Abstract
Introduction
Optimizing placement of Automated External Defibrillators (AED) can increase survival after an out-of-hospital cardiac arrest (OHCA). Using postal collection boxes (PCB) as locations for AEDs could potentially enhance accessibility and streamline maintenance. In this study, we modeled the hypothetical effects of deploying AEDs at PCB locations.
Hypothesis
We hypothesized that PCB-AEDs would increase AED coverage overall and in residential areas, and reduce the distance from OHCA to an AED.
Methods
AEDs in Pittsburgh, PA were identified by the University of Pittsburgh Resuscitation Logistics and Informatics Venture (n=747). PCB locations were obtained from the United States Postal Service (n=479). OHCA locations from 2009 to 2014 were obtained from the Pittsburgh site of the Resuscitation Outcomes Consortium. AED coverage assuming a ¼ mile radius around each AED was estimated for known AEDs, PCB-AEDs (hypothetical AED locations), and known AEDs augmented by PCB-AEDs, both overall and for residential and non-residential zones. Linear distance from each OHCA to the nearest AED was calculated and compared between the sets.
Results
The set of known AEDs augmented with PCB-AEDs covered more of the city overall (55% vs 30%), as well as greater proportions of residential (62% vs 27%) and non-residential areas (45% vs 30%). The median distance from OHCA to AED was significantly shorter when known AEDs were augmented with PCB-AEDs (0.12mi vs 0.32mi; p = 0.001).
Keywords: AED, defibrillator, cardiac arrest, map
Introduction
More than 350,000 OHCAs occur annually in the United States and survival rates are generally low, though there is indication that rates are improving over time.1 The use of automated external defibrillators (AED) and bystander-initiated cardiopulmonary resuscitation (CPR) can improve survival rates and neurological outcomes.2–3 AED accessibility and awareness of locations is not always optimal.4 AEDs are not necessarily placed uniformly and tend to be geographically clustered, potentially increasing bystander AED retrieval times and subsequent arrival times at an OHCA.5 Strategies for deploying public AEDs should ideally provide a wide and equitable coverage area while facilitating rapid access, maintenance, and location recognition.
Postal collection boxes (PCBs), or public mailboxes, are part of the infrastructure of national postal systems in the United States and elsewhere. PCBs serve as collection points for letters and small packages and can be located indoors or outdoors, as well as in in commercial zones or residential zones. PCBs are prevalent in most cities and are intended to be easily accessible and readily recognizable. Moreover, by virtue of their role in national postal systems, PCBs are part of vast, comprehensive logistics networks that include transportation and delivery systems. Taken altogether, these features suggest a potential role for PCBs as AED locations.
To our knowledge, no study has considered the utility or effects of using PCBs as public AED locations. Therefore, we conducted a preliminary study to investigate the impact of a hypothetical PCB-based AED deployment strategy in the City of Pittsburgh, Pennsylvania. We hypothesized that integrating PCB-located AEDs into an existing network of AEDs would result in greater AED coverage throughout the City, as well as shorter distances between AEDs and historical OHCA events.
Methods
This study was conducted under an existing protocol approved by the University of Pittsburgh Institutional Review Board for analysis of OHCA incidence and outcomes in the City of Pittsburgh.
AED Coverage Estimates
Locations of AEDs within the incorporated limits of the City of Pittsburgh, PA (n=747) were collected by the University of Pittsburgh’s Resuscitation Logistics and Informatics Venture (ReLIVe) and associated partner programs. Mechanisms for locating AEDs included crowdsourcing through the HeartMap Challenge6, direct contact with AED distribution programs, and active searching throughout the city by study personnel. AED locations were first recorded as street addresses and then geocoded to latitude/longitude coordinates using the publically available Quantum Geographic Information Systems (QGIS, ver. 2.12.1, QGIS Development Team) software suite. The final location data set of “known AEDs” included all AEDs located by March 20, 2017.
PCB locations (n=479) within the city limits were obtained from the United States Postal Service as street addresses and geocoded to latitude/longitude coordinates using QGIS.7 PCB locations included only public use PCBs (blue boxes), not feeder locations (green boxes) used only by mail carriers. The geocoded locations of all qualifying PCBs were taken as the location data set for the hypothetical PCB-AEDs throughout this study.
We estimated AED coverage with and without inclusion of PCB-AEDs using three different methods. In the first method we determined the percentage of census tracts containing at least one AED with and without augmentation by PCB-AEDs. This method provided a general picture of the availability of AEDs in different areas of the City, but little spatial resolution for knowing whether the AEDs would be accessible equitably to the population in each census tract when needed. In the second method we determined the proportion of the total spatial area of the City covered by known AEDs with and without augmentation by PCB-AEDs, assuming that each AED was reasonably accessible in a ¼ mile radius around its base location. This method would afford a sense of the effect of PCB locations on accessibility using a distance limitation that corresponds to approximately 3 minutes of walking time at a brisk walking pace of 5 miles per hour. In the third method, we determined the proportion of the total residential area of the city covered, with the same ¼ mile access assumption. This method was intended to understand the added value of PCB-AEDs in reaching OHCA events in residential areas, since it is known that most AEDs tend to be located in public buildings while most OHCA events tend to occur in private locations. Proportions were reported in percentages. For comparison, and to reflect geographic regions or case circumstances in which a ¼ mile radius might be infeasible, we repeated the above analyses with an alternative 1/8 mile radius assumption.
AED – OHCA Distance Estimates
Case data for all EMS-assessed OHCA from 2007–2014 were obtained from the Pittsburgh Site for Resuscitation Outcomes Consortium (n = 2765). The Resuscitation Outcomes Consortium consisted of 10 regional clinical centers conducting research on out-of-hospital cardiac arrest and major trauma from 2005–2016.8 The street address of each OHCA event was retrieved from the electronic patient care report using a custom MATLAB (The Mathworks, Natick, MA) script and geocoded into latitude/longitude coordinates with QGIS.
To assess the distance between AEDs and OHCAs during the capture period of this cohort, we restricted our known AED data set to just those AEDs that were in our database as of December 31, 2014. We then separately calculated the direct linear (“as the crow flies”) distance from each OHCA to the nearest known AED, the nearest PCB-AED, and the nearest of either, using the QGIS Hub Lines tool. Linear distance was chosen to avoid making assumptions about the probable path of responders retrieving the devices, as well as to provide an analogy to electronic bystander dispatch systems that alert volunteers to nearby cardiac arrests and AEDs, generally by linear proximity. (See Supplement for a preliminary treatment using a street distance approach.) The distance was initially calculated in arc degrees and then converted into feet. Mean (SD) distance from OHCA to AED was calculated for each set. To determine the net benefit of including PCB-AEDs, we calculated the average difference in distance from AED to OHCA using known AEDs only and known AEDs augmented by PCB-AED sets, as well as the proportion of OHCA cases with a reduced distance to AED after addition of PCB-AEDs. Distances from OHCA to AED were compared between sets with the Wilcoxon Signed-Rank test due to non-normally distributed data. An alpha level of 0.05 was used as the criterion of statistical significance, and all statistical calculations were performed in Stata 14 (StataCorp, College Station, Tx).
Results
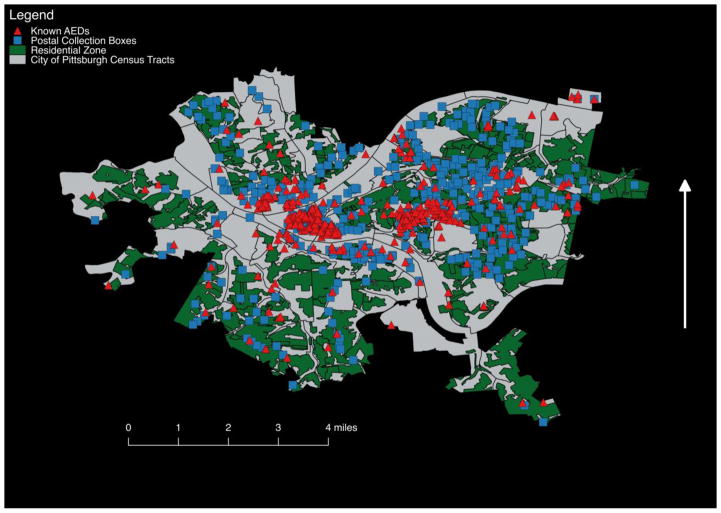
Figure 1 shows a map of the distribution of known AEDs and PCBs throughout the City of Pittsburgh, against the backdrop of residential zoning space. The City is divided into a total of 138 census tracts overlapping 90 individual neighborhoods of mixed zoning. Of the total spatial area of the City, 43% is zoned residential, where the category residential collapses several noncommercial categories that include Residential Single-Unit Detached (Very-Low Density), Residential Single-Unit Detached (Very-Low Density), Residential Two Unit (Very Low Density), Residential Single-Unit Attached (Moderate Density), Residential Three Unit Attached (Moderate Density), Residential Multi-Unit (Moderate Density), Residential Multi-Unit (High Density), and Residential Multi-Unit (Very-High Density). The remaining zoning codes were combined into a single non-residential category.
Figure 1. Spatial Distribution of Known AEDS and PCBs in the City of Pittsburgh.
AED locations are shown as red triangles. PCB locations are shown as blue squares. Residential zones are shaded in green. Abbreviations: AED – Automated External Defibrillator; PCB – Postal Collection Box.
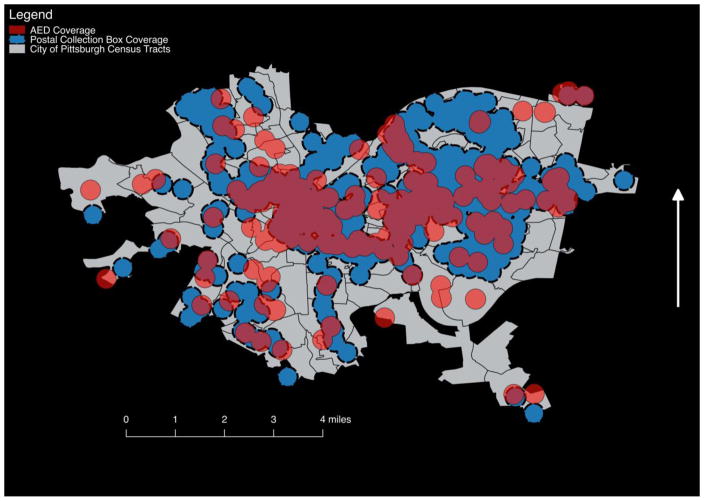
Known AEDs are present in 58% of census tracts, with a median (IQR) of 1 (0–3) AEDs per tract and a range of 0–236. PCBs are present in 71% of census tracts, with a median (IQR) of 2 (0–5) PCBs per tract and a range of 0–62. Overall, 8% of all known AEDs and 33% of PCBs fall within residential zoning areas. Assuming a ¼ mile accessibility radius, 30% of the City overall is currently covered by known AEDs, while 47% would be covered by PCB-AEDs alone and 55.44% would be covered by known AEDs augmented with PCB-AEDs. Assuming a 1/8 mile radius, these change to 12%, 21% and 27%, respectively. Of the area zoned residential throughout the City, 27% are covered by known AEDs, 53% would be covered by PCB-AEDs, and 62% would be covered by known AEDs augmented with PCB-AEDs. Under a 1/8 mile radius constraint, these change to 26%, 41% and 44%, respectively. In area zoned non-residential, 30% was covered by known AEDs and 45% was covered by known AEDs augmented by PCB-AEDs, or 15% and 25% assuming a 1/8 mile radius. Figure 2 shows a map of coverage areas by each method under the ¼ mile assumption.
Figure 2. AED Coverage Areas Using PCBs or Known AED Locations.
AED coverage area was estimated as a ¼ mile radius around each device for both known AED locations and hypothetical AEDs located at PCBs. Coverage area for known AEDs is shaded in red. Coverage area for PCB-AEDs is shaded in blue. Overlapping areas appear a darker red. Abbreviations: AED – Automated External Defibrillator; PCB – Postal Collection Box.
The median distance to OHCA was 0.32 mi (IQR=0.17–0.53) for known AEDs, 0.16 mi(IQR=0.09–0.33) for PCB-AEDs alone, and 0.12 mi(IQR=0.06–0.25) for known AEDs augmented by PCB-AEDs (AEDs vs AEDs augmented by PCB-AEDs; p < 0.001). Among all OHCAs, the distance from OHCA to AED was shorter in 57% of cases when augmenting known AEDs with PCB-AEDs.
Discussion
Our findings show that PCBs in the City of Pittsburgh offer a convenient opportunity for systematically placing AEDs to increase overall AED coverage. PCBs are distributed across the city more equitably than current known AEDs, with a 4-fold greater proportion falling in residential zoning areas and a substantial proportion affording coverage of residential areas by proximity. Residential coverage is critical to increasing access to AEDs for that majority of OHCA cases that occur in the home.1 Even so, the benefit of PCB-AEDs was not limited to residential areas, as overall coverage was increased in non-residential areas as well. Additionally, while the greatest numerical coverage benefit was seen when a ¼ mile accessibility radius was assumed around each AED, benefits were still observed with a shorter 1/8 mile radius.
Access to publically accessible AEDs is a critical and effective piece of the chain of survival. Since the early 2000s, PAD programs have successfully used systematic AED dissemination schemes, including placement in casinos, airports, and federal buildings, and a multi-center trial in 2004.9–13 Despite this, multiple studies have identified a need for better correspondence between AED placement and OHCA incidence.5,14–15 Sun et al recently conducted a comprehensive analysis of potential public locations for AEDs in the Toronto, Ontario area, finding that automated teller machines (ATMs) and coffee shops may be ideal locations for AEDs.13 The analogy between ATMs and PCBs is noteworthy. By comparison, ATMs have dedicated electronic data network access and periodic or on-demand servicing by maintenance personnel, whereas PCBs do not typically have an internet connection but do have daily visits by personnel regardless of demand load. Otherwise, both are readily recognizable, part of robust logistical networks with delivery service, and widely distributed. Importantly, the zoning distribution of ATMs and PCBs may vary. ATMs may be less common in heavily residential areas since they are likely to be clustered with commercial structures where access to cash is useful. At least in our study, a third of all PCBs were found in residentially zoned areas. In Paris, France, Dahan et al explored the potential for systematic deployment of outdoor AEDs at post offices, subway stations, bike-share stations, and pharmacies.16 Post office deployment, though not entirely analogous to PCB deployment, was calculated to afford a 324m (~0.2mi) average distance between AEDs and historical OHCA events, which was comparable to the 0.16mi OHCA to PCB-AED distance observed in our study.
Our study has several limitations. We have made several assumptions in modeling this hypothetical deployment of AEDs. Our estimates of AED coverage rely on the assumption that ¼ mile maximum distance to retrieve an AED is feasible. Assuming a brisk 5 mile per hour walking or jogging pace, this constraint creates a maximum retrieval time of 6 minutes from the boundary of the ¼ radius to the AED and back. In many areas with fast EMS response times, this time may be competitive with or longer than it takes for EMS to arrive and apply an AED. In rural areas this may be competitive, but shorter distances would be more ideal. We also estimated response distances by assuming direct linear travel, which may obscure actual response distances and times in areas where linear distance is not a good approximation for actual travel paths. Our OHCA locations included all cases, including those assessed but not treated by EMS, which may overestimate the OHCA burden and therefore underestimate the AED-to-OHCA distances. While this may be true after the fact, we think the most sound prospective plan for deploying AEDs would take into account total OHCA burden, not probability of EMS treatment. Lastly, our study assumes that deployment of AEDs at PCBs is feasible with respect to the environmental conditions accompanying outdoor placement. Storage cases do exist for placing AEDs in outdoor environments, however the specific requirements, costs and effects of accommodating outdoor conditions were not explored in this study. The possibility of theft is an important extension of this issue. Indoor AEDs in public buildings may benefit from surveillance cameras, building staff or integrated security systems as theft deterrents. PCB-AEDs would theoretically be vulnerable to theft or vandalism much as any outdoor public infrastructure is. Technological innovations may mitigate this problem to an extent, for instance by requiring a code to retrieve the AED from a secure container mounted to the PCB. However, locking AEDs could conceivably lead to reduction in accessibility during true emergencies, and it is unclear how serious the threat of theft or vandalism actually is. A study by Perbedy et al. found that among 1,716 AEDs placed publicly in the US and Canada between 2000 and 2003, a total of 20 (1.1%) devices were stolen in 17 incidents.17 The authors report that the majority of the stolen AEDs were kept in locked areas, not open and freely accessible. Further work is needed to determine the appropriate level of protections if AEDs are to be placed on PCBs.
Conclusions
Augmenting existing deployments of publicly accessible AEDs with AEDs deployed at PCB locations can increase AED spatial coverage in both residential and non-residential areas, as well as reduce the average distance from AED to OHCA.
Supplementary Material
Acknowledgments
We are grateful to the men and women of the City of Pittsburgh Bureau of EMS for their service and cooperation.
Dr. Salcido’s salary was supported during the study period by NHLBI grants (K12HL109068, R01HL117979, and R21HL135369) and grants from the Henry L. Hillman Foundation, which also supports the Resuscitation Logistics and Informatics Venture, and the Medic One Foundation.
Footnotes
Conflict of Interest Disclosure
The authors do not believe that any current or past financial relationships represent conflicts of interest with respect to the scientific or ethical integrity of this study.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Writing Group Members; Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Després JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jiménez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER, 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB American Heart Association Statistics Committee.; Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2016 Update:A Report From the American Heart Association. Circulation. 2016 Jan 26;133(4):e38–360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 2.Berdowski J, Blom MT, Bardai A, Tan HL, Tijssen JG, Koster RW. Impact of onsite or dispatched automated external defibrillator use on survival after out-of-hospital cardiac arrest. Circulation. 2011 Nov 15;124(20):2225–32. doi: 10.1161/CIRCULATIONAHA.110.015545. [DOI] [PubMed] [Google Scholar]
- 3.Kitamura T, Kiyohara K, Sakai T, Matsuyama T, Hatakeyama T, Shimamoto T, Izawa J, Fujii T, Nishiyama C, Kawamura T, Iwami T. Public-Access Defibrillation and Out-of-Hospital Cardiac Arrest in Japan. N Engl J Med. 2016 Oct 27;375(17):1649–1659. doi: 10.1056/NEJMsa1600011. [DOI] [PubMed] [Google Scholar]
- 4.Leung AC, Asch DA, Lozada KN, Saynisch OB, Asch JM, Becker N, Griffis HM, Shofer F, Hershey JC, Hill S, Branas CC, Nichol G, Becker LB, Merchant RM. Where are lifesaving automated external defibrillators located and how hard is it to find them in a large urban city? Resuscitation. 2013 Jul;84(7):910–4. doi: 10.1016/j.resuscitation.2013.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moon S, Vadeboncoeur TF, Kortuem W, Kisakye M, Karamooz M, White B, Brazil P, Spaite DW, Bobrow BJ. Analysis of out-of-hospital cardiac arrest location and public access defibrillator placement in Metropolitan Phoenix, Arizona. Resuscitation. 2015 Apr;89:43–9. doi: 10.1016/j.resuscitation.2014.10.029. [DOI] [PubMed] [Google Scholar]
- 6.Elrod JB, Merchant R, Daya M, et al. Public health surveillance of automated external defibrillators in the USA: protocol for the dynamic automated external defibrillator registry study. BMJ Open. 2017;7:e014902. doi: 10.1136/bmjopen-2016-014902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Find Locations USPS Postal. n.d Retrieved March 31, 2017, from https://tools.usps.com/go/POLocatorAction!input.action.
- 8.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, Davis D, Idris A, Stiell I Resuscitation Outcomes Consortium Investigators. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008 Sep 24;300(12):1423–31. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Caffrey SL, Willoughby PJ, Pepe PE, Becker LB. Public use of automated external defibrillators. N Engl J Med. 2002 Oct 17;347(16):1242–7. doi: 10.1056/NEJMoa020932. [DOI] [PubMed] [Google Scholar]
- 10.Valenzuela TD, Roe DJ, Nichol G, Clark LL, Spaite DW, Hardman RG. Outcomes of rapid defibrillation by security officers after cardiac arrest in casinos. N Engl J Med. 2000 Oct 26;343(17):1206–9. doi: 10.1056/NEJM200010263431701. [DOI] [PubMed] [Google Scholar]
- 11.Kilaru AS, Leffer M, Perkner J, Sawyer KF, Jolley CE, Nadkarni LD, Shofer FS, Merchant RM. Use of automated external defibrillators in US federal buildings: implementation of the Federal Occupational Health public access defibrillation program. J Occup Environ Med. 2014 Jan;56(1):86–91. doi: 10.1097/JOM.0000000000000042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hallstrom AP, Ornato JP, Weisfeldt M, Travers A, Christenson J, McBurnie MA, Zalenski R, Becker LB, Schron EB, Proschan M Public Access Defibrillation Trial Investigators. Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004 Aug 12;351(7):637–46. doi: 10.1056/NEJMoa040566. [DOI] [PubMed] [Google Scholar]
- 13.Sun CLF, Brooks SC, Morrison LJ, Chan TCY On behalf of the Rescu Epistry Investigators. Ranking Businesses and Municipal Locations by Spatiotemporal Cardiac Arrest Risk to Guide Public Defibrillator Placement. Circulation. 2017;135:1104–1119. doi: 10.1161/CIRCULATIONAHA.116.025349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yoon CG, Jeong J, Kwon IH, Lee JH. Availability and use of public access defibrillators in Busan Metropolitan City, South Korea. Springerplus. 2016 Sep 9;5(1):1524. doi: 10.1186/s40064-016-3201-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deakin CD, Shewry E, Gray HH. Public access defibrillation remains out of reach for most victims of out-of-hospital sudden cardiac arrest. Heart. 2014 Apr;100(8):619–23. doi: 10.1136/heartjnl-2013-305030. [DOI] [PubMed] [Google Scholar]
- 16.Dahan B, Jabre P, Karam N, Misslin R, Bories MC, Tafflet M, Bougouin W, Jost D, Beganton F, Beal G, Pelloux P, Marijon E, Jouven X. Optimization of automated external defibrillator deployment outdoors: An evidence-based approach. Resuscitation. 2016 Nov;108:68–74. doi: 10.1016/j.resuscitation.2016.09.010. [DOI] [PubMed] [Google Scholar]
- 17.Peberdy MA, Ottingham LV, Groh WJ, Hedges J, Terndrup TE, Pirrallo RG, Mann NC, Sehra R PAD Investigators. Adverse events associated with lay emergency response programs: the public access defibrillation trial experience. Resuscitation. 2006 Jul;70(1):59–65. doi: 10.1016/j.resuscitation.2005.10.030. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.