Abstract
There are currently no studies that determine the total burden that tendinopathy places on patients and society. A systematic search was conducted to understand the impact of tendinopathy. It demonstrated that the current prevalence is underestimated, particularly in active populations, such as athletes and workers. Search results demonstrate that due to the high prevalence, impact on patients' daily lives and the economic impact due to work-loss, treatments are significantly higher than currently observed. A well-accepted definition by medical professionals and the public will improve documentation and increase awareness, in order to better tackle the disease burden.
Keywords: incidence, prevalence, quality-of-life, socio-economic, tendinopathy
Introduction
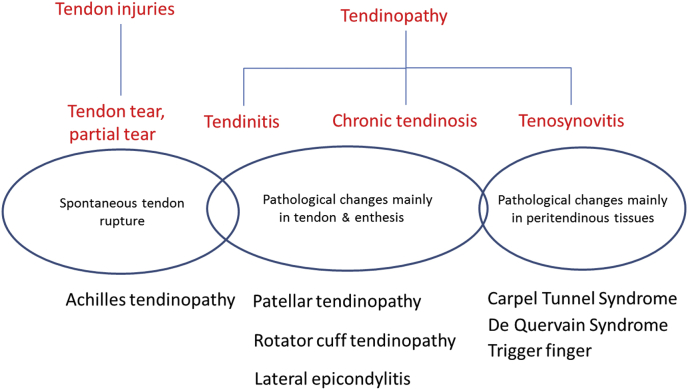
Clinicians obtain insight into the burden of tendinopathy from their patients, yet their ability to alleviate this burden remains limited. From their observations, it is to be believed that tendinopathy has a significant socio-economic impact, but there is no direct evidence to support this claim. This review aims to determine the socio-economic burden of tendinopathy and how this burden may be alleviated. The definition and classification of tendinopathy currently adopted by medical subject headings are displayed in Figure 1. Tendinopathy is a blanket term for “tendinitis”, “tendinosis”, and “tenosynovitis”. “Tendinitis” was the original term to define pain and inflammation within the tendon, and “tendinosis” was the preferential term to describe the degenerative changes observed. Strictly speaking, “tenosynovitis” refers to inflammation of the synovial sheath surrounding the tendon, thus it should not be regarded as tendinopathy in which degenerative changes are mainly observed in the tendon itself. By contrast, spontaneous tendon rupture, which occurs without prior symptoms, is attributed to mechanical weakness of tendons due to tendinopathic changes.1 In summary, tendinopathy is characterised by chronic tendon degeneration, resulting in pain and rupture, which are the basic criteria used when searching for relevant information.
Figure 1.
Nomenclature, definitions, and types of tendon disorders.
The disease burden of tendinopathy can be primarily reflected by the number of patients, the effect on the patients' quality-of-life, cost effectiveness of treatments, and the economic implications of work disability. Therefore, we performed a systematic search of prevalence and incidence data of tendinopathy, and gathered information about quality-of-life, work disability, and treatments specific to tendinopathy.
Prevalence and incidence of tendinopathy
A literature search was performed in PubMed in October 2015 using the search strategy: (Tendinopathy OR tendinitis OR tendonitis OR tendinosis OR tendon rupture OR tendon tear OR jumper's knee OR Sinding-Larsen-Johansson OR epicondylitis OR tennis elbow) AND (prevalence OR incidence OR epidemiology). Studies are included if prevalence or incidence of tendinopathy was reported. Studies on tenosynovitis and traumatic injuries were excluded. Non-English studies, reviews, animal, and cadaveric studies were also excluded. The search returned 1819 articles, of which 132 were included based on the selection criteria. The search results were tabulated according to the nature of the cohort (athletes, workers, general population, and patients with comorbidities), sample size, age group, type of tendinopathy involved, and the reported prevalence and incidence data.
Of the cohorts identified, athletes formed the major cohort with 42 studies, followed by workers (36 studies), individuals in the general population (35 studies), and individuals with comorbidities (19 studies). Achilles' tendinopathy, patellar tendinopathy, epicondylitis, and rotator cuff tendinopathy are identified as four major types of tendinopathy according to numbers of studies and the reported prevalence. The results are shown in Table 1.
Table 1.
Prevalence and incidence of tendinopathy in different cohorts.
| 1st Author, year, Ref | Group | Cohort | N | Age | Type of tendinopathy | Prevalence | Incidence |
|---|---|---|---|---|---|---|---|
| Zapata, 200671 | General | Students | 791 | Adolescent | Tendonitis | 2 | n/a |
| Salaffi, 200523 | General | Italian general population | 2155 | Adults | LE | 0.7 | n/a |
| Miranda, 200518 | General | General population | 8028 | Adults | RC tendinitis | 2 | n/a |
| Rechardt, 201072 | General | General population | 6237 | Adults | RC tendinitis | 2.8 | n/a |
| Tajika, 201424 | General | Japanese mountain village community | 422 | Adults | LE | 3.8 | n/a |
| Joseph, 201273 | General | Asymptomatic active university student body | 52 | Adults | AT (US) | 3.8 | n/a |
| Koplas, 201127 | General | Elbow MRI examinations | 801 | Adults | Triceps tendon tear | 3.8 | n/a |
| Waldecker, 201274 | General | Non-athletes in orthopaedic clinic | 697 | Adults | AT tendinopathy | 5.6 | n/a |
| Schibany, 200475 | General | Asymptomatic patients | 212 | Adults | Supraspinatus rupture (US) | 6 | n/a |
| Zwerver, 201139 | General | Nonelite athletes | 891 | Adults | Jumper's knee | 8.5 | n/a |
| Fairley, 201435 | General | Community with no history of knee pain or injury | 297 | Adults | PT (MRI) | 28.3 | n/a |
| Walker-Bone, 201244 | General | General population | 6038 | Adults | LE ME |
0.7 0.6 |
n/a |
| Shiri, 200621 | General | General population | 4783 | Adults | LE ME |
1.3 0.4 |
n/a |
| Alvarez-Nemegyei, 201128 | General | General population | 12,686 | Adults | RC tendinopathy Bicipital tendinopathy AT tendinopathy |
2.4 0.3 0.1 |
n/a |
| Walker-Bone, 200422 | General | General population | 6038 | Adults | RC tendinitis Bicipital tendinitis LE ME |
3.3 0.4 0.7 0.6 |
n/a |
| Shiri, 200719 | General | General population | 6254 | Adults | RC tendinitis Bicipital tendinitis LE ME |
3.8 0.5 1.1 0.3 |
n/a |
| Girish, 201136 | General | Asymptomatic shoulders | 51 | Adults | Supraspinatus (US) Subscapularis (US) Supraspinatus tear (US) |
39 25 22 |
n/a |
| Safran, 200276 | General | General population | 279,500 | Adults | Biceps tendon rupture | n/a | 1.2/100,000 PY |
| Witvrouw, 200152 | General | Students without knee conditions | 138 | Adults | PT tendinitis | n/a | 13.8% (2 y CI) |
| Huttunen, 201469 | General | Nationwide Sweden | 27,702 | Adults | AT rupture | n/a | 29.5/100,000 PY |
| Ostor, 200577 | General | General population | 17,000 | Adults | RC tendinopathy | n/a | 8.1/1000 PY |
| Cretnik, 201078 | General | General population | 572,929 | Adults Elderly |
AT rupture | n/a | 7.6/100,000 PY 1.3/100,000 PY |
| Darmawan, 199525 | General | Indonesian population | 1118 | All | Epicondylitis | 6.6 | n/a |
| Moller, 199679 | General | Malmo population | n/a | All | AT rupture | n/a | 0.06 (4 y CI) |
| Clayton, 200880 | General | General population | 535,000 | All | AT rupture | n/a | 11.3/100,000 PY |
| Levi, 199781 | General | Copenhagen population | n/a | All | AT rupture | n/a | 13.4/100,000 PY |
| Leppilahti, 199682 | General | Oulu population | n/a | All | AT rupture | n/a | 18/100,000 PY |
| Houshian, 199883 | General | Danish county | 220,000 | All | AT rupture | n/a | 37.3/100,000 PY |
| Maffulli, 199984 | General | General population | n/a | All | AT rupture | n/a | 6/100,000 PY |
| van der Linden, 200170 | General | General population | n/a | All | Tendon rupture | n/a | 6.32/100,000 PY |
| Suchak, 200585 | General | Canada general population | 967,200 | All | AT rupture | n/a | 8.3/100,000 PY |
| Chard, 198720 | General | Geriatric unit not admitted for shoulder complaints | 100 | Elderly | RC tendinitis RC rupture |
5 7 |
n/a |
| Horowitz, 201326 | General | General population | n/a | n/a | Retropharyngeal calcific tendinitis | n/a | 0.5/100,000 PY |
| de Jonge, 201186 | General | General population | 57,725 | n/a | AT tendinopathy | n/a | 1.8/1000 PY |
| Nyyssonen, 200887 | General | Finnish population | 5.2m | n/a | AT rupture | n/a | 11.5/100,000 PY |
| McCormack, 199088 | Worker | Textile workers | 2047 | Adults | Epicondylitis | 2 | n/a |
| Roquelaure, 200615 | Worker | Workers | 2685 | Adults | LE | 2.4 | n/a |
| Almeida, 201289 | Worker | Workers | 951 | Adults | Tendinitis | 3.2 | n/a |
| Frost, 200290 | Worker | Workers | 782 | Adults | Shoulder tendinitis | 3.2 | n/a |
| Descatha, 200391 | Worker | Workers | 1757 | Adults | ME | 5.2 | 1.5% (annual CI) |
| Fan, 200992 | Worker | Workers | 733 | Adults | LE | 5.2 | n/a |
| Rosenbaum 201393 | Worker | Latino poultry workers | 516 | Adults | Epicondylitis | 5.8 | n/a |
| Kryger, 200794 | Worker | Computer workers with neck or arm pain | 1369 | Adults | LE | 5.8 | n/a |
| Kaergaard, 200095 | Worker | Sewing machine operators | 243 | Adults | RC tendinitis | 5.8 | n/a |
| Dimberg, 198796 | Worker | Workers | 540 | Adults | LE | 7.4 | n/a |
| Roto, 198497 | Worker | Male meat cutters | 90 | Adults | Epicondylitis | 8.9 | n/a |
| Ono, 199898 | Worker | Nursery school cooks | 209 | Adults | Epicondylitis | 11.5 | n/a |
| Leclerc, 200199 | Worker | Workers | 598 | Adults | LE | 12.2 | 12.2% (3 y CI) |
| Capone, 2010100 | Worker | Plastic surgeons | 339 | Adults | Epicondylitis | 13.5 | n/a |
| Ritz, 1995101 | Worker | Workers | 290 | Adults | Epicondylitis | 14.1 | n/a |
| Chiang, 1993102 | Worker | Workers in fish-processing | 207 | Adults | Epicondylitis | 15 | n/a |
| Barrero, 2012103 | Worker | Workers flower industry | 158 | Adults | Epicondylitis | 15.2 | n/a |
| Auerbach, 201116 | Worker | Spine surgeons | 561 | Adults | LE | 18 | n/a |
| Forde, 2005104 | Worker | Ironworkers | 981 | Adults | Tendonitis | 19 | n/a |
| Sansone, 201537 | Worker | Female cashier | 199 | Adults | RC calcific tendinopathy (US) | 22.6 | n/a |
| Cunha-Miranda, 201034 | Worker | Workers | 410,496 | Adults | Shoulder tendonitis Elbow tendonitis Lower limb tendonitis |
0.6 0.3 0.1 |
n/a |
| Werner, 2002105 | Worker | Dental hygienists | 305 | Adults | Shoulder tendinitis Elbow tendinitis |
13 6 |
n/a |
| Gold, 2009106 | Worker | Automobile manufacturing workers | 1214 | Adults | LE ME RC tendonitis |
3.3 2.2 12 |
n/a |
| Pullopdissakul, 2013107 | Worker | Workers | 591 | Adults | LE ME |
3.4 1.7 |
n/a |
| Nordander, 2009108 | Worker | Workers | 2677 | Adults | Supraspinatus tendonitis Infraspinatus tendonitis Bicipital tendonitis LE ME |
4.4 3 3.8 2.3 1.2 |
n/a |
| Silverstein, 2006109 | Worker | Workers | 436 | Adults | RC tendinitis | 4.4–7.6 | 2.9–5.5/100 PY |
| Ozdolap, 201317 | Worker | Coal miners | 80 | Adults | LE ME |
41.2 12.5 |
n/a |
| Werner, 200538 | Worker | Dental hygiene students Clerical workers |
343 164 |
Adults | Upper extremity tendinitis | 5 12 |
n/a |
| Fan, 2014110 | Worker | Workers | 607 | Adults | Epicondylitis LE ME |
6 5 2 |
7.9/100 PY 5.1/100 PY 2.4/100 PT |
| Garg, 2014111 | Worker | Workers | 536 | Adults | LE | 7.3 | 3.67/100 PY |
| Alexandre, 2011112 | Worker | Dentist Physicians Lawyers General population |
173,094 | Adults | Tendinitis | 8.7 5.6 5.5 3.2 |
n/a |
| Herquelot, 2013113 | Worker | Workers | 3710 | Adults | LE | n/a | 1.0/100 PY |
| Werner, 2005114 | Worker | Workers | 501 | Adults | Upper extremity tendonitis | n/a | 4.5% (annual CI) |
| Fan, 2014 Feb115 | Worker | Workers | 611 | Adults | LE | n/a | 4.9/100 PY |
| Descatha, 2013116 | Worker | Workers | 699 | Adults | Epicondylitis LE ME |
n/a | 6.9% (36 mo CI) 4.9% (36 mo CI) 4.3% (36 mo CI) |
| McGaughey, 2003117 | Worker | Expeditioners | 292.3 PY | Adults | AT tendonitis | n/a | 9.2/100 PY |
| Barber Foss, 2012118 | Athletes | Female basketball players | 419 | Adolescent | SLJ | 5 | n/a |
| Tenforde, 201112 | Athletes | High school athletes | 748 | Adolescent | AT tendonitis | 7.8 | n/a |
| Emerson, 2010119 | Athletes | Elite gymnasts | 40 | Adolescent | AT tendinopathy | 15 | n/a |
| Steinberg, 2011120 | Athletes | Nonprofessional female dancers | 1336 | Adolescent | Ankle & foot tendonitis | 18.8 | n/a |
| Cassel, 201510 | Athletes | Adolescent athletes | 760 | Adolescent | AT tendinopathy PT tendinopathy AT rupture |
1.8 5.6 0.1 |
n/a |
| Gisslen, 2005121 | Athletes | Swedish elite junior volleyball players | 57 | Adolescent | Jumper's knee PT (US) |
21 28.9 |
n/a |
| Le Gall, 2007122 | Athletes | Early maturing athletes Late maturing athletes |
233 | Adolescent | Tendinopathy | n/a | 0.06/1000 AE 0.02/1000 AE |
| Barber Foss, 2014123 | Athletes | Female middle school athletes | 268 | Adolescent | SLJ | n/a | 0.3/1000 AE |
| Beachy, 2014124 | Athletes | Middle school athletes | 14,038 | Adolescent | Tendinitis | n/a | 0.7/1000 AE |
| Leanderson, 2011125 | Athletes | Ballet dancers | 476 | Adolescent | Foot tendinosis Jumper's knee Tendonitis genu Tendinosis groin |
n/a | 11.8% (7 y CI) 6.5% (7 y CI) 5.2% (7 y CI) 8.6% (7 y CI) |
| Hickey, 1997126 | Athletes | Elite female basketball players | 49 | Adolescent | PT tendinitis | n/a | 30.6% (6 y CI) |
| Dubravcic-Simunjak, 2003127 | Athletes | Junior figure skaters | 469 | Adolescent | Jumper's knee AT tendinitis |
n/a | 8.1 (5 y CI) 2.1 (5 y CI) |
| Hagglund, 2011128 | Athletes | Elite male soccer players | 2229 | Adults | PT tendinopathy | 2.4 (season prevalence) | 0.1/1000 h |
| Buda, 201311 | Athletes | Climbers | 144 | Adults | AT tendinitis | 12.5 | n/a |
| Pieber, 20125 | Athletes | Climbers | 193 | Adults | Epicondylitis | 13.1 | n/a |
| Durcan, 2014129 | Athletes | Elite rugby academies | 83 | Adults | PT tendinopathy | 13.3 | n/a |
| Lian, 20058 | Athletes | Elite athletes | 613 | Adults | Jumper's knee | 14.2 | n/a |
| McCarthy, 20137 | Athletes | Women's basketball | 496 | Adults | PT tendinitis | 17 | n/a |
| van der Worp, 20119 | Athletes | Basketball & volleyball players | 1505 | Adults | Patellar tendinopathy | 17.8 | n/a |
| Cook, 1998130 | Athletes | Elite athletes | 160 | Adults | PT (US) | 22 | n/a |
| Lopes, 20093 | Athletes | Athletes referred to PT | 434 | Adults | Tendinopathy | 22.4 | n/a |
| Wang, 20014 | Athletes | Elite volleyball athletes | 59 | Adults | RC tendinitis | 23.7 | n/a |
| Monteleone, 201433 | Athletes | Elite beach volleyball players | 53 | Adults | RC (US) | 30 | n/a |
| Longo, 201113 | Athletes | Veteran track & field athlete | 174 | Adults Elderly | PT tendinopathy | 46.6 | n/a |
| Rooks, 1995131 | Athletes | Rock climbers | 39 | Adults | Upper extremity tendinitis | 50 | n/a |
| Walls, 2010132 | Athletes | Professional dancers | 18 | Adults | AT tendinopathy (MRI) | 78 | n/a |
| Hagemann, 2004133 | Athletes | Marathon kayakers | 52 | Adults | Supraspinatus (MRI) Supraspinatus tear (MRI) Subscapularis (MRI) Subscapularis tear (MRI) |
11.5 7.7 1.9 1.9 |
n/a |
| Reuter, 2008134 | Athletes | Ironman triathletes | 23 | Adults | RC partial tear Shoulder tendinopathy |
22 43 |
n/a |
| Hadala, 2009135 | Athletes | Elite yacht sailors | 30 | Adults | Epicondylitis Biceps brachii tendinitis Shoulder tendinopathy |
30 3.3 13.3 |
n/a |
| Comin, 201340 | Athletes | Ballet dancers | 79 | Adults | AT (US) PT (US) |
8.9 8.9 |
n/a |
| Marshall, 2007136 | Athletes | Collegiate women's softball athletes | 9389 | Adults | Shoulder tendinitis Elbow tendinitis |
n/a | 0.12/1000 AE 0.04/1000 AE |
| Krupnick, 1998137 | Athletes | White water paddlers | 54 | Adults | Tendonitis | n/a | 0.19/100 AE |
| Kelly, 2004138 | Athletes | Elite football quarterbacks | 1534 | Adults | Biceps tendinitis | n/a | 0.5/100 AE |
| Parekh, 2009139 | Athletes | National Football League | n/a | Adults | AT rupture | n/a | 0.9% (per game CI) |
| Heir, 1996140 | Athletes | Military conscripts | 6488 | Adults | AT tendinitis Shoulder tendinitis |
n/a | 13.5/1000 conscript-mo 2.1/1000 conscript-mo |
| Wolf, 2010141 | Athletes | US military population | n/a | Adults | LE ME |
n/a | 2.3/1000 PY 0.8/1000 PY |
| McFarland, 1998142 | Athletes | Collegiate baseball players | 12,828 AE | Adults | RC tendinitis | n/a | 3.4/1000 AE |
| White, 2007143 | Athletes | US army soldiers | 93,224 AE | Adults | Tendon rupture | n/a | 5.6/100 AE |
| Milgrom, 2003144 | Athletes | Male infantry recruits | 1405 | Adults | AT tendinopathy | n/a | 6.8% (4 period each 14 wk CI) |
| McMahon, 20146 | Athletes | Elite athletes | 141 | Elderly | RC tendinosis RC partial tear RC complete rupture |
16.3 48.2 21.3 |
n/a |
| Kettunen, 2011145 | Athletes | Former elite male athletes | 785 | Elderly | Shoulder tendinopathy Shoulder tendon rupture |
n/a | 33% (lifetime CI) 19% (lifetime CI) |
| Kujala, 200541 | Athletes | Former elite male athletes | 785 | Elderly | AT rupture AT tendinopathy |
n/a | 8.3% (lifetime CI) 23.9% (lifetime CI) |
| Njobvu, 200629 | Patients | HIV positive patients | 65 | Adults | Tendinitis | 3.1 | n/a |
| Cannon, 2007146 | Patients | Cervical radiculopathy with upper limb symptoms | 191 | Adults | LE | 4.7 | n/a |
| Hautmann, 2014147 | Patients | Patients with painful heel | 101 | Adults | AT tendinitis | 11.9 | n/a |
| Frey, 200731 | Patients | Overweight or obese | 738 | Adults | Ankle & foot tendinitis | 16.7 | n/a |
| Finley, 200432 | Patients | Manual wheelchair users | 52 | Adults | Biceps tendonitis | 30.1 | n/a |
| Baumann, 2008148 | Patients | Diagnostic shoulder arthroscopies | 1007 | Adults | Shoulder tendinitis Shoulder partial tear |
1.5 0.8 |
n/a |
| Chhajed, 2002149 | Patients | Lung transplant recipients treated with ciprofloxacin | 101 | Adults | AT tendonitis AT rupture |
15.8 5.9 |
n/a |
| Ramirez, 2014150 | Patients | Patients with greater trochanteric pain | 107 | Adults | Gluteus medius tendinosis Gluteus minimus tendinosis |
36.4 67.3 |
n/a |
| Taunton, 2002151 | Patients | Patients with running related injury | 2002 | Adults | PT tendinopathy AT tendinopathy |
4.2 4.8 |
n/a |
| Bird, 2001152 | Patients | Patients with greater trochanteric pain | 24 | Adults | Gluteus medius tear Gluteus medius tendinitis |
45.8 37.5 |
n/a |
| Shah, 200830 | Patients | Stroke patients with painful shoulder | 89 | Adults | RC tendinopathy RC tear |
53 35 |
n/a |
| Pong, 2012153 | Patients | Stroke patients with hemiplegic shoulders | 76 | Adults | Shoulder tendinopathy | 68.4 Acute 80.3 Chronic |
n/a |
| Kingzett-Taylor, 1999154 | Patients | Patients with buttock, lateral hip, or groin pain | 250 | Adults | Gluteal tear Gluteal tendinosis |
8.8 5.2 |
n/a |
| Chung, 2013155 | Patients | Nurses with musculoskeletal disorder | 3914 | Adults | ME LE |
n/a | 0.25% (1 y CI) 0.58% (1 y CI) |
| Barge-Caballero, 2008156 | Patients | Heart transplant patients under quinolones | 149 | Adults | AT tendinopathy AT rupture |
n/a | 9.4% (11 y CI) 2% (11 y CI) |
| Ramos, 2009157 | Patients | Patients with knee pain | 318 | All | PT tendinopathy | 32.3 | n/a |
| Helliwell, 2003158 | Patients | Patients with soft tissue disorders | 1382 | All | Shoulder tendinitis LE |
11.3 6.3 |
n/a |
| Sode, 2007159 | Patients | First time fluoroquinolone users | 28262 | All | AT rupture | n/a | 0.02 (90 d CI) |
| Zakaria, 2014160 | Patients | Diabetes patients | 1296 | Elderly | Tendon rupture | n/a | 5.21/1000 PY |
AE = athlete exposure; AT = Achilles tendon; CI = cumulative incidence; h = hours; LE = lateral epicondylitis; ME = medial epicondylitis; MRI = magnetic resonance imaging diagnosed; N = sample/cohort size; n/a = not available; PT = patellar tendon; PY = person-years; RC = rotator cuff; SLJ = Sinding-Larsen-Johansson; US = ultrasound diagnosed; y = years.
Results
Athletes
The high intensity and frequency of physical activities in athletes exposes this group to overuse injuries due to the high stress exerted on the tendons. Records of medical attendance in the 2004 Olympics2 and 2007 Pan-American Games3 show that tendinopathy was within the top three most treated conditions in athletes. This record represents the significance of tendinopathy as a widespread condition in this group.
Studies on the prevalence of upper extremity tendinopathy in athletes have observed small cohorts, yet data from studies with the largest sample sizes place the prevalence for rotator cuff tendinopathy at 23.7% in volleyball players, and epicondylitis at 13.1% in climbers.4, 5 Older age may also play a role as evidenced in a study on elderly athletes where prevalence was seen to be as high as 48.2%.6 There is no study on upper extremity tendinopathy in adolescents to our knowledge. A study on patellar tendinopathy reported a prevalence of approximately 17% in adults and 5.6% in adolescents.7, 8, 9, 10 Similarly, Achilles' tendinopathy was reported to be 12.5% in adults and 7.8% in adolescents.11, 12 Adolescents are seemingly less affected by tendinopathy based on these values alone. There is however no clear evidence that age influences tendinopathy.13 In agreement with previous studies,13, 14 no clear trend is observed when comparing the prevalence or incidence between male and female athletes.
Lower extremity tendinopathy, particularly that of the patellar tendon, is the most frequently studied and arguably the most commonly affected. However, sports-related tendinopathy is challenging to generalise due to the difference in anatomical sites affected and the degree of exposure. For instance, dancers present with higher prevalence of Achilles' tendinopathy, while rowers would more frequently present with rotator cuff tendinopathy or epicondylitis. In addition, the degree of sport participation would differ widely between recreational athletes and professional athletes, but professional or elite athletes may suffer greater economic losses from injury as compared to recreational athletes. Studies on the degree of participation, the associated risk of tendinopathy development, and the associated impact would be valuable further studies.
Workers
Occupational exposure is of particular relevance because of the high economic impact procured by productivity-loss and compensation for disease. Highly repetitive movements are commonly observed in daily work tasks, and coupled with poor workplace ergonomics, workers are placed at an increased risk of developing tendinopathy. A distinction can be made between workers and athletes in that occupational exposure typically consists of relatively low demand and highly repetitive movements over a longer period of time compared to athletic exposure. Worker cohorts have generally been larger than the athlete cohort. Many of these cohorts have been merged from different workplaces and may possibly be highly heterogeneous even within the same study. Tendinopathy in workers is almost exclusively observed in the upper extremity. The most common and arguably most prevalent of which is lateral epicondylitis. A prevalence of 2–3% have been observed, but rates as high as 18% and 41% have also been reported in spine surgeons and coal miners, respectively.15, 16, 17 Similar to athletic exposures, it is evident that the type of work influences the prevalence of tendinopathy.17 Relative risk in occupational exposure with regards to frequency of repetitive motion, length of exposure, and ergonomic factors may be worthwhile studies.
General population
In the general population, the prevalence of clinically diagnosed rotator cuff tendinopathy in adults was reported to range from 2% to 3.8%,18, 19 with a marginally higher prevalence observed in the elderly population at 5–7%.20 Although it may not be accurate to compare values from different studies, it is worth noting that the value in the general population approaches that of the worker cohorts. In the elbow joint, prevalence of lateral epicondylitis and medial epicondylitis in European cohorts were reported at 0.7–1.3% and 0.3–0.6%, respectively.19, 21, 22, 23 Two outliers were reported on lateral epicondylitis in a Japanese mountain village cohort at 3.8% and on epicondylitis in the Indonesian general population at 6.6%.24, 25 The divergence in values in these groups suggest that societal aspects also come into play and may be influenced by environmental, cultural, or economic differences among societies. Age and gender do not seem to influence tendinopathy within this cohort. Although upper extremity tendinopathy has been more frequently studied in the general population, less common conditions have also been observed, such as retropharyngeal tendinitis (0.5/100,000 person-years) triceps tendon tears (3.8%)26, 27 and bicipital tendinitis (0.3%–0.5%).19, 28
Comorbidity cohorts
Nineteen studies reported tendinopathy in cohorts with other associated conditions such as HIV positive patients,29 stroke survivors,30 obese cohorts,31 wheelchair users,32 etc. (Table 1). Some studies do not investigate the association of tendinopathy with other disease conditions, but instead report tendinopathy as part of a group of patients with musculoskeletal complaints in general. A general trend of increased prevalence is seen when compared with the general population; however due to the variety of conditions, and how they impact tendinopathy, the data cannot be utilised to assess the prevalence of tendinopathy within this cohort. These studies provide evidence that there are intrinsic risk factors for tendinopathy and research into the relationship between them would be worthwhile in understanding the aetiology of tendinopathy.
Summary of systematic review
There is currently a gap in the available evidence on incidence rates as most studies carried out on the general population are on tendinopathic ruptures only. The actual prevalence of tendinopathy may be higher due to diagnosis. Clinical diagnosis is the main diagnostic technique, with radiological imaging, such as magnetic resonance imaging (MRI) and ultrasound being used to support the diagnosis. Studies that defined tendinopathy using radiological imaging revealed a higher incidence rate compared with studies that used clinical evaluation only.33, 34, 35, 36, 37, 38, 39 This discrepancy is caused by the inclusion of patients who did not present with symptoms at the time of examination, suggesting that asymptomatic patients are left unnoticed in tendinopathy diagnosis.40 This is important since the lifetime cumulative incidence of retired elderly athletes is approximately 25%, suggesting that symptoms may develop later than when the injury was sustained.41
In summary, specific types of tendinopathy are more prevalent in the different groups. Epicondylitis and rotator cuff tendinopathy were preferentially investigated in workers and the general population, with workers having a higher prevalence and incidence of tendinopathy. Patellar tendinopathy was more frequently investigated in the athlete population, revealing a higher prevalence and incidence when compared with the other groups. Finally, age and sex does not seem to play a factor in tendinopathy.
Effects of tendinopathy on quality-of-life and cost-effectiveness of treatment
A community-based survey compared the socio-economic impacts of four musculoskeletal conditions including tendinitis (tendinopathy), rheumatoid arthritis, osteoarthritis, and lower back pain. Although tendinopathy was found to be less influential to work loss,42 shoulder tendinopathy took approximately 10 months to heal and workers take greater amounts of sick leave to recover,43, 44, 45 report being less productive at work,9 and require workers' compensation for disease.46, 47 Finally, even though patients may return to work within 6 weeks following operative repair, recovery may take a few months.48 The burden placed on daily activities cannot be ignored, with one study claiming that about a quarter of patients with tennis elbow (epicondylitis) reported difficulty in activities such as dressing, carrying objects, driving, and sleeping.49 The indirect costs can reach great amounts in terms of productivity loss and worker's compensation. Up to 5% of patients with lateral epicondylitis have claimed sickness absence with an average duration of 29 days in a year.44 Thus, absenteeism (in the working population aged 25–64) due to lateral epicondylitis in the United Kingdom alone is estimated to cost £27 million using 2012 global population statistics and median wage.44, 50, 51 Productivity-loss and disease compensation associated with tendinopathy are remarkable, and the high prevalence of tendinopathy, as revealed by the search results on tendinopathy prevalence, suggests that the disease burden may be greater than currently understood.
The goals of tendinopathy treatment are pain reduction, recurrence prevention, and return to sports or preinjury functionality. Treatment aims to remain conservative with oral nonsteroidal anti-inflammatory drugs, corticosteroid injections, and physical therapy as the mainstay in tendinopathy management. Other therapies include injections of platelet-rich plasma or autologous blood. Finally, failure of conservative treatments leads to surgical intervention to excise the tendinopathic tissue and repair the ruptured tendon.52, 53 Yet the cost analysis on various tendinopathy treatments is inadequate. Direct outpatient medical costs were reported as ranging from €430/patient for corticosteroid injection to €921/patient for physical therapy, for lateral epicondylitis (currency in 2004).54 Repeated medical visits are also a concern as lateral epicondylitis is recurrent, and almost half of those affected have seen their general practitioner within the past 12 months.44 Cost/quality-adjusted-life-years for physical therapy and corticosteroid injection were £18,962 and £20,518, respectively, values which fall within the benchmark of £20,000 to £30,000 (currency in 2015) and are comparable to the common drug treatments for osteoarthritis and osteoporosis (currency in 2005 and 2004, respectively).55, 56, 57 Economic evaluations on other tendinopathic conditions are lacking and research on this aspect would be valuable.
Documentation and awareness of tendinopathy
Although tendinopathy is well-recognised in the academic field as listed in the medical subject headings, only tendinitis and spontaneous tendon ruptures are stated within the current version of International Classification of Diseases (ICD) by the World Health Organization (WHO), but tendinosis and tendinopathy are absent.58 Tendinitis and tendinosis, continue to be mainstay diagnostic terms, but as tendinopathy has become the accepted term within the medical field, it should be similarly recognised by the public. Healthcare organisations, such as WHO and the Centre for Disease Control (CDC), and orthopaedic organisations, such as the Bone Joint Decade (BJD) and the Fracture Fragility Network (FFN), do not have definitions or information for the term “tendinopathy”. Evidence from our search has demonstrated that despite clinical diagnosis being the mainstay diagnostic technique, MRI and ultrasound are favourable, particularly for asymptomatic patients. Implementation of a standardised, radiological technique, would allow for the inclusion of symptomatic patients, asymptomatic patients, and patients with ruptures to be recognised under the definition of tendinopathy.
Failure to recognise and report an incident, and failure to seek medical attention, amongst other factors may lead to two thirds of tendinopathy cases going unreported, thus the proportion of individuals with tendinopathy may be higher than reported.59 Tendinopathy appears to be particularly prevalent in productive populations that actively contribute to societal development, such as athletes and workers. Despite these indications that tendinopathy may be highly prevalent in society, it remains an under-recognised disease.
Osteoarthritis and osteoporosis are well recognised and studied by researchers, WHO, CDC, and are also key topics in BJD and FFN. These diseases are particularly prevalent in the elderly, thus, their impact on productive demographics may be lower, when compared with tendinopathy.60, 61 The National Coalition for Osteoporosis and Related Bone Diseases (with support from WHO) and The Arthritis Foundation (with support from CDC) have published action plans to address insufficiencies in tackling osteoporosis and osteoarthritis, respectively.62, 63 The Australian government published their own action plan (similar to the aforementioned plans) to tackle osteoporosis, osteoarthritis, and rheumatoid arthritis.64 These action plans provide a framework to implement research, prevention, treatment, and education within the public. Internet resources are playing a greater role in how the public recognises diseases. Both CDC and WHO have published data on recognising symptoms, prevention, and treating both osteoarthritis and osteoporosis, targeted toward the general public for easy access to information. Our search results have demonstrated that tendinopathy is not well-documented in relation to other diseases; however, the awareness of risk-factors of osteoporosis and osteoarthritis are well-recognised, such as obesity and diabetes, allowing for better disease prevention. The International Osteoporosis Foundation and National Osteoporosis Foundation conducted a study to determine the global prevalence of osteoporosis, and the North Staffordshire Osteoarthritis Project conducted a census to determine the prevalence and impact of osteoarthritis.65, 66 These studies demonstrate that greater awareness, leads to support by well-established organisations, and aid in determining disease prevalence and impact. Current healthcare registries are a useful tool in tracking and studying diseases, and this has helped study the prevalence of osteoporosis through hip fracture and osteoarthritis through total knee replacements.67 Thus, this implores the question as to why tendinopathy does not receive similar awareness and action, when the prevalence may be similar to osteoarthritis and osteoporosis.
Determining the true prevalence of tendinopathy is the first step in studying the impact that tendinopathy has on society, and for this, national health registries are a useful tool, with Sweden, Finland, and The Netherlands using their own registries to study the prevalence of tendon rupture.68, 69, 70 However, in order for national health registries to run effectively, they require standardised nomenclature and diagnostics. For example, the Swedish Hospital Discharge Registry utilises the ICD in their system, yet without the recognition of tendinopathy in the database, incidences are not recorded. There is currently no organisation specialising in raising awareness for tendinopathy. Through such an organisation of specialists in this field, we may present a greater front in establishing these standardised definitions of tendinopathy, and having established this, it is necessary to approach international organisations such as WHO, CDC, BJD, and FFN, to gain recognition of the disease in professional fields, as well as have the term properly recognised by the ICD. Establishing these foundational aspects, tendinopathy may be better recognised by the public, patients may be encouraged to seek earlier medical attention, resources will be appropriately allocated to alleviate the burden of tendinopathy, and conclusive studies on the prevalence and socio-economic impact of tendinopathy can be implemented.
Conclusion
The definition of tendinopathy is variable, making proper documentation difficult. Tendinopathy should be defined using widely accepted criteria used by professionals, to include symptomatic, asymptomatic, and rupture patients. Our search results demonstrate that tendinopathy is prevalent in a variety of demographics, particularly in younger generations that are most active in society, yet the public awareness is low. By encouraging awareness in both the professional and public fields, we will enhance our understanding and make appropriate changes in how to tackle the disease.
These proposed changes will be slow, and require persistent effort from experts in the field of tendinopathy. Furthermore, the capacity to make such changes varies widely around the globe, in which some societies may not be able to implement the same systems or interventions as others. However, through these actions we may be able to enhance global awareness of the disease and relieve the burden tendinopathy currently places on society.
Conflicts of interest
The authors have no conflicts of interest relevant to this article.
Funding/support
No financial or material support of any kind was received for the work described in this article.
References
- 1.Kader D., Mosconi M., Benazzo F. Achilles tendon rupture. In: Maffulli N., Renstrom P., Leadbetter W.B., editors. Tendon Injuries. Springer London; London: 2005. pp. 187–200. [Google Scholar]
- 2.Athanasopoulos S., Kapreli E., Tsakoniti A. The 2004 Olympic games: physiotherapy services in the Olympic Village polyclinic. Br J Sports Med. 2007;41(9):603–609. doi: 10.1136/bjsm.2007.035204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lopes A.D., Barreto H.J., Aguiar R.C. Brazilian physiotherapy services in the 2007 Pan-American Games: injuries, their anatomical location and physiotherapeutic procedures. Phys Ther Sport. 2009;10:67–70. doi: 10.1016/j.ptsp.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 4.Wang H.K., Cochrane T. A descriptive epidemiological study of shoulder injury in top level English male volleyball players. Int J Sports Med. 2001;22:159–163. doi: 10.1055/s-2001-11346. [DOI] [PubMed] [Google Scholar]
- 5.Pieber K., Angelmaier L., Csapo R. Acute injuries and overuse syndromes in sport climbing and bouldering in Austria: a descriptive epidemiological study. Wien Klin Wochenschr. 2012;124:357–362. doi: 10.1007/s00508-012-0174-5. [DOI] [PubMed] [Google Scholar]
- 6.McMahon P.J., Prasad A., Francis K.A. What is the prevalence of senior-athlete rotator cuff injuries and are they associated with pain and dysfunction? Clin Orthop Relat Res. 2014;472:2427–2432. doi: 10.1007/s11999-014-3560-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCarthy M.M., Voos J.E., Nguyen J.T. Injury profile in elite female basketball athletes at the Women's National Basketball Association combine. Am J Sports Med. 2013;41:645–651. doi: 10.1177/0363546512474223. [DOI] [PubMed] [Google Scholar]
- 8.Lian O.B., Engebretsen L., Bahr R. Prevalence of jumper's knee among elite athletes from different sports: a cross-sectional study. Am J Sports Med. 2005;33:561–567. doi: 10.1177/0363546504270454. [DOI] [PubMed] [Google Scholar]
- 9.van der Worp H., van Ark M., Roerink S. Risk factors for patellar tendinopathy: a systematic review of the literature. Br J Sports Med. 2011;45:446–452. doi: 10.1136/bjsm.2011.084079. [DOI] [PubMed] [Google Scholar]
- 10.Cassel M., Baur H., Hirschmüller A. Prevalence of Achilles and patellar tendinopathy and their association to intratendinous changes in adolescent athletes. Scand J Med Sci Sports. 2015;25:e310–e318. doi: 10.1111/sms.12318. [DOI] [PubMed] [Google Scholar]
- 11.Buda R., Di Caprio F., Bedetti L. Foot overuse diseases in rock climbing: an epidemiologic study. J Am Podiatr Med Assoc. 2013;103:113–120. doi: 10.7547/1030113. [DOI] [PubMed] [Google Scholar]
- 12.Tenforde A.S., Sayres L.C., McCurdy M.L. Overuse injuries in high school runners: lifetime prevalence and prevention strategies. PM R. 2011;3:125–131. doi: 10.1016/j.pmrj.2010.09.009. quiz 131. [DOI] [PubMed] [Google Scholar]
- 13.Longo U.G., Rittweger J., Garau G. Patellar tendinopathy in master track and field athletes: influence of impact profile, weight, height, age and gender. Knee Surg Sports Traumatol Arthrosc. 2011;19:508–512. doi: 10.1007/s00167-010-1314-y. [DOI] [PubMed] [Google Scholar]
- 14.Longo U.G., Rittweger J., Garau G. No influence of age, gender, weight, height, and impact profile in achilles tendinopathy in masters track and field athletes. Am J Sports Med. 2009;37:1400–1405. doi: 10.1177/0363546509332250. [DOI] [PubMed] [Google Scholar]
- 15.Roquelaure Y., Ha C., Leclerc A. Epidemiologic surveillance of upper-extremity musculoskeletal disorders in the working population. Arthritis Rheum. 2006;55:765–778. doi: 10.1002/art.22222. [DOI] [PubMed] [Google Scholar]
- 16.Auerbach J.D., Weidner Z.D., Milby A.H. Musculoskeletal disorders among spine surgeons: results of a survey of the Scoliosis Research Society membership. Spine (Phila Pa 1976) 2011;36:E1715–E1721. doi: 10.1097/BRS.0b013e31821cd140. [DOI] [PubMed] [Google Scholar]
- 17.Ozdolap S., Emre U., Karamercan A. Upper limb tendinitis and entrapment neuropathy in coal miners. Am J Ind Med. 2013;56:569–575. doi: 10.1002/ajim.22163. [DOI] [PubMed] [Google Scholar]
- 18.Miranda H., Viikari-Juntura E., Heistaro S. A population study on differences in the determinants of a specific shoulder disorder versus nonspecific shoulder pain without clinical findings. Am J Epidemiol. 2005;161:847–855. doi: 10.1093/aje/kwi112. [DOI] [PubMed] [Google Scholar]
- 19.Shiri R., Varonen H., Heliövaara M. Hand dominance in upper extremity musculoskeletal disorders. J Rheumatol. 2007;34:1076–1082. [PubMed] [Google Scholar]
- 20.Chard M.D., Hazleman B.L. Shoulder disorders in the elderly (a hospital study) Ann Rheum Dis. 1987;46:684–687. doi: 10.1136/ard.46.9.684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shiri R., Viikari-Juntura E., Varonen H. Prevalence and determinants of lateral and medial epicondylitis: a population study. Am J Epidemiol. 2006;164:1065–1074. doi: 10.1093/aje/kwj325. [DOI] [PubMed] [Google Scholar]
- 22.Walker-Bone K., Palmer K.T., Reading I. Prevalence and impact of musculoskeletal disorders of the upper limb in the general population. Arthritis Rheum. 2004;51:642–651. doi: 10.1002/art.20535. [DOI] [PubMed] [Google Scholar]
- 23.Salaffi F., De Angelis R., Grassi W. Prevalence of musculoskeletal conditions in an Italian population sample: results of a regional community-based study. I. The MAPPING study. Clin Exp Rheumatol. 2005;23:819–828. [PubMed] [Google Scholar]
- 24.Tajika T., Kobayashi T., Yamamoto A. Prevalence and risk factors of lateral epicondylitis in a mountain village in Japan. J Ortho Surg. 2014;22:240–243. doi: 10.1177/230949901402200227. [DOI] [PubMed] [Google Scholar]
- 25.Darmawan L., Valkenburg H.A., Muirden K.D. The prevalence of soft tissue rheumatism. Rheumatol Int. 1995;15:121–124. doi: 10.1007/BF00302129. [DOI] [PubMed] [Google Scholar]
- 26.Horowitz G., Ben-Ari O., Brenner A. Incidence of retropharyngeal calcific tendinitis (longus colli tendinitis) in the general population. Otolaryngol Head Neck Surg. 2013;148:955–958. doi: 10.1177/0194599813482289. [DOI] [PubMed] [Google Scholar]
- 27.Koplas M.C., Schneider E., Sundaram M. Prevalence of triceps tendon tears on MRI of the elbow and clinical correlation. Skeletal Radiol. 2011;40:587–594. doi: 10.1007/s00256-010-1043-9. [DOI] [PubMed] [Google Scholar]
- 28.Alvarez-Nemegyei J., Peláez-Ballestas I., Rodriguez-Amado J. Prevalence of rheumatic regional pain syndromes in adults from Mexico: a community survey using COPCORD for screening and syndrome-specific diagnostic criteria. J Rheumatol. 2011;86:15–20. doi: 10.3899/jrheum.100953. [DOI] [PubMed] [Google Scholar]
- 29.Njobvu P., McGill P. Soft tissue rheumatic lesions and HIV infection in Zambians. J Rheumatol. 2006;33:2493–2497. [PubMed] [Google Scholar]
- 30.Shah R.R., Haghpanah S., Elovic E.P. MRI findings in painful post-stroke shoulder. Stroke. 2008;39:1808–1813. doi: 10.1161/STROKEAHA.107.502187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Frey C., Zamora J. The effects of obesity on orthopaedic foot and ankle pathology. Foot Ankle Int. 2007;28:996–999. doi: 10.3113/FAI.2007.0996. [DOI] [PubMed] [Google Scholar]
- 32.Finley M.A., Rodgers M.M. Prevalence and identification of shoulder pathology in athletic and nonathletic wheelchair users with shoulder pain: a pilot study. J Rehabil Res Dev. 2004;41:395–402. doi: 10.1682/jrrd.2003.02.0022. [DOI] [PubMed] [Google Scholar]
- 33.Monteleone G., Tramontana A., McDonald K. Ultrasonographic evaluation of the shoulder in elite Italian beach volleyball players. J Sports Med Physical Fitness. 2014 [PubMed] [Google Scholar]
- 34.Cunha-Miranda L., Carnide F., Lopes M.F. Prevalence of rheumatic occupational diseases - PROUD study. Acta Reumatol Port. 2010;35:215–226. [PubMed] [Google Scholar]
- 35.Fairley J., Toppi J., Cicuttini F.M. Association between obesity and magnetic resonance imaging defined patellar tendinopathy in community-based adults: a cross-sectional study. BMC Musculoskelet Disord. 2014;15:266–272. doi: 10.1186/1471-2474-15-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Girish G., Lobo L.G., Jacobson J.A. Ultrasound of the shoulder: asymptomatic findings in men. AJR Am J Roentgenol. 2011;197:W713–W719. doi: 10.2214/AJR.11.6971. [DOI] [PubMed] [Google Scholar]
- 37.Sansone V.C., Meroni R., Boria P. Are occupational repetitive movements of the upper arm associated with rotator cuff calcific tendinopathies? Rheumatol Int. 2015;35:273–280. doi: 10.1007/s00296-014-3086-z. [DOI] [PubMed] [Google Scholar]
- 38.Werner R.A., Franzblau A., Gell N. Prevalence of upper extremity symptoms and disorders among dental and dental hygiene students. J Calif Dent Assoc. 2005;33:123–131. [PubMed] [Google Scholar]
- 39.Zwerver J., Bredeweg S.W., van den Akker-Scheek I. Prevalence of Jumper's knee among nonelite athletes from different sports: a cross-sectional survey. Am J Sports Med. 2011;39:1984–1988. doi: 10.1177/0363546511413370. [DOI] [PubMed] [Google Scholar]
- 40.Comin J., Cook J.L., Malliaras P. The prevalence and clinical significance of sonographic tendon abnormalities in asymptomatic ballet dancers: a 24-month longitudinal study. Br J Sports Med. 2013;47:89–92. doi: 10.1136/bjsports-2012-091303. [DOI] [PubMed] [Google Scholar]
- 41.Kujala U.M., Sarna S., Kaprio J. Cumulative incidence of achilles tendon rupture and tendinopathy in male former elite athletes. Clin J Sport Med. 2005;15:133–135. doi: 10.1097/01.jsm.0000165347.55638.23. [DOI] [PubMed] [Google Scholar]
- 42.Kramer J.S., Yelin E.H., Epstein W.V. Social and economic impacts of four musculoskeletal conditions. A study using national community-based data. Arthritis Rheum. 1983;26:901–907. doi: 10.1002/art.1780260712. [DOI] [PubMed] [Google Scholar]
- 43.Bonde J.P., Mikkelsen S., Anderson J.H. Prognosis of shoulder tendonitis in repetitive work: a follow up study in a cohort of Danish industrial and service workers. Occ Environ Med. 2003;60:E8. doi: 10.1136/oem.60.9.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Walker-Bone K., Palmer K.T., Reading I. Occupation and epicondylitis: a population-based study. Rheumatology (Oxford) 2012;51:305–310. doi: 10.1093/rheumatology/ker228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Serazin C., Ha C., Bodin J. Employment and occupational outcomes of workers with musculoskeletal pain in a French region. Occ Environ Med. 2013;70:143–148. doi: 10.1136/oemed-2012-100685. [DOI] [PubMed] [Google Scholar]
- 46.Grewal R., MacDermid J.C., Shah P. Functional outcome of arthroscopic extensor carpi radialis brevis tendon release in chronic lateral epicondylitis. J Hand Surg-Am Vol. 2009;34A:849–857. doi: 10.1016/j.jhsa.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 47.Palmer K.T., Harris E.C., Coggon D. Compensating occupationally related tenosynovitis and epicondylitis: a literature review. Occ Med-Oxford. 2007;57(1):67–74. doi: 10.1093/occmed/kql127. [DOI] [PubMed] [Google Scholar]
- 48.Seil R., Litzenburger H., Kohn D. Arthroscopic treatment of chronically painful calcifying tendinitis of the supraspinatus tendon. Arthroscopy-J Arthroscopic Related Surg. 2006;22:521–527. doi: 10.1016/j.arthro.2006.01.012. [DOI] [PubMed] [Google Scholar]
- 49.Alizadehkhaiyat O., Fisher A.C., Kemp G.J. Pain, functional disability, and psychologic status in tennis elbow. Clin J Pain. 2007;23:482–489. doi: 10.1097/AJP.0b013e31805f70fa. [DOI] [PubMed] [Google Scholar]
- 50.Distribution of Median and Mean Income and Tax by Age Range and Gender. Personal Income by Tax Year 2015. Available from:https://www.gov.uk/government/statistics/distribution-of-median-and-mean-income-and-tax-by-age-range-and-gender-2010-to-2011. [accessed 12.02.16].
- 51.Population, total. 2011–2015. Available from:http://data.worldbank.org/indicator/SP.POP.TOTL [accessed 12.02.16].
- 52.Witvrouw E., Bellemans J., Lysens R. Intrinsic risk factors for the development of patellar tendinitis in an athletic population – a two-year prospective study. Am J Sports Med. 2001;29:190–195. doi: 10.1177/03635465010290021201. [DOI] [PubMed] [Google Scholar]
- 53.Dragoo J.L., Wasterlain A.S., Braun H.J. Platelet-rich plasma as a treatment for patellar tendinopathy a double-blind, randomized controlled trial. Am J Sports Med. 2014;42:610–618. doi: 10.1177/0363546513518416. [DOI] [PubMed] [Google Scholar]
- 54.Korthals-de Bos I.B.C., Smidt N., van Tulder M.W. Cost effectiveness of interventions for lateral epicondylitis – results from a randomised controlled trial in primary care. Pharmacoeconomics. 2004;22:185–195. doi: 10.2165/00019053-200422030-00004. [DOI] [PubMed] [Google Scholar]
- 55.Coombes B.K., Connelly L., Bisset L. Economic evaluation favours physiotherapy but not corticosteroid injection as a first-line intervention for chronic lateral epicondylalgia: evidence from a randomised clinical trial. Br J Sports Med. 2015 doi: 10.1136/bjsports-2015-094729. [DOI] [PubMed] [Google Scholar]
- 56.Stevenson M., Jones M.L., De Nigris E. A systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosis. Health Technol Ass. 2005;9:1–6. doi: 10.3310/hta9220. [DOI] [PubMed] [Google Scholar]
- 57.Yen Z.S., Lai M.S., Wang C.T. Cost-effectiveness of treatment strategies for osteoarthritis of the knee in Taiwan. J Rheumatol. 2004;31:1797–1803. [PubMed] [Google Scholar]
- 58.International Classification of Diseases (ICD). Classifications 2015. Available from:http://www.who.int/classifications/icd/en/. [accessed 12.02.16].
- 59.Geneva International Labour Office . Int Labour Office; Geneva, Switzerland: 2012. Safe Work, Estimating the Economic Costs of Occupational Injuries and Illnesses in Developing Countries: Essential Information for Decision Makers. [Google Scholar]
- 60.Osteoarthritis. Arthritis. 2015 http://www.cdc.gov/arthritis/basics/osteoarthritis.htm Available from: [accessed 12.02.16] [Google Scholar]
- 61.Looker A.C., Frenk S.M. 2015. Percentage of Adults Aged 65 and over with Osteoporosis or Low Bone Mass at the Femur Neck or Lumbar Spine: United States, 2005–2010.http://www.cdc.gov/nchs/data/hestat/osteoporsis/osteoporosis2005_2010.htm NCHS Health E-Stat. Available from: [accessed 12.02.16] [Google Scholar]
- 62.National Coalition for Osteoporosis and Related Bone Diseases . National Coalition for Osteoporosis and Related Bone Diseases; Washington D.C., North America: 2009. National Action Plan for Bone Health: Recommendations from the Summit for a National Action Plan for Bone Health. [Google Scholar]
- 63.Arthritis Foundation . Arthritis Foundation; USA: 2010. A National Public Health Agenda for Osteoarthritis 2010. [DOI] [PubMed] [Google Scholar]
- 64.National Arthritis and Musculoskeletal Conditions Advisory Group . 2004. Evidence to Support the National Action Plan for Osteoarthritis, Rheumatoid Arthritis and Osteoporosis: Opportunities to Improve Health-related Quality of Life and Reduce the Burden of Disease and Disability. Australian Government Department of Health and Ageing. Canberra, Australia: Editor. [Google Scholar]
- 65.Johnell O., Kanis J.A. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int. 2004;15:897–902. doi: 10.1007/s00198-004-1627-0. [DOI] [PubMed] [Google Scholar]
- 66.Thomas E., Peat G., Harris L. The prevalence of pain and pain interference in a general population of older adults: cross-sectional findings from the North Staffordshire Osteoarthritis Project (NorStOP) Pain. 2004;110:361–368. doi: 10.1016/j.pain.2004.04.017. [DOI] [PubMed] [Google Scholar]
- 67.Delaunay C. Registries in orthopaedics. Orthop Traumatol Surg Res. 2015;101(1 Suppl.):S69–S75. doi: 10.1016/j.otsr.2014.06.029. [DOI] [PubMed] [Google Scholar]
- 68.Mattila V.M., Huttunen T.T., Haapasalo H. Declining incidence of surgery for Achilles tendon rupture follows publication of major RCTs: evidence-influenced change evident using the Finnish registry study. Br J Sports Med. 2015;49(16):1084–1086. doi: 10.1136/bjsports-2013-092756. [DOI] [PubMed] [Google Scholar]
- 69.Huttunen T.T., Kannus P., Rolf C. Acute achilles tendon ruptures incidence of injury and surgery in Sweden between 2001 and 2012. Am J Sports Med. 2014;42:2419–2423. doi: 10.1177/0363546514540599. [DOI] [PubMed] [Google Scholar]
- 70.van der Linden P.D., Nab H.W., Simonian S. Fluoroquinolone use and the change in incidence of tendon ruptures in the Netherlands. Pharm World Sci. 2001;23:89–92. doi: 10.1023/a:1011254030271. [DOI] [PubMed] [Google Scholar]
- 71.Zapata A.L., Moraes A.J., Leone C. Pain and musculoskeletal pain syndromes related to computer and video game use in adolescents. Eur J Pediatr. 2006;165:408–414. doi: 10.1007/s00431-005-0018-7. [DOI] [PubMed] [Google Scholar]
- 72.Rechardt M., Shiri R., Karppinen J. Lifestyle and metabolic factors in relation to shoulder pain and rotator cuff tendinitis: a population-based study. BMC Musculoskelet Disord. 2010;11:165. doi: 10.1186/1471-2474-11-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Joseph M.F., Trojian T.H., Anderson J.M. Incidence of morphologic changes in asymptomatic achilles tendons in an active young adult population. J Sport Rehabil. 2013;22:249–253. doi: 10.1123/jsr.21.3.249. [DOI] [PubMed] [Google Scholar]
- 74.Waldecker U., Hofmann G., Drewitz S. Epidemiologic investigation of 1394 feet: coincidence of hindfoot malalignment and Achilles tendon disorders. Foot Ankle Surg. 2012;18:119–123. doi: 10.1016/j.fas.2011.04.007. [DOI] [PubMed] [Google Scholar]
- 75.Schibany N., Zehetgruber H., Kainberger F. Rotator cuff tears in asymptomatic individuals: a clinical and ultrasonographic screening study. Eur J Radiol. 2004;51:263–268. doi: 10.1016/S0720-048X(03)00159-1. [DOI] [PubMed] [Google Scholar]
- 76.Safran M.R., Graham S.M. Distal biceps tendon ruptures: incidence, demographics, and the effect of smoking. Clin Orthop Relat Res. 2002;404:275–283. [PubMed] [Google Scholar]
- 77.Ostor A.J., Richards C.A., Prevost A.T. Diagnosis and relation to general health of shoulder disorders presenting to primary care. Rheumatology (Oxford) 2005;44:800–805. doi: 10.1093/rheumatology/keh598. [DOI] [PubMed] [Google Scholar]
- 78.Cretnik A., Kosir R., Kosanovic M. Incidence and outcome of operatively treated achilles tendon rupture in the elderly. Foot Ankle Int. 2010;31:14–18. doi: 10.3113/FAI.2010.0014. [DOI] [PubMed] [Google Scholar]
- 79.Moller A., Astron M., Westlin N. Increasing incidence of Achilles tendon rupture. Acta Orthop Scand. 1996;67:479–481. doi: 10.3109/17453679608996672. [DOI] [PubMed] [Google Scholar]
- 80.Clayton R.A., Court-Brown C.M. The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury. 2008;39:1338–1344. doi: 10.1016/j.injury.2008.06.021. [DOI] [PubMed] [Google Scholar]
- 81.Levi N. The incidence of Achilles tendon rupture in Copenhagen. Injury. 1997;28:311–313. doi: 10.1016/s0020-1383(96)00200-8. [DOI] [PubMed] [Google Scholar]
- 82.Leppilahti J., Puranen J., Orava S. Incidence of Achilles tendon rupture. Acta Orthop Scand. 1996;67:277–279. doi: 10.3109/17453679608994688. [DOI] [PubMed] [Google Scholar]
- 83.Houshian S., Tscherning T., Riegels-Nielsen P. The epidemiology of Achilles tendon rupture in a Danish county. Injury. 1998;29:651–654. doi: 10.1016/s0020-1383(98)00147-8. [DOI] [PubMed] [Google Scholar]
- 84.Maffulli N., Waterston S.W., Squair J. Changing incidence of Achilles tendon rupture in Scotland: a 15-year study. Clin J Sport Med. 1999;9:157–160. doi: 10.1097/00042752-199907000-00007. [DOI] [PubMed] [Google Scholar]
- 85.Suchak A.A., Bostick G., Reid D. The incidence of Achilles tendon ruptures in Edmonton, Canada. Foot Ankle Int. 2005;26:932–936. doi: 10.1177/107110070502601106. [DOI] [PubMed] [Google Scholar]
- 86.de Jonge S., van den Berg C., de Vos R.J. Incidence of midportion Achilles tendinopathy in the general population. Br J Sports Med. 2011;45:1026–1028. doi: 10.1136/bjsports-2011-090342. [DOI] [PubMed] [Google Scholar]
- 87.Nyyssonen T., Luthje, Kroger H. The increasing incidence and difference in sex distribution of Achilles tendon rupture in Finland in 1987-1999. Scand J Surg. 2008;97:272–275. doi: 10.1177/145749690809700312. [DOI] [PubMed] [Google Scholar]
- 88.McCormack R.R., Jr., Inman R.D., Wells A. Prevalence of tendinitis and related disorders of the upper extremity in a manufacturing workforce. J Rheumatol. 1990;17 958–694. [PubMed] [Google Scholar]
- 89.Almeida M.C., Cezar-Vaz M.R., Soares J.F. The prevalence of musculoskeletal diseases among casual dock workers. Rev Lat Am Enfermagem. 2012;20:243–250. doi: 10.1590/s0104-11692012000200005. [DOI] [PubMed] [Google Scholar]
- 90.Frost P., Bonde J.P., Mikkelsen S. Risk of shoulder tendinitis in relation to shoulder loads in monotonous repetitive work. Am J Ind Med. 2002;41:11–18. doi: 10.1002/ajim.10019. [DOI] [PubMed] [Google Scholar]
- 91.Descatha A., Leclerc A., Chastang J.F. Medial epicondylitis in occupational settings: prevalence, incidence and associated risk factors. J Occup Environ Med. 2003;45:993–1001. doi: 10.1097/01.jom.0000085888.37273.d9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Fan Z.J., Silverstein B.A., Bao S. Quantitative exposure-response relations between physical workload and prevalence of lateral epicondylitis in a working population. Am J Ind Med. 2009;52:479–490. doi: 10.1002/ajim.20700. [DOI] [PubMed] [Google Scholar]
- 93.Rosenbaum D.A., Grzywacz J.G., Chen H. Prevalence of epicondylitis, rotator cuff syndrome, and low back pain in Latino poultry workers and manual laborers. Am J Ind Med. 2013;56:226–234. doi: 10.1002/ajim.22127. [DOI] [PubMed] [Google Scholar]
- 94.Kryger A.I., Lassen C.F., Andersen J.H. The role of physical examinations in studies of musculoskeletal disorders of the elbow. Occup Environ Med. 2007;64:776–781. doi: 10.1136/oem.2005.026260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kaergaard A., Andersen J.H. Musculoskeletal disorders of the neck and shoulders in female sewing machine operators: prevalence, incidence, and prognosis. Occup Environ Med. 2000;57:528–534. doi: 10.1136/oem.57.8.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Dimberg L. The prevalence and causation of tennis elbow (lateral humeral epicondylitis) in a population of workers in an engineering industry. Ergonimics. 1987;30:573–579. doi: 10.1080/00140138708969746. [DOI] [PubMed] [Google Scholar]
- 97.Roto P., Kivi P. Prevalence of epicondylitis and tenosynovitis among meatcutters. Scand J Work, Environ Health. 1984;10:203–205. doi: 10.5271/sjweh.2344. [DOI] [PubMed] [Google Scholar]
- 98.Ono Y., Nakamura R., Shimaoka M. Epicondylitis among cooks in nursery schools. Occup Environ Med. 1998;55:172–179. doi: 10.1136/oem.55.3.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Leclerc A., Landre M.F., Chastang J.F. Upper-limb disorders in repetitive work. Scand J Work Environ Health. 2001;27:268–278. doi: 10.5271/sjweh.614. [DOI] [PubMed] [Google Scholar]
- 100.Capone A.C., Parikh P.M., Gatti M.E. Occupational injury in plastic surgeons. Plast Reconstr Surg. 2010;125:1555–1561. doi: 10.1097/PRS.0b013e3181d62a94. [DOI] [PubMed] [Google Scholar]
- 101.Ritz B.R. Humeral epicondylitis among gas- and waterworks employees. Scand J Work Environ Health. 1995;21:478–486. doi: 10.5271/sjweh.64. [DOI] [PubMed] [Google Scholar]
- 102.Chiang H., Ko Y.C., Chen S.S. Prevalence of shoulder and upper-limb disorders among workers in the fish-processing industry. Scand J Work Environ Health. 1993;19:126–131. doi: 10.5271/sjweh.1496. [DOI] [PubMed] [Google Scholar]
- 103.Barrero L.H., Pulido J.A., Berrio S. Physical workloads of the upper-extremity among workers of the Colombian flower industry. Am J Ind Med. 2012;55:926–939. doi: 10.1002/ajim.22102. [DOI] [PubMed] [Google Scholar]
- 104.Forde M.S., Punnett L., Wegman D.H. Prevalence of musculoskeletal disorders in union ironworkers. J Occup Environ Hyg. 2005;2:203–212. doi: 10.1080/15459620590929635. [DOI] [PubMed] [Google Scholar]
- 105.Werner R.A., Hamann C., Franzblau A. Prevalence of carpal tunnel syndrome and upper extremity tendinitis among dental hygienists. J Dent Hyg. 2002;76:126–132. [PubMed] [Google Scholar]
- 106.Gold J.E., d'Errico A., Katz J.N. Specific and non-specific upper extremity musculoskeletal disorder syndromes in automobile manufacturing workers. Am J Ind Med. 2009;52:124–132. doi: 10.1002/ajim.20653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Pullopdissakul S., Ekpanyaskul C., Taptagaporn S. Upper extremities musculoskeletal disorders: prevalence and associated ergonomic factors in an electronic assembly factory. Int J Occup Med Environ Health. 2013;26:751–761. doi: 10.2478/s13382-013-0150-y. [DOI] [PubMed] [Google Scholar]
- 108.Nordander C., Ohlsson K., Akesson I. Risk of musculoskeletal disorders among females and males in repetitive/constrained work. Ergonomics. 2009;52:1226–1239. doi: 10.1080/00140130903056071. [DOI] [PubMed] [Google Scholar]
- 109.Silverstein B.A., Viikari-Juntura E., Fan Z.J. Natural course of nontraumatic rotator cuff tendinitis and shoulder symptoms in a working population. Scand J Work Environ Health. 2006;32:99–108. doi: 10.5271/sjweh.985. [DOI] [PubMed] [Google Scholar]
- 110.Fan Z.J., Bao S., Silverstein B.A. Predicting work-related incidence of lateral and medial epicondylitis using the strain index. Am J Ind Med. 2014;57:1319–1330. doi: 10.1002/ajim.22383. [DOI] [PubMed] [Google Scholar]
- 111.Garg A., Kapellusch J.M., Hegmann K.T. The strain index and TLV for HAL: risk of lateral epicondylitis in a prospective cohort. Am J Ind Med. 2014;57:286–302. doi: 10.1002/ajim.22279. [DOI] [PubMed] [Google Scholar]
- 112.Alexandre P.C., da Silva I.C., de Souza L.M. Musculoskeletal disorders among Brazilian dentists. Arch Environ Occup Health. 2011;66:231–235. doi: 10.1080/19338244.2011.564571. [DOI] [PubMed] [Google Scholar]
- 113.Herquelot E., Bodin J., Roquelaure Y. Work-related risk factors for lateral epicondylitis and other cause of elbow pain in the working population. Am J Ind Med. 2013;56:400–409. doi: 10.1002/ajim.22140. [DOI] [PubMed] [Google Scholar]
- 114.Werner R.A., Franzblau A., Gell N. A longitudinal study of industrial and clerical workers: predictors of upper extremity tendonitis. J Occ Rehabil. 2005;15:37–46. doi: 10.1007/s10926-005-0872-1. [DOI] [PubMed] [Google Scholar]
- 115.Fan Z.J., Silverstein B.A., Bao S. The association between combination of hand force and forearm posture and incidence of lateral epicondylitis in a working population. Hum Factors. 2014;56:151–165. doi: 10.1177/0018720813492327. [DOI] [PubMed] [Google Scholar]
- 116.Descatha A., Dale A.M., Jaegers L. Self-reported physical exposure association with medial and lateral epicondylitis incidence in a large longitudinal study. Occup Environ Med. 2013;70:670–673. doi: 10.1136/oemed-2012-101341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.McGaughey I., Sullivan P. The epidemiology of knee and ankle injuries on Macquarie Island. Injury. 2003;34:842–846. doi: 10.1016/s0020-1383(03)00032-9. [DOI] [PubMed] [Google Scholar]
- 118.Barber Foss K.D., Myer G.D., Chen S.S. Expected prevalence from the differential diagnosis of anterior knee pain in adolescent female athletes during preparticipation screening. J Athl Train. 2012;47:519–524. doi: 10.4085/1062-6050-47.5.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Emerson C., Morrissey D., Perry M. Ultrasonographically detected changes in Achilles tendons and self reported symptoms in elite gymnasts compared with controls–an observational study. Man Ther. 2010;15:37–42. doi: 10.1016/j.math.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 120.Steinberg N., Siev-Ner I., Peleg S. Injury patterns in young, non-professional dancers. J Sports Sci. 2011;29:47–54. doi: 10.1080/02640414.2010.521167. [DOI] [PubMed] [Google Scholar]
- 121.Gisslen K., Gyulai C., Soderman K. High prevalence of jumper's knee and sonographic changes in Swedish elite junior volleyball players compared to matched controls. Br J Sports Med. 2005;39:298–301. doi: 10.1136/bjsm.2004.014290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Le Gall F., Carling C., Reilly T. Biological maturity and injury in elite youth football. Scand J Med Sci Sports. 2007;17:564–572. doi: 10.1111/j.1600-0838.2006.00594.x. [DOI] [PubMed] [Google Scholar]
- 123.Barber Foss K.D., Myer G.D., Hewett T.E. Epidemiology of basketball, soccer, and volleyball injuries in middle-school female athletes. Phys Sportsmed. 2014;42:146–153. doi: 10.3810/psm.2014.05.2066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Beachy G., Rauh M. Middle school injuries: a 20-year (1988-2008) multisport evaluation. J Athl Train. 2014;49:493–506. doi: 10.4085/1062-6050-49.2.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Leanderson C., Leanderson J., Wykman A. Musculoskeletal injuries in young ballet dancers. Knee Surg Sports Traumatol Arthrosc. 2011;19:1531–1535. doi: 10.1007/s00167-011-1445-9. [DOI] [PubMed] [Google Scholar]
- 126.Hickey G.J., Fricker P.A., McDonald W.A. Injuries of young elite female basketball players over a six-year period. Clin J Sport Med. 1997;7:252–256. doi: 10.1097/00042752-199710000-00002. [DOI] [PubMed] [Google Scholar]
- 127.Dubravcic-Simunjak S., Pecina M., Kuipers H. The incidence of injuries in elite junior figure skaters. Am J Sports Med. 2003;31:511–517. doi: 10.1177/03635465030310040601. [DOI] [PubMed] [Google Scholar]
- 128.Hagglund M., Zwerver J., Ekstrand J. Epidemiology of patellar tendinopathy in elite male soccer players. Am J Sports Med. 2011;39:1906–1911. doi: 10.1177/0363546511408877. [DOI] [PubMed] [Google Scholar]
- 129.Durcan L., Coole A., McCarthy E. The prevalence of patellar tendinopathy in elite academy rugby: a clinical and imaging study. J Sci Med Sport. 2014;17:173–176. doi: 10.1016/j.jsams.2013.05.014. [DOI] [PubMed] [Google Scholar]
- 130.Cook J.L., Khan K.M., Harcourt P.R. Patellar tendon ultrasonography in asymptomatic active athletes reveals hypoechoic regions: a study of 320 tendons. Victorian Institute of Sport Tendon Study Group. Clin J Sport Med. 1998;8:73–77. doi: 10.1097/00042752-199804000-00001. [DOI] [PubMed] [Google Scholar]
- 131.Rooks M.D., Johnston R.B., Ensor C.D. Injury patterns in recreational rock climbers. Am J Sports Med. 1995;23:683–685. doi: 10.1177/036354659502300608. [DOI] [PubMed] [Google Scholar]
- 132.Walls R.J., Brennan S.A., Hodnett P. Overuse ankle injuries in professional Irish dancers. Foot Ankle Surg. 2010;16:45–49. doi: 10.1016/j.fas.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 133.Hagemann G., Rijke A.M., Mars M. Shoulder pathoanatomy in marathon kayakers. Br J Sports Med. 2004;38:413–417. doi: 10.1136/bjsm.2002.003699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Reuter R.M., Hiller W.D., Ainge G.R. Ironman triathletes: MRI assessment of the shoulder. Skeletal Radiol. 2008;37:737–741. doi: 10.1007/s00256-008-0516-6. [DOI] [PubMed] [Google Scholar]
- 135.Hadala M., Barrios C. Sports injuries in an America's Cup yachting crew: a 4-year epidemiological study covering the 2007 challenge. J Sports Sci. 2009;27:711–717. doi: 10.1080/02640410902785487. [DOI] [PubMed] [Google Scholar]
- 136.Marshall S.W., Hamstra-Wright K.L., Dick R. Descriptive epidemiology of collegiate women's softball injuries: national Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2003–2004. J Athl Train. 2007;42:286–294. [PMC free article] [PubMed] [Google Scholar]
- 137.Krupnick J.E., Cox R.D., Summers R.L. Injuries sustained during competitive white-water paddling: a survey of athletes in the 1996 Olympic trials. Wilderness Environ Med. 1998;9:14–18. doi: 10.1580/1080-6032(1998)009[0014:isdcww]2.3.co;2. [DOI] [PubMed] [Google Scholar]
- 138.Kelly B.T., Barnes R.P., Powell J.W. Shoulder injuries to quarterbacks in the national football league. Am J Sports Med. 2004;32:328–331. doi: 10.1177/0363546503261737. [DOI] [PubMed] [Google Scholar]
- 139.Parekh S.G., Wray W.H., 3rd, Brimmo O. Epidemiology and outcomes of Achilles tendon ruptures in the National Football League. Foot Ankle Spec. 2009;2:283–286. doi: 10.1177/1938640009351138. [DOI] [PubMed] [Google Scholar]
- 140.Heir T., Glomsaker Epidemiology of musculoskeletal injuries among Norwegian conscripts undergoing basic military training. Scand J Med Sci Sports. 1996;6:186–191. doi: 10.1111/j.1600-0838.1996.tb00088.x. [DOI] [PubMed] [Google Scholar]
- 141.Wolf J.M., Mountcastle S., Burks R. Epidemiology of lateral and medial epicondylitis in a military population. Mil Med. 2010;175:336–339. doi: 10.7205/milmed-d-09-00086. [DOI] [PubMed] [Google Scholar]
- 142.McFarland E.G., Wasik M. Epidemiology of collegiate baseball injuries. Clin J Sport Med. 1998;8:10–13. doi: 10.1097/00042752-199801000-00003. [DOI] [PubMed] [Google Scholar]
- 143.White D.W., Wenke J.C., Mosely D.S. Incidence of major tendon ruptures and anterior cruciate ligament tears in US Army soldiers. Am J Sports Med. 2007;35:1308–1314. doi: 10.1177/0363546507301256. [DOI] [PubMed] [Google Scholar]
- 144.Milgrom C., Finestone A., Zin D. Cold weather training: a risk factor for achilles paratendinitis among recruits. Foot & Ankle Int. 2003;24:398–401. doi: 10.1177/107110070302400504. [DOI] [PubMed] [Google Scholar]
- 145.Kettunen J.A., Kujala U., Sarna S. Cumulative incidence of shoulder region tendon injuries in male former elite athletes. Int J Sports Med. 2011;32:451–454. doi: 10.1055/s-0031-1273701. [DOI] [PubMed] [Google Scholar]
- 146.Cannon D.E., Dillingham T.R., Miao H. Musculoskeletal disorders in referrals for suspected cervical radiculopathy. Arch Phys Med Rehabil. 2007;88:1256–1259. doi: 10.1016/j.apmr.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 147.Hautmann M.G., Neumaier U., Kolbl O. Re-irradiation for painful heel spur syndrome. Retrospective analysis of 101 heels. Strahlenther Onkol. 2014;190:298–303. doi: 10.1007/s00066-013-0462-7. [DOI] [PubMed] [Google Scholar]
- 148.Baumann B., Genning K., Bohm D. Arthroscopic prevalence of pulley lesions in 1007 consecutive patients. J Shoulder Elbow Surg. 2008;17:14–20. doi: 10.1016/j.jse.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 149.Chhajed P.N., Plit M.L., Hopkins P.M. Achilles tendon disease in lung transplant recipients: association with ciprofloxacin. Eur Respir J. 2002;19:469–471. doi: 10.1183/09031936.02.00257202. [DOI] [PubMed] [Google Scholar]
- 150.Ramirez J., Pomes I., Sobrino-Guijarro B. Ultrasound evaluation of greater trochanter pain syndrome in patients with spondyloarthritis: are there any specific features? Rheumatol Int. 2014;34:947–952. doi: 10.1007/s00296-014-2947-9. [DOI] [PubMed] [Google Scholar]
- 151.Taunton J.E., Ryan M.B., Clement D.B. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med. 2002;36:95–101. doi: 10.1136/bjsm.36.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Bird P.A., Oakley S.P., Shnier R. Prospective evaluation of magnetic resonance imaging and physical examination findings in patients with greater trochanteric pain syndrome. Arthritis Rheum. 2001;44:2138–2145. doi: 10.1002/1529-0131(200109)44:9<2138::AID-ART367>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 153.Pong Y., Wang L.Y., Huang Y.C. Sonography and physical findings in stroke patients with hemiplegic shoulders: a longitudinal study. J Rehabil Med. 2012;44:553–557. doi: 10.2340/16501977-0987. [DOI] [PubMed] [Google Scholar]
- 154.Kingzett-Taylor A., Tirman P.F.J., Feller J. Tendinosis and tears of gluteus medius and minimus muscles as a cause of hip pain: MR imaging findings. AJR Am J Roentgenol. 1999;173:1123–1126. doi: 10.2214/ajr.173.4.10511191. [DOI] [PubMed] [Google Scholar]
- 155.Chung Y.C., Hung C.T., Li S.F. Risk of musculoskeletal disorder among Taiwanese nurses cohort: a nationwide population-based study. BMC Musculoskelet Disord. 2013;14:144. doi: 10.1186/1471-2474-14-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Barge-Caballero E., Crespo-Leiro M.G., Paniagua-Martin M.J. Quinolone-related Achilles tendinopathy in heart transplant patients: incidence and risk factors. J Heart Lung Transplant. 2008;27:46–51. doi: 10.1016/j.healun.2007.09.021. [DOI] [PubMed] [Google Scholar]
- 157.Ramos L.A., Carvalho R.T., Garms E. Prevalence of pain on palpation of the inferior pole of the patella among patients with complaints of knee pain. Clinics. 2009;64:199–202. doi: 10.1590/S1807-59322009000300009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Helliwell P.S. Towards epidemiological criteria for soft-tissue disorders of the arm. Occ Med. 2003;53:313–319. doi: 10.1093/occmed/kqg034. [DOI] [PubMed] [Google Scholar]
- 159.Sode J., Obel N., Hallas J. Use of fluroquinolone and risk of Achilles tendon rupture: a population-based cohort study. Eur J Clin Pharmacol. 2007;63:499–503. doi: 10.1007/s00228-007-0265-9. [DOI] [PubMed] [Google Scholar]
- 160.Zakaria M.H., Davis W.A., Davis T.M. Incidence and predictors of hospitalization for tendon rupture in type 2 diabetes: the Fremantle diabetes study. Diabet Med. 2014;31:425–430. doi: 10.1111/dme.12344. [DOI] [PubMed] [Google Scholar]