Abstract
Background
The use of low-molecular-weight heparin bridge therapy during warfarin interruption for elective surgery/procedures increases bleeding. Other predictors of bleeding in this setting are not well described.
Methods
BRIDGE was a randomized, double-blind, placebo-controlled trial of bridge therapy with dalteparin 100IU/kg twice daily in patients with atrial fibrillation requiring warfarin interruption. Bleeding outcomes were documented from the time of warfarin interruption until up to 37 days post-procedure. Multiple logistic regression and time-dependent hazard models were used to identify major bleeding predictors.
Results
We analyzed 1,813 patients of whom 895 received bridging and 918 received placebo. Median patient age was 72.6 years and 73.3% were male. Forty-one major bleeding events occurred at a median time of 7.0 days (interquartile range: 4.0–18.0 days) post-procedure. Bridge therapy was a baseline predictor of major bleeding (odds ratio [OR] = 2.4; 95% confidence interval [CI]: 1.2–4.8), as was a history of renal disease (OR=2.9; 95% CI: 1.4–6.0), and high bleeding risk procedures (vs. low bleeding risk procedures) (OR=2.9; 95% CI: 1.4–5.9). Perioperative aspirin use (OR=3.6; 95% CI: 1.1–11.9) and post-procedure INR >3.0 (OR=2.1; 95%CI: 1.5–3.1) were time-dependent predictors of major bleeding. Major bleeding was most common in the first 10 days compared to 11–37 days post-procedure (OR=3.5; 95% CI: 1.8–6.9).
Conclusions
In addition to bridge therapy, perioperative aspirin use, post-procedure INR >3.0, a history of renal failure, and having a high bleeding risk procedure increase the risk of major bleeding around the time of an elective surgery/procedure requiring warfarin interruption.
Trial Registration
https://clinicaltrials.gov/ct2/show/NCT00786474 (NCT00786474)
Introduction
It is estimated that 10–15% of patients taking warfarin require temporary interruption of the anticoagulant therapy for a surgery/procedure each year [1–3]. Clinical practice guidelines recommend stopping warfarin 5 days prior to most surgeries/procedures to allow for normalization of the international normalized ratio (INR) and full restoration of clotting factor activity [4]. Warfarin inactivates production of vitamin K-dependent clotting factors indirectly through inhibition of vitamin K epoxide reductase [5]. As a result, there is a delay in re-establishing a therapeutic anticoagulant effect of 5–7 days after warfarin is restarted [5], and a longer period may be required in the post-procedure setting [6, 7]. Patients with atrial fibrillation may be susceptible to potentially avoidable thromboembolic complications during this period of warfarin withdrawal and re-initiation around a surgery or invasive procedure which led to the practice of bridge therapy with low-molecular-weight heparin (LMWH) in an attempt to mitigate this risk [8].
The Bridging Anticoagulation in Patients who Require Temporary Interruption of Warfarin Therapy for an Elective Invasive Procedure or Surgery (BRIDGE) trial randomized patients with atrial fibrillation to either bridging with therapeutic-dose dalteparin or matching placebo during warfarin interruption for an elective surgery/procedure [6]. Foregoing bridging with LMWH resulted in significantly less major bleeding than bridge therapy. In addition to use of LMWH bridging, other perioperative bleeding risk factors have been previously described. General risk factors for bleeding include active bleeding or untreated bleeding disorders, previous bleeding, severe hepatic or renal failure, thrombocytopenia, acute stroke, and uncontrolled hypertension [9]. In addition, a randomized trial of heparin prophylaxis after major abdominal surgery found that male sex, malignancy, and gynecologic or complex surgical cases conferred an increased risk of postoperative bleeding [10], whereas a randomized trial of perioperative aspirin use found that continuing aspirin in the perioperative period conferred a 2-fold increased risk for major bleeding [11]. Other observational studies have evaluated risk factors for bleeding in a perioperative setting [12–14]. However, their non-random allocation of patients to perioperative heparin bridging or no bridging has the potential to affect ascertainment of bleeding risk factors because the decision to bridge or not bridge is unlikely to have been independent of the presence of other bleeding risk factors.
We accessed the BRIDGE trial data set with the aim of identifying, apart from LMWH bridging, additional potentially-modifiable predictors of perioperative bleeding in patients with atrial fibrillation who interrupted warfarin for an elective surgery/procedure.
Methods
Study Design and Oversight
The BRIDGE study was a double-blind, placebo-controlled trial that was designed by the steering committee and approved by institutional review boards at each participating center. The Duke Clinical Research Institute, Durham NC, managed the study and the clinical coordinating center was responsible for subject randomization and distribution of study drug. Additional details regarding the BRIDGE study design and oversight have been described previously [6]. Funding for this analysis was provided by a grant awarded to Drs. Ortel and Hasselblad from the National Heart, Lung, and Blood Institute. The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper and its final contents.
Patients
Eligible patients were ≥18 years of age; had chronic or paroxysmal atrial fibrillation or flutter confirmed by electrocardiography or pacemaker interrogation; had received warfarin for at least 3 months with a therapeutic INR range of 2.0–3.0; were undergoing an elective operation or other invasive procedure that required warfarin interruption; and had at least one of the following stroke risk factors: congestive heart failure or left ventricular dysfunction, hypertension, age ≥75 years, diabetes mellitus, or previous stroke, systemic embolism, or transient ischemic attack. Exclusion criteria were presence of a mechanical heart valve; stroke, systemic embolism or transient ischemic attack within the previous 12 weeks; major bleeding within the previous 6 weeks; creatinine clearance (CrCl) <30 mL/min; platelets <100 × 109/L; or planned cardiac, intracranial, or intraspinal surgery. Additional inclusion and exclusion criteria details may be found in the supplementary appendix associated with the primary publication [6].
Procedures
Eligible patients were randomly assigned to receive dalteparin sodium, 100 IU/kg subcutaneously twice-daily, or matching placebo injections. Warfarin was stopped 5 days prior to the procedure and dalteparin or placebo injections were administered beginning 3 days before the surgery/procedure, with the last dose given approximately 24 hours pre-procedure. Injections were restarted in the postoperative period either at 12–24 hours or 48–72 hours after low and high bleeding risk procedures; respectively, and continued for 5–10 days post-procedure until a therapeutic INR was re-established. Definition of procedure-related bleeding risk (major/high risk and minor/low risk) was guided by the study protocol. Low bleeding risk procedures included gastrointestinal endoscopy, cardiac catheterization, cataract removal, dental and dermatologic procedure as well as any other surgery or procedure lasting less than 1 hour. High bleeding risk procedures included major intra-abdominal surgery (e.g. bowel or visceral organ resection), major orthopedic surgery, peripheral arterial revascularization, urologic procedures, pacemaker/defibrillator insertion, biopsy of a visceral organ, polypectomy, and other procedures lasting 1 hour or greater. Final determination of bleeding risk was left to the site investigator’s discretion. Management of antiplatelet therapy was also left to the site investigator’s discretion in the perioperative period. Patient follow-up occurred at least weekly by phone with the final encounter 30–37 days post-procedure.
Study Outcomes
Major bleeding was assessed from the day of warfarin withdrawal through 37 days after the procedure and defined according to the criteria set forth by the Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis [15]. Specifically, the definition of major bleeding included: fatal bleeding; symptomatic bleeding involving a critical area or organ; non-surgical site bleeding causing a decrease in hemoglobin ≥20 g/L, or leading to transfusion of ≥2 units of whole blood or packed red cells; surgical site bleeding that requires a second intervention or hemarthrosis of sufficient size as to interfere with rehabilitation; or surgical site bleeding that is unexpected and prolonged and/or sufficiently large to cause hemodynamic instability with an associated decrease in hemoglobin ≥20 g/L.
Statistical Analysis
Patient characteristics were summarized using descriptive statistics. Categorical baseline variables were presented as frequencies or proportions. Continuous variables were presented as medians with 25th and 75th percentiles. The general methodology for the analysis of the major bleeding data from the date of the procedure through day 37 can be thought of as a Cox Proportional Hazards Model with time-dependent covariates. The actual implementation used multiple logistic regression analysis estimated by maximum likelihood methods as described by Allison [16]. Each individual's status, starting at randomization, was separated into single-day increments, and these were treated as distinct observations. This methodology allows each person to contribute risk information for each day after warfarin withdrawal until a major bleed or day 37, whichever comes first. Statistical significance was declared based on a P-value <0.05.
Characteristics included for the bleeding analysis were identified from previously published bleeding risk models or selected due to biologic probability [10–12, 17–20]. The putative determinants of bleeding risk included in the regression model were as follows: patient age >65 years; patient sex (male or female); history of heart failure (yes or no); hypertension (yes or no); diabetes (yes or no); prior stroke or transient ischemic attack (yes or no); history of liver disease (yes or no); history of gastrointestinal hemorrhage (yes or no); history of renal disease (yes or no); perioperative aspirin use [yes (continued uninterrupted or interrupted) or no]; post-procedure INR level (1.0-point increments above 1.0); perioperative bridging therapy use (yes or no); and procedure-associated bleeding risk classification (high or low).
Results
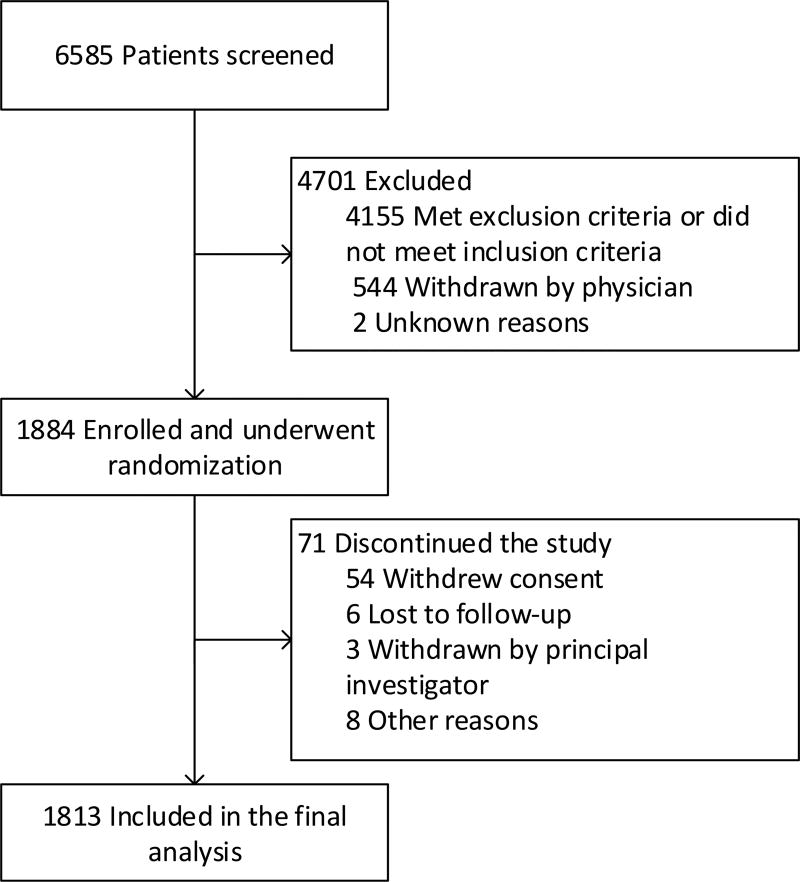
There were 1,813 patients from the BRIDGE trial included in this analysis (Figure 1). As shown in Table 1, the median patient age was 72.6 years, 73.3% were male, and the median body weight was 92.5 kg. The median CHA2DS2VASc score was 4 (range: 1–9) with 25% of patients having a CHA2DS2VASc score ≥5. Concomitant antiplatelet medications were taken in 41.2% of patients, of which the majority was aspirin. Among aspirin users, aspirin continued uninterrupted throughout the procedure in 60.5% of patients. Among the remaining aspirin users, aspirin was stopped ≥7 days pre-procedure or stopped <7 days pre-procedure in 28.2%, and 11.3% of patients, respectively. Low bleeding risk surgery/procedures made up the majority of cases representing 89.3% overall (Table 2); however, 30.1% were managed as high bleeding risk whereby the resumption of study medication (dalteparin or placebo) was delayed for 48–72 hours post-procedure.
Figure 1. Patient Dispositions.
Table 1.
Baseline Patient Characteristics
| Characteristic | Value |
|---|---|
|
| |
| Age – yr | 72.6 (65.7, 78.0) |
|
| |
| Male sexa | 1329 (73.3) |
|
| |
| Weight – kg | 92.5 (79.6, 108.9) |
|
| |
| CHA2DS2VASc scoreb | 4 (3, 5) |
|
| |
| History of heart failurea | 576 (31.8) |
|
| |
| Hypertensiona | 1581 (87.2) |
|
| |
| Diabetes mellitusa | 749 (41.3) |
|
| |
| Strokea | 173 (9.5) |
|
| |
| Transient ischemic attacka | 151 (8.3) |
|
| |
| Myocardial infarctiona | 278 (15.3) |
|
| |
| Renal diseasea | 192 (10.6) |
|
| |
| Solid malignant diseasea | 115 (6.4) |
|
| |
| Medication usea | |
| Aspirin | 623 (34.4) |
| Clopidogrel | 46 (2.5) |
| Nonsteroidal anti-inflammatory drug | 57 (3.2) |
| COX-2 inhibitor | 21 (1.2) |
|
| |
| Laboratory values | |
| Hemoglobin – g/dl | 13.9 (12.8, 14.9) |
| Platelet count – platelets × 103/mm3 | 203 (170, 239) |
| Serum creatinine – mg/dL | 1.0 (0.9, 1.2) |
Continuous measures are medians (25th, 75th percentiles); COX-2 – type II cyclooxygenase
- Data presented as number (percent)
- CHA2DS2VASc is a score used to estimate stroke risk in patients with atrial fibrillation. The score ranges from 0 to 9; 1 point each is assigned for congestive heart failure, hypertension, diabetes, age 65 – 75, vascular disease, and female sex; 2 points are assigned for age > 75 and history of stroke or transient ischemic attack.
Table 2.
Surgery and Procedure Types and Bleeding Risk Categorya
| Minor/low bleeding risk (n=1519) | Number (%)b |
| Gastrointestinal | 744 (49.0) |
| Cardiothoracic | 280 (18.4) |
| Orthopedic | 100 (6.6) |
| Urologic | 84 (5.5) |
| Dermatologic | 71 (4.7) |
| General surgery | 65 (4.3) |
| Interventional radiology | 46 (3.0) |
| Opthalmologic | 45 (3.0) |
| Dental | 40 (2.6) |
| ENT (ear, nose, and throat) | 22 (1.4) |
| Vascular surgery | 12 (0.8) |
| Gynecologic | 8 (0.5) |
| Other | 2 (0.1) |
| Major/high bleeding risk (n=182) | Number (%)c |
| Orthopedic | 58 (31.9) |
| Urologic | 46 (25.3) |
| General surgery | 29 (15.9) |
| ENT (ear, nose, and throat) | 16 (8.8) |
| Gastrointestinal | 10 (5.5) |
| Vascular surgery | 8 (4.4) |
| Gynecologic | 8 (4.4) |
| Cardiothoracic | 6 (3.3) |
| Other | 1 (0.5) |
– 122 patients had missing procedure information
– Percent of those having a minor/low bleeding risk procedure
– Percent of those having a major/high bleeding risk procedure
There was a total of 41 patients who sustained a major bleeding event, 12 in the no-bridging arm (1.3%) and 29 in the bridging arm (3.2%). The median time to major bleeding was 7.0 days after surgery (interquartile range: 4 to 18 days). There were no fatal bleeding events. Major bleeding was more common during first 10 days after a surgery/procedure than during the subsequent 11–37 days post-procedure (odds ratio [OR]=3.5; 95% confidence interval [CI]: 1.8–6.9, p=0.0002). Use of dalteparin bridging was a baseline predictor of major bleeding (OR=2.4; 95% CI: 1.2–4.8, p=0.0098), as was history of renal failure (OR=2.9; 95% CI: 1.4–6.0, p=0.0060) (Table 3). In addition, perioperative use of aspirin (OR=3.6; 95% CI: 1.1–11.9, p=0.0375) and a post-procedure supratherapeutic INR >3.0 (OR=2.1; 95%CI: 1.5–3.1 p<.0001) were both significant time-dependent predictors of major bleeding.
Table 3.
Predictors of Major Bleeding
| Significant Characteristics | Odds Ratio | 95% Confidence Interval |
P-Value | |
|---|---|---|---|---|
| Perioperative aspirin continuation | 3.576 | 1.077 | 11.874 | 0.0375 |
| Postprocedure day 0 to 10a | 3.505 | 1.797 | 6.867 | 0.0002 |
| High bleeding risk procedureb | 2.861 | 1.390 | 5.890 | 0.0043 |
| History of renal disease | 2.853 | 1.351 | 6.027 | 0.0060 |
| Dalteparin bridge therapy | 2.443 | 1.240 | 4.813 | 0.0098 |
| INR > 3 (per unit) | 2.115 | 1.466 | 3.052 | <.0001 |
| Nonsignificant Characteristics | ||||
| History of liver disease | 1.743 | 0.387 | 7.852 | 0.4691 |
| History of heart failure | 1.538 | 0.806 | 2.935 | 0.1915 |
| History of gastrointestinal bleeding | 1.449 | 0.466 | 4.509 | 0.5221 |
| History of stroke or TIA | 1.444 | 0.676 | 3.087 | 0.3425 |
| Age > 65 years | 1.353 | 0.593 | 3.089 | 0.4728 |
| History of hypertension | 1.320 | 0.465 | 3.752 | 0.6019 |
| History of diabetes | 1.063 | 0.560 | 2.019 | 0.8513 |
| Female sexc | 0.946 | 0.460 | 1.946 | 0.8805 |
C-index = 0.655
– Referent group is days 11 through 37;
– Referent group is low bleeding risk procedures;
–Referent group is male sex
INR - international normalized ratio; TIA – transient ischemic attack
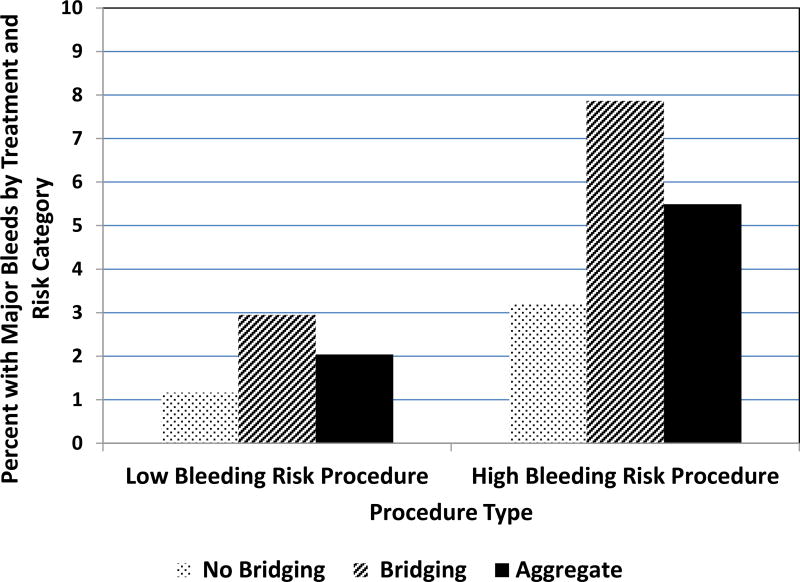
Patients having high bleeding risk surgery/procedures were at greater risk of major bleeding than those having low bleeding risk procedures (OR=2.9; 95% CI: 1.4–5.9, p=0.0043) (Figure 2). Relative to the no-bridging arm, the absolute risk for major bleeding associated with bridge therapy was numerically in high bleeding risk surgery/procedures where there the absolute risk was increased 4.6% compared to 1.8% in low risk surgery/procedures. However, the test for an interaction between bridge therapy and procedure bleeding type resulted in a chi-square of 0.0665, p = 0.7965, indicating no evidence of an interaction.
Figure 2. Major Bleeding by Bridge Therapy and Procedure Bleeding Risk Category.
Absolute risk of major bleeding within 37 days of low bleeding risk surgery/procedures was 1.2% and 2.9% in the placebo and dalteparin arms, respectively. Absolute risk of major bleeding within 37 days of high bleeding risk surgery/procedures was 3.2% and 7.9% in the placebo and dalteparin arms, respectively. The aggregate column is the overall bleeding rate (bridging and no bridging) for low and high bleeding risk groups which were 2.0% and 5.5%, respectively (OR=2.9; 95% CI: 1.4–5.9, p=0.0043).
Discussion
In patients from the BRIDGE trial with atrial fibrillation who interrupted warfarin for an elective surgery/procedure, major bleeding was more common after a high bleeding risk surgery/procedure and most frequently occurred during the first 10 days post-procedure. In addition to bridging therapy, we found patients with a history of renal failure and those taking aspirin were at greater risk for major bleeding. Finally, supratherapeutic INR values postoperatively were also associated with major bleeding.
The predictors of major bleeding identified in this analysis are biologically plausible (high bleeding risk procedures, aspirin use, elevated INR) or are markers of patient comorbidity (renal failure). In their retrospective evaluation of 2484 invasive procedures in patients with a variety of warfarin indications, Tafur and colleagues similarly identified use of low-molecular weight heparin bridge therapy as a risk factor for perioperative major bleeding [12]. In addition, presence of a mitral mechanical heart valve, history of bleeding, and active malignancy were independent predictors of major bleeding, but not use of aspirin [12]. High bleeding risk procedures and thrombocytopenia (platelets < 150,000 × 109/L) were associated with major bleeding in the bridge therapy group, but not the total population. The BRIDGE trial did not include patients with mechanical heart valves or thrombocytopenia, so these characteristics were not evaluated in the present analysis. Although history of gastrointestinal bleeding did not significantly predict major bleeding in BRIDGE, the OR=1.449 was directionally consistent with the risk identified in the Tafur analysis (Hazard Ratio=2.6, 95% CI 1.5–4.5) [12].
Of the calculators developed for estimating bleeding risk during anticoagulation in patients with atrial fibrillation, only the HAS-BLED score has been specifically assessed in the perioperative setting [13, 17–20]. A prospective registry of 1,000 patients on vitamin K antagonist therapy who required treatment interruption for an elective surgery/procedure and received various heparin bridging regimens found a HAS-BLED score ≥3 was predictive of perioperative clinically-relevant bleeding (hazard ratio=11.8; 95% CI: 5.6–24.9). This study is important as it increased awareness regarding the need for perioperative bleeding risk assessment. However, the study was not able to described predictors of major bleeding as only one major bleeding event was identified [13]. In addition, the HAS-BLED score does not account for the bleeding risk associated with the procedure. Our analysis found that having a high bleeding risk procedure was one of the strongest predictors of perioperative major bleeding.
This analysis of the BRIDGE trial data set has several strengths compared to previous studies. Patient characteristics were determined in a standardized manner at the time of study enrollment. Major bleeding outcomes were validated by an independent adjudication committee based on standardized, objective criteria. Unlike the HAS-BLED analysis which included lower doses of low-molecular weight heparin [13], BRIDGE provided therapeutic low-molecular weight heparin doses in randomized, double-blind fashion.
There are also potential limitations of the present study. The BRIDGE trial excluded patients with significant bleeding risk factors such as severe renal insufficiency (CrCl <30 mL/min), severe hepatic insufficiency, thrombocytopenia and recent (within 3 months) gastrointestinal bleeding. However, such factors would be less relevant for the perioperative management of warfarin-treated patients since such patients (with severe hepatic insufficiency, thrombocytopenia, recent bleeding) would not typically be eligible to receive anticoagulant therapy. Precise information regarding the timing of perioperative aspirin interruption and resumption was not available and, consequently, it is possible that the magnitude of the associated increased bleeding risk with aspirin continuation might be affected depending on when aspirin was stopped and resumed. However, our findings are consistent with observational studies [21] and randomized trial findings [11] indicating that perioperative use of aspirin within 7 days of an elective surgery/procedure increases bleeding risk. Although the 41 major bleeding events identified in our analysis represents the largest prospectively identified sample to date, larger registries with greater power are likely required to definitively identify less common patient characteristics that predict bleeding in the perioperative setting. In addition, our analysis included 12 predictors compared to 41 major bleeding events which is an event per variable ratio of 3.4. Event per variable ratios < 5 are vulnerable to type I error and bias away from the null hypothesis [22]. Our findings should be interpreted with caution as a low event per variable ratio increases the risk of falsely identifying predictors or overestimating their respective importance [22].
The clinical implications of our findings should be considered within the context of related studies and according to whether risk factors for bleeding are modifiable. Thus, perioperative avoidance of aspirin is both a modifiable risk factor for bleeding and has been consistently found to increase perioperative bleeding risk by 1.5- to 2-fold [11, 21,23]. On the other hand, the absolute increased risk for major bleeding of ~1% with perioperative continuation of aspirin appears modest [11], and its continuation may be reasonable in selected high-risk patients such as those with a recently-implanted coronary stent, at least until additional studies better inform this management issue. Our finding that the surgeries/procedures classified as high bleeding risk in BRIDGE were, indeed, associated with a 2- to 3-fold increased risk for bleeding appears to validate this classification scheme, which was empirically derived prior to the BRIDGE trial, and may help alert clinicians to patients in whom perioperative anticoagulants should be administered cautiously. Additional studies are needed to further refine and validate classification of bleeding risk for a surgery/procedure.
In summary, we found that among patients with atrial fibrillation who required warfarin interruption for an elective surgery/procedure, perioperative aspirin use, post-procedure INR >3.0, a history of renal failure, and undergoing a high bleeding risk surgery/procedure increase the risk of perioperative major bleeding.
Supplementary Material
Acknowledgments
Drs. Clark, Douketis, Schulman, Hasselblad and Ortel designed the research. Dr. Hasselblad performed the statistical analysis. Dr. Clark drafted the manuscript. Drs. Douketis, Schulman, Hasselblad, Kindzelski, and Ortel interpreted the analysis and revised the manuscript. Dr. Ortel had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Supported by grants from the National Heart, Lung, and Blood Institute for clinical coordinating center (U01HL087229, to Dr. Ortel) and for the data coordinating center (U01HL086755) to Dr. Hasselblad. Eisai supplied the active drug, dalteparin sodium (Fragmin), through an unrestricted investigator-initiated grant to Dr. Ortel.
Dr. Douketis reports receiving fees for serving on advisory boards from Biotie, Portola, and the Medicines Company, honoraria from Bristol-Myers Squibb, Pfizer, and Sanofi Aventis, consulting fees from Boehringer Ingelheim, Bayer, Janssen, Bristol-Myers Squibb, Daiichi-Sankyo, and Actelio, and grant support from Boehringer Ingelheim. Dr. Ortel received consulting fees from Instrumentation Laboratory, CSL Behring, and Daiichi-Sankyo, and grant support from instrumentation Laboratory.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No other potential conflict of interest relevant to this article was reported.
References
- 1.Healey JS, et al. Periprocedural Bleeding and Thromboembolic Events With Dabigatran Compared With Warfarin: Results From the Randomized Evaluation of Long-Term Anticoagulation Therapy (RE-LY) Randomized Trial. Circulation. 2012;126(3):343–348. doi: 10.1161/CIRCULATIONAHA.111.090464. [DOI] [PubMed] [Google Scholar]
- 2.Sherwood MW, et al. Outcomes of temporary interruption of rivaroxaban compared with warfarin in patients with nonvalvular atrial fibrillation: results from the rivaroxaban once daily, oral, direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation (ROCKET AF) Circulation. 2014;129(18):1850–9. doi: 10.1161/CIRCULATIONAHA.113.005754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garcia D, et al. Management and clinical outcomes in patients treated with apixaban vs warfarin undergoing procedures. Blood. 2014;124(25):3692–8. doi: 10.1182/blood-2014-08-595496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Douketis JD, et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed. American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e326S–50S. doi: 10.1378/chest.11-2298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ageno W, et al. Oral anticoagulant therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed. American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e44S–88S. doi: 10.1378/chest.11-2292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Douketis JD, et al. Perioperative Bridging Anticoagulation in Patients with Atrial Fibrillation. N Engl J Med. 2015;373(9):823–33. doi: 10.1056/NEJMoa1501035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Halbritter KM, et al. Bridging anticoagulation for patients on long-term vitamin-K-antagonists. A prospective 1 year registry of 311 episodes. J Thromb Haemost. 2005;3(12):2823–5. doi: 10.1111/j.1538-7836.2005.01674.x. [DOI] [PubMed] [Google Scholar]
- 8.Douketis JD. Perioperative management of warfarin therapy: to bridge or not to bridge, that is the question. Mayo Clin Proc. 2008;83(6):628–9. doi: 10.4065/83.6.628. [DOI] [PubMed] [Google Scholar]
- 9.Gould MK, et al. Prevention of VTE in nonorthopedic surgical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed. American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e227S–77S. doi: 10.1378/chest.11-2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cohen AT, Wagner MB, Mohamed MS. Risk factors for bleeding in major abdominal surgery using heparin thromboprophylaxis. Am J Surg. 1997;174(1):1–5. doi: 10.1016/S0002-9610(97)00050-0. [DOI] [PubMed] [Google Scholar]
- 11.Devereaux PJ, et al. Aspirin in patients undergoing noncardiac surgery. N Engl J Med. 2014;370(16):1494–503. doi: 10.1056/NEJMoa1401105. [DOI] [PubMed] [Google Scholar]
- 12.Tafur AJ, et al. Predictors of major bleeding in peri-procedural anticoagulation management. J Thromb Haemost. 2012;10(2):261–7. doi: 10.1111/j.1538-7836.2011.04572.x. [DOI] [PubMed] [Google Scholar]
- 13.Omran H, et al. The HAS-BLED score predicts bleedings during bridging of chronic oral anticoagulation. Results from the national multicentre BNK Online bRiDging REgistRy (BORDER) Thromb Haemost. 2012;108(1):65–73. doi: 10.1160/TH11-12-0827. [DOI] [PubMed] [Google Scholar]
- 14.Hammerstingl C, et al. Bridging of chronic oral anticoagulation with enoxaparin in patients with atrial fibrillation: results from the prospective BRAVE registry. Cardiovasc Ther. 2009;27(4):230–8. doi: 10.1111/j.1755-5922.2009.00099.x. [DOI] [PubMed] [Google Scholar]
- 15.Schulman S, et al. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in surgical patients. J Thromb Haemost. 2010;8(1):202–4. doi: 10.1111/j.1538-7836.2009.03678.x. [DOI] [PubMed] [Google Scholar]
- 16.Allison PD. Survival Analysis using the SAS® System: A practical guide. Cary, North Carolina: SAS Institute; 1995. [Google Scholar]
- 17.Pisters R, et al. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138(5):1093–100. doi: 10.1378/chest.10-0134. [DOI] [PubMed] [Google Scholar]
- 18.Fang MC, et al. A new risk scheme to predict warfarin-associated hemorrhage: The ATRIA (Anticoagulation and Risk Factors in Atrial Fibrillation) Study. J Am Coll Cardiol. 2011;58(4):395–401. doi: 10.1016/j.jacc.2011.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gage BF, et al. Clinical classification schemes for predicting hemorrhage: results from the National Registry of Atrial Fibrillation (NRAF) Am Heart J. 2006;151(3):713–9. doi: 10.1016/j.ahj.2005.04.017. [DOI] [PubMed] [Google Scholar]
- 20.O'Brien EC, et al. The ORBIT bleeding score: a simple bedside score to assess bleeding risk in atrial fibrillation. Eur Heart J. 2015;36(46):3258–64. doi: 10.1093/eurheartj/ehv476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Burger W, et al. Low-dose aspirin for secondary cardiovascular prevention - cardiovascular risks after its perioperative withdrawal versus bleeding risks with its continuation - review and meta-analysis.[see comment] Journal of Internal Medicine. 2005;257(5):399–414. doi: 10.1111/j.1365-2796.2005.01477.x. [DOI] [PubMed] [Google Scholar]
- 22.Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol. 2007;165:710–8. doi: 10.1093/aje/kwk052. [DOI] [PubMed] [Google Scholar]
- 23.anonymous. Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: Pulmonary Embolism Prevention (PEP) trial.[see comment] Lancet. 2000;355(9212):1295–302. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.