percent of ca. cervix due to HPV 16/18 | 2.94 (1.45–5.88) | 2.89 (1.18–7.05) |
| Not concerned about side effects | 8.35 (3.56–19.58) | 3.61 (1.10–11.87) |
| Sure of good enough effect | 3.06 (1.49–6.31) | 2.12 (0.79–5.67) |
| Not worried re. screening popularity | 2.60 (1.78–5.28) | 1.37 (0.52–3.59) |
| Not concerned on experts disagreement | 11.95 (5.63–25.35) | 7.31 (2.73–19) |
All independent variables significantly associated with the dependent variable in crude log. regression analyses were included in the multivariate analysis and are shown in the table.
Independent variables in crude log. regression analyses included age, profession, the three self-reported variables (presented in Table 1) and three selected actual knowledge variables (top three variables in Table 2) and four selected attitude variables (top four variables in Table 3). All independent variables selected from Table 1–3 are marked in these tables withd.
Significant differences presented in bold.
95(90–100) % of the PHNs who themselves administered the HPV vaccination would vaccinate their 12-year-old daughter, as well as 80(70–90) % of GPs under 40 years. 54 (45–63) % of GPs would vaccinate an older daughter aged 13–17 years; 80 (73–87) % would recommend the vaccine for the same age-group to patients requesting information.
An association existed between the 90% of PHNs regularly viewing the NIPH website (Table 4) and willingness to vaccinate their 12-year-old daughter (p = 0.007). Such association did not exist in the one third of GPs regularly viewing the website (p = 0.712) The PHC personnel had great confidence in the NIPH, and this confidence was associated with a positive attitude to vaccination; 92(87–97) % of PHNs (p < 0.001) and 84 (77–91) % of GPs (p = 0.009).
Discussion
Self-reported and actual knowledge of HPV infection, cervical cancer and their interrelationship has improved among PHNs and GPs in Northern Norway compared with a national survey before the HPV vaccination programme started [23]. Interestingly, self-reported knowledge was much higher than actual knowledge in both professional groups, and barely half of these PHC professionals knew that HPV infection causes cervical cancer. This was, however, the only knowledge question where GPs answered correctly more often than PHNs. Attitudes to HPV vaccination among the GPs and PHNs are predominantly positive. Concern about expert disagreement and side effects are the attitudes most strongly associated with low willingness to vaccinate one’s 12-year-old daughter. While more than nine in ten PHNs wanted to vaccinate their daughter, two of three GPs shared that view.
Strengths and weaknesses of the study
The age distribution among all respondents, the proportion of women and GP specialists did not differ from GPs and PHNs in Northern Norway. We therefore consider our sample fairly representative of the PHC personnel, and thus providing trustworthy study results useful for public health authorities responsible for the Norwegian HPV prevention programmes and providers of training of PHC personnel. However, when only one third of the eligible professionals participate, selection bias cannot be ruled out. Much debate about the vaccine may have encouraged those among GPs holding a less positive view on HPV vaccination to participate. That one third of GPs did not have a clear positive attitude to vaccinate their daughter may support this view. Implementing the vaccination programme in Norway is among prioritized responsibilities of PHNs. This may have discouraged participation among PHNs who were not in favour of the vaccine, which obviously may be a very difficult position to hold for a PHN. If this is the case, such selection bias can explain some of the differences among GPs and PHNs.
One limitation of the study is the low response rate. Some GPs will always be absent from their practice for specialist training, maternity and sick leave, which also may be the case for PHNs. However, response rates of 25–50% among doctors are not uncommon [27–31], may vary in different work situations and be lower in online than postal surveys [30]. Possible causes are time pressures, lack of financial incentive, many similar requests, little feedback on findings and like ours, long questionnaires [27].
Knowledge, attitudes and related information sources among PHC professionals
Four of five GPs obtained information about the vaccine from the Journal of the Norwegian Medical Association and the Norwegian magazine Dagens Medisin. GPs’ main information sources thus were the platforms where debates and critical views on the HPV vaccine were present. The NIPH is a national expert body on vaccines. Fewer GPs than PHNs used the HPV-related numerous NIPH information sources, which is natural since PHNs carry out the vaccination programme initiated by the NIPH [10,24–26]. GPs' main task is to provide individual advice on HPV vaccination for their patients, but they also carry out the cervix cancer screening programme. Therefore, it is not out of place to expect that GPs are knowledgeable on topics related to prevention of cervix and other HPV-related cancers. An obvious barrier to uptake of information on HPV-related issues among GPs, is their low user rate of the NIPH information sources.
Even though 84% of GPs in our study had great confidence in NIPH, the minority may also have lost trust the NIPH after the influenza pandemic which coincided with the initiation of the HPV vaccination programme. Handling of the pandemic influenza outbreak put the Norwegian PHC personnel under heavy strain [32]. In Northern Norway, the district medical officers in charge of infectious disease control and doctors working in the school health services, usually also do clinical work as GPs. The capacity among GPs to acquire new knowledge on HPV vaccination, well carried out by the PHNs, may thus have been limited at programme start. GPs may also have been more attentive to attitudes held by the Norwegian College of General Practice, and the editor of the Journal of the Norwegian Medical Association calling for a postponement of the programme [21,13–17,19].
Nine out of ten PHNs used the pharmaceutical industry as a source of information, compared to half of the GPs, which indicates that the industry may have identified PHNs as an important target group for its marketing. The manufacturer of the vaccine chosen for the Norwegian programme has been criticised for its marketing methods in the US [33]. In the public debate in Denmark and in Norway, the manufactures were criticised for under-reporting the risks and over-reporting the benefits of HPV vaccination, and for hidden competing interests among high-ranking health officials and expects [4]. However, the PHNs were more knowledgeable than the GPs on nearly all issues relating to HPV vaccination. This is not surprising, because GPs are less involved in the HPV vaccination programme, if they do not work in school health services. Norwegian PHC professionals did no worry that HPV vaccination would influence sexual behaviour. A large study on sexual behaviour among HPV vaccinated and non-vaccinated young Nordic women support that view [34].
Would you vaccinate your daughter?
The percentage of GPs who would vaccinate a 12-year-old daughter (68%) was roughly equal to that of girls completing first round of vaccination (67%) [24], hence GPs would vaccinate their children like the general population. GPs and PHNs who had confidence in the NIPH, were more positive to vaccinate their daughter than those who did not share that view. A Swiss study shows that many doctors disregard the official vaccination programme for their children although complying with it for their patients [35]. This concurs with GPs being more likely to vaccinate patients than their own daughters in our study. However, GPs are more willing to vaccinate their 12-year-old daughter within the programme, than a slightly older daughter outside the programme (68% vs. 54%). Older doctors are more sceptical to the vaccine, perhaps because the issue of vaccinating one’s own daughter seems less relevant for this age group.
Comparison of knowledge and attitudes among GPs from different countries
Australian GPs had moderate knowledge of HPV infection and vaccination one year after initiation of the Australian vaccination programme for 13-year-old girls; Younger and female GPs had greater knowledge of HPV than older GPs [31]. Italian GPs reported a lack of knowledge on HPV infection and vaccination, with no difference in knowledge by age, gender, level of education or region of origin [36]. Norwegian GPs reported low to moderate knowledge, no gender difference and no greater knowledge among younger GPs. 77% of Australian GPs had no concerns about the safety of the vaccine, interpreted as being slightly more positive than Norwegian GPs, even though questions were not directly comparable. Surprisingly, GPs from Norway, Australia and Italy, have in common weak knowledge of HPV infection and vaccination. This is a challenge for public health authorities, and GPs themselves in providing individual advice to parents and patients.
Conclusions
Barely half of PHC professionals knew that HPV infection causes cervical cancer, PHNs carry out the vaccination programme and had higher actual and self-reported knowledge than GPs who mostly carry out the cervix cancer screening programme and provide individual advice to parents and patients on HPV vaccination. Contrary to half of the GPs, most PHNs acquired information from the pharmaceutical industry. Both professional groups had high confidence in NIPH. PHNs used NIPH’s numerous information source on HPV, while GPs had a low user rate, which may appear as a barrier to better knowledge among GPs. More than nine in ten PHNs wanted to vaccinate their 12-year-old daughter compared to two of three GPs. A positive attitude towards HPV vaccination was strongly associated with younger age, being a PHN, and not concerned about side effects or expert disagreement. The study results can be utilized to update curricula for medical and nurse students, and to guide postgraduate training of PHC personnel by the NIPH and the Cancer Registry of Norway.
Acknowledgements
The authors gratefully acknowledge the contribution of all participating PHNs and GPs.
Funding Statement
This work was supported by the General Practice Research Unit, UiT The Arctic University of Norway; the National Centre of Rural Medicine and the General Practice Research Committee under the Norwegian College of General Practice.
Disclosure statement
KN attended a two-day course for gynaecologists on the HPV vaccine arranged by Sanofi Pasteur MSD in autumn 2009. OJA and EK have no competing interests to declare.
Ethics
The Norwegian Social Science Data Services approved the study (no 24842) and all data were de-identified.
Notes on contributors
Karin Nilsen, GP specialist, Bodin Surgery, Bodø, Norway.
Olaf Gjerløw Aasland, Senior researcher, Institute for Studies of the Medical Profession (LEFO), Oslo, Norway.
Elise Klouman, Associated professor, Department of Community Medicine (ISM), UiT The Arctic University of Norway, Tromsø, Norway.
References
- 1.Cancer in Norway 2012 – Cancer incidence, mortality, survival and prevalence in Norway. Oslo: Cancer Registry of Norway; 2014. [Google Scholar]
- 2.Kyrgiou M, Kolioupoulos G, Martin-Hirsch P, et al. . Obstetric outcomes after conservative treatment of intraepithelial or early invasive cervical lesions: systematic review and meta-analysis. Lancet. 2006;3867:483–498. [DOI] [PubMed] [Google Scholar]
- 3.Albrechtsen S, Rasmussen S, Thoresen S, et al. . Pregnancy outcome in women before and after cervical conisation: population based cohort study. Bmj. 2008;337:a1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sander BB, Rebolj M, Valentiner-Branth P, et al. . Introduction of human papillomavirus vaccination in Nordic countries. Vaccine. 2012;30:1425–1433. [DOI] [PubMed] [Google Scholar]
- 5.Monsonego J, Cortes J, Greppe E, et al. . Benefits of vaccinating young adult women with the quadrivalent human papillomavirus (types 6, 11, 16 and 18) vaccine. Vaccine. 2010;28:8065–8072. [DOI] [PubMed] [Google Scholar]
- 6.Hawkes D, Lea CE, Berryman MJ.. Answering human papillomavirus vaccine concerns; a matter of science and time. Infect Agents Cancer. 2013;8:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Apter D, Wheeler CM, Paavonen J, et al. . Efficacy of human papillomavirus 16 and 18 (HPV-16/18) AS04-adjuvanted vaccine against cervical infection and precancer in young women: final event-driven analysis of the randomized, double-blind PATRICIA trial. Clin Vaccine Immunol. 2015;22:361–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schiller JT, Castellsagué X, Garland SM.. A review of clinical trials of human papillomavirus prophylactic vaccines. Vaccine. 2012;30:F123–F138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Should HPV vaccines be mandatory for all adolescents? Editorial Lancet. 2006;38:1212. [DOI] [PubMed] [Google Scholar]
- 10.Klouman E, Berstad AKH, Feiring B, et al. . Vaksine mot humant papillomavirus (HPV) [The human papillomavirus vaccine]. Oslo: Norwegian Institute of Public Health; 2007:9. [Google Scholar]
- 11.The Norwegian State Budget 2009: HPV-vaksine [The HPV vaccine]. Oslo: Ministry of Finance; 2008. [Google Scholar]
- 12.Guidance for the Introduction of HPV Vaccines in EU Countries European Centre for Disease Prevention and Control. Guidance Report. Stockholm, January 2008 [Google Scholar]
- 13.Haug C. Drømmevaksine eller fortsatt en drøm? [A dream vaccine or still a dream?]. Tidsskr Nor Legeforen. 2007;127:1331. [PubMed] [Google Scholar]
- 14.Haug C. Forskning og fantasi [Research and fantasy]. Tidsskr nor Legeforen 2007;127:1489. [PubMed] [Google Scholar]
- 15.Haug C. HPV-vaksinen – fortsatt viktige ubesvarte spørsmål [The HPV vaccine – still important unanswered questions]. Tidsskr nor Legeforen 2007;127:1625. [PubMed] [Google Scholar]
- 16.Haug C. Fra undring til uro. [From wonder to unease]. Tidsskr nor Legeforen. 2007;127:1763. [PubMed] [Google Scholar]
- 17.Haug C. Prioritering på papiret – og i praksis. [Priorities on paper – and in practice]. Tidsskr nor Legeforen. 2008;128:917. [PubMed] [Google Scholar]
- 18. Kvalitets-og prioriteringsrådet anbefaler HPV-vaksine. [National Council for Priority Setting in Health Care endorses HPV vaccination] Oslo; 2008. Available from: www.kunnskapssenteret.no/index.php?back =2&artikkelid=1090.
- 19.Haug CJ. Human papillomavirus vaccination – reasons for caution. N Engl J Med. 2008;359:861–862. [DOI] [PubMed] [Google Scholar]
- 20.Haug C. The risks and benefits of HPV vaccination. Jama. 2009;302:795–796. [DOI] [PubMed] [Google Scholar]
- 21. HPV vaksine - svar på forespørsel fra Sosial- og helsedirektoratet [The HPV vaccine - a response to an inquiry from The Social and Health Directorate]. Version 2. Norwegian College of General Practice; 2008.
- 22. Betenkeligheter ved innføring av HPV-vaksinen i barnevaksinasjons-programmet – Bioteknologinemnda anmoder om å utsette oppstart [Concerns about the inclusion of the HPV vaccine in the childhood vaccination programme – The Norwegian Biotechnology Advisory Board calls for the start to be postponed]. Oslo:2009.
- 23.Stålcrantz J, Brox N. Vaksine mot livmorhalskreft i barnevaksinasjonsprogrammet: Kunnskap og holdninger blant helsepersonell. [Vaccination against cervical cancer in the childhood vaccination programme: knowledge and attitudes among health care personnel] Helsesøstre 2009;2:70–73. [Google Scholar]
- 24.Årsrapport for HPV-vaksine i barnevaksinasjonsprogrammet 2012. [Annual report on the HPV vaccine in the childhood vaccination programme]. (Vol. 106717, p. 2). Oslo. [Google Scholar]
- 25. Statistikk for HPV-vaksinasjon i barnevaksinasjonsprogrammet [Statistics for HPV vaccination in the childhood vaccination programme]; 2017. Available from: https://www.fhi.no/hn/helseregistre-og-registre/sysvak/dekkningsstatistikk/
- 26.Faktahefte: Humant papillomavirus (HPV), livmorhalskreft og HPV-vaksine [Facts booklet on the human papillomavirus (HPV), cervical cancer and the HPV vaccine]. Oslo: Norwegian Institute of Public Health; 2010. [Google Scholar]
- 27.Aasland O, Falkum E.. Legekårsundersøkelsen [Survey of Norwegian doctors’ quality of life]. Tidsskr nor Laegeforen 1994;114:3054. [Google Scholar]
- 28.Fosse A. Å leve og la dø – lindrende behandling i kommunehelsetjenesten [Live and let die – palliative care in local health services]. Utposten 2011;5:32–34. [Google Scholar]
- 29.Bachmann C, Berg E, Spigset O, et al. . Benzodiazepinliknende hypnotika – holdninger og forskrivningspraksis blant allmennleger [Benzodiazepine-like hypnotics – attitudes and prescription practices among GPs]. Tidsskr nor Legeforen 2008;128:166–170. [PubMed] [Google Scholar]
- 30.Crouch S, Robinson P, Pitts M.. A comparison of general practitioner response rates to electronic and postal surveys in the setting of the National STI Prevention Program. Aust N Z J Public Health. 2011;35:187–189. [DOI] [PubMed] [Google Scholar]
- 31.Brotherton JML, Leask J, Jackson C, et al. . National survey of general practitioners’ experience of delivering the National Human Papillomavirus Vaccination Program. Sex Health. 2010;7:291–298. [DOI] [PubMed] [Google Scholar]
- 32.Rørtveit S, Hunskår S, Wensaas KA, et al. . Influensapandemien hausten 2009 i ein vestlandskommune [The influenza pandemic in a Norwegian municipality autumn 2009. Article in Norwegian] Tidsskr Nor Legeforen. 2011;131:675–679. [DOI] [PubMed] [Google Scholar]
- 33.Rothman SM, Rothman DJ.. Marketing HPV vaccine: implications for adolescent health and medical professionalism. Jama. 2009;302:781–786. [DOI] [PubMed] [Google Scholar]
- 34.Hansen BT, Kjaer SK, Arnheim-Dahlstrøm L, et al. . Human papillomavirus (HPV) vaccination and subsequent sexual behaviour: evidence from a large survey of Nordic women. Vaccine. 2014;32:4945–4953. [DOI] [PubMed] [Google Scholar]
- 35.Posfay-Barbe KM, Heininger U, Aebi C, et al. . How do physicians immunize their own children? Differences among pediatricians and nonpediatricians. Pediatrics. 2005;116:e623–e633. [DOI] [PubMed] [Google Scholar]
- 36.Signorelli C, Odone A, Pezzetti F, Spagnoli F, Visiarell F, Ferrari A, et al. (Human Papillomavirus infection and vaccination: knowledge and attitudes of Italian general practitioners). Epidemiol Prev. 2014;38:88–92. Italian. [PubMed] [Google Scholar]