Abstract
Ligament balancing is one of the most important surgical techniques for successful total knee arthroplasty. It has traditionally been recommended that medial and lateral as well as flexion and extension gaps are equal. This article reviews the relevant literature and discusses the clinical importance of the aforementioned gaps. Current evidence indicates that achieving medial stability throughout the range of motion should be a high priority in ligament balancing in total knee arthroplasty. Finally, the medial stabilising surgical technique, which aims to achieve good medial stability in posterior cruciate-retaining total knee arthroplasty, is introduced.
Keywords: alignment, biomechanics, implant design, ligament balancing, total knee arthroplasty
Introduction
Total knee arthroplasty (TKA) involves resection of the medial and lateral menisci; moreover, the anterior cruciate ligament is usually resected, and the posterior cruciate ligament (PCL) is sometimes sacrificed. Therefore, knee stability should be achieved by the remaining ligamentous structures and articular surface geometry. Varus–valgus and rotational stability can be obtained mainly by proper tensioning of collateral and capsular ligaments.1 Therefore, surgical technique is critical for maintaining knee stability after TKA. This review article summarises previous reports and our studies, and discusses the most important factors in ligament balancing in TKA for osteoarthritis with varus deformity. Furthermore, a surgical technique for achieving adequate medial stability is introduced.
Principles of ligament balancing in TKA
Recent technological advances have enabled the accurate evaluation of soft tissue tension intraoperatively.2 However, the goal of soft tissue balancing is unclear. The classical concept of TKA is the achievement of equal medial and lateral gaps as well as equal flexion and extension gaps. However, this concept and whether it is possible in all cases remains controversial. In this article, the concept of ligament balancing is subcategorised into four parts: medial extension, medial flexion, lateral extension, and lateral flexion gaps.
Medial extension gap: how tight/loose can the knee be left?
How tight the knee can be left in extension intraoperatively to avoid postoperative flexion contracture remains unclear.3 A few studies have evaluated the relationship between intraoperative soft tissue tension and postoperative extension angle.4 Therefore, we evaluated the effect of extension gap on postoperative flexion contracture.5 In that study, intraoperative extension gap was evaluated in 75 knees with varus deformity after TKA using the NexGen LPS (Zimmer, Warsaw, IN, USA). The gap was measured with a femoral component using a tension device applying a distraction force of 178 N. A “component gap” was defined as the distance calculated by subtracting the selected thickness of the tibial component, including the polyethylene liner from the measured gap. Postoperative extension angle was measured by radiography. The knee was extended by the patient's own leg weight when the heel was raised 10 cm above the table. Flexion contracture was defined as the angle between the anatomical axis of the distal femur and the proximal tibia exceeding 5°. As a result, the tight group (medial component gap: <0 mm) showed 10% flexion contracture at 1 year postoperatively, the slightly tight group (medial component gap: 0–1 mm) still had 8% flexion contracture, and the group with knees with >1 mm medial component gap showed no flexion contracture. These results suggest that >1 mm laxity at the medial side after implantation is necessary to avoid flexion contracture.
How loose can the knee be left? First and foremost, the patient should not feel unstable. One benchmark would be the stability of normal knees. We previously measured knee laxity in normal knees by stress radiography and found that the medial side was opened 2.4° when a valgus stress of 147 N was applied.6 Ishii et al7 report that excellent clinical results were achieved in patients with 3–4° valgus laxity after TKA. These studies suggest that 2–4° laxity does not make patients feel unstable after TKA. Therefore, we suggest that medial extension laxity should be 1–3 mm to avoid flexion contracture and a feeling of instability (note that 1° medial laxity equals approximately 1.05 mm when the transverse diameter of the tibia is 80 mm).
Medial flexion gap: should it be adjusted to the extension gap?
A clinical study by Takayama et al8 indicates that tight flexion decreases range of motion after TKA. In addition, Jeffcote et al9 report that a flexion gap that is more than 2 mm greater than the extension gap decreases tibial forces in deep knee flexion. Therefore, flexion tightness should definitely be avoided, but how much looseness can be tolerated? In normal knees, at the medial side, knee laxity at flexion is almost equal to knee laxity in extension or slightly lax at 1–2 mm.10 We previously evaluated the effect of looseness in knee flexion on clinical outcome in 50 patients after TKA.11 Stress radiographs were taken while a lateral traction force of 50 N was applied perpendicular to the lower leg at 80° knee flexion, and the angle between a line tangential to the femoral condyles and a line through the tibial joint surface was measured. Patient satisfaction, symptoms, and knee function according to the new Knee Society scoring system were compared between the knees with ≥3° medial flexion laxity (medial loose group) and those with <3° medial flexion laxity (medial tight group). The scores of the medial loose and tight groups were 22 and 30 for satisfaction (out of 40), 16 and 20 for symptoms (out of 25), and 19 and 24 for standard activities (out of 30), respectively. Our fluoroscopic analysis also showed that a greater medial flexion gap caused larger anterior translation in knee flexion.12 On the basis of these studies, we recommend that the medial flexion gap should be close to the medial extension gap to achieve near-normal knee conditions as well as to improve postoperative function and patient satisfaction.
Lateral extension gap: should it be equal to the medial side?
Our study of normal knees shows that the lateral side should be 2.5° laxer than the medial side.6 Here, we discuss the case of osteoarthritic knees. We investigated knee laxity of osteoarthritic knees during TKA.13 In that study, the extension gap was measured after the distal part of the femur and proximal part of the tibia were resected. The patients were divided into the mild, moderate, and severe varus groups, which had preoperative hip–knee–ankle angles of <10°, 10–20°, and >20°, respectively. Measurements were made after removing osteophytes with a distraction force of 178 N. The results show that lateral soft tissue laxity increased with increasing severity of knee deformities. However, the medial side did not contract with increasing varus deformity. These results suggest that release on the medial side is unnecessary to make a space for implant replacement, even in severely deformed knees.
However, gap imbalance increases with increasing knee deformity up to 5 mm, prompting the determination of solutions for this imbalance. One of the classical methods for treating this situation is medial release. Krackow and Mihalko14 report that complete release of the medial collateral ligament (MCL) increases medial instability to 6.9° in full extension but to 13.4° in 90° of flexion. Furthermore, Mullaji et al15 state that releasing the MCL by 6–8 cm enlarges the medial extension and flexion gaps to 2.8 mm and 7.0 mm, respectively. These findings highlight the difficultly in managing extension imbalance by medial release alone; medial release would cause flexion instability in such cases.
Another important point is how much ligament imbalance can be left. Here, we focus on lift-off motion, because joint laxity theoretically increases the risk of lift-off motion. As lift-off motion of the femoral component possibly increases wear of the articular surface,16 it should be avoided after TKA. Hamai et al17 evaluated the effect of static knee instability by stress radiography on dynamic lift-off motion in fluoroscopy; the static varus–valgus laxity or differences in the laxities (i.e., imbalance) on the stress radiograph did not influence lift-off. Moreover, 90% of their patients had neutral alignment. We also evaluated effects of alignment and ligament balance on lift-off motion using computer simulations, which have recently been used and validated in the field of TKA.18, 19, 20, 21, 22, 23, 24 We used KneeSIM software (LifeMOD/KneeSIM 2010; LifeModeler Inc., San Clemente, CA, USA) to evaluate the effects of alignment and laxity on lift-off motion. Our results show that lift-off motion occurs with 5° varus alignment, or with a combination of 2° varus deformity and 2 mm lateral laxity.25 However, no lift-off motion was detected in knees with neutral to 1° varus malalignment even when the knees had 5 mm lateral laxity.
In summary, lateral laxity of 3° is close to normal conditions, which would not cause a feeling of instability. Lateral laxity theoretically increases the risk of lift-off motion, however, these risks would decrease with neutral alignment. Lateral laxity up to 5° in extension would be acceptable when neutral alignment is achieved.
Lateral flexion gap: should the objective be a rectangular gap?
The gap technique rotates the femoral component to achieve equal medial and lateral flexion gaps, forming a rectangular gap.26 Many clinical and cadaveric studies show that in normal knees, the lateral soft tissue is laxer than the medial soft tissue during flexion.6, 10, 27 Corroborating this, an magnetic resonance imaging study by Tokuhara et al28 shows that the lateral side is 4.6 mm laxer than the medial side. Kobayashi et al29 report that lateral laxity during knee flexion is related to good range of motion. Another clinical study by Seon et al30 shows no difference between knees with rectangular and nonrectangular flexion gaps with respect to knee score or range of motion. Our fluoroscopic analysis shows that lateral static instability at knee flexion is not related to lift-off motion during stairway up–down motion.11 Thus, to date, no studies indicate that a rectangular flexion gap can improve clinical results. Although a certain degree of lateral laxity in flexion is acceptable, there are not enough data to clarify the “safe range” of imbalance with regard to patient symptoms or implant longevity.
An important question is how much rotation of the femoral component is required to achieve a rectangular gap in clinical situations. Fehring31 reports that the femoral component is rotated by approximately 7–8° from the posterior condylar axis, whereas another study by Heesterbeek et al32 reports a rotation of 3–12°. After medial release, the femoral component tends to be in more internal rotation, which can be considered the worst-case scenario. If medial release is performed to produce an equal medial–lateral extension gap, the medial flexion gap usually increases more than the extension gap. Finally, the femoral component should be rotated internally to produce a rectangular flexion gap. Many studies report that an internally rotated femoral component causes patellofemoral problems33, 34, 35 and worsens knee function.36 As mentioned above, the medial soft tissue structure is not contracted (i.e., normal) even in severely deformed varus knees, whereas lateral soft tissue structure is stretched (i.e., abnormal). Therefore, if the normal side is released to adjust it to the abnormal side, another abnormal condition, i.e., medial instability, would occur.
On the basis of the available clinical and biomechanical studies, we recommend that the following principles should be followed for ligament balancing in TKA for varus knees: (1) the medial extension gap should be within 1–3 mm to avoid flexion contracture and a feeling of instability; (2) the medial flexion gap should be equal to the medial extension gap (or 1–2 mm larger), because this provides close to normal stability and a larger medial flexion gap would worsen knee function; (3) lateral extension laxity up to 3° does not cause severe clinical problems, or a risk of lift-off motion decreases with neutral alignment; and (4) the femoral component should not be internally rotated to adjust the flexion gap.
Alignment and ligament balancing
Bellemans et al37 report that the incidence of a natural limb alignment of ≥3° varus, which is termed constitutional varus, is approximately 32% in men and 17% in women. They suggest that aiming for neutral alignment can result in overcorrection in some patients and report that patients with a slight undercorrection have better function and pain scores than those with neutral alignment.38 Their cadaveric study shows that restoration of constitutional alignment in TKA leads to more physiological strain in the collateral ligaments.39 However, there is no definite way to determine the degree of constitutional varus in a patient, and the “safe zone” of varus alignment is unknown. Some clinical studies report that undercorrection does not worsen clinical results40 and that design modification can prevent wear problems even with malalignment.41, 42, 43 Nevertheless, concerns about tibial collapse in varus alignment remain.44, 45, 46
Howell et al47, 48 propose kinematic alignment as a way to maximally utilise ligamentous function. Better functional results were reported with kinematically aligned TKA than mechanically aligned TKA.49 Kinematically aligned TKA aims to reproduce the preosteoarthritic joint surface and does not align with any axis that has been used in the mechanical axis method. However, the precise preosteoarthritic morphology cannot be determined, and this technique incurs a risk of coronal malalignment, especially for patients with severe constitutional varus. Although these two new ideas have some unresolved problems,50 they pose the very interesting idea that postoperative knee function can be improved by preserving ligamentous tension rather than by sticking to the mechanical alignment.
Surgical technique: medial stabilising TKA
The abovementioned clinical and biomechanical studies indicate that achieving near-normal medial stability in knee extension and flexion is very important for better functional outcomes. By contrast, no results indicate that lateral stability should be close to the medial side. For longevity, aiming for neutral alignment still seems to be the best target, because there is no safe zone for malalignment. Here, we propose a medial stabilising technique for posterior cruciate-retaining TKA. This technique aims for neutral coronal alignment with near-normal medial stability.
Femoral bone resection
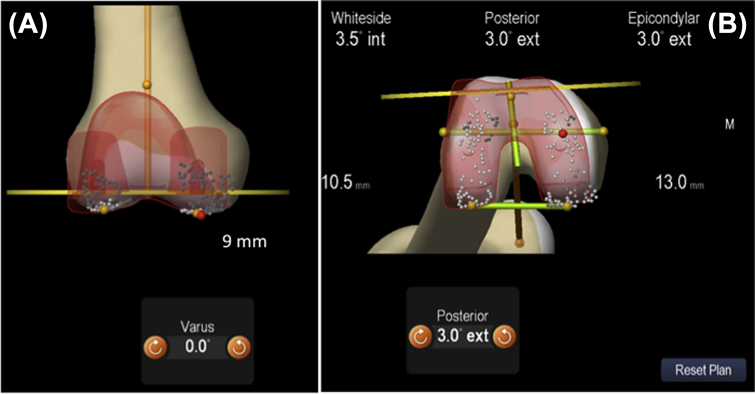
In the proposed technique, the distal femur is cut perpendicular to its mechanical axis. The level of bone cutting is adjusted so that the same thickness of bone as the implant is resected from the medial side. The thickness of the resected bone should be measured using callipers. Rotational alignment of the femoral component is adjusted to the surgical epicondylar axis to improve patellar tracking. The size of the femoral component is determined on the basis of the posterior reference. The amount of bone resected is very important for achieving proper tension of the MCL and PCL. Considering that the distal part of the femur is more worn than the posterior part,51, 52, 53 the size and location of the femoral component are determined so that the resected bone at the medial posterior condyle is 1–2 mm thicker than the implant thickness (Figure. 1). This procedure avoids excessive tension of the MCL or PCL throughout knee motion.
Figure 1.
Surgical planning of the femoral resection. (A) A 9-mm section (same thickness as that of the implant) is resected from the distal medial part. (B) A 13-mm section (1 mm thicker than the implant; NexGen CR Flex) is resected from the posterior medial part.
Tibial bone resection
The tibia should also be cut perpendicular to the mechanical axis in the coronal plane. Maintaining the preoperative tibial slope is important for achieving PCL function.54, 55, 56 However, to preserve the PCL attachment and avoid excessive slope, we may cut the proximal tibia with a posterior slope that is 2–3° less than the preoperative slope.57, 58 Approximately 10 mm of bone is resected from the most proximal part of the lateral tibial plateau, however, resection level and posterior slope should be changed according to the knee implant system. Rotational alignment of the tibial component is adjusted to the anteroposterior axis of the tibia (i.e., the Akagi line59) to avoid rotational mismatch between the femoral and tibial components.
Ligament balancing in extension
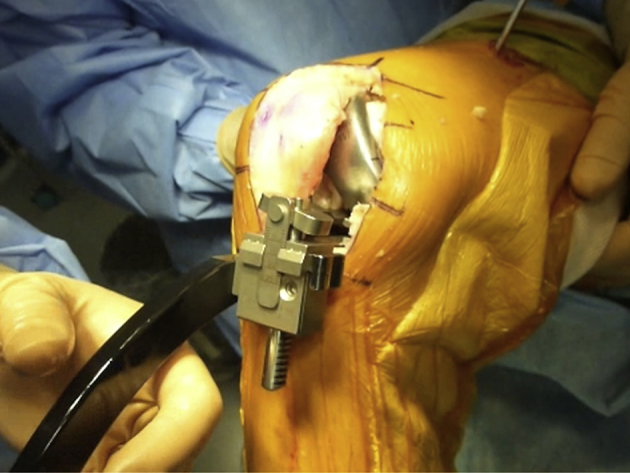
With the femoral trial component, the medial extension gap is measured using a small tensor applying a distraction force of 89 N (Figure. 2). The thickness of the tibial insert is selected so that an intercomponent gap of >1 mm is achieved in order to avoid flexion contracture.5 No medial release is usually required to make spaces for implants when adequate amounts of bones are resected from the femoral and tibial sides. Lateral laxity up to 3° can be left, because this does not cause severe clinical problems. Extensive medial release is not recommended for achieving an equal mediolateral extension gap, because this procedure would cause medial laxity in flexion.
Figure 2.

Extension gap measurement. The medial extension gap is measured using a small tensor. The tensor shows a gap of 11 mm, therefore, a 10-mm tibial component was selected to achieve a 1-mm intercomponent gap.
Ligament balancing in flexion
The proposed surgical technique might tighten the PCL when the proximal tibia is cut with a decreased posterior tibial slope. Because the PCL is more difficult to manage if loose, a relatively tight PCL is planned. The medial flexion gap is then measured using the tensor (Figure. 3); if the gap is smaller than that in extension, the tension of the PCL is too tight, because the PCL is the primary restraint for medial flexion stability.60 There are three options to resolve this situation: decreasing the anteroposterior size of the femoral component, increasing the tibial slope, or releasing the PCL. We prefer using knee systems that allow an adjustable anteroposterior size or tibial slope without additional bone resection, because the effect of PCL release is uncertain. Because the rotational alignment of the femoral component is adjusted to the bony landmark in this surgical technique, the lateral soft tissue may be laxer than the medial side in varus knees. When the PCL and MCL are retained, ligamentous release solely on the medial soft tissue cannot resolve this ligament imbalance. However, as described above, creating a rectangular flexion space is not always necessary for successful TKA.
Figure 3.
Flexion gap measurement. In this case, the medial flexion gap is 9 mm. The minus-size femoral component of the NexGen CR was selected to equalise flexion–extension gap (the minus-size femoral component is 2 mm smaller than the standard component).
With all trial components inserted, the roll back of the femoral component is examined (Figure. 4). In the normal knee, the femoral medial condyle contacts the posterior third of the tibial articular surface61; this can be a benchmark for normal PCL tension.
Figure 4.

Evaluation of posterior roll back of the medial condyle of the femoral component. The distance from the distal end of the femoral component to the anterior end of the tibial component is measured. When using NexGen CR flex size D and four components, a 10-mm step-off means that the femoral component contacts the posterior third of the tibial component.
Summary
Available clinical and biomechanical studies indicate that medial stability is very important for improving clinical results in TKA. Slight undercorrection of coronal alignment can decrease ligament imbalance but incurs a risk of varus malalignment. Therefore, aiming for near-normal medial stability with neutral alignment is one of the best solutions in TKA for medial osteoarthritis of the knee. Meticulous bone resection is very important for achieving this in posterior cruciate-retaining TKA, and the technique described herein is one example of a medial stabilising surgical technique.
Conflicts of interest
The authors have no conflicts of interest relevant to this article.
Funding/support
No financial or material support of any kind was received for the work described in this article.
References
- 1.Matsuda S., Miura H., Nagamine R. Knee stability in posterior cruciate ligament retaining total knee arthroplasty. Clin Orthop Relat Res. 1999;366:169–173. doi: 10.1097/00003086-199909000-00021. [DOI] [PubMed] [Google Scholar]
- 2.Mitsuyasu H., Matsuda S., Fukagawa S. Enlarged post-operative posterior condyle tightens extension gap in total knee arthroplasty. J Bone Joint Surg Br. 2011;93:1210–1216. doi: 10.1302/0301-620X.93B9.25822. [DOI] [PubMed] [Google Scholar]
- 3.Mitsuyasu H., Matsuda S., Miura H. Flexion contracture persists if the contracture is more than 15 degrees at 3 months after total knee arthroplasty. J Arthroplast. 2011;26:639–643. doi: 10.1016/j.arth.2010.04.023. [DOI] [PubMed] [Google Scholar]
- 4.Asano H., Muneta T., Sekiya I. Soft tissue tension in extension in total knee arthroplasty affects postoperative knee extension and stability. Knee Surg Sports Traumatol Arthrosc. 2008;16:999–1003. doi: 10.1007/s00167-008-0591-1. [DOI] [PubMed] [Google Scholar]
- 5.Okamoto S., Okazaki K., Mitsuyasu H. Extension gap needs more than 1-mm laxity after implantation to avoid post-operative flexion contracture in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014;22:3174–3180. doi: 10.1007/s00167-014-2858-z. [DOI] [PubMed] [Google Scholar]
- 6.Okazaki K., Miura H., Matsuda S. Asymmetry of mediolateral laxity of the normal knee. J Orthop Sci. 2006;11:264–266. doi: 10.1007/s00776-006-1009-x. [DOI] [PubMed] [Google Scholar]
- 7.Ishii Y., Matsuda Y., Noguchi H. Effect of soft tissue tension on measurements of coronal laxity in mobile-bearing total knee arthroplasty. J Orthop Sci. 2005;10:496–500. doi: 10.1007/s00776-005-0935-3. [DOI] [PubMed] [Google Scholar]
- 8.Takayama K., Matsumoto T., Kubo S. Influence of intra-operative joint gaps on post-operative flexion angle in posterior cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012;20:532–537. doi: 10.1007/s00167-011-1594-x. [DOI] [PubMed] [Google Scholar]
- 9.Jeffcote B., Nicholls R., Schirm A. The variation in medial and lateral collateral ligament strain and tibiofemoral forces following changes in the flexion and extension gaps in total knee replacement. A laboratory experiment using cadaver knees. J Bone Joint Surg Br. 2007;89:1528–1533. doi: 10.1302/0301-620X.89B11.18834. [DOI] [PubMed] [Google Scholar]
- 10.Ghosh K.M., Merican A.M., Iranpour F. Length-change patterns of the collateral ligaments after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012;20:1349–1356. doi: 10.1007/s00167-011-1824-2. [DOI] [PubMed] [Google Scholar]
- 11.Matsuda S. Paper Presented at 1st Congress of APKASS. April 14–15, 2014. Knee stability and implant design of total knee arthroplasty. Nara, Japan. [Google Scholar]
- 12.Nakamura S., Ito H., Yoshitomi H. Analysis of the flexion gap on in vivo knee kinematics using fluoroscopy. J Arthroplast. 2015;30:1237–1242. doi: 10.1016/j.arth.2015.01.046. [DOI] [PubMed] [Google Scholar]
- 13.Okamoto S., Okazaki K., Mitsuyasu H. Lateral soft tissue laxity increases but medial laxity does not contract with varus deformity in total knee arthroplasty. Clin Orthop Relat Res. 2013;471:1334–1342. doi: 10.1007/s11999-012-2745-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krackow K.A., Mihalko W.M. The effect of medial release on flexion and extension gaps in cadaveric knees: implications for soft-tissue balancing in total knee arthroplasty. Am J Knee Surg. 1999;12:222–228. [PubMed] [Google Scholar]
- 15.Mullaji A., Sharma A., Marawar S. Quantification of effect of sequential posteromedial release on flexion and extension gaps: a computer-assisted study in cadaveric knees. J Arthroplast. 2009;24:795–805. doi: 10.1016/j.arth.2008.03.018. [DOI] [PubMed] [Google Scholar]
- 16.Jennings L.M., Bell C.I., Ingham E. The influence of femoral condylar lift-off on the wear of artificial knee joints. Proc Inst Mech Eng H. 2007;221:305–314. doi: 10.1243/09544119JEIM215. [DOI] [PubMed] [Google Scholar]
- 17.Hamai S., Miura H., Okazaki K. No influence of coronal laxity and alignment on lift-off after well-balanced and aligned total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014;22:1799–1804. doi: 10.1007/s00167-013-2500-5. [DOI] [PubMed] [Google Scholar]
- 18.Morra E.A., Rosca M., Greenwald J.F. The influence of contemporary knee design on high flexion: a kinematic comparison with the normal knee. J Bone Joint Surg Am. 2008;90(suppl 4):195–201. doi: 10.2106/JBJS.H.00817. [DOI] [PubMed] [Google Scholar]
- 19.Colwell C.W., Jr., Chen P.C., D'Lima D. Extensor malalignment arising from femoral component malrotation in knee arthroplasty: effect of rotating-bearing. Clin Biomech (Bristol, Avon) 2011;26:52–57. doi: 10.1016/j.clinbiomech.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 20.Mizu-uchi H., Colwell C.W., Jr., Matsuda S. Effect of total knee arthroplasty implant position on flexion angle before implant-bone impingement. J Arthroplast. 2011;26:721–727. doi: 10.1016/j.arth.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 21.Mihalko W.M., Williams J.L. Total knee arthroplasty kinematics may be assessed using computer modeling: a feasibility study. Orthopedics. 2012;35:40–44. doi: 10.3928/01477447-20120919-56. [DOI] [PubMed] [Google Scholar]
- 22.Mizu-Uchi H., Colwell C.W., Jr., Fukagawa S. The importance of bony impingement in restricting flexion after total knee arthroplasty: computer simulation model with clinical correlation. J Arthroplast. 2012;27:1710–1716. doi: 10.1016/j.arth.2012.03.041. [DOI] [PubMed] [Google Scholar]
- 23.Morra E.A., Heim C.S., Greenwald A.S. Preclinical computational models: predictors of tibial insert damage patterns in total knee arthroplasty: AAOS exhibit selection. J Bone Joint Surg Am. 2012;94:e137. doi: 10.2106/JBJS.K.00914. (131–135) [DOI] [PubMed] [Google Scholar]
- 24.Kuriyama S., Ishikawa M., Furu M. Malrotated tibial component increases medial collateral ligament tension in total knee arthroplasty. J Orthop Res. 2014;32:1658–1666. doi: 10.1002/jor.22711. [DOI] [PubMed] [Google Scholar]
- 25.Matsuda S. Paper Presented at 2014 ICJR Pan Pacific Congress. July 16–19, 2014. Computer simulation in TKA. Kona, Hawaii, USA. [Google Scholar]
- 26.Dennis D.A., Komistek R.D., Kim R.H. Gap balancing versus measured resection technique for total knee arthroplasty. Clin Orthop Relat Res. 2010;468:102–107. doi: 10.1007/s11999-009-1112-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nowakowski A.M., Majewski M., Muller-Gerbl M. Measurement of knee joint gaps without bone resection: “physiologic” extension and flexion gaps in total knee arthroplasty are asymmetric and unequal and anterior and posterior cruciate ligament resections produce different gap changes. J Orthop Res. 2012;30:522–527. doi: 10.1002/jor.21564. [DOI] [PubMed] [Google Scholar]
- 28.Tokuhara Y., Kadoya Y., Nakagawa S. The flexion gap in normal knees. An MRI study. J Bone Joint Surg Br. 2004;86:1133–1136. doi: 10.1302/0301-620x.86b8.15246. [DOI] [PubMed] [Google Scholar]
- 29.Kobayashi T., Suzuki M., Sasho T. Lateral laxity in flexion increases the postoperative flexion angle in cruciate-retaining total knee arthroplasty. J Arthroplast. 2012;27:260–265. doi: 10.1016/j.arth.2011.04.025. [DOI] [PubMed] [Google Scholar]
- 30.Seon J.K., Song E.K., Park S.J. The use of navigation to obtain rectangular flexion and extension gaps during primary total knee arthroplasty and midterm clinical results. J Arthroplast. 2011;26:582–590. doi: 10.1016/j.arth.2010.04.030. [DOI] [PubMed] [Google Scholar]
- 31.Fehring T.K. Rotational malalignment of the femoral component in total knee arthroplasty. Clin Orthop Relat Res. 2000;380:72–79. doi: 10.1097/00003086-200011000-00010. [DOI] [PubMed] [Google Scholar]
- 32.Heesterbeek P.J., Jacobs W.C., Wymenga A.B. Effects of the balanced gap technique on femoral component rotation in TKA. Clin Orthop Relat Res. 2009;467:1015–1022. doi: 10.1007/s11999-008-0539-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Berger R.A., Crossett L.S., Jacobs J.J. Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res. 1998;356:144–153. doi: 10.1097/00003086-199811000-00021. [DOI] [PubMed] [Google Scholar]
- 34.Akagi M., Matsusue Y., Mata T. Effect of rotational alignment on patellar tracking in total knee arthroplasty. Clin Orthop Relat Res. 1999;366:155–163. doi: 10.1097/00003086-199909000-00019. [DOI] [PubMed] [Google Scholar]
- 35.Matsuda S., Miura H., Nagamine R. Effect of femoral and tibial component position on patellar tracking following total knee arthroplasty: 10-year follow-up of Miller–Galante I knees. Am J Knee Surg. 2001;14:152–156. [PubMed] [Google Scholar]
- 36.Kawahara S., Okazaki K., Matsuda S. Internal rotation of femoral component affects functional activities after TKA—survey with the 2011 Knee Society Score. J Arthroplast. 2014;29:2319–2323. doi: 10.1016/j.arth.2013.11.017. [DOI] [PubMed] [Google Scholar]
- 37.Bellemans J., Colyn W., Vandenneucker H. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? the concept of constitutional varus. Clin Orthop Relat Res. 2012;470:45–53. doi: 10.1007/s11999-011-1936-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vanlommel L., Vanlommel J., Claes S. Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc. 2013;21:2325–2330. doi: 10.1007/s00167-013-2481-4. [DOI] [PubMed] [Google Scholar]
- 39.Delport H., Labey L., Innocenti B. Restoration of constitutional alignment in TKA leads to more physiological strains in the collateral ligaments. Knee Surg Sports Traumatol Arthrosc. 2014 doi: 10.1007/s00167-014-2971-z. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 40.Parratte S., Pagnano M.W., Trousdale R.T. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am. 2010;92:2143–2149. doi: 10.2106/JBJS.I.01398. [DOI] [PubMed] [Google Scholar]
- 41.Nishikawa K., Okazaki K., Matsuda S. Improved design decreases wear in total knee arthroplasty with varus malalignment. Knee Surg Sports Traumatol Arthrosc. 2014;22:2635–2640. doi: 10.1007/s00167-013-2506-z. [DOI] [PubMed] [Google Scholar]
- 42.Matsuda S., Miura H., Nagamine R. Changes in knee alignment after total knee arthroplasty. J Arthroplast. 1999;14:566–570. doi: 10.1016/s0883-5403(99)90078-5. [DOI] [PubMed] [Google Scholar]
- 43.Matsuda S., Whiteside L.A., White S.E. The effect of varus tilt on contact stresses in total knee arthroplasty: a biomechanical study. Orthopedics. 1999;22:303–307. doi: 10.3928/0147-7447-19990301-06. [DOI] [PubMed] [Google Scholar]
- 44.Fang D.M., Ritter M.A., Davis K.E. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplast. 2009;24:39–43. doi: 10.1016/j.arth.2009.04.034. [DOI] [PubMed] [Google Scholar]
- 45.Wong J., Steklov N., Patil S. Predicting the effect of tray malalignment on risk for bone damage and implant subsidence after total knee arthroplasty. J Orthop Res. 2011;29:347–353. doi: 10.1002/jor.21221. [DOI] [PubMed] [Google Scholar]
- 46.Halder A., Kutzner I., Graichen F. Influence of limb alignment on mediolateral loading in total knee replacement: in vivo measurements in five patients. J Bone Joint Surg Am. 2012;94:1023–1029. doi: 10.2106/JBJS.K.00927. [DOI] [PubMed] [Google Scholar]
- 47.Howell S.M., Kuznik K., Hull M.L. Results of an initial experience with custom-fit positioning total knee arthroplasty in a series of 48 patients. Orthopedics. 2008;31:857–863. doi: 10.3928/01477447-20080901-15. [DOI] [PubMed] [Google Scholar]
- 48.Howell S.M., Papadopoulos S., Kuznik K.T. Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg Sports Traumatol Arthrosc. 2013;21:2271–2280. doi: 10.1007/s00167-013-2621-x. [DOI] [PubMed] [Google Scholar]
- 49.Dossett H.G., Estrada N.A., Swartz G.J. A randomised controlled trial of kinematically and mechanically aligned total knee replacements: two-year clinical results. Bone Joint J. 2014;96-B:907–913. doi: 10.1302/0301-620X.96B7.32812. [DOI] [PubMed] [Google Scholar]
- 50.Ishikawa M., Kuriyama S., Ito H. Kinematic alignment produces near-normal knee motion but increases contact stress after total knee arthroplasty: a case study on a single implant design. Knee. 2015;22:206–212. doi: 10.1016/j.knee.2015.02.019. [DOI] [PubMed] [Google Scholar]
- 51.Howell S.M., Howell S.J., Hull M.L. Assessment of the radii of the medial and lateral femoral condyles in varus and valgus knees with osteoarthritis. J Bone Joint Surg Am. 2010;92:98–104. doi: 10.2106/JBJS.H.01566. [DOI] [PubMed] [Google Scholar]
- 52.Nam D., Lin K.M., Howell S.M. Femoral bone and cartilage wear is predictable at 0 degrees and 90 degrees in the osteoarthritic knee treated with total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014;22:2975–2981. doi: 10.1007/s00167-014-3080-8. [DOI] [PubMed] [Google Scholar]
- 53.Matsuda S., Miura H., Nagamine R. Anatomical analysis of the femoral condyle in normal and osteoarthritic knees. J Orthop Res. 2004;22:104–109. doi: 10.1016/S0736-0266(03)00134-7. [DOI] [PubMed] [Google Scholar]
- 54.Matsuda S., Miura H., Nagamine R. Posterior tibial slope in the normal and varus knee. Am J Knee Surg. 1999;12:165–168. [PubMed] [Google Scholar]
- 55.Singerman R., Dean J.C., Pagan H.D. Decreased posterior tibial slope increases strain in the posterior cruciate ligament following total knee arthroplasty. J Arthroplast. 1996;11:99–103. doi: 10.1016/s0883-5403(96)80167-7. [DOI] [PubMed] [Google Scholar]
- 56.Seo S.S., Kim C.W., Kim J.H. Clinical results associated with changes of posterior tibial slope in total knee arthroplasty. Knee Surg Relat Res. 2013;25:25–29. doi: 10.5792/ksrr.2013.25.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Feyen H., Van Opstal N., Bellemans J. Partial resection of the PCL insertion site during tibial preparation in cruciate-retaining TKA. Knee Surg Sports Traumatol Arthrosc. 2013;21:2674–2679. doi: 10.1007/s00167-012-1997-3. [DOI] [PubMed] [Google Scholar]
- 58.Matziolis G., Mehlhorn S., Schattat N. How much of the PCL is really preserved during the tibial cut? Knee Surg Sports Traumatol Arthrosc. 2012;20:1083–1086. doi: 10.1007/s00167-011-1696-5. [DOI] [PubMed] [Google Scholar]
- 59.Akagi M., Oh M., Nonaka T. An anteroposterior axis of the tibia for total knee arthroplasty. Clin Orthop Relat Res. 2004;420:213–219. doi: 10.1097/00003086-200403000-00030. [DOI] [PubMed] [Google Scholar]
- 60.Kadoya Y., Kobayashi A., Komatsu T. Effects of posterior cruciate ligament resection on the tibiofemoral joint gap. Clin Orthop Relat Res. 2001;391:210–217. doi: 10.1097/00003086-200110000-00023. [DOI] [PubMed] [Google Scholar]
- 61.Fukagawa S., Matsuda S., Tashiro Y. Posterior displacement of the tibia increases in deep flexion of the knee. Clin Orthop Relat Res. 2010;468:1107–1114. doi: 10.1007/s11999-009-1118-x. [DOI] [PMC free article] [PubMed] [Google Scholar]