Abstract
We conducted a meta-analysis of neurobehavioral and neurocognitive indices of impulsivity in relation to suicidal thoughts and behaviors, as well as non-suicidal self-injury (NSSI). In our systematic review, 34 studies were identified and submitted to a random-effects meta-analysis. A small pooled effect size was observed for the association between behavioral impulsivity and NSSI (OR=1.34, p < .05). A small-to-medium pooled effect size (OR=2.23, p < .001) was found for the association between behavioral impulsivity and suicide attempts, and a medium-to-large pooled effect size was observed for this outcome in relation to cognitive impulsivity (OR=3.14, p < .01). Length of time between suicide attempt and impulsivity assessment moderated the strength of the relation between impulsivity and attempts, with a large pooled effect size (OR=5.54, p < .001) evident when the suicide attempt occurred within a month of behavioral impulsivity assessment. Studies of clinically significant NSSI temporally proximal to impulsivity assessment are needed. Longitudinal research is required to clarify the prognostic value of behavioral and cognitive impulsivity for short-term risk for self-harm.
Keywords: impulsivity, non-suicidal self-injury, suicide, suicidal ideation, suicide attempts
1. Introduction
Suicide continues to be a major public health concern. Despite increased intervention efforts to address this issue, the prevalence rate of this behavior has increased 24% over the last 15 years (Centers for Disease Control and Prevention, 2016a). In contrast, mortality rates for other leading causes of death have declined appreciably, with death from pediatric cancer, for example, down 20% over this same time period (Centers for Disease Control and Prevention, 2016b). To advance our ability effectively to prevent suicide, there is a need for a better understanding of potential processes underlying the occurrence of suicidal thoughts and behaviors.
Similarly in need of progress in this regard is non-suicidal self-injury (NSSI), defined as direct and deliberate destruction of one's own bodily tissue in the absence of suicidal intent (Nock, 2010), a clinical phenomenon of particular concern, given the current absence of empirically supported treatments for this behavior (Calati and Courtet, 2016; Ougrin et al., 2015). In addition to being a clinical concern in its own right, NSSI has recently been identified as a stronger predictor of future suicidal behaviors than is their past occurrence (Asarnow et al., 2011; Wilkinson et al., 2011). In fact, a recent meta-analysis has found NSSI to be the strongest risk factor, among all forms of self-injurious thoughts and behaviors, for suicide attempts, with a large pooled effect size observed for this relationship (Ribeiro et al., 2016). One mechanism of potential relevance to suicide and NSSI is impulsivity. It is featured in several theoretical models of these self-harm behaviors (Mann et al., 2005; Nock, 2010; van Heeringen and Mann, 2014; Van Orden et al., 2010). Furthermore, it is among the most widely studied constructs in relation to suicide (Wenzel and Beck, 2008), and has been similarly much studied in the context of NSSI (Hamza et al., 2015). Meta-analyses have recently been conducted to evaluate the strength of the association between impulsivity and suicide attempts (Anestis et al., 2014) and NSSI (Hamza et al., 2015), respectively.
Although these meta-analytic reviews offer a significant advancement in our understanding of impulsivity in relation to NSSI and suicidal behavior, important aspects of these relationships remain unaddressed. In particular, although the previous meta-analysis of impulsivity and suicide (Anestis et al., 2014) cleanly observed the important distinction between suicidal behavior and related constructs (e.g., NSSI and suicidal ideation; see Brent, 2011; Klonsky et al., 2016; Mars et al., 2014; van Heeringen et al., 2011; Wichstrøm, 2009), impulsivity, conversely, was treated as a single homogenous, unitary construct. The recent review of impulsivity and NSSI (Hamza et al., 2015) provided a methodological advancement in several ways, including by differentiating between different facets of impulsivity in commonly used self-report measures, and by conducting analyses with task-based indices of impulsivity separately from these self-report indices. Yet, this review did not distinguish between notably different facets of impulsivity indexed by the task-based measures, instead grouping them together as a single variable in analyses. Furthermore, it included only three studies employing these task-based measures, which hindered its ability accurately to characterize the strength of the relationship between associated facets of impulsivity and NSSI.
Although the approaches adopted in these reviews are consistent with self-harm research in general, in that most studies of impulsivity and self-injurious thoughts and behaviors have utilized unidimensional measures of impulsivity without a clear conceptual framework for this construct, these reviews stand in contrast with the broader impulsivity literature, and addictions research particularly, wherein impulsivity has been recognized as a multidimensional construct, with important distinctions existing between different aspects of this construct (Cyders and Coskunpinar, 2011; Hamilton et al., 2015a, 2015b; Whiteside and Lynam, 2001; Winstanley et al., 2006). Indeed, several facets of impulsivity are believed to differ in their underlying neural basis (Hamilton et al., 2015a; Winstanley et al., 2006). Several researchers have therefore stated that observing the multidimensional nature of impulsivity is essential for its potential to provide a more sensitive means for studying suicide risk (Klonsky and May, 2010; Watkins and Meyer, 2013).
Within a behavioral and cognitive neuroscience framework (Peters and Büchel, 2011; Robbins et al., 2012; Winstanley et al., 2010), impulsivity has been conceptualized as involving (i) impulsive choice (i.e., cognitive impulsivity) and (ii) impulsive action (i.e., behavioral or motor impulsivity). Cognitive impulsivity is characterized by the tendency to prefer small immediate rewards over larger delayed ones. In contrast, behavioral impulsivity refers to difficulty preventing the initiation of a behavior or stopping a behavior that has already been initiated (for thorough treatments by the International Society for Research on Impulsivity of these two forms of impulsivity, their respective underlying neural circuitry, and relevant measurement considerations, see Hamilton et al., 2015a, 2015b). Supporting the view that these two forms of impulsivity are distinct facets of the same construct, they have been found to be weakly correlated with each other (Hamilton et al., 2015a; Lane et al., 2003; Reynolds et al., 2006).
This distinction between these dimensions of impulsivity has been supported by the finding across multiple studies that they possess distinct underlying neural correlates (Hamilton et al., 2015a; van Gaalen et al., 2006a, 2006b; Whelan et al., 2012; Winstanley et al., 2006). Specifically, the orbitofrontal cortex (OFC) and basolateral amygdala (BLA) appear to be uniquely involved in cognitive impulsivity (Ouellet et al., 2015; Peters and Büchel, 2011; Winstanley et al., 2006, 2004), but not behavioral impulsivity (Bari and Robbins, 2013; Winstanley et al., 2006). Additionally, several studies have consistently found that activation of the ventral striatum and ventral medial prefrontal cortex (vmPFC) is correlated with discounting of future rewards in a commonly used paradigm for indexing cognitive impulsivity, the delay discounting task (Peters and Büchel, 2011). Moreover, studies involving lesions to the nucleus accumbens have found no measurable effect on performance on behavioral impulsivity paradigms (e.g., the stop signal task), but an appreciable decline in performance on measures of cognitive impulsivity (e.g., the delay discounting task; Winstanley et al., 2006). In contrast, the ventrolateral PFC, particularly the right inferior frontal gyrus (rIFG) has been implicated in behavioral impulsivity, with much of the supporting evidence coming from lesion and fMRI studies with tasks measuring response inhibition (Aron et al., 2003; Bari and Robbins, 2013; Winstanley et al., 2006). These forms of impulsivity, and observing the distinction between them, are therefore important insofar as they may function as distinct bio-behavioral risk factors for self-injurious thoughts and behaviors (Brent, 2009; Joiner et al., 2005; Spirito and Esposito-Smythers, 2006). Maintaining the distinction between behavioral and cognitive impulsivity is of particular value insofar as establishing their potential respective associations with self-injurious thoughts and behaviors may elucidate the underlying neural processes (e.g., the rIFG in the case of behavioral impulsivity and OFC in the case of cognitive impulsivity) relevant to these clinical outcomes.
Not only is the distinction between cognitive and behavioral impulsivity important, but so too is the conceptual distinction between task-based measures, typically used to indexed these aspects of impulsivity, and self-report measures of this construct. Self-report questionnaires are generally viewed as trait indicators of impulsivity, whereas task-based measures are more state-sensitive indices of this construct1 (Cyders and Coskunpinar, 2011; Dougherty et al., 2004a; Moeller et al., 2001). Supporting the significance of this conceptual distinction, several studies have found these trait and state-sensitive measures of impulsivity to be only modestly correlated with each other (Bagge et al., 2013; Cyders and Coskunpinar, 2012, 2011; Peters and Büchel, 2011; Reynolds et al., 2008; Wu et al., 2009), and of particular relevance to the current context, to differ notably in their relation with self-harm (Glenn and Klonsky, 2010). This state-sensitive nature of neurobehavioral and neurocognitive indicators of impulsivity makes them of particular interest in the study of self-injurious thoughts and behaviors insofar as they have potential to inform models of short-term risk, rather than general risk, for these outcomes. That is, although trait impulsivity, the predominant focus of prior meta-analyses (Anestis et al., 2014; Hamza et al., 2015), may be of relevance to determining long-term risk, state-sensitive indices of impulsivity have the potential to address the identified need for indicators of immediate risk for self-injurious thoughts and behaviors (National Action Alliance for Suicide Prevention, 2014). Furthermore, self-report measures of trait impulsivity are naturally more vulnerable to response biases (e.g., minimization in individuals disinclined to be viewed as impulsive), and given their inherently subjective nature, accurate only insofar as the respondent has insight into his or her own behavioral tendencies (Cyders and Coskunpinar, 2011; Nisbett and Wilson, 1977). For these reasons, as well, task-based measures may more accurate reflect their intended construct and thus be of greater utility in assessing risk.
Collapsing across behavioral and cognitive impulsivity and combining self-report and task-based methodologies therefore risks obscuring meaningful differences in their relation with self-injurious thoughts and behaviors. Adopting theoretically driven operationalizations of impulsivity that observe distinctions between different aspects of this construct is important for its greater potential to contribute to the empirical literature. Thus, the objective of the current meta-analysis was to build on prior reviews by evaluating impulsivity within a behavioral and cognitive neuroscience perspective in association with NSSI and suicidal thoughts and behaviors, specifically, focusing exclusively on state-sensitive neurobehavioral and neurocognitive indices of impulsivity. In this meta-analysis, behavioral and cognitive impulsivity were examined separately in association with these clinical outcomes, with the aim of characterizing the strength of these relationships across existing studies in the empirical literature.
2. Method
2.1. Search strategy and eligibility criteria
A systematic search of the literature was conducted in PsycINFO and MEDLINE to identify studies of potential relevance to the current review. The following search string was applied: (suicid* OR self-harm OR parasuicid* OR self-injur* OR mutilat*) AND (impulsiv* OR “response inhibition” OR “delay discounting” OR “delayed reward” OR “stop signal” OR “continuous performance” OR “attentional control” OR “behavioural control” OR “behavioral control” OR “go/no” OR “go no”). The search results were limited to: (i) English-language publications, (ii) journal publications, and (iii) publications since and including the year (2001) of the first study of self-injurious thoughts and behaviors (Horesh, 2001) to utilize a neurobehavioral or neurocognitive measure of impulsivity. This search strategy yielded a total of 2,590 articles, of which 1,752 were unique reports. Each unique search result was reviewed by at least two independent raters to determine eligibility. In cases where the eligibility of an article could not be ruled out based on the title and abstract, the full text was also examined. Discrepancies in coding article eligibility were rare (0.7% of unique search results) and resolved by the first author.
The study inclusion criteria were: (i) NSSI and/or any aspect of suicidal ideation or behavior (e.g., suicidal ideation [SI], suicide attempt) was assessed, with the distinction between NSSI and suicide attempts being observed in studies including at least one of these outcomes; (ii) the time frame covered by the measure of NSSI and/or suicidal ideation and behavior was consistent across all study participants; (iii) neurobehavioral or neurocognitive indices of impulsivity, consistent with conceptualizations of these constructs by the International Society for Research on Impulsivity (see Hamilton et al., 2015a, 2015b), were included; and (iv) quantitative data were presented on the association between any of these forms of impulsivity and NSSI and/or any aspect of suicidal ideation and behavior. In the case of studies where more information on the measurement of NSSI or suicidal ideation or behavior was needed to determine study eligibility, every effort was made to obtain additional details in other publications describing the measure (e.g., other publications based on the same dataset) and through direct contact with the corresponding authors.
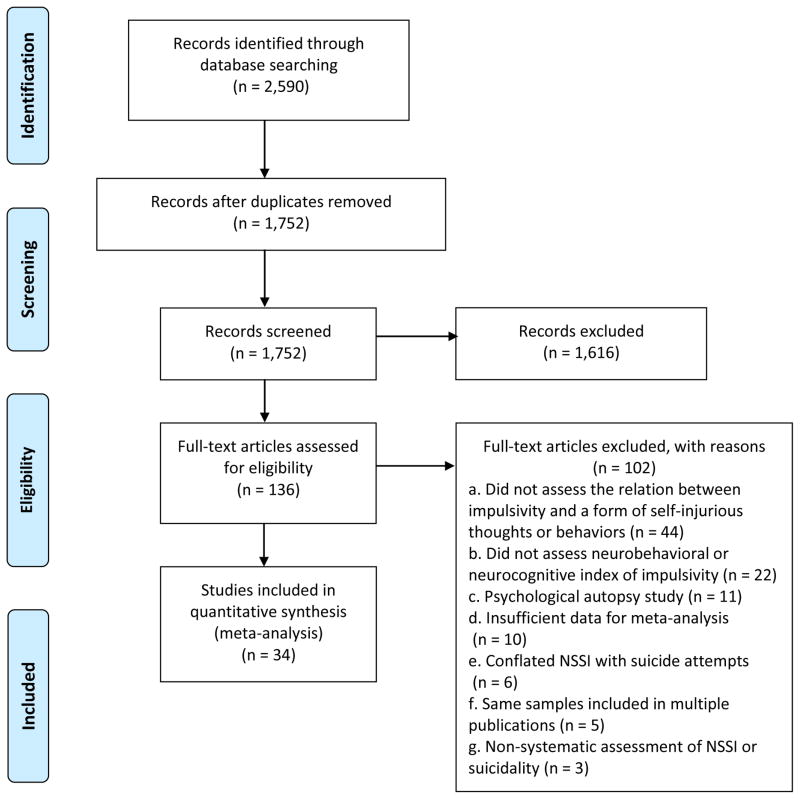
Using these inclusion criteria, we excluded 1,616 reports based on their titles and abstracts. After this initial screen, an additional 102 were excluded based on a detailed full-text review, leaving a set of 34 publications satisfying the eligibility criteria (see Figure 1 for PRISMA flow chart). Studies were excluded based on full-text review because they: (i) did not assess the relation between impulsivity and a specific form of self-injurious thoughts or behaviors (n = 44); (ii) did not include neurobehavioral or neurocognitive indices of impulsivity (n = 22); (iii) were psychological autopsy studies (n = 11); (iv) provided insufficient data for meta-analysis (n = 10)2; (v) conflated NSSI with suicide attempts (n = 6); (vi) featured a sample that overlapped with that of a study already selected for inclusion and examined the same form of impulsivity in relation to the same outcome of interest (n = 5);3 (vii) provided a non-systematic assessment of NSSI or suicidal ideation or behavior across participants (n = 3); and (viii) were a narrative review publication (n = 1).
Figure 1.
PRISMA flow chart of literature search
2.2. Data extraction
To conduct our primary analyses and to assess for potential moderators, we extracted all necessary data for computing effect size (e.g., means, standard deviations, and sample size), as well as data on nine study characteristics. Four sample characteristics were extracted: (i) sample age group (i.e., youth versus adult); (ii) mean age of sample; (iii) sample clinical status (i.e., community versus clinical or mixed); and (iv) percentage of female participants in the study sample. Data for five study design characteristics were also extracted, including: (i) form of self-injurious thoughts or behaviors (i.e., NSSI, SI, suicide attempt, impulsiveness of attempt, and severity of suicidal behavior); (ii) self-harm instrument (i.e. self-report versus interview); (iii) time-frame of self-harm assessment; (iv) cross-sectional versus longitudinal design; and (v) form of impulsivity assessed (i.e., behavioral or cognitive). As noted above, we adhered to the International Society for Research on Impulsivity’s conceptualizations of these aspects of impulsivity (Hamilton et al., 2015a, 2015b). In particular, the following paradigms, along with their variations, were included as measures of behavioral impulsivity: the go/no-go task, stop-signal task, and continuous performance test. Of the existing measures of cognitive impulsivity, only the delay discounting task has been used in studies of self-harm. These studies have been included in this review.
Among these sample and study design characteristics, the following were evaluated as potential moderators: sample age, sample clinical status, percentage of female participants in the study sample, self-harm instrument, time-frame of self-harm assessment, and cross-sectional versus longitudinal design. Of these potential moderators, several were of particular interest. First, given the conceptualization of task-based measures of impulsivity as being state-sensitive, we were especially interested in evaluating whether significantly larger effects would be observed for studies assessing impulsivity more proximally to the occurrence of self-injurious thoughts and behaviors. Additionally, the association between impulsivity, at least at the trait level, and suicidal behavior has been found to be stronger in adolescence than in early adulthood (Kasen et al., 2011; McGirr et al., 2008). We therefore evaluated whether a similar stronger effect for task-based indices of impulsivity and self-injurious thoughts and behaviors would be observed in adolescents relative to adults.
2.3. Data analysis
All analyses were conducted with Comprehensive Meta-Analysis Version 3.3.070 (Biostat, 2014). The odds ratio (OR) was used as the primary index of effect size. In cases where ORs were not reported, they were derived whenever possible from available data reported in the study (e.g., means and standard deviations, correlation). All ORs were calculated such that values greater than 1 indicated a positive association between impulsivity and self-injurious thoughts or behaviors (i.e., impulsivity is associated with greater odds of engaging in NSSI or self-injurious thoughts or behaviors). The overall weighted effect size was calculated by pooling ORs across all relevant studies. For all analyses, random-effects models were generated in preference to fixed-effects models, so as to account for the high expected heterogeneity across studies resulting from differences in samples, measures, and design. Heterogeneity across the studies was evaluated using the I2 statistic. I2 indicates the percentage of the variance in an effect estimate that is due to heterogeneity across studies rather than sampling error (i.e., chance). Low heterogeneity is indicated by I2 values of around 25%, and moderate heterogeneity by I2 values of 50%. Substantial heterogeneity that is due to real differences in study samples and methodology is indicated by an I2 value of 75%, which suggests that the observed heterogeneity is more than would be expected with random error (Higgins et al., 2003). In cases where high heterogeneity is observed, random-effects models are more appropriate than fixed-effects models in that they account for this heterogeneity by incorporating both sampling and study-level errors, with the pooled effect size representing the mean of a distribution of true effect sizes instead of a single true effect size. In contrast, fixed-effects models assume that a single true effect size exists across all studies and any variance detected is due strictly to sampling error. It thus estimates only within-study variance.
High heterogeneity is indicative of the need for moderator analyses to account for potential sources of this heterogeneity. Each potential moderator was first assessed individually, with the effect size at each level of the moderator estimated. Where possible and significance was detected for at least one moderator, these analyses were followed with a meta-regression with unrestricted maximum likelihood evaluating all moderators simultaneously. A common concern in meta-analyses is the possibility of publication bias. That is, studies with small effect sizes or non-significant findings are less likely to be published, and thus may be more likely to be excluded from meta-analyses, resulting in a potentially inflated estimate of the overall effect size. To assess for the presence of a potential publication bias, the following publication bias indices were calculated: Orwin’s fail-safe N (Orwin, 1983), Duval and Tweedie’s trim-and-fill analysis (Duval and Tweedie, 2000), and Egger’s regression intercept (Egger et al., 1997). Orwin’s fail-safe N is an index of the robustness of the overall effect, providing an estimate of how many studies with an effect size of zero would be required to reduce the overall effect size in a meta-analysis to a trivial or non-significant effect. Egger’s regression test assesses for the presence of a common form of bias, whether small studies tend to yield larger effects and are thereby biasing the results. Duval and Tweedie’s trim-and-fill analysis first generates an estimate of the number of studies likely missing due to publication bias, based on asymmetry in a funnel plot of the standard error of each study in a meta-analysis (based on the study’s sample size) against the study’s effect size, and then imputes the pooled effect size accounting for these missing studies.
3. Results
Thirty four publications assessing the relation between an aspect of impulsivity (i.e., behavioral or cognitive) and an aspect of self-injurious thoughts or behaviors were included in the meta-analysis.4 Six publications, reporting on seven studies, examined the relation between impulsivity and NSSI (Auerbach et al., 2014; Fikke et al., 2011; Glenn and Klonsky, 2010; Janis and Nock, 2009; McCloskey et al., 2012; Vega et al., 2015); four evaluated impulsivity in association with SI (Booij et al., 2006; Cáceda et al., 2014; Dombrovski et al., 2011; Westheide et al., 2008); 26 publications assessed impulsivity and suicide attempts (Brenner et al., 2015; Bridge et al., 2015; Cáceda et al., 2014; Chamberlain et al., 2013; de Moraes et al., 2013; Dombrovski et al., 2011; Dougherty et al., 2009, 2004b; Homaifar et al., 2012; Horesh, 2001; Jones et al., 2004; Keilp et al., 2014, 2008; Liu et al., 2012; Malloy-Diniz et al., 2009; Mathias et al., 2011; Nangle et al., 2006; Pan et al., 2011; Raust et al., 2007; Richard-Devantoy et al., 2012, 2011, Swann et al., 2009, 2005; Westheide et al., 2008; Wojnar et al., 2009; Wu et al., 2009); three examined impulsivity relative to impulsiveness of suicide attempt (Dombrovski et al., 2011; Vanyukov et al., 2016; Wojnar et al., 2009); and three evaluated severity of suicide attempts as an outcome (Dombrovski et al., 2011; Keilp et al., 2008; Swann et al., 2005).5 For a summary of study details, see Table 1. Although four studies employed a longitudinal design, all analyses of impulsivity and some aspect of self-harm were cross-sectional. Additionally, none of the studies featured self-report measures of suicide attempts.6 These study design considerations were therefore not included in any moderator analyses. A summary of all analyses is presented in Table 2.
Table 1.
Study characteristics
| Study Author(s) (year) | Na | % Femalea | Mean Agea | Sample | Self-Harm Measure(s) | Self-Harm Time Frame | Impulsivity Type(s) | Impulsivity Measure(s) |
|---|---|---|---|---|---|---|---|---|
| Non-Suicidal Self-Injury | ||||||||
| Auerbach et al. (2014) | 194 | 74.23 | 15.53 | Clinical | Interview (SITBI) | 1 month | Behavioral | CPT |
| Fikke et al. (2011)b | 97 | 75.26 | 14.73 | Community | Self-report (FASM) | 12 months | Behavioral | SST |
| Glenn & Klonsky (2010) | 152 | 70.85 | 19.46 | Community | Self-report (ISAS) & Interview (SSM) | Lifetime | Behavioral | SST |
| Janis & Nock (2009) Study 1 | 94 | 77.66 | 17.18 | Mixed | Interview (SITBI) | Lifetime | Behavioral | CPT |
| Janis & Nock (2009) Study 2 | 40 | 50.00 | 23.05 | Mixed | Interview (SITBI) | Lifetime | Behavioral, Cognitive | CPT, DDT |
| McCloskey et al. (2012)c | 74 | 58.23 | 36.68 | Community | Self-report (DSHI) | Lifetime | Behavioral | CPT, GNG |
| Vega et al. (2015) | 51 | 100.0 | 31.14 | Mixed | Self-report (ISAS) | Lifetime | Behavioral | SST |
| Suicide Attempts | ||||||||
| Brenner et al. (2015)e,f | 60 | 17.65 | 53.70 | Mixed | Interview (LSASII) | Lifetime | Behavioral | CPT |
| Bridge et al. (2015) | 80 | 75.00 | 15.60 | Clinical | Interview (CSHF) | 12 months | Cognitive | DDT |
| Cáceda et al. (2014)d | 82 | 56.10 | 41.30 | Mixed | Interview (C-SSRS) | 72 hours | Cognitive | DDT |
| Chamberlain et al. (2013) | 304 | 30.26 | 21.80 | Community | Interview (MINI) | Lifetime | Behavioral | SST |
| de Moraes et al. (2013) | 95 | 68.00 | 40.94 | Clinical | Interview (SSM) | Lifetime | Behavioral | CPT |
| Dombrovski et al. (2011)d | 114 | 53.51 | 68.72 | Mixed | Interview (SCID) | Lifetime | Cognitive | DDT |
| Dougherty et al. (2004)f,g | 40 | 65.00 | 29.73 | Community | Interview (LPC-2) | Lifetime | Behavioral | CPT |
| Dougherty et al. (2009) | 56 | 75.00 | 14.88 | Clinical | Interview (LPC-2) | Lifetime | Behavioral, Cognitive | SST, DDT |
| Homaifar et al. (2012)f | 47 | 6.00 | 51.20 | Mixed | Interview (CSHF) | Lifetime | Behavioral | CPT |
| Horesh (2001) | 66 | 66.66 | 15.83 | Clinical | Clinical care/intake assessment | 18 days | Behavioral | CPT |
| Jones et al. (2004)d,h | 126 | — | 35.11 | Mixed | Clinical care/intake assessment | 3 days | Behavioral | SSM |
| Keilp et al. (2008) | 244 | 55.74 | 38.00 | Mixed | Interview (CSHF) | Lifetime | Behavioral | CPT |
| Keilp et al. (2014)i | 161 | 88.82 | 43.31 | Clinical | Interview (CSHF) | Lifetime | Behavioral | CPT, GNG |
| Liu et al. (2012) | 466 | 30.30 | 42.20 | Clinical | Interview (ASI) | Lifetime | Cognitive | DDT |
| Malloy-Diniz et al. (2009) | 89 | 65.17 | 38.65 | Mixed | Interview (SSM) | Lifetime | Behavioral | CPT |
| Mathias et al. (2011) | 59 | 100.0 | 15.00 | Clinical | Interview (LHA) | Lifetime | Behavioral, Cognitive | SST, DDT |
| Nangle et al. (2006) | 78 | 25.64 | 45.91 | Clinical | Interview (SCID) | Lifetime | Behavioral | CPT |
| Pan et al. (2011) | 44 | 56.82 | 15.77 | Mixed | Interview (CSHF) | Lifetime | Behavioral | GNG |
| Raust et al. (2007) | 69 | 52.17 | 42.20 | Mixed | Interview (DIGS) | Lifetime | Behavioral | GNG |
| Richard-Devantoy et al. (2011) | 20 | 70.00 | 74.10 | Clinical | Clinical care/intake assessment | 10 days | Behavioral | GNG |
| Richard-Devantoy et al. (2012) | 60 | 61.67 | 76.30 | Mixed | Clinical care/intake assessment | 10 days | Behavioral | GNG |
| Swann et al. (2005)f | 48 | 64.58 | 35.80 | Clinical | Interview (SSM) | Lifetime | Behavioral | CPT |
| Swann et al. (2009) | 80 | 57.14 | 36.14 | Mixed | Interview (SSM) | Lifetime | Behavioral | CPT |
| Westheide et al. (2008)j | 58 | 41.38 | 38.45 | Clinical | Clinical care/intake assessment | 3 months | Behavioral | GNG |
| Wojnar et al. (2009) | 154 | 24.03 | 43.70 | Clinical | Interview (MINI) | Lifetime | Behavioral | SST |
| Wu et al. (2009)f | 38 | 62.96 | 38.43 | Clinical | Interview (CIDI) | Lifetime | Behavioral | CPT |
| Suicidal Ideation | ||||||||
| Booij et al. (2006)d | 18 | 57.89 | 43.85 | Clinical | Interview (SCID) | Lifetime | Behavioral | CPT |
| Cáceda et al. (2014)d | 62 | 54.84 | 42.87 | Mixed | Interview (C-SSRS) | 72 hours | Cognitive | DDT |
| Dombrovski et al. (2011)d | 85 | 52.94 | 69.38 | Mixed | Self-report (BSS) | Current | Cognitive | DDT |
| Westheide et al. (2008) | 29 | 41.38 | 37.46 | Clinical | Self-report (BSS) | Current | Behavioral | GNG |
| Impulsiveness of Suicide Attempt | ||||||||
| Dombrovski et al. (2011)d | 29 | 55.17 | 66.77 | Clinical | Interview (SIS: planning subscale) | Lifetime | Cognitive | DDT |
| Vanyukov et al. (2016) | 12 | 38.46 | 70.38 | Mixed | Interview (SIS: planning subscale) | Lifetime | Cognitive | DDT |
| Wojnar et al. (2009) | 66 | 22.73 | 41.48 | Clinical | Interview (MINI) | Lifetime | Behavioral | SST |
| Severity of Suicide Attempt | ||||||||
| Dombrovski et al. (2011)d | 29 | 55.17 | 66.77 | Clinical | Interview (BLS) | Lifetime | Cognitive | DDT |
| Keilp et al. (2008) | 95 | 65.26 | 36.47 | Mixed | Interview (Beck’s medical damage rating scale) | Lifetime | Behavioral | CPT |
| Swann et al. (2005)f | 22 | 66.67 | 34.83 | Clinical | Interview (SSM) | Lifetime | Behavioral | CPT |
Note: ASI = Addiction Severity Index; BLS = Beck Lethality Scale; BSS = Beck Scale for Suicide Ideation; CIDI = Composite International Diagnostic Interview; CPT = Continuous Performance Task; CSHF = Columbia Suicide History Form; C-SSRS = Columbia Suicide Severity Rating Scale; DDT = Delay Discounting Task; DIGS = Diagnostic Interview for Genetic Studies; DSHI = Deliberate Self-Harm Inventory; FASM = Functional Assessment of Self-Mutilation; GNG = Go/No-Go; ISAS = Inventory of Statements About Self-Injury; LHA = Lifetime History of Aggression; LPC-2 = Lifetime Parasuicide Count-2; LSASII = Lifetime Suicide Attempt Self-Injury Interview; MINI = Mini International Neuropsychiatric Interview; SASII = Suicide Attempt Self-Injury Interview; SCID = Structured Clinical Interview for DSM; SIS = Beck Suicide Intent Scale; SITBI = Self-Injurious Thoughts and Behaviors Interview; SSM = study-specific measure; SST = Stop Signal Task.
The number, mean age, and % female of participants included in relevant analyses, rather than of the entire study sample, are presented and were incorporated in moderator analyses whenever available.
Separate effects were reported by sex.
Data for the GNG, rather than the CPT, were included in the meta-analysis because (i) data for the former task were available for a larger number of participants, and (ii) a reward incentive was provided for performance on the GNG, potentially increasing its ecological validity.
These studies employed a longitudinal design but reported cross-sectional findings of the association between impulsivity and self-harm. In cases where this association was examined cross-sectionally at multiple time-points, baseline data were included in the meta-analysis.
This study included participants with traumatic brain injury (TBI). These participants were excluded from the meta-analysis, thereby avoiding the potential confounding effect of TBI on CPT performance.
These studies used a version of the CPT that includes the Immediate and Delayed Memory Task (IMT/DMT). Data from the IMT, rather than the DMT, were included in the meta-analysis, so as to avoid potential memory confounds on task performance.
This study reported unique effects for first-time suicide attempters and repeat attempters. As it was not possible to combine data for these two groups, data for first-time attempters were included in the meta-analysis to provide a more conservative pooled effect size estimate.
Percentage of female participants was not reported.
Data for the GNG, rather than the CPT, were included in the meta-analysis because the data reported for the CPT indexed inattention instead of impulsivity.
Sex was not reported for clinical controls but was not significantly different from that of suicide attempters. The percentage of female participants in the suicide attempter group was therefore used for the total sample in moderator analyses.
Table 2.
Meta-analytic results for behavioral and cognitive impulsivity in relation to non-suicidal self-injury and suicidality
| Behavioral impulsivity
|
Cognitive impulsivity
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| k | N | OR | 95% CI | p | k | N | OR | 95% CI | p | |
| Non-Suicidal Self-Injury | 8 | 702 | 1.34 | 1.00–1.79a | <.05 | 1 | 40 | 2.49 | .80–7.80 | .12 |
| Suicide Attempts | 22 | 1,996 | 2.23 | 1.69–2.94 | < .001 | 6 | 857 | 3.14 | 1.48–6.67 | <.01 |
| Degree of Planning in Attempt | 1 | 66 | .30 | .12–.75 | .01 | 2 | 41 | .14 | .02–.81 | <.05 |
| Severity of Attempt | 2 | 117 | 1.55 | .76–3.15 | .23 | 1 | 29 | .10 | .02–.41 | <.01 |
| Suicidal Ideation | 2 | 47 | 2.43 | .84–7.02 | .10 | 2 | 147 | 6.47 | 2.35–17.79 | < .001 |
Note: k = number of unique effects; OR = pooled odds ratio; CI = confidence interval Effect size estimates where k < 3 should be considered unstable and interpreted with a degree of caution.
The lower end of the confidence interval was rounded down but exceeded 1.00.
3.1. NSSI
Across seven studies with eight unique effects,7 behavioral impulsivity was positively associated with NSSI. The weighted mean OR was 1.34 (95% CI = 1.00–1.79),8 p < .05. Since I2 < .01%, indicating low heterogeneity, moderator analyses were not conducted. As none of the studies reported statistically significant findings, assessment of publication bias was not indicated. A reliable estimate of the strength of the association between cognitive impulsivity and NSSI was not possible as only one study (Janis and Nock, 2009) examined this relationship.
3.2. Suicide attempts
For the association between behavioral impulsivity and suicide attempts, across 22 studies, pooled OR = 2.23 (95% CI = 1.69–2.94), p < .001. Heterogeneity was moderately high (I2 = 53.47%, p < .01), indicating the appropriateness of moderator analyses. In our moderator analyses, the strength of the association between behavioral impulsivity and suicide attempts did not change as a function of the mean age of the study sample, regardless of whether mean age was treated as a categorical (p = .47) or continuous variable (b = .01, p = .21). This association was also not moderated by the percentage of female participants in each study (b < .01, p = .37). Time-frame of suicide attempt assessment was a significant moderator (p =.001), with attempts occurring within a month prior to behavioral impulsivity assessment being associated with a stronger effect (OR = 5.54 [95% CI = 2.99–10.26], p < .001) than were attempts occurring at any point within the lifetime (OR = 1.78 [95% CI = 1.42–2.23], p < .001). In a meta-regression analysis, past-month suicide attempts remained more strongly associated with behavioral impulsivity than did lifetime attempts (b = 1.03, p < .001), whereas the strength of association between behavioral impulsivity and suicide attempts did not vary as function of age (b < .01, p = .43) and percentage of female participants in the sample (b < .01, p = .43).9 Separate analyses were conducted with suicide attempters compared to clinical controls and healthy controls, respectively. When suicide attempters were compared to clinical controls, the pooled OR was 1.70 (95% CI = 1.34–2.15), p < .001. In contrast, when suicide attempters were compared to healthy controls, the pooled OR was 4.05 (95% CI = 1.93–8.49), p < .001.
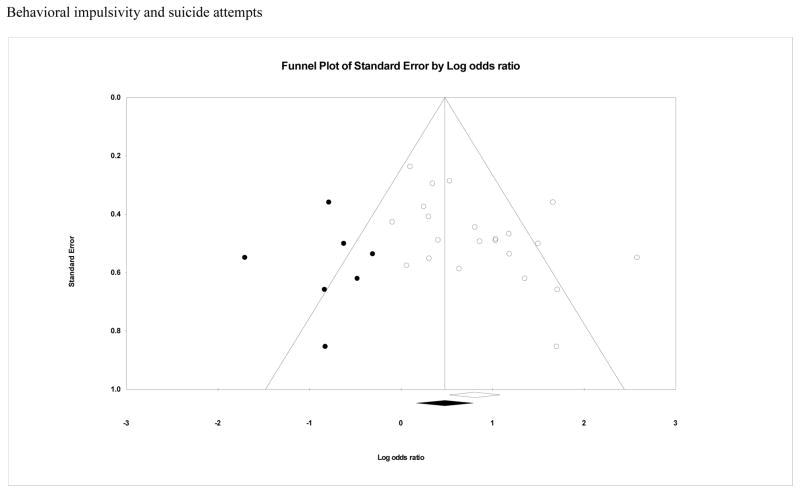
In our assessment of potential publication bias, Orwin’s fail-safe-N indicated that 164 unpublished studies with an OR of 1.0 would be required to reduce the pooled effect size for the relation between behavioral impulsivity and suicide attempts to 1.1 (our a priori trivial effect size), suggesting that the observed weighted effect size is relatively robust. Egger’s regression test, however, indicated that significant publication bias was present (intercept = 2.53, [95% CI = .61–4.45], t(20) = 2.75, p < .05). Additionally, the funnel plot of effect sizes was notably asymmetrical (Figure 2). When the trim-and-fill method was used to correct parameter estimates for potential publication bias, the adjusted weighted OR was reduced to 1.61 (95% CI = 1.18–2.20).
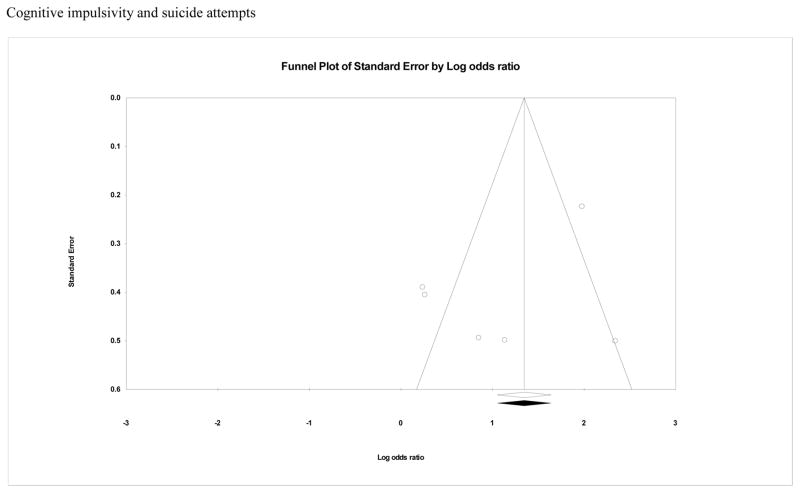
Figure 2.
Funnel plot for effect sizes in the meta-analyses. The vertical line indicates the weighted mean effect. Open circles indicate observed effects for actual studies, and closed circles indicate imputed effects for studies believed to be missing due to publication bias. The clear diamond reflects the unadjusted weighted mean effect size, whereas the black diamond reflects the weighted mean effect size after adjusting for publication bias.
The weighted effect size for the relation between cognitive impulsivity and suicide attempts, across six studies, was OR = 3.14 (95% CI = 1.48–6.67), p < .01. Heterogeneity was high (I2 = 82.34%, p < .001), suggesting moderator analyses were warranted. The strength of the association between cognitive impulsivity and suicide attempts was not moderated by mean age as a categorical (p = .21) or continuous variable (b < .01, p = .89). Likewise, the percentage of female participants in the sample was not a significant moderator (b = −.02, p = .14). Again, time-frame of suicide attempt assessment moderated the strength of the association between cognitive impulsivity and suicide attempts (p < .05), with attempts occurring within a month prior to cognitive impulsivity assessment associated with a stronger effect (OR = 10.44 [95% CI = 3.91–27.87], p < .001) than were attempts assessed over the lifetime (OR = 2.52 [95% CI = 1.11–5.72], p < .05). This finding should be interpreted with caution, however, as only one study (Cáceda et al., 2014) assessed cognitive impulsivity in relation to suicide attempts occurring within the past month. A meta-regression analysis was therefore not conducted. In separate analyses comparing suicide attempters to clinical and healthy controls, respectively, no differences were observed for healthy controls (OR = 7.98 [95% CI = .34–186.48], p = .20), but attempters were more impulsive than clinical controls (OR = 2.84 [95% CI = 1.34–6.03], p < .01). Again, caution must be exercised in interpreting the finding regarding healthy controls, as it included only two studies (Cáceda et al., 2014; Dombrovski et al., 2011).
No evidence of publication bias was found. Orwin’s fail-safe-N indicated that 66 unpublished studies with an OR of 1.0 would be required to reduce the pooled effect size for the relation between cognitive impulsivity and suicide attempts to 1.1. Egger’s regression test intercept = −3.39, (95% CI = −11.60–4.82], t(4) = 1.15, p = .32). The funnel plot of effect sizes was symmetrical (Figure 2).
3.3. NSSI versus suicide attempts
When the relation between behavioral impulsivity and NSSI was directly compared to that for this form of impulsivity and suicide attempts, a significant difference in effect size was observed (p = .01), with the association being stronger in the case of suicide attempts. With there being only one study of cognitive impulsivity and NSSI, it was not possible to compare the magnitude of this association with that for this type of impulsivity and suicide attempts.
3.4. Exploratory analyses
Exploratory analyses were conducted for specific aspects of suicidal ideation or behavior when two unique effects were available for the association between these outcomes and a specific facet of impulsivity. Additionally, effect sizes were also presented when only one unique effect was available. A measure of caution should be taken in interpreting these results, as a low number of effects may yield unstable estimates of effect sizes.
Across two studies of SI and behavioral impulsivity, no significant association was observed, with the weighted mean OR being 2.43 (95% CI = .84–7.02), p = .10. Contrastingly, across two studies of SI and cognitive impulsivity, the pooled OR was 6.47 (95% CI = 2.35–17.79), p < .001).
In the one study to assess impulsiveness of suicide attempts in relation to behavioral impulsivity, highly impulsive individuals were less likely to make planned attempts (OR = .30 [95% CI = .12–.75], p = .01). Across two studies of cognitive impulsivity, a negative association was also observed with planned attempts (OR = .14 [95% CI = .02–0.81], p = .03).
High-severity suicide attempts did not differ from low-severity attempts across two studies in terms of behavioral impulsivity (OR = 1.55 [95% CI = .76–3.15], p = .23). In the one study to examine suicide attempt severity relative to cognitive impulsivity, greater severity of attempt was associated with lower cognitive impulsivity (OR = .10 [95% CI = .02–.41], p < .01)..
Finally, in the single study to evaluate NSSI in relation to cognitive impulsivity, a non-significant association was found, albeit with a medium effect size (OR = 2.49 [95% CI = .80–7.80], p = .12).
4. Discussion
This review provides general support for self-injurious thoughts and behaviors being associated with greater impulsivity, as conceptualized within a behavioral and cognitive neuroscience perspective. The current findings differ significantly, however, from those of prior meta-analyses of suicide attempts (Anestis et al., 2014) and NSSI (Hamza et al., 2015), respectively, with larger mean effect sizes observed in the present case. These differences warrant consideration.
First, although we found greater behavioral impulsivity to be related to NSSI, interestingly, no significant effects were observed at the level of individual studies, and a recent meta-analysis (Hamza et al., 2015) similarly did not find a significant pooled effect. When considered together with the small pooled effect in the current meta-analysis, this discrepancy likely indicates that each of the primary studies and the prior meta-analysis (k = 3) were underpowered to detect an effect of this size. Caution should also be exercised in interpreting this modest effect, particularly when considering the degree to which clinically significant NSSI was present in these studies. Most studies featured NSSI inclusion criteria or subgroups with average frequency for this behavior falling below DSM-5 (American Psychiatric Association, 2013) criterion A (i.e., five days over 12 months; Fikke et al., 2011; Glenn and Klonsky, 2010; McCloskey et al., 2012; Vega et al., 2015). Additionally, only one study (Auerbach et al., 2014) assessed NSSI over a period of under 12 months, an important consideration given the state-sensitive nature of behavioral impulsivity measures (Cyders and Coskunpinar, 2011; Dougherty et al., 2004a; Moeller et al., 2001). Whether larger effects would be observed in studies with clinically significant NSSI proximal to assessment of behavioral impulsivity remains to be determined.
In the current meta-analysis, a small-to-medium effect was observed for the relation between suicide attempts and behavioral impulsivity, and a medium-to-large effect in the case of cognitive impulsivity. Contrastingly, in the previous meta-analysis of trait impulsivity and suicide attempts, a small effect was reported (Anestis et al., 2014). This difference is accentuated when recency of suicide attempt relative to time of assessment of behavioral impulsivity was considered in the current meta-analysis, particularly when restricted to past-month attempts, which yielded a large effect size. Of note, lifetime suicide attempts were associated with a significantly smaller effect comparable to that observed in the prior meta-analysis. Collectively, this pattern of findings may, in part, be accounted for by the exclusive focus of the current meta-analysis on neurobehavioral and neurocognitive indices of impulsivity, which as mentioned above, are state-sensitive (Cyders and Coskunpinar, 2011; Dougherty et al., 2004a; Moeller et al., 2001), and the contrasting emphasis of the prior meta-analysis on self-report trait impulsivity. Additionally, given that assessments of suicide attempts over the lifetime appear most common in the literature, and thus likely are most represented in the prior meta-analysis, this design characteristic may have diminished its observed effect size.
The findings of the current meta-analysis have implications for future study. Given the finding of a stronger association with behavioral impulsivity for suicide attempts relative to NSSI, an interesting question that remains unresolved is whether any observed relation with these state-sensitive indices of impulsivity, for NSSI is simply an artifact of their shared association with suicidal behavior. Such a possibility is not implausible, given that suicidal and non-suicidal self-harm are strongly associated with each other (Klonsky et al., 2013; Ribeiro et al., 2016). Thus, individuals with a history of suicide attempts frequently have a history of NSSI as well. Additionally, a proportion of participants in studies of NSSI with a history of this behavior but not suicide attempts at the time of assessment are likely eventually to attempt. The current review was unable to assess this possibility. As a step toward evaluating this question, future research is required directly comparing three groups: (i) individuals with no self-harm history, (ii) those with a history of NSSI but not suicide attempts, (iii) those with a history of suicide attempts. If the association between impulsivity and NSSI is a function of their shared relation to suicidal behavior, no significant difference would be observed between the individuals with no self-harm history and the “pure” NSSI group, and both groups would be less impulsive than the suicide attempt group. In contrast, if NSSI is associated with impulsivity independent of suicidal behavior, both self-harm groups would be more impulsive than the group with no self-harm history.
Particularly noteworthy too is that all studies in this review employed cross-sectional analyses. Research featuring longitudinal analyses is required to evaluate whether behavioral and cognitive impulsivity are simply correlates of, or more importantly, risk factors for, self-injurious thoughts and behaviors. Constructs that are only correlated with these clinical phenomena have no prognostic value, whereas risk factors, by definition, temporally precede and predict these outcomes, and therefore are of particular clinical importance (Kraemer et al., 1997).
Moreover, although notable as an indicator of general risk, trait impulsivity, a fixed marker of risk by definition, cannot inform our understanding of causal risk factors for self-injurious thoughts and behaviors (Kraemer et al., 2001, 1997). In contrast, state-sensitive neurobehavioral and neurocognitive indices of impulsivity, inasmuch as they may prove to be variable markers of risk, hold promise as candidates for causal risk factors for these outcomes. Furthermore, as mentioned above, these latter indices of impulsivity are more clinically meaningful insofar as they may reflect proximal, rather than general, risk for self-injurious thoughts and behaviors; they may lend temporal clarity as to when clinical intervention is warranted for at-risk individuals. That is, whereas trait impulsivity may aid in identifying who is at risk, indices of state-sensitive impulsivity may facilitate determination of when these individuals are most at risk. That the strength of the association between behavioral impulsivity and suicide attempts was significantly stronger in the current meta-analysis when the assessment of the former was more proximal to the occurrence of the latter is congruent with this possibility. Longitudinal research evaluating the predictive validity of these indices, especially for short-term risk, is therefore indicated.
Within this context, there is a need to employ multiple task-based measures reflecting different facets of impulsivity, particularly to maintain the distinction between behavioral and cognitive impulsivity, in studying risk for self-injurious thoughts and behaviors (Gorlyn, 2005) to the extent that potentially observed associations may elucidate neural mechanisms relevant to short-term risk for these clinical outcomes. If behavioral impulsivity is a short-term prospective predictor of suicide attempts, for example, the rIFG may be implicated in proximal risk for this behavior (Aron et al., 2003; Winstanley et al., 2006). Similarly, to the degree that cognitive impulsivity prospectively predicts proximal risk for this outcome, the OFC may be of particular relevance (Ouellet et al., 2015; Winstanley et al., 2006, 2004).
Such knowledge has direct treatment implications. Specifically, if neurobehavioral and neurocognitive facets of impulsivity are indeed prospectively predictive of self-injurious thoughts and behaviors, they may have added clinical value as variable markers of risk, relative to fixed risk markers, in having potential to serve as modifiable targets of intervention and to inform the development of future strategies for reducing risk for these outcomes in vulnerable populations. As just one example of this possibility, transcranial direct current stimulation (tDCS) is a non-invasive stimulation technique for modulating cortical excitability through the application of weak electrical currents between two scalp electrodes placed over the target cortical regions. tDCS neuromodulation of various targets has been increasingly applied in treatment research (e.g., to relieve major depression Meron et al., 2015), but it has also been used for experimental manipulation of neural networks to enhance or diminish specific cognitive functions or symptoms, including impulsivity. Anodal tDCS applied to the rIFG appears to reduce behavioral impulsivity (Cai et al., 2016; Cunillera et al., 2014; Ditye et al., 2012; Stramaccia et al., 2015), whereas anodal tDCS to the left OFC has been found to lead to a reduction in cognitive impulsivity (Ouellet et al., 2015). If behavioral and cognitive impulsivity are implicated in short-term risk for self-injurious thoughts and behaviors, tDCS may therefore have potential to become a new protocol for addressing these clinical outcomes, through targeting the respective underlying neural circuitry of these facets of impulsivity. With the current limited progress in the treatment of suicidal behavior and NSSI (Calati and Courtet, 2016; Ougrin et al., 2015), there remains a pressing need for the development of novel treatment paradigms for these behaviors. Such treatment development may be significantly aided by a better understanding of neurobehavioral and neurocognitive facets of impulsivity, insofar as they have potential to inform our understanding of the processes underlying short-term risk for these clinical outcomes.
Highlights.
Meta-analysis of behavioral and cognitive impulsivity in relation to self-injury
Behavioral impulsivity was associated with non-suicidal self-injury (NSSI)
Behavioral and cognitive impulsivity were associated with suicide attempts
Link with behavioral impulsivity was stronger for past-month than lifetime attempts
Studies with clinically significant NSSI and longitudinal research are needed
Acknowledgments
Preparation of this manuscript was supported in part by the National Institute of Mental Health of the National Institutes of Health under Award Numbers R01MH101138 and R21MH112055. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agency.
Footnotes
Here, we refer to the influence of the individual’s current state on performance on a specific measure of impulsivity, rather than self-reported general tendencies for affect to increase impulsivity (e.g., negative urgency).
These 10 studies were excluded after attempts to contact the study authors did not produce sufficient data for inclusion in the meta-analysis. An eleventh study (Dombrovski et al., 2011) similarly did not report data required for meta-analysis, but was retained after the necessary data were obtained from the study authors.
Several studies featured overlapping samples. Whenever it remained unclear after inspection of the full text whether two studies reported on overlapping samples, the study authors were contacted to seek clarity on this issue. In cases where two studies used the same or overlapping samples but examined different outcomes (e.g., NSSI and suicide attempts), both studies were retained for respective analyses involving these outcomes. In all but one case where two studies used overlapping samples to examine the same outcome, identical measures of behavioral or cognitive impulsivity were also used. In these cases, the study with the larger sample size for the relevant analysis was retained. For the one case where two studies (Keilp et al., 2013, 2008) used overlapping samples to assess the same outcome and different measures of behavioral impulsivity were employed, the study (Keilp et al., 2008) that afforded the larger sample size for analysis was retained.
Several studies employed multiple measures of impulsivity and/or examined several aspects of self-harm.
A fifth study, not counted here, also examined impulsivity in relation to suicide attempt severity but did not report sufficient data for inclusion in the relevant analysis, and contacting the study authors yielded no additional data.
Several studies featured essentially verbally administered self-report measures of this outcome. It was not always possible, however, reliably to differentiate between these measures and genuine interviews.
One study yielded separate effects for males and females (Fikke et al., 2011).
The lower end of the confidence interval was rounded down but exceeded 1.00.
Results are presented for age as a continuous variable. When it was considered as a categorical variable, the results remained essentially unchanged.
Financial Disclosure None of the authors have any conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. American Psychiatric Association; Washington, DC: 2013. [Google Scholar]
- Anestis MD, Soberay KA, Gutierrez PM, Hernández TD, Joiner TE. Reconsidering the link between impulsivity and suicidal behavior. Personal Soc Psychol Rev. 2014;18:366–386. doi: 10.1177/1088868314535988. [DOI] [PubMed] [Google Scholar]
- Aron AR, Fletcher PC, Bullmore ET, Sahakian BJ, Robbins TW. Stop-signal inhibition disrupted by damage to right inferior frontal gyrus in humans. Nat Neurosci. 2003;6:115–116. doi: 10.1038/nn1003. [DOI] [PubMed] [Google Scholar]
- Asarnow JR, Porta G, Spirito A, Emslie G, Clarke G, Wagner KD, Vitiello B, Keller M, Birmaher B, McCracken J, Mayes T, Berk M, Brent DA. Suicide attempts and nonsuicidal self-injury in the Treatment of Resistant Depression in Adolescents: Findings from the TORDIA study. J Am Acad Child Adolesc Psychiatry. 2011;50:772–781. doi: 10.1016/j.jaac.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach RP, Kim JC, Chango JM, Spiro WJ, Cha C, Gold J, Esterman M, Nock MK. Adolescent nonsuicidal self-injury: examining the role of child abuse, comorbidity, and disinhibition. Psychiatry Res. 2014;220:579–584. doi: 10.1016/j.psychres.2014.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagge CL, Littlefield AK, Rosellini AJ, Coffey SF. Relations among behavioral and questionnaire measures of impulsivity in a sample of suicide attempters. Suicide Life-Threatening Behav. 2013;43:460–467. doi: 10.1111/sltb.12030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bari A, Robbins TW. Inhibition and impulsivity: behavioral and neural basis of response control. Prog Neurobiol. 2013;108:44–79. doi: 10.1016/j.pneurobio.2013.06.005. [DOI] [PubMed] [Google Scholar]
- Biostat. Comprehensive Meta-Analysis Version 3. 2014. [Google Scholar]
- Booij L, Swenne CA, Brosschot JF, Haffmans PMJ, Thayer JF, Van der Does AJW. Tryptophan depletion affects heart rate variability and impulsivity in remitted depressed patients with a history of Suicidal ideation. Biol Psychiatry. 2006;60:507–514. doi: 10.1016/j.biopsych.2006.02.010. [DOI] [PubMed] [Google Scholar]
- Brenner LA, Bahraini N, Homaifar BY, Monteith LL, Nagamoto H, Dorsey-Holliman B, Forster JE. Executive functioning and suicidal behavior among veterans with and without a history of traumatic brain injury. Arch Phys Med Rehabil. 2015;96:1411–1418. doi: 10.1016/j.apmr.2015.04.010. [DOI] [PubMed] [Google Scholar]
- Brent D. Nonsuicidal self-injury as a predictor of suicidal behavior in depressed adolescents. Am J Psychiatry. 2011;168:452–454. doi: 10.1176/appi.ajp.2011.11020215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent D. In search of endophenotypes for suicidal behavior. Am J Psychiatry. 2009;166:1087–1089. doi: 10.1176/appi.ajp.2009.09081131. [DOI] [PubMed] [Google Scholar]
- Bridge JA, Reynolds B, McBee-Strayer SM, Sheftall AH, Ackerman J, Stevens J, Mendoza K, Campo JV, Brent DA. Impulsive aggression, delay discounting, and adolescent suicide attempts: effects of current psychotropic medication use and family history of suicidal behavior. J Child Adolesc Psychopharmacol. 2015;25:114–123. doi: 10.1089/cap.2014.0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cáceda R, Durand D, Cortes E, Prendes-Alvarez S, Moskovciak T, Harvey PD, Nemeroff CB. Impulsive choice and psychological pain in acutely suicidal depressed patients. Psychosom Med. 2014;76:445–451. doi: 10.1097/PSY.0000000000000075. [DOI] [PubMed] [Google Scholar]
- Cai Y, Li S, Liu J, Li D, Feng Z, Wang Q, Chen C, Xue G. The role of the frontal and parietal cortex in proactive and reactive inhibitory control: A transcranial direct current stimulation study. J Cogn Neurosci. 2016;28:177–186. doi: 10.1162/jocn_a_00888. [DOI] [PubMed] [Google Scholar]
- Calati R, Courtet P. Is psychotherapy effective for reducing suicide attempt and non-suicidal self-injury rates? Meta-analysis and meta-regression of literature data. J Psychiatr Res. 2016;79:8–20. doi: 10.1016/j.jpsychires.2016.04.003. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Increase in Suicide in the United States, 1999–2014 [WWW Document] 2016a URL http://www.cdc.gov/nchs/products/databriefs/db241.htm.
- Centers for Disease Control and Prevention. Declines in cancer death rates among children and adolescents in the United States, 1999–2014 [WWW Document] 2016b URL http://www.cdc.gov/nchs/products/databriefs/db257.htm.
- Chamberlain SR, Odlaug BL, Schreiber LRN, Grant JE. Clinical and neurocognitive markers of suicidality in young adults. J Psychiatr Res. 2013;47:586–591. doi: 10.1016/j.jpsychires.2012.12.016. [DOI] [PubMed] [Google Scholar]
- Cunillera T, Fuentemilla L, Brignani D, Cucurell D, Miniussi C. A simultaneous modulation of reactive and proactive inhibition processes by anodal tDCS on the right inferior frontal cortex. PLoS One. 2014;9:e113537. doi: 10.1371/journal.pone.0113537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders MA, Coskunpinar A. The relationship between self-report and lab task conceptualizations of impulsivity. J Res Pers. 2012;46:121–124. doi: 10.1016/j.jrp.2011.11.005. [DOI] [Google Scholar]
- Cyders MA, Coskunpinar A. Measurement of constructs using self-report and behavioral lab tasks: Is there overlap in nomothetic span and construct representation for impulsivity? Clin Psychol Rev. 2011;31:965–982. doi: 10.1016/j.cpr.2011.06.001. [DOI] [PubMed] [Google Scholar]
- de Moraes PHP, Neves FS, Vasconcelos AG, Lima IMM, Brancaglion M, Sedyiama CY, Fuentes D, Romano-Silva MA, Corrêa H, Malloy-Diniz LF. Relationship between neuropsychological and clinical aspects and suicide attempts in euthymic bipolar patients. Psicol Reflexão e Crítica. 2013;26:160–167. doi: 10.1590/S0102-79722013000100017. [DOI] [Google Scholar]
- Ditye T, Jacobson L, Walsh V, Lavidor M. Modulating behavioral inhibition by tDCS combined with cognitive training. Exp Brain Res. 2012;219:363–368. doi: 10.1007/s00221-012-3098-4. [DOI] [PubMed] [Google Scholar]
- Dombrovski AY, Szanto K, Siegle GJ, Wallace ML, Forman SD, Sahakian B, Reynolds CF, III, Clark L. Lethal forethought: Delayed reward discounting differentiates high- and low-lethality suicide attempts in old age. Biol Psychiatry. 2011;70:138–144. doi: 10.1016/j.biopsych.2010.12.025. doi:16/j.biopsych.2010.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty DM, Mathias CW, Marsh-Richard DM, Prevette KN, Dawes MA, Hatzis ES, Palmes G, Nouvion SO. Impulsivity and clinical symptoms among adolescents with non-suicidal self-injury with or without attempted suicide. Psychiatry Res. 2009;169:22–27. doi: 10.1016/j.psychres.2008.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty DM, Mathias CW, Marsh DM, Moeller FG, Swann AC. Suicidal behaviors and drug abuse: Impulsivity and its assessment. Drug Alcohol Depend., Drug Abuse and Suicidal Behavior. 2004a;76:S93–S105. doi: 10.1016/j.drugalcdep.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Dougherty DM, Mathias CW, Marsh DM, Papageorgiou TD, Swann AC, Moeller FG. Laboratory measured behavioral impulsivity relates to suicide attempt history. Suicide Life-Threatening Behav. 2004b;34:374–385. doi: 10.1521/suli.34.4.374.53738. [DOI] [PubMed] [Google Scholar]
- Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fikke LT, Melinder A, Landrø NI. Executive functions are impaired in adolescents engaging in non-suicidal self-injury. Psychol Med. 2011;41:601–610. doi: 10.1017/S0033291710001030. [DOI] [PubMed] [Google Scholar]
- Glenn CR, Klonsky ED. A multimethod analysis of impulsivity in nonsuicidal self-injury. Personal Disord. 2010;1:67–75. doi: 10.1037/a0017427. [DOI] [PubMed] [Google Scholar]
- Gorlyn M. Impulsivity in the prediction of suicidal behavior in adolescent populations. Int J Adolesc Med Health. 2005;17:205–209. doi: 10.1515/ijamh.2005.17.3.205. [DOI] [PubMed] [Google Scholar]
- Hamilton KR, Littlefield AK, Anastasio NC, Cunningham KA, Fink LHL, Wing VC, Mathias CW, Lane SD, Schütz CG, Swann AC, Lejuez CW, Clark L, Moeller FG, Potenza MN. Rapid-response impulsivity: Definitions, measurement issues, and clinical implications. Personal Disord Theory, Res Treat. 2015a;6:168–181. doi: 10.1037/per0000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton KR, Mitchell MR, Wing VC, Balodis IM, Bickel WK, Fillmore M, Lane SD, Lejuez CW, Littlefield AK, Luijten M, Mathias CW, Mitchell SH, Napier TC, Reynolds B, Schütz CG, Setlow B, Sher KJ, Swann AC, Tedford SE, White MJ, Winstanley CA, Yi R, Potenza MN, Moeller FG. Choice impulsivity: Definitions, measurement issues, and clinical implications. Personal Disord Theory, Res Treat. 2015b;6:182–198. doi: 10.1037/per0000099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamza CA, Willoughby T, Heffer T. Impulsivity and nonsuicidal self-injury: A review and meta-analysis. Clin Psychol Rev. 2015;38:13–24. doi: 10.1016/j.cpr.2015.02.010. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homaifar BY, Brenner LA, Forster JE, Nagamoto H. Traumatic brain injury, executive functioning, and suicidal behavior: a brief report. Rehabil Psychol. 2012;57:337–341. doi: 10.1037/a0030480. [DOI] [PubMed] [Google Scholar]
- Horesh N. Self-report vs. computerized measures of impulsivity as a correlate of suicidal behavior. Crisis. 2001;22:27–31. doi: 10.1027//0227-5910.22.1.27. [DOI] [PubMed] [Google Scholar]
- Janis IB, Nock MK. Are self-injurers impulsive?: Results from two behavioral laboratory studies. Psychiatry Res. 2009;169:261–267. doi: 10.1016/j.psychres.2008.06.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner TE, Brown JS, Wingate LR. The psychology and neurobiology of suicidal behavior. Annu Rev Psychol. 2005;56:287–314. doi: 10.1146/annurev.psych.56.091103.070320. [DOI] [PubMed] [Google Scholar]
- Jones K, Kinsella GJ, Ong B, Scheinkestel C. Supervisory attentional control following carbon monoxide poisoning. J Int Neuropsychol Soc. 2004;10:843–850. doi: 10.1017/s135561770410605x. [DOI] [PubMed] [Google Scholar]
- Kasen S, Cohen P, Chen H. Developmental course of impulsivity and capability from age 10 to age 25 as related to trajectory of suicide attempt in a community cohort. Suicide Life-Threatening Behav. 2011;41:180–192. doi: 10.1111/j.1943-278X.2011.00017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keilp JG, Beers SR, Burke AK, Melhem NM, Oquendo MA, Brent DA, Mann JJ. Neuropsychological deficits in past suicide attempters with varying levels of depression severity. Psychol Med. 2014;44:2965–2974. doi: 10.1017/S0033291714000786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keilp JG, Gorlyn M, Oquendo MA, Burke AK, Mann JJ. Attention deficit in depressed suicide attempters. Psychiatry Res. 2008;159:7–17. doi: 10.1016/j.psychres.2007.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keilp JG, Gorlyn M, Russell M, Oquendo MA, Burke AK, Harkavy-Friedman J, Mann JJ. Neuropsychological function and suicidal behavior: attention control, memory and executive dysfunction in suicide attempt. Psychol Med. 2013;43:539–551. doi: 10.1017/S0033291712001419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky ED, May A. Rethinking impulsivity in suicide. Suicide Life-Threatening Behav. 2010;40:612–619. doi: 10.1521/suli.2010.40.6.612. [DOI] [PubMed] [Google Scholar]
- Klonsky ED, May AM, Glenn CR. The relationship between nonsuicidal self-injury and attempted suicide: Converging evidence from four samples. J Abnorm Psychol. 2013;122:231–237. doi: 10.1037/a0030278. [DOI] [PubMed] [Google Scholar]
- Klonsky ED, May AM, Saffer BY. Suicide, suicide attempts, and suicidal ideation. Annu Rev Clin Psychol. 2016;12:307–330. doi: 10.1146/annurev-clinpsy-021815-093204. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Kazdin AE, Offord DR, Kessler RC, Jensen PS, Kupfer DJ. Coming to terms with the terms of risk. Arch Gen Psychiatry. 1997;54:337–343. doi: 10.1001/archpsyc.1997.01830160065009. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. Am J Psychiatry. 2001;158:848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- Lane SD, Cherek DR, Rhodes HM, Pietras CJ, Tcheremissine OV. Relationships among laboratory and psychometric measures of impulsivity: Implications in substance abuse and dependence. Addict Disord Their Treat. 2003;2:33–40. doi: 10.1097/00132576-200302020-00001. [DOI] [Google Scholar]
- Liu RT, Vassileva J, Gonzalez R, Martin EM. A comparison of delay discounting among substance users with and without suicide attempt history. Psychol Addict Behav. 2012;26:980–985. doi: 10.1037/a0027384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malloy-Diniz LF, Neves FS, Abrantes SSC, Fuentes D, Corrêa H. Suicide behavior and neuropsychological assessment of type I bipolar patients. J Affect Disord. 2009;112:231–236. doi: 10.1016/j.jad.2008.03.019. [DOI] [PubMed] [Google Scholar]
- Mann JJ, Apter A, Bertolote J, Beautrais A, Currier D, Haas A, Hegerl U, Lonnqvist J, Malone K, Marusic A, Mehlum L, Patton G, Phillips M, Rutz W, Rihmer Z, Schmidtke A, Shaffer D, Silverman M, Takahashi Y, Varnik A, Wasserman D, Yip P, Hendin H. Suicide prevention strategies: A systematic review. JAMA. 2005;294:2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- Mars B, Heron J, Crane C, Hawton K, Kidger J, Lewis G, Macleod J, Tilling K, Gunnell D. Differences in risk factors for self-harm with and without suicidal intent: findings from the ALSPAC cohort. J Affect Disord. 2014;168:407–414. doi: 10.1016/j.jad.2014.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathias CW, Dougherty DM, James LM, Richard DM, Dawes MA, Acheson A, Hill-Kapturczak N. Intolerance to delayed reward in girls with multiple suicide attempts. Suicide Life-Threatening Behav. 2011;41:277–286. doi: 10.1111/j.1943-278X.2011.00027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCloskey MS, Look AE, Chen EY, Pajoumand G, Berman ME, Mc Closkey MS. Nonsuicidal self-injury: Relationship to behavioral and self-rating measures of impulsivity and self-aggression. Suicide Life-Threatening Behav. 2012;42:197–209. doi: 10.1111/j.1943-278X.2012.00082.x. [DOI] [PubMed] [Google Scholar]
- McGirr A, Renaud J, Bureau A, Seguin M, Lesage A, Turecki G. Impulsive-aggressive behaviours and completed suicide across the life cycle: A predisposition for younger age of suicide. Psychol Med. 2008;38:407–417. doi: 10.1017/S0033291707001419. [DOI] [PubMed] [Google Scholar]
- Meron D, Hedger N, Garner M, Baldwin DS. Transcranial direct current stimulation (tDCS) in the treatment of depression: Systematic review and meta-analysis of efficacy and tolerability. Neurosci Biobehav Rev. 2015;57:46–62. doi: 10.1016/j.neubiorev.2015.07.012. [DOI] [PubMed] [Google Scholar]
- Moeller FG, Barratt ES, Dougherty DM, Schmitz JM, Swann AC. Psychiatric aspects of impulsivity. Am J Psychiatry. 2001;158:1783–1793. doi: 10.1176/appi.ajp.158.11.1783. [DOI] [PubMed] [Google Scholar]
- Nangle JM, Clarke S, Morris DW, Schwaiger S, McGhee KA, Kenny N, Murphy K, Gill M, Corvin A, Donohoe G. Neurocognition and suicidal behaviour in an Irish population with major psychotic disorders. Schizophr Res. 2006;85:196–200. doi: 10.1016/j.schres.2006.03.035. [DOI] [PubMed] [Google Scholar]
- National Action Alliance for Suicide Prevention. A prioritized research agenda for suicide prevention: An action plan to save lives. National Institute of Mental Health and the Research Prioritization Task Force; Rockville, MD: 2014. [Google Scholar]
- Nisbett RE, Wilson TD. Telling more than we can know: Verbal reports on mental processes. Psychol Rev. 1977;84:231–259. doi: 10.1037/0033-295X.84.3.231. [DOI] [Google Scholar]
- Nock MK. Self-injury. Annu Rev Clin Psychol. 2010;6:339–363. doi: 10.1146/annurev.clinpsy.121208.131258. [DOI] [PubMed] [Google Scholar]
- Orwin RG. A Fail-safe N for effect size in meta-analysis. J Educ Stat. 1983;8:157–159. doi: 10.2307/1164923. [DOI] [Google Scholar]
- Ouellet J, McGirr A, Van den Eynde F, Jollant F, Lepage M, Berlim MT. Enhancing decision-making and cognitive impulse control with transcranial direct current stimulation (tDCS) applied over the orbitofrontal cortex (OFC): A randomized and sham-controlled exploratory study. J Psychiatr Res. 2015;69:27–34. doi: 10.1016/j.jpsychires.2015.07.018. [DOI] [PubMed] [Google Scholar]
- Ougrin D, Tranah T, Stahl D, Moran P, Asarnow JR. Therapeutic interventions for suicide attempts and self-harm in adolescents: Systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2015;54:97–107. e2. doi: 10.1016/j.jaac.2014.10.009. [DOI] [PubMed] [Google Scholar]
- Pan LA, Batezati-Alves SC, Almeida JRC, Segreti A, Akkal D, Hassel S, Lakdawala S, Brent DA, Phillips ML. Dissociable patterns of neural activity during response inhibition in depressed adolescents with and without suicidal behavior. J Am Acad Child Adolesc Psychiatry. 2011;50:602–611. doi: 10.1016/j.jaac.2011.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters J, Büchel C. The neural mechanisms of inter-temporal decision-making: Understanding variability. Trends Cogn Sci. 2011;15:227–239. doi: 10.1016/j.tics.2011.03.002. [DOI] [PubMed] [Google Scholar]
- Raust A, Slama F, Mathieu F, Roy I, Chenu A, Koncke D, Fouques D, Jollant F, Jouvent E, Courtet P, Leboyer M, Bellivier F. Prefrontal cortex dysfunction in patients with suicidal behavior. Psychol Med. 2007;37:411–419. doi: 10.1017/S0033291706009111. [DOI] [PubMed] [Google Scholar]
- Reynolds B, Ortengren A, Richards JB, de Wit H. Dimensions of impulsive behavior: Personality and behavioral measures. Pers Individ Dif. 2006;40:305–315. doi: 10.1016/j.paid.2005.03.024. [DOI] [Google Scholar]
- Reynolds B, Penfold RB, Patak M. Dimensions of impulsive behavior in adolescents: Laboratory behavioral assessments. Exp Clin Psychopharmacol. 2008;16:124–131. doi: 10.1037/1064-1297.16.2.124. [DOI] [PubMed] [Google Scholar]
- Ribeiro JD, Franklin JC, Fox KR, Bentley KH, Kleiman EM, Chang BP, Nock MK. Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: a meta-analysis of longitudinal studies. Psychol Med. 2016;46:225–236. doi: 10.1017/S0033291715001804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richard-Devantoy S, Annweiler C, Le Gall D, Garré JB, Olié JP, Beauchet O. Cognitive inhibition in suicidal depressed elderly: a case-control pilot study. J Clin Psychiatry. 2011;72:871–872. doi: 10.4088/JCP.10l06797. [DOI] [PubMed] [Google Scholar]
- Richard-Devantoy S, Jollant F, Kefi Z, Turecki G, Olié JP, Annweiler C, Beauchet O, Le Gall D. Deficit of cognitive inhibition in depressed elderly: A neurocognitive marker of suicidal risk. J Affect Disord. 2012;140:193–199. doi: 10.1016/j.jad.2012.03.006. [DOI] [PubMed] [Google Scholar]
- Robbins TW, Gillan CM, Smith DG, de Wit S, Ersche KD. Neurocognitive endophenotypes of impulsivity and compulsivity: towards dimensional psychiatry. Trends Cogn Sci. 2012;16:81–91. doi: 10.1016/j.tics.2011.11.009. [DOI] [PubMed] [Google Scholar]
- Spirito A, Esposito-Smythers C. Attempted and completed suicide in adolescence. Annu Rev Clin Psychol. 2006;2:237–266. doi: 10.1146/annurev.clinpsy.2.022305.095323. [DOI] [PubMed] [Google Scholar]
- Stramaccia DF, Penolazzi B, Sartori G, Braga M, Mondini S, Galfano G. Assessing the effects of tDCS over a delayed response inhibition task by targeting the right inferior frontal gyrus and right dorsolateral prefrontal cortex. Exp Brain Res. 2015;233:2283–2290. doi: 10.1007/s00221-015-4297-6. [DOI] [PubMed] [Google Scholar]
- Swann AC, Dougherty DM, Pazzaglia PJ, Pham M, Steinberg JL, Moeller FG. Increased impulsivity associated with severity of suicide attempt history in patients with bipolar disorder. Am J Psychiatry. 2005;162:1680–1687. doi: 10.1176/appi.ajp.162.9.1680. [DOI] [PubMed] [Google Scholar]
- Swann AC, Lijffijt M, Lane SD, Steinberg JL, Moeller FG. Severity of bipolar disorder is associated with impairment of response inhibition. J Affect Disord. 2009;116:30–36. doi: 10.1016/j.jad.2008.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Gaalen MM, Brueggeman RJ, Bronius PFC, Schoffelmeer ANM, Vanderschuren LJMJ. Behavioral disinhibition requires dopamine receptor activation. Psychopharmacology (Berl) 2006a;187:73–85. doi: 10.1007/s00213-006-0396-1. [DOI] [PubMed] [Google Scholar]
- van Gaalen MM, van Koten R, Schoffelmeer ANM, Vanderschuren LJMJ. Critical involvement of dopaminergic neurotransmission in impulsive decision making. Biol Psychiatry. 2006b;60:66–73. doi: 10.1016/j.biopsych.2005.06.005. [DOI] [PubMed] [Google Scholar]
- van Heeringen C, Bijttebier S, Godfrin K. Suicidal brains: A review of functional and structural brain studies in association with suicidal behaviour. Neurosci Biobehav Rev. 2011;35:688–698. doi: 10.1016/j.neubiorev.2010.08.007. [DOI] [PubMed] [Google Scholar]
- van Heeringen K, Mann JJ. The neurobiology of suicide. Lancet Psychiatry. 2014;1:63–72. doi: 10.1016/S2215-0366(14)70220-2. [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE. The interpersonal theory of suicide. Psychol Rev. 2010;117:575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanyukov PM, Szanto K, Hallquist MN, Siegle GJ, Reynolds CF, Forman SD, Aizenstein HJ, Dombrovski AY. Paralimbic and lateral prefrontal encoding of reward value during intertemporal choice in attempted suicide. Psychol Med. 2016;46:381–391. doi: 10.1017/S0033291715001890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vega D, Vilà-Balló A, Soto À, Amengual J, Ribas J, Torrubia R, Rodríguez-Fornells A, Marco-Pallarés J. Preserved error-monitoring in borderline personality disorder patients with and without non-suicidal self-injury behaviors. PLoS One. 2015;10:e0143994. doi: 10.1371/journal.pone.0143994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins HB, Meyer TD. Is there an empirical link between impulsivity and suicidality in bipolar disorders? A review of the current literature and the potential psychological implications of the relationship. Bipolar Disord. 2013;15:542–558. doi: 10.1111/bdi.12090. [DOI] [PubMed] [Google Scholar]
- Wenzel A, Beck AT. A cognitive model of suicidal behavior: Theory and treatment. Appl Prev Psychol. 2008;12:189–201. doi: 10.1016/j.appsy.2008.05.001. [DOI] [Google Scholar]
- Westheide J, Quednow BB, Kuhn KU, Hoppe C, Cooper-Mahkorn D, Hawellek B, Eichler P, Maier W, Wagner M. Executive performance of depressed suicide attempters: The role of suicidal ideation. Eur Arch Psychiatry Clin Neurosci. 2008;258:414–421. doi: 10.1007/s00406-008-0811-1. [DOI] [PubMed] [Google Scholar]
- Whelan R, Conrod PJ, Poline JB, Lourdusamy A, Banaschewski T, Barker GJ, Bellgrove MA, Büchel C, Byrne M, Cummins TDR, Fauth-Bühler M, Flor H, Gallinat J, Heinz A, Ittermann B, Mann K, Martinot JL, Lalor EC, Lathrop M, Loth E, Nees F, Paus T, Rietschel M, Smolka MN, Spanagel R, Stephens DN, Struve M, Thyreau B, Vollstaedt-Klein S, Robbins TW, Schumann G, Garavan H Consortium the I. Adolescent impulsivity phenotypes characterized by distinct brain networks. Nat Neurosci. 2012;15:920–925. doi: 10.1038/nn.3092. [DOI] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR. The Five Factor Model and impulsivity: Using a structural model of personality to understand impulsivity. Pers Individ Dif. 2001;30:669–689. doi: 10.1016/S0191-8869(00)00064-7. [DOI] [Google Scholar]
- Wichstrøm L. Predictors of non-suicidal self-injury versus attempted suicide: Similar or different? Arch Suicide Res. 2009;13:105–122. doi: 10.1080/13811110902834992. [DOI] [PubMed] [Google Scholar]
- Wilkinson P, Kelvin R, Roberts C, Dubicka B, Goodyer I. Clinical and psychosocial predictors of suicide attempts and nonsuicidal self-injury in the Adolescent Depression Antidepressants and Psychotherapy Trial (ADAPT) Am J Psychiatry. 2011;168:495–501. doi: 10.1176/appi.ajp.2010.10050718. [DOI] [PubMed] [Google Scholar]
- Winstanley CA, Eagle DM, Robbins TW. Behavioral models of impulsivity in relation to ADHD: Translation between clinical and preclinical studies. Clin Psychol Rev. 2006;26:379–395. doi: 10.1016/j.cpr.2006.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winstanley CA, Olausson P, Taylor JR, Jentsch JD. Insight into the relationship between impulsivity and substance abuse from studies using animal models. Alcohol Clin Exp Res. 2010;34:1306–1318. doi: 10.1111/j.1530-0277.2010.01215.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winstanley CA, Theobald DEH, Cardinal RN, Robbins TW. Contrasting roles of basolateral amygdala and orbitofrontal cortex in impulsive choice. J Neurosci. 2004;24:4718–4722. doi: 10.1523/JNEUROSCI.5606-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wojnar M, Ilgen MA, Czyz E, Strobbe S, Klimkiewicz A, Jakubczyk A, Glass J, Brower KJ. Impulsive and non-impulsive suicide attempts in patients treated for alcohol dependence. J Affect Disord. 2009;115:131–139. doi: 10.1016/j.jad.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu CS, Liao SC, Lin KM, Tseng MMC, Wu ECH, Liu SK. Multidimensional assessments of impulsivity in subjects with history of suicidal attempts. Compr Psychiatry. 2009;50:315–321. doi: 10.1016/j.comppsych.2008.09.006. [DOI] [PubMed] [Google Scholar]