Abstract
Background
Medial patella-femoral ligament reconstruction (MPFLR) using hamstring tendon is the main procedure for recurrent patellar instability. The anterior half of the peroneus longus tendon (AHPLT) has been proven to be a useful alternate to the hamstring tendon in knee ligament reconstruction. The purpose of this study was to evaluate the clinical outcome of MPFLR using the new graft.
Methods
Forty-five patients with recurrent patellar instability received MPFLR using the AHPLT. Tibial tubercle transfer and lateral release were also performed. Follow-ups were performed at 12 months and 24 months postoperatively, and computed tomography was performed immediately following the operation and at follow-up. The passive patella glide test was performed prior to surgery, during the operation, and at each follow-up point. Knee function was evaluated preoperatively and postoperatively using the International Knee Documentation Committee, Lysholm, Kujala, and Tegner rating scales.
Results
Forty patients were followed for 2 years and received complete serial computed tomography examinations and functional evaluations. The correction of the static patellar position remained through the follow-ups. Functional evaluations at 2 years revealed statistical significant improvement over preoperative status, with International Knee Documentation Committee subjective score, Lysholm score, Kujala score, and Tegner score.
Conclusion
AHPLT is a promising alternative graft for MPFLR, together with lateral release and tibial tubercle transfer, satisfactory static patellar position, and functional outcomes have been achieved in the treatment of recurrent patellar dislocation in adults.
Level of evidence
Level IV, case series.
Keywords: anterior half of the peroneus longus tendon, functional outcomes, medial patello-femoral ligament reconstruction, recurrent patellar instability
Introduction
The optimal surgical treatment for patellar dislocation or instability is still controversial. The medial patella-femoral ligament (MPFL) provides approximately 60% of the total medial restraining force against lateral patellar displacement1 and is often damaged or deficient during patellar dislocation.2, 3, 4 MPFL reconstruction (MPFLR), which directly addresses the deficiencies of the medial restraining structure, is one of the primary methods in the treatment of patellar instability. Many different methods of MPFLR have been reported in literature. Among these techniques, MPFLR with a hamstring tendon graft is the treatment of choice.5 However, harvesting the hamstring tendon is sometimes technically demanding6, 7 and incision near the knee causes cosmetic concern in most of the patients. Thus, attention has been transferred to the anterior half of the peroneus longus tendon (AHPLT), which is superficial in the distal leg and can be easily harvested, and results in an incision that causes little cosmetic concern. When the feasibility of using the AHPLT as a graft had been proven in a previous study,8 it became the mainstream graft choice for MPFLR in our clinical practice.
This study was conducted to evaluate the clinical outcomes of MPFLR as a combined procedure using the AHPLT in treating recurrent patellar instability. Our hypothesis was that MPFLR using the AHPLT would yield satisfactory clinical results.
Materials and methods
This is a prospective study. From 2010 to 2012, 45 adult patients with recurrent patellar instability underwent MPFLR using the AHPLT. Tibial tubercle (TT) anteromedialisation and lateral release were performed in all patients. All the procedures were operated by the senior author.
The indications for MPFLR with the AHPLT in this study were recurrent patellar dislocation or instability in a patient. All patients had more than two episodes of dislocation or one episode of dislocation plus multiple episodes of instability (lateral excursion of the patella without dislocation). All patients with a previous surgery for patellar instability, those with patellar or lateral femoral condyle fractures, patella alta, or patella baja were excluded for this study.
Prior to the surgery, patellar apprehension, lateral translation (translation of up to more than one-half of the patella width considered abnormal), and soft versus firm endpoint to lateral patellar translation at a 30°-knee flexion were evaluated. Congruence angle, lateral patella angle, patella tilt angle, lateral translation, and the TT-trochlea groove (TT-TG) distance9, 10, 11 were evaluated on the computed tomography (CT) scan. MPFL sprains or tears and patellofemoral joint chondromalacia were evaluated using magnetic resonance imaging. The International Knee Documentation Committee (IKDC) subjective score, Kujala score, Lysholm score, and Tegner score were also documented.
The indication for TT medialisation in this study was a TT-TG distance of at least 15 mm. Patients with high-riding patella needing TT distalisation, severe trochlear dysplasia12 that needed trochlear plasty, and severe femoral anteversion or valgus knee deformity were excluded from this study.
Surgical technique
Graft preparation
Surgery was carried out with the patient under general anaesthesia. The AHPLT was harvested from the same leg with the one-incision tendon-stripping technique or the two-incision tendon-peeling technique as reported by Zhao and Huangfu.8 After scraping off the muscle, both ends of the tendon were sutured with a #1 absorbable suture in a whip-stitch style.
MPFLR
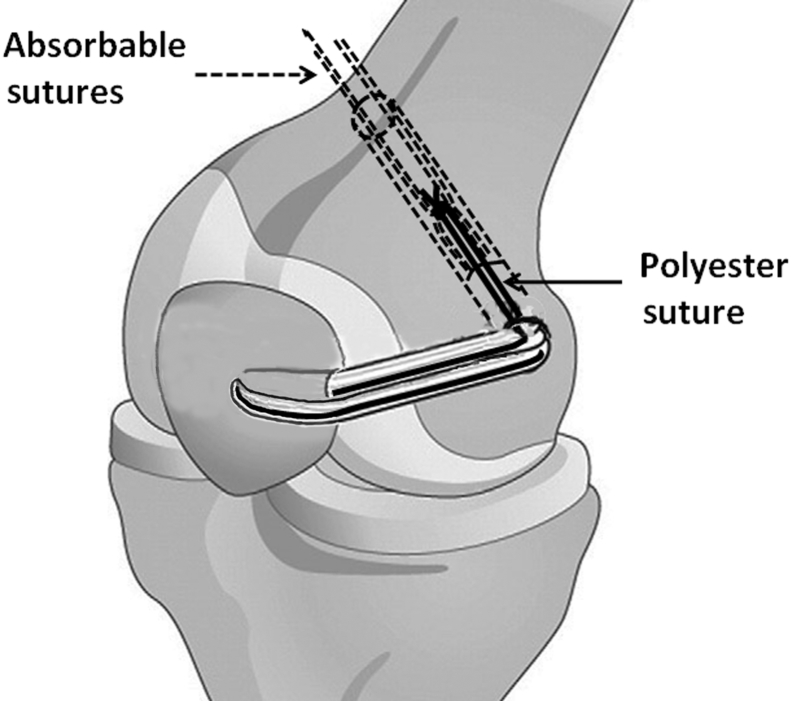
At 90° of knee flexion, the superior and inferior poles and the widest point of the patella were palpated. A 1-cm longitudinal incision was made at the medial side of the patella at a level near its broadest point. A 2.5-mm Kirshner wire was then drilled transversely through the patella, just distal to the maximal width line. The guide wire was then overdrilled with a drill width corresponding to the width of the tendon (Figure 1). A 2-cm-long longitudinal incision was made over the medial epicondyle to expose it. A 6-mm-wide tunnel was created 5 mm posterior and 5 mm proximal to the medial epicondyle. The tunnel was made in the distal medial towards the proximal lateral and exited from the lateral side of the femoral shaft instead of from the lateral femoral condyle to reduce joint disturbance.
Figure 1.
Medial patella-femoral ligament reconstruction with polyester suture augmentation through oblique patellar tunnel.
The graft, accompanied by one #5 Eithibond (Ethicon, Somerville, NJ, USA) polyester thread, was passed through the patellar tunnel medially to laterally and pulled back over the anterior surface of the patella. The Eithibond polyester thread was used as an augmentation, as reported by Xie et al.13 Lateral release was performed with tissue scissors by pulling the patella medially with the graft. Both ends of the graft and the thread limbs were then passed subcutaneously from the medial patella incision to the medial femoral epicondyle incision. With the graft ends adjusted side by side, the absorbable sutures from the two ends were tied together to form a knot about 1 cm from the graft ends. The graft was pulled into the femoral tunnel by pulling the absorbable sutures (Figure 1). The knee was then brought to full flexion several times to accommodate the graft. At 45° of knee flexion, the graft was fixed with an 8-mm nonmetal interference screw.
After graft fixation, lateral patellar glide and end point examination in 30° knee flexion were taken immediately during the operation to ensure a normal lateral patella glide and firm end point in all the patients.
TT transfer
This procedure is a modification of Fulkerson's osteotomy.14 A 4-cm longitudinal incision was first made along the lateral edge of the TT. Through this movable skin window, an oblique osteotomy from the medial edge of the tibial insertion of the patella tendon to the lateral ridge of the proximal tibia was performed, to detach the TT from the proximal tibia. The TT fragment was 6–8 cm in length and had a tapering distal end. The proximal end of the bone fragment was transferred anteromedially, with the distal tapering end left in place. The purpose of this medialisation was to reduce the TT-TG distance to 5–10 mm. Two Kirshner wires perpendicular to the osteotomy surface and one along the sagittal plane were used to fix the transferred TT in the desired position (Figure 2).
Figure 2.
Tibial tubercle anteromedialisation.
Postoperative treatment and clinical evaluation
A hinged brace was used for 6 weeks and locked in extension while walking. Partial to full weight bearing was allowed immediately after operation. Range-of-motion exercises began immediately, but the knee flexion angle was restricted to 45°, 90°, and 120° in the 1st, 2nd, and 3rd 2-week periods following the operation, respectively. Straight-leg raising, vastus medialis exercises, and proprioception training began 6 weeks following the operation; running and agility training began after 4 months after operation.
CT examinations were performed immediately following the operation and at 12 months and 24 months to evaluate the position of the patella. The function of the knee was evaluated at 12 months and 24 months postoperatively using the IKDC, Kujala, Lysholm, and Tegner rating scales. Foot and ankle functions were assessed using the American Orthopaedic Foot and Ankle Society scale and the Foot and Ankle Disability Index.
CT imaging evaluation
Preoperative and postoperative measurements from the CT images were taken and analysed by the senior author. In the CT images obtained prior to and following the operation, the congruence angle, lateral patella angle, patella tilt degree, and lateral patellar translation were measured. The images were measured using a Digimizer software system (Digimizer, version 3.1.2.0; MedCalc Software, Mariakerke, Belgium) as described by Zhao et al.15 First, a proximal standard image and a distal standard image (DSI) were defined. Measurements were then taken by copying the reference point or line from the proximal standard image to the DSI. The TT-TG distance was measured using the most proximal cut through the TT and the DSI.
Statistical analysis
For clinical examination data, the preoperative and final results were compared using the paired Student t test or the Chi-square test. For the CT examination data, an analysis of variance analysis was first performed using the F-test. When significant differences were observed using the F-test, multiple comparisons between the results from each pair of time points were performed using the Newman–Keuls q test. One episode of redislocation and multiple episodes of instability were considered as failure. For all the statistical analysis, SPSS software (version 14; SPSS Inc., Chicago, IL, USA) was used, with the significance level set at 0.05.
Results
The senior author performed each operation and performed the preoperative, intraoperative, and postoperative clinical examinations. Complete follow-up was achieved for 40 patients receiving complete serial CT examinations and functional evaluations (Table 1). Three patients were lost at follow-up because of broken contact, and two were excluded because they were unable to attend the 2-year follow up due to travel inconveniency.
Table 1.
Patient demographic data.
| Variables | n = 40 |
|---|---|
| Male/female (n) | 4/36 |
| Age (y, range) | 26.1 ± 6.9 (15–45) |
| Left side/right side (n) | 17/23 |
| Duration of dislocation (mo, range) | 31.0 ± 4.7 (8–60) |
| No. of dislocations (value, range) | 2.4 ± 1.8 (1–5) |
| No. of instability (value, range) | 12.9 ± 5.9 (0–20) |
The average preoperative and postoperative American Orthopaedic Foot and Ankle Society scores for all of the patients were 97.4 ± 2.0 and 97.2 ± 1.6, respectively (p = 0.85), and similar results were conducted in the Foot and Ankle Disability Index (96.8 ± 2.2 vs. 96.9 ± 2.5, p = 0.91). No donor site morbidities were observed.
In the preoperative magnetic resonance imaging examination, MPFL sprain or tear was observed in 31 of the 40 patients in the case series. All patients showed chondromalacia in the patella and lateral femoral trochlea. The preoperative TT-TG distance were 18.7 ± 3.1 mm, the postoperative TT-TG distance were 6.9 ± 2.1 mm.
Clinical examination
Apprehension test
Prior to the operation, 28 patients in the cohort had positive apprehension tests. Following the operation, except for one patient showing a positive apprehension test, all the other patients showed a negative apprehension test at either the 12-month or 24-month time point. There was a statistically significant difference between the preoperative and final examination results (Table 2).
Table 2.
Results of the apprehension test and lateral patellar translation examination.
| No. of patients with positive apprehension test | Time | n = 40 | |
| Preoperative | 28 | ||
| 12 mo | 1 | ||
| 24 mo | 1 | ||
| χ2 = 45.433, p < 0.001a | |||
| No. of patients with lateral patella translation | Normal | Abnormal | |
| Preoperative | 0 | 40 | |
| 12 mo | 38 | 2 | |
| 24 mo | 38 | 2 | |
| χ2 = 72.8, p < 0.001a | |||
Comparative results between preoperative and final follow-up data.
Lateral patellar translation
Prior to the operation, all patients exhibited abnormal lateral translation. Following the operation, a total of three and four patients exhibited abnormal lateral patellar translation at the 12-month and 24-month time point, respectively. Statistically significant differences were observed between the preoperative and final examination results (Table 2).
Firm endpoint in lateral translation examination
Prior to the operation, no patient exhibited a firm endpoint in the lateral patellar translation examination. Following the operation, all patients exhibited firm end points, at either the 12 months or 24 months.
CT examination
The analysis indicated a statistically significant difference (p < 0.05) between the intertime-point variance and the intratime-point variance with respect to the congruence angle, lateral patella angle, patella tilt angle, and lateral patellar translations.
No significant deterioration of the patellar position and rotation regarding these three angles and lateral patellar translation was observed based on analyses at each follow-up time point. With respect to the preoperative and 24-month measurement results of the three angles and the lateral patellar translation, statistically significant differences were observed (Table 3).
Table 3.
Computed tomography evaluation results.
| Follow-up time point | Mean ± SD |
p between each pair of time points |
||||
|---|---|---|---|---|---|---|
| 0 mo | 12 mo | 24 mo | 60 mo | |||
| Congruence angle (°) | Preoperative | −26.2 ± 16.1 | + | + | + | + |
| 0 mo | 4.9 ± 3 .3 | − | − | − | ||
| 12 mo | 4.0 ± 4.9 | − | − | |||
| 24 mo | 3.8 ± 5.1 | − | ||||
| Lateral patella angle (°) | Preoperative | −15.9 ± 11.8 | + | + | + | + |
| 0 mo | 5.3 ± 4.8 | − | − | − | ||
| 12 mo | 4.1 ± 3.9 | − | − | |||
| 24 mo | 3.1 ± 4.9 | − | ||||
| Patella tilt angle (°) | Preoperative | 21.1 ± 15.3 | + | + | + | + |
| 0 mo | −1.1 ± 3.9 | − | − | − | ||
| 12 mo | 1.9 ± 6.4 | − | − | |||
| 24 mo | 3.2 ± 7.2 | − | ||||
| Lateral patella translation (mm) | Preoperative | 15.4 ± 5.9 | + | + | + | + |
| 0 mo | 1.6 ± 2.1 | − | − | − | ||
| 12 mo | 2.6 ± 3.1 | − | − | |||
| 24 mo | 3.5 ± 4.6 | − | ||||
+ = p < 0.05; – = p > 0.05; SD = standard deviation.
Functional outcomes
With respect to the 12-month and 24-month rating outcome of the IKDC subjective score, Lysholm score, Kujala score, or Tegner score, statistically significant improvements were observed when compared with the preoperative outcome (Table 4). Finally, no patient experienced episodes of redislocation, and one patient experienced multiple episodes of patellar instability, albeit without redislocation to result in a failure rate of 2.5%.
Table 4.
Functional score (n = 40).
| Preoperative | 12 mo | 24 mo | |
|---|---|---|---|
| IKDC subjective score | 52.1 ± 7.1 | 81.9 ± 6.6 | 85.1 ± 5.3 |
| t = 27.430, p < 0.001a | |||
| Lysholm score | 58.0 ± 4.5 | 89.8 ± 3.7 | 94.3 ± 2.9 |
| t = 42.884, p < 0.001a | |||
| Kujala score | 73.8 ± 6.5 | 94.9 ± 5.8 | 98.7 ± 5.6 |
| t = 18.355, p < 0.001a | |||
| Tegner score | 3.6 ± 1.9 | 6.1 ± 2.0 | 6.6 ± 1.9 |
| t = 7.061, p < 0.001a |
IKDC = International Knee Documentation Committee.
Comparative results between preoperative and follow-up data.
Discussion
The results of this study show that after MPFLR using the AHPLT, satisfactory clinical findings were obtained, and the position of the patella can be corrected and maintained. With regard of the functional recovery, MPFLR using the AHPLT also achieved satisfactory results. A statistically significant functional improvement was observed with respect to the IKDC, Lysholm, Kujala, and Tegner scores, which indicates that this technique was qualified. When redislocation and multiple episodes of instability were considered failure, a failure rate of only 2.5% was observed at 2 years, which favours this technique.
Because the MPFL is the main restraining structure against lateral patellar displacement and is often deficient during patellar dislocation, MPFLR, which directly addresses this insufficient structure, has gained popularity in recent years. Many MPFLR techniques have been reported in literature. The clinical results are encouraging, with quite low or even no recurrence.5 Among these techniques, a free hamstring graft is the most often used tissue for MPFLR.4, 16, 17, 18, 19, 20, 21
The PLT is superficial in the distal leg and can be easily harvested. It takes only 5–10 minutes to harvest the AHPLT.8 In the biomechanical study regarding the AHPLT and the hamstring tendons, the AHPLT showed similar strength to semitendinosus tendon (ST), with a length a little bit shorter than the ST.8 Thus, the PLT may represent a potential autograft. Moreover, when TT transfer is needed, in order to avoid multiple incisions or a long incision near the TT the AHPLT is considered as an ideal graft for MPFLR.
The use of additional procedures combined with MPFLR is controversial. Lateral release may reduce the lateral pulling force during knee flexion and may give the reconstructed medial structure an improved biomechanical advantage for healing and remoulding. Medial TT transfer was performed in patients with a TT-TG distance greater than 15 mm, to reduce the TT-TG distance to 5–10 mm. This may also be considered excessive given that in the normal population the TT-TG distance may be greater than this value. No medial dislocation, subluxation, or medial overstressing was observed due to this apparent overcorrection of the lateral release and medial TT transfer.10
It is noteworthy that polyester suture augmentation was used in MPFLR. In previous studies, the stability status of the patella always deteriorated over time,15, 22 which reflected a loss in the corrected position of the patella and a reoccurrence of abnormal passive lateral patellar glide. However, when polyester suture augmentation was used, the stability status of the patella could be maintained.13 After MPFLR with the AHPLT or ST, the graft tissue experiences a decrease in strength, which causes the stability status of the patella to deteriorate after MPFLR. Besides, the initial adequate strength of the reconstructed MPFL may not be the same during the possible remoulding period of the tendon and may not be the same as its final strength. Thus, a protection effect for the reconstructed structure was expected during its weak period by adding a stiff material within the graft. In the present study, all of the patients maintained the firm end point obtained in the operation and the corrected position of the patella at the final follow-up.
The primitive MPFL inserts on the medial side of the patella in a fan-type manner.23 MPFLR with a narrow graft insertion site on the medial patella may not restore the anatomy of the primitive MPFL. MPFLR with a wide graft insertion site along the medial patella may be better.24, 25 However, the advantage of this type of wide patellar insertion MPFLR still needs to be explored and verified.
There were several limitations in this study. First of all, the clinical examinations were dependent on the examiner and may be inaccurate and the results may therefore not be so reliable with respect to the differences between the preoperative and postoperative results. Secondly, bias may also have been present in the measurements of the CT images. Also, the number of the patients in this study was limited, and lack of a control group gives this study less strength on an evidence level. Furthermore, the TT medialisation, which was performed in all cases, may take the primary effect on the satisfactory clinical results, and shield the role of MPFLR, although we consider the reconstructed MPFL as the main structure maintaining the corrected position of the patella. A study including patients undergoing only MPFLR, together with a comparison with the ST graft, measurement of dynamic patella tracking, and long-term follow-up, may be better to evaluate the effect of MPFLR using AHPLT.
Conclusion
AHPLT is a promising alternative graft for MPFL reconstruction, together with lateral release and TT transfer, this combined procedure could achieve satisfactory static patellar position and functional outcome in the treatment of recurrent patellar instability and prevention of dislocation recurrence.
Conflicts of interest
The authors have no conflicts of interest relevant to this article.
Funding/support
This research was funded by the National Natural Science Foundation of China, Grant Number 31400800. The study was performed at the Department of Sports Medicine, Shanghai Sixth People's Hospital, Shanghai Jiaotong University, 600 Yishan Road, Shanghai, China.
References
- 1.Desio S.M., Burks R.T., Bachus K.N. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26:59–65. doi: 10.1177/03635465980260012701. [DOI] [PubMed] [Google Scholar]
- 2.Garth W.P., Jr., DiChristina D.G., Holt G. Delayed proximal repair and distal realignment after patellar dislocation. Clin Orthop Relat Res. 2000;377:132–144. doi: 10.1097/00003086-200008000-00019. [DOI] [PubMed] [Google Scholar]
- 3.Nomura E., Horiuchi Y., Inoue M. Correlation of MR imaging findings and open exploration of medial patellofemoral ligament injuries in acute patellar dislocations. Knee. 2002;9:139–143. doi: 10.1016/s0968-0160(02)00002-9. [DOI] [PubMed] [Google Scholar]
- 4.Schottle P.B., Fucentese S.F., Romero J. Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patellar instability. Knee Surg Sports Traumatol Arthrosc. 2005;13:516–521. doi: 10.1007/s00167-005-0659-0. [DOI] [PubMed] [Google Scholar]
- 5.Buckens C.F., Saris D.B. Reconstruction of the medial patellofemoral ligament for treatment of patellofemoral instability: a systematic review. Am J Sports Med. 2010;38:181–188. doi: 10.1177/0363546509353132. [DOI] [PubMed] [Google Scholar]
- 6.Miller S.L., Gladstone J.N. Graft selection in anterior cruciate ligament reconstruction. Orthop Clin North Am. 2002;33:675–683. doi: 10.1016/s0030-5898(02)00027-5. [DOI] [PubMed] [Google Scholar]
- 7.Solman C.G., Jr., Pagnani M.J. Hamstring tendon harvesting. Reviewing anatomic relationships and avoiding pitfalls. Orthop Clin North Am. 2003;34:1–8. doi: 10.1016/s0030-5898(02)00025-1. [DOI] [PubMed] [Google Scholar]
- 8.Zhao J., Huangfu X. The biomechanical and clinical application of using the anterior half of the peroneus longus tendon as an autograft source. Am J Sports Med. 2012;40:662–671. doi: 10.1177/0363546511428782. [DOI] [PubMed] [Google Scholar]
- 9.Biedert R.M., Gruhl C. Axial computed tomography of the patellofemoral joint with and without quadriceps contraction. Arch Orthop Trauma Surg. 1997;116:77–82. doi: 10.1007/BF00434106. [DOI] [PubMed] [Google Scholar]
- 10.Koeter S., Horstmann W.G., Wagenaar F.C. A new CT scan method for measuring the tibial tubercle trochlear groove distance in patellar instability. Knee. 2007;14:128–132. doi: 10.1016/j.knee.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 11.Sasaki T., Yagi T. Subluxation of the patella. Investigation by computerized tomography. Int Orthop. 1986;10:115–120. [PubMed] [Google Scholar]
- 12.Dejour D., Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc. 2007;15:39–46. doi: 10.1097/JSA.0b013e31803035ae. [DOI] [PubMed] [Google Scholar]
- 13.Xie G., Zhao J., Huangfu X. Medial patellofemoral ligament reconstruction using semitendinosus tendons: polyester suture augmentation versus nonaugmentation. Am J Sports Med. 2012;40:1365–1374. doi: 10.1177/0363546512441324. [DOI] [PubMed] [Google Scholar]
- 14.Fulkerson J.P. Anteromedialisation of the tibial tuberosity for patellofemoral malalignment. Clin Orthop Relat Res. 1983;177:176–181. [PubMed] [Google Scholar]
- 15.Zhao J., Huangfu X., He Y. Recurrent patellar dislocation in adolescents: medial retinaculum plication versus vastus medialis plasty. Am J Sports Med. 2012;40:123–132. doi: 10.1177/0363546511420551. [DOI] [PubMed] [Google Scholar]
- 16.Ahmad C.S., Brown G.D., Stein B.S. The docking technique for medial patellofemoral ligament reconstruction: surgical technique and clinical outcome. Am J Sports Med. 2009;37:2021–2027. doi: 10.1177/0363546509336261. [DOI] [PubMed] [Google Scholar]
- 17.Ellera Gomes J.L., Stigler Marczyk L.R., Cesar de Cesar P. Medial patellofemoral ligament reconstruction with semitendinosus autograft for chronic patellar instability: a follow-up study. Arthroscopy. 2004;20:147–151. doi: 10.1016/j.arthro.2003.11.006. [DOI] [PubMed] [Google Scholar]
- 18.Gomes J.E. Comparison between a static and a dynamic technique for medial patellofemoral ligament reconstruction. Arthroscopy. 2008;24:430–435. doi: 10.1016/j.arthro.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 19.Nomura E., Inoue M. Hybrid medial patellofemoral ligament reconstruction using the semitendinous tendon for recurrent patellar dislocation: minimum 3 years' follow-up. Arthroscopy. 2006;22:787–793. doi: 10.1016/j.arthro.2006.04.078. [DOI] [PubMed] [Google Scholar]
- 20.Ronga M., Oliva F., Longo U.G. Isolated medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2009;37:1735–1742. doi: 10.1177/0363546509333482. [DOI] [PubMed] [Google Scholar]
- 21.Watanabe T., Muneta T., Ikeda H. Visual analog scale assessment after medial patellofemoral ligament reconstruction: with or without tibial tubercle transfer. J Orthop Sci. 2008;13:32–38. doi: 10.1007/s00776-007-1196-0. [DOI] [PubMed] [Google Scholar]
- 22.Zhao J., Huangfu X., He Y. The role of medial retinaculum plication versus medial patellofemoral ligament reconstruction in combined procedures for recurrent patellar instability in adults. Am J Sports Med. 2012;40:1355–1364. doi: 10.1177/0363546512439193. [DOI] [PubMed] [Google Scholar]
- 23.LaPrade R.F., Engebretsen A.H., Ly T.V. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89:2000–2010. doi: 10.2106/JBJS.F.01176. [DOI] [PubMed] [Google Scholar]
- 24.Christiansen S.E., Jacobsen B.W., Lund B. Reconstruction of the medial patellofemoral ligament with gracilis tendon autograft in transverse patellar drill holes. Arthroscopy. 2008;24:82–87. doi: 10.1016/j.arthro.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 25.Schottle P.B., Hensler D., Imhoff A.B. Anatomical double-bundle MPFL reconstruction with an aperture fixation. Knee Surg Sports Traumatol Arthrosc. 2010;18:147–151. doi: 10.1007/s00167-009-0868-z. [DOI] [PubMed] [Google Scholar]