Abstract
Background
Mucoid degeneration of the anterior cruciate ligament (ACL) is mostly observed in middle-aged patients with knee pain and limited range of motion. Although arthroscopic resection of the degenerated ACL is the treatment of choice following the failure of conservative management, the extent of the excision and subsequent ACL reconstruction for postoperative knee instability remains controversial.
Case reports
We present four cases of mucoid degeneration of the ACL in patients aged <40 years, and suggest a suitable treatment strategy for younger patients. All four patients (mean age, 33.8 years) were diagnosed with mucoid degeneration of the ACL based on characteristic clinical symptoms and magnetic resonance imaging. Arthroscopic resection of the affected portion of the ACL was performed as follows: partial resection in two cases with limited hypertrophy, and total ACL resection in the remaining two cases with degeneration involving the entire ligament. Preoperative symptoms disappeared in all cases after resection of the lesions. In the two patients with partial resection, the ACL was completely torn during subsequent sports activities despite showing no symptoms of instability for 2 years postoperatively. All four patients, including the two treated by total resection, underwent ACL reconstruction using an autogenous hamstring tendon.
Conclusion
Considering the rupture of residual ACL fibres after partial resection and the inevitability of total ACL resection due to degeneration of the entire ligament, ACL reconstruction should be considered in younger patients with symptomatic mucoid degeneration of the ACL.
Keywords: anterior cruciate ligament, mucoid degeneration, reconstruction, young patient
Introduction
Mucoid degeneration of the anterior cruciate ligament (ACL) is a rare condition in clinical practice. It is mostly observed in middle-aged patients with knee pain and limited range of motion. Since its first description by Kumar et al1 in 1999, several reports have described its characteristic features, including clinical findings, imaging, arthroscopic findings, and histology.2, 3, 4, 5, 6, 7, 8, 9 Although arthroscopic resection of the affected ACL is the treatment of choice following the failure of conservative management, the extent of the ACL excision and subsequent ACL reconstruction for postoperative knee instability remains controversial.4, 5, 8
According to previous reports, most patients do not complain of postoperative instability.1, 2, 4, 5, 8, 9 Kim et al4 reported that 91 patients with a mean age of 61 years had no instability symptoms; however, osteoarthritic changes were observed in all patients. In other studies, patients did not exhibit instability symptoms due to low sports activity despite being relatively young.8, 9 However, Lintz et al5 reported instability in 48% of 29 arthroscopically treated patients at final follow up. All patients were aged <50 years and exercised regularly. Young patients who are motivated to participate in sports activities tend to have more subjective instability symptoms than older and sedentary patients. A different treatment option should be considered for young patients because mucoid degeneration of the ACL is observed mostly in middle-aged patients, and previously reported treatment options are not necessarily sufficient for young patients. We present four cases of mucoid degeneration of the ACL in patients aged ≤40 years and suggest a suitable treatment for young patients interested in sports.
Case reports
Four patients (3 men and 1 woman; mean age at diagnosis 34 years; range, 26–38 years) diagnosed with mucoid degeneration of the ACL underwent surgery. All patients complained of knee pain during deep flexion and limited range of motion. One had an apparent extension deficit, with a heel-height distance of 8 cm. Symptoms started insidiously, except in one patient who had definite trauma, and the duration of symptoms ranged from 3 months to 17 months, with an average duration of 9 months. Magnetic resonance imaging revealed an ill-defined, enlarged ligament with intermediate signal intensity in T1-weighted images and high signal intensity in T2-weighted images, despite maintenance of continuity (Fig. 1, Fig. 2). After failure of conservative treatment, including nonsteroidal anti-inflammatory drugs, physiotherapy, and joint injection, all patients underwent arthroscopic surgery. Written informed consent was obtained from the patients.
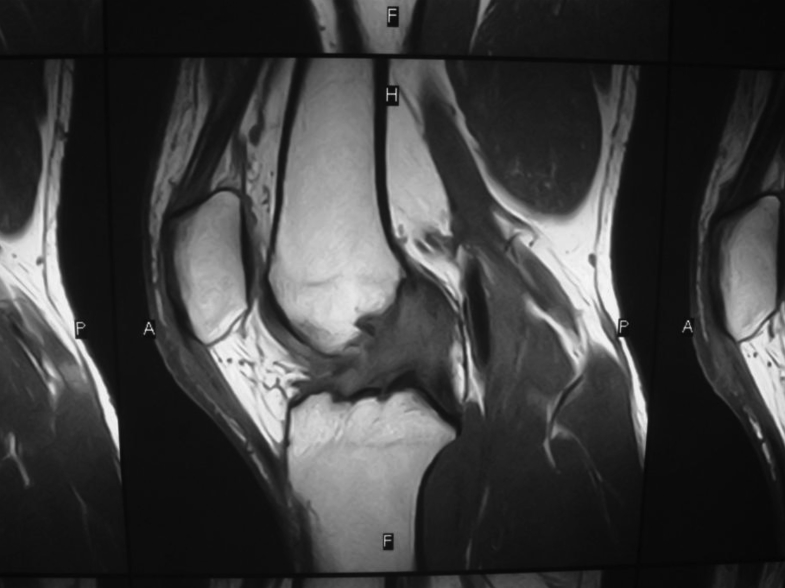
Fig. 1.
Magnetic resonance imaging findings show an enlarged ligament with intermediate signal intensity on T1-weighted images.
Fig. 2.

Magnetic resonance imaging findings show high signal intensity on T2-weighted images, despite maintenance of continuity.
Arthroscopic findings showed that the hypertrophied ACL, with loss of synovial coverage, filled the intercondylar area (Fig. 3). Although the ACL was not torn, a yellow substance was detected within the fibres when probed in all cases. Anteromedial fibres, which were mainly affected, were partially resected in two patients. After resection of approximately 50% of the whole ACL, the remaining ACL was still taut when probed. Total resection was inevitable for the remaining two patients. One patient had a degenerated mass that occupied almost the entire ACL and the other patient exhibited inflammation of the entire femoral attachment.
Fig. 3.

Arthroscopic findings show that the hypertrophied anterior cruciate ligament, with loss of synovial coverage, filled the intercondylar area.
The excised segments were histologically examined after staining with haematoxylin and eosin. The knee was not immobilized postoperatively. All patients were allowed to bear weight as tolerated and encouraged to perform an active range of motion exercises immediately.
Histological examination of the excised fragments revealed the presence of multifocal myxoid changes within ACL collagen fibres and oedematous fibrous tissue (Fig. 4). Locally, neovascularization was found in two cases, and an increase in synovia in two cases. In all patients, preoperative knee pain disappeared gradually, and full range of motion was achieved after motion exercises.
Fig. 4.

Histological examination of the excised fragments reveal the presence of multifocal myxoid changes (large black arrow) within anterior cruciate ligament collagen fibres (black arrow) and oedematous fibrous tissue.
Although the two patients with partially resected ACL had no symptoms of knee instability, the ACL was completely torn during running and playing volleyball, respectively, 2 years after the initial operation. Both patients underwent ACL reconstruction using an autogenous hamstring tendon at 1 month and 4 months, respectively, after injury. For the remaining two patients with total ACL resection, second-staged ACL reconstruction was already planned at the time of total ACL resection because subsequent instability of the knee was inevitable. After achieving pain relief and full range of motion, ACL reconstruction was performed in the same manner. Postoperatively, the side-to-side difference in anterior laxity at manual force using a KT-2000 arthrometer (MEDmetric Corp., San Diego, CA, USA) was 1.0 ± 0.8 mm (range, 0–2 mm). The pivot shift test showed glide in only one patient. All patients returned to their previous activity level without preoperative symptoms and knee instability.
Discussion
As previously reported, typical symptoms of mucoid degeneration of the ACL include knee pain during deep flexion and painful limitation of motion.3, 4, 5, 8, 9 Although the causes of pain in mucoid degeneration of the ACL remain unknown,3, 4, 8 it is well established that resection of the degenerated portion of the ACL leads to resolution of symptoms.1, 2, 3, 4, 5, 6, 7, 8, 9 Kim et al4 and Narvekar and Gajjar8 reported that partial resection of the hypertrophied posterolateral (PL) portion provided effective symptom relief, probably due to the removal of the mechanical impingement of the hypertrophied PL portion on the tibiofemoral joint. Kim et al4 found no lesions in the anteromedial (AM) bundle, whereas Cha et al2 reported that among 68 knees with mucoid degeneration of the ACL, both AM and PL bundles were affected in 69% of the knees, and the PL bundle only was affected in 31%. In the present series, both AM and PL bundles were affected in two cases. The interstitial degenerated portion of the ACL may be missed or underdiagnosed, given the difficulty in diagnosing the affected portion based on arthroscopic findings alone. Therefore, it is doubtful whether partial resection would completely relieve the preoperative symptoms.
The issue of subsequent ACL reconstruction for postoperative instability is also debatable.2, 4, 5 It is apparent that the remaining ACL fibres after partial resection have insufficient mechanical strength to prevent excessive knee motion, such as tibial anterior translation and rotation. After total resection, this inability becomes more pronounced. Lintz et al5 reported a mean postoperative side-to-side difference of 8 mm (range, 5–13 mm) using Telos dynamic radiography (telos Arzt- und Krankenhausbedarf Gmbh, Hungen, Germany), and 55% of 29 patients showed a positive Lachman test postoperatively. Under such conditions, there is a high risk of “giving way” and concomitant intra-articular injury, particularly in active young patients. Indeed, one of our patients who underwent partial resection of the ACL sustained a complete ACL tear during jogging. In general, it is unusual for people with normal ACL function to sustain ACL injuries when jogging. In recent years, the technique of ACL reconstruction has been refined, and good clinical results have been reported.10 Thus, early ACL reconstruction should be performed after ACL resection to regain normal knee stability, particularly in young and active patients.
Conclusion
Considering the rupture of residual ACL fibres after partial resection and the inevitability of total ACL resection due to degeneration of the entire ligament, early ACL reconstruction should be conducted in young and active patients.
Conflicts of interest
All contributing authors declare no conflicts of interest.
References
- 1.Kumar A., Bickerstaff D.R., Grimwood J.S., Suvarna S.K. Mucoid cystic degeneration of the cruciate ligament. J Bone Joint Surg Br. 1999;81:304–305. doi: 10.1302/0301-620x.81b2.9243. [DOI] [PubMed] [Google Scholar]
- 2.Cha J.R., Lee C.C., Cho S.D., Youm Y.S., Jung K.H. Symptomatic mucoid degeneration of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2012;21:658–663. doi: 10.1007/s00167-012-1991-9. [DOI] [PubMed] [Google Scholar]
- 3.Fealy S., Kenter K., Dines J.S., Warren R.F. Mucoid degeneration of the anterior cruciate ligament. Arthroscopy. 2001;17:e37. doi: 10.1053/jars.2001.26878. [DOI] [PubMed] [Google Scholar]
- 4.Kim T.H., Lee D.H., Lee S.H., Kim J.M., Kim C.W., Bin S.I. Arthroscopic treatment of mucoid hypertrophy of the anterior cruciate ligament. Arthroscopy. 2008;24:642–649. doi: 10.1016/j.arthro.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 5.Lintz F., Dejour D., Pujol N., Boisrenoult P., Beaufils P. Mucoid degeneration of the anterior cruciate ligament: selecting the best treatment option. Orthop Trauma Surg Res. 2010;96:400–406. doi: 10.1016/j.otsr.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 6.Lintz F., Pujol N., Boisrenoult P., Bargoin K., Beaufils P., Dejour D. Anterior cruciate ligament mucoid degeneration: a review of the literature and management guidelines. Knee Surg Sports Traumatol Arthrosc. 2011;19:1326–1333. doi: 10.1007/s00167-011-1433-0. [DOI] [PubMed] [Google Scholar]
- 7.McIntyre J., Moelleken S., Tirman P. Mucoid degeneration of the anterior cruciate ligament mistaken for ligamentous tears. Skeletal Radiol. 2001;30:312–315. doi: 10.1007/s002560100336. [DOI] [PubMed] [Google Scholar]
- 8.Narvekar A., Gajjar S. Mucoid degeneration of the anterior cruciate ligament. Arthroscopy. 2004;20:141–146. doi: 10.1016/j.arthro.2003.11.030. [DOI] [PubMed] [Google Scholar]
- 9.Nishimori M., Sumen Y., Sakaridani K. Mucoid degeneration of the anterior cruciate ligament—a report of two cases. Magn Reson Imaging. 2004;22:1325–1328. doi: 10.1016/j.mri.2004.08.023. [DOI] [PubMed] [Google Scholar]
- 10.Amano H., Toritsuka Y., Uchida R., Mae T., Ohzono K., Shino K. Outcome of anatomical double-bundle ACL reconstruction using hamstring tendons via an outside-in approach. Knee Surg Sports Traumatol Arthrosc. 2015;23:1222–1230. doi: 10.1007/s00167-014-2950-4. [DOI] [PubMed] [Google Scholar]