Abstract
Sternal Wound Infections (SWI) represent a dangerous complication after cardiac surgery entailing significantly longer hospital stays and worse short-term survival, especially in case of deep infections (DSWI) with the onset of osteomielitis or mediastinitis. The real incidence of SWI can be estimated between 0.25% and 10%; among the risk factors for sternal dehiscences after a longitudinal median sternotomy, several experiences underline the role of diabetes as an independent risk factor for post-operative infections, especially in patients affected by COPD with higher BMI. The application of a negative-pressure therapy, through instill modality too, assures a wound cleansing through periodic irrigation of topical solutions with particulate secretion removal; moreover it improves the granulation process owing to the increased blood flow and makes the size wound reduction easier, representing very often the treatment of first-line in DSWI and an optimal bridge for another reconstructive procedure of the sternal defect. The following case report shows how a plastic surgical approach associated to the adoption of a VAC-therapy instill after specific antibiotic-therapy has integrated and optimized the trend of a very complex clinical circumstance.
Keywords: Deep sternal wound infections, Mediastinitis, Vacuum-assisted closure therapy, Skin grafting
Introduction
Sternal Wound Infections (SWI) represent a dangerous complication after cardiac surgery entailing significantly longer hospital stays and worse short-term survival, especially in case of deep infections (DSWI) with the onset of osteomielitis or mediastinitis. In the literature, the real incidence of SWI1 is estimated between 0.25% and 10%, while we can gain an insight into the prognostic impact of mediastinitis thinking about the high mortality rate between 14–47% related to this complication, that usually presents an incidence between 1–2.4%. Hereafter we describe a case in which a plastic surgical approach associated to the adoption of a VAC-therapy instill after specific antibiotic-therapy has integrated and optimized the trend of a very complex clinical circumstance.
Case report
A 65-year old female was admitted at our division to undergo coronary artery bypass grafting procedure; about her medical history, the patient suffered from essential arterial hypertension, diabetes mellitus in insulin-therapy and mild obesity. Transthoracic echocardiography revealed an ejection fraction about 50% with inferior wall and posterior septum medio-basal acynesia, whereas the coronarography pointed out a three-vessel disease with involvement of the left main coronary artery. Thus, the patient underwent CABG through LIMA-LAD and SVG-OM-PDA according to the sequential technique; after surgery our conventional broad-spectrum antibiotic prophylaxis, relied on the administration of cefotaxime, was started.
The post-operative course was characterized by an early psychomotor agitation, a severe glycemic decompensation and the presence of mild serosity at the third inferior sternal segment which was the result of likely lipolysis; in the 11th post-operative day, because of sternal diastasis with mechanical respiratory failure, the patient underwent a surgical revision according to Robicsek technique together to bilateral mobilization of major pectoralis muscles. During the following week we noticed plentiful particulate secretions with spontaneous reopening of the last segment of the surgical wound; quickly we started the Vacuum-Assisted Closure (VAC) therapy instill with a negative pressure up to −100 mmHg as adjuvant treatment, while the microbiological cultures at first isolated, as a pathogen agent, an Enterobacter sensitive to teicoplanin and tigecyclin. Probably because of an antibiotic-therapy toxicity too, the patient developed a renal failure with creatinine serum values about 5 mg/dL, nevertheless avoiding renal dialysis. Furthermore, intense asthenia, persistent fever between 37–38.5°C and humor tone disturbances appeared, reducing markedly the global compliance of the patient.
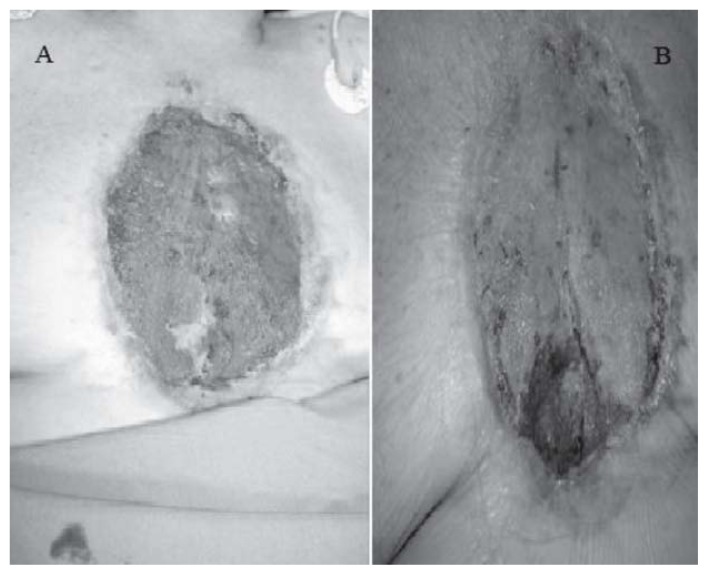
The following wound cultures showed the eradication of the Enterobacter infection, but revealed a positivity for Pseudomomas Aeruginosa, multiresistent to all antibiotics except for colistin according to the antibiogram exam. After 85 post-operative days, we had an extensive soft tissue loss with bone exposure and communication with pericardial cavity even if the wound secretions were significantly diminished; once achieved a good granulation process in the most of sternal wound, showing flat edges and a satisfactory bed (Figure 1A), plastic surgeons performed another procedure consisting in a skin grafting harvested from the right thigh, leading to partial coverage of tissue loss in order to accelerate the healing process.
Figure 1 A–B.
Sternal wound before (A) and after (B) the skin grafting.
The skin grafting showed rapidly an optimal engraftment (Figure 1B), whereas the inferior tract of wound, characterized by a persistent mild serosity, was treated with the negative-pressure therapy for about other two weeks and subsequently with advanced medications made of greasy gauzes and nanocystalline silver (Acticoat7). Therefore the patient was discharged and after a month the healing process was totally completed through a secondary intention repair (Figure 2).
Figure 2.
Healing process completed.
Discussion and conclusion
As for sternal dehiscences on infective basis, we have to distinguish between superficial infections, regarding subcutaneous tissues or skin, and deep infections (DSWI), with muscular fascia or deeper surfaces involvement in accordance with one or more criteria recognized by the US Centers for Disease Control for surgical-site infections or to the El Oakley-Wright classification system. Sternocutaneous fistulas, subcutaneous abscesses or chronic osteomyelitis, requiring another surgical procedure after the discharge without meeting the criteria for DSWI, are commonly defined late chronic sternal infections (2).
Among the risk factors for sternal dehiscences (1) after a longitudinal median sternotomy (summarized in Table 1), several experiences underline the role of diabetes as an independent risk factor for post-operative infections, especially in patients affected by COPD with higher BMI; that’s why a careful pre-operative evaluation of the glycosylated haemoglobin could allow us to identify high-risk subsets to apply further prevention measures. The same post-operative glycemic decompensation is the worst determinant of final outcome, therefore it’s essential to achieve as better as possible glycemic control, also through intravenous insulin infusion. Nowadays the concurrent use of both internal thoracic arteries (BITAs) is commonly associated to subsequent devascularization of sternum, even if a potential blood flow redistribution is possible by completing the harvesting of internal mammary artery before its bifurcation in superior epigastric and muscolophrenic branches. About the microbiological spectrum, continuous changes are standing out, so that the most common pathogens detected in DSWI are Staphylococcus Aureus and/or Coagulase-negative (CoNS), especially methicillin-resistant species, followed by Gram-negative as Pseudomonas Aeruginosa, Klesbiella Pneumoniae or Enterobacter spp. with increasing incidence and multi-drug resistance. Some new currents of thought claim the pre-operative use of statins as protective factor against the onset of a post-operative infection after CABG because of its immunomodulatory effects (3); thus, we should think about this interesting link in our daily clinical experience.
Table 1.
RISK FACTORS FOR DEEP STERNAL WOUND INFECTIONS (DSWI).
| Risk Factors for Deep Sternal Wound Infections (DSWI) |
|---|
| Age |
| Female gender |
| Obesity |
| Current smoker |
| Diabetes mellitus |
| Peripheral arterial disease |
| COPD |
| Renal failure |
| Low ejection fraction (<30%) |
| BITAs harvesting |
| Connective tissue disorders |
| Prolonged post-operative ventilation |
Treatment options of DSWI include multiple debridements of necrotic tissues, sternal resinthesys with rewiring until a total sternectomy with reconstruction through bilateral pectorals or abdominis rectus muscle flaps or an omentoplasty (4, 5), which, by laparoscopic way too, shows the benefits related to its vascularization and immunological features. Nevertheless, it should be considered as the last step in the treatment of DSWI (5). The application of a negative-pressure therapy, especially through instill modality, assures a wound cleansing through periodic irrigation of topical solutions with particulate secretion removal; moreover it improves the granulation process owing to the increased blood flow, absorbs secretions making the size wound reduction (2) easier. Nowadays this device, used since 1997 (Morykwas and others), commonly represents the first–line treatment for DSWI because of its easy reproducibility and safety without particular complications, being also an optimal bridge for another reconstructive procedure of the sternal defect (2).
As suggested from our experience, once totally eradicated the infection by guided antibiotic-therapy, the skin grafting represents a very useful option to accelerate the healing process of surgical wound in case of extensive soft tissue loss. In conclusion, a good strategy must aim to a biomechanical stability through early and aggressive strategies of surgical debridement, a complete eradication of pathogens detected and the use of a negative-pressure wound therapy till the most recommended reconstructive technique chosen for each specific clinical background.
Footnotes
Conflict of interest
The authors have no conflict of interest relevant to this publication.
References
- 1.Landes G, Harris PG, Sampalis JS, Brutus JP, Cordoba C, Ciaburro H, Bernier C, Nikolis A. Outcomes in the management of sternal dehiscence by plastic surgery: a ten-year review in one university center. Ann Plast Surg. 2007 Dec;59(6):659–66. doi: 10.1097/SAP.0b013e31803b370b. [DOI] [PubMed] [Google Scholar]
- 2.Steingrimsson S, Gottfredsson M, Gudmundsdottir I, Sjögren J, Gudbjartsson T. Negative-pressure wound therapy for deep sternal wound infections reduces the rate of surgical interventions for early re-infections. Interact Cardiovasc Thorac Surg. 2012;15:406–410. doi: 10.1093/icvts/ivs254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kayani WT, Bandeali SJ, Lee VV, Elayda M, Khan A, Nambi V, Jneid H, Alam M, Wilson JM, Huang HD, Birnbaum Y, Ballantyne CM, Virani SS. Association between statins and infections after coronary artery bypass grafting. Int J Cardiol. 2012 Oct 6; doi: 10.1016/j.ijcard.2012.09.060. [DOI] [PubMed] [Google Scholar]
- 4.Schols R, Lauwers T, Geskes G, Van der Hulst R. Deep sternal wound infection after open heart surgery: current treatment insights. A retrospective study of 36 cases. Eur J Plast Surg. 2011;34(6):487–492. doi: 10.1007/s00238-011-0573-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Brabandere K, Jacobs-Tulleneers-Thevissen D, Czapla J, La Meir M, Delvaux G, Wellens F. Negative-pressure wound therapy and laparoscopic omentoplasty for deep sternal wound infections after median sternotomy. Tex Heart Inst J. 2012;39(3):367–371. [PMC free article] [PubMed] [Google Scholar]