Abstract
Purpose
African medical schools are expanding, straining resources at tertiary health facilities. Decentralizing clinical training can alleviate this tension. This study assessed the impact of decentralized training and contribution of undergraduate medical students at health facilities.
Method
Participants were from 11 Medical Education Partnership Initiative–funded medical schools in 10 African countries. Each school identified two clinical training sites—one rural and the other either peri-urban or urban. Qualitative and quantitative data collection tools were used to gather information about the sites, student activities, and staff perspectives between March 2015 and February 2016. Interviews with site staff were analyzed using a collaborative directed approach to content analysis, and frequencies were generated to describe site characteristics and student experiences.
Results
The clinical sites varied in level of care but were similar in scope of clinical services and types of clinical and nonclinical student activities. Staff indicated that students have a positive effect on job satisfaction and workload. Respondents reported that students improved the work environment, institutional reputation, and introduced evidence-based approaches. Students also contributed to perceived improvements in quality of care, patient experience, and community outreach. Staff highlighted the need for resources to support students.
Conclusions
Students were seen as valuable resources for health facilities. They strengthened health care quality by supporting overburdened staff and by bringing rigor and accountability into the work environment. As medical schools expand, especially in low-resource settings, mobilizing new and existing resources for decentralized clinical training could transform health facilities into vibrant service and learning environments.
The World Health Organization (WHO) recently released the report “Global Strategy on Human Resources for Health: Workforce 2030,” highlighting the need for an estimated 14 million additional health workers, appropriately trained to meet the needs of the communities they will serve.1 To meet these demands, medical education institutions will need to innovate in the way they train health professionals to increase student numbers and to provide clinical education that prepares students for the case mix, demographics, and resources available in the communities they will serve.
In Sub-Saharan Africa, the demand for physicians has prompted considerable growth in the number of medical schools and student enrollment.2 In 2011, of 168 Sub-Saharan African medical schools, 60 (35%) had opened in the 25 years prior.2 Such rapid expansion has placed considerable strain on educational facilities, particularly teaching hospitals, where direct student–patient and student–supervisor interactions form the basis for traditional learning. One strategy used to mitigate this strain is to decentralize clinical training, or send medical students to non-tertiary-care settings for clinical rotations.3,4
Decentralized training at district hospitals and community health facilities has long been a part of medical education as an approach to provide students exposure to different levels of care and a broader case mix than they would typically encounter at teaching hospitals.5–8 The WHO recommends decentralized placements for training as an important part of the strategy to expand the primary care and rural workforce.9
Decentralization of training sites requires medical schools to address the tension that exists between educational institutions—driven primarily by the need to produce competent graduates—and health service facilities, which have a primary mission to care for patients, often with limited human and physical resources. Worley et al10 have written about a symbiotic medical education system where students are an integral part of a mutually beneficial relationship between such stakeholders. Yet, while much has been written about the benefit to students of training in community settings, the value to health facilities is less clear.11,12 Students learn about community medicine and social determinants of health, yet little is known about students’ contribution to patient care, particularly in low-resource settings,3,4,10,13 and few studies describe medical students’ impact on staff or patient satisfaction.14,15
The Medical Education Partnership Initiative (MEPI), a U.S. government-funded program to improve the health workforce in Africa, brought together a network of medical schools in the region and provided a timely opportunity to examine this issue further. MEPI was a five-year effort (2010–2015) to increase the capacity and quality of medical education in Africa. MEPI directly supported 11 medical schools in 10 African countries through programmatic grants, and funding was leveraged toward three overarching themes: (1) increasing training capacity in schools, (2) improving the retention of graduates in-country, and (3) increasing the capacity for local research.16 Schools determined how they would use their funding based on local priorities. Therefore, funding was used for a wide range of educational activities including, but not limited to, improving clinical training sites. One common area where schools invested efforts was evaluation of their education activities, particularly in decentralizing clinical training and strengthening community-based education (CBE).3,4
A number of technical working groups (TWGs) were established to facilitate discussion and collaboration among MEPI-funded schools. One such group was the CBE TWG, which brought together faculty that played leadership roles in facilitating student learning at district and community health facilities. A previous publication emanating from this TWG detailed the different types of community-based training the schools provide.4 In this report we describe a unique collaborative study conducted by some members of the CBE TWG, and we investigate how undergraduate medical students impact the staff and services of health facilities where they train.
TWG members recognized that efforts to strengthen and expand decentralized education would require sustained commitment and investment and, therefore, decided to collaborate on research that would demonstrate the value of their education activities to the broader health system. They aimed to produce research and evaluation that could engage both traditional stakeholders of medical education as well as investors in health system strengthening who may not typically invest in education or health workforce. MEPI, therefore, served as a catalyst for this collaborative study.
To better understand the relationship between education activities and health services, we determined that a qualitative approach would be best. From previous literature and site visits to the MEPI-participating schools, and from TWG members’ experiences in each country, we developed a common framework that linked academic activity to potential impact on health facilities (Figure 1).3,4,13–22 Developing this framework allowed our study team, with members from 10 different countries, to identify common elements of education activities and common areas of intersection between medical students and health facilities such as staff interactions, quality of care, patient experiences, and facility outreach. In this study we used this common framework to extend the understanding of how undergraduate medical students can make contributions to the health facilities where they train.
Figure 1.
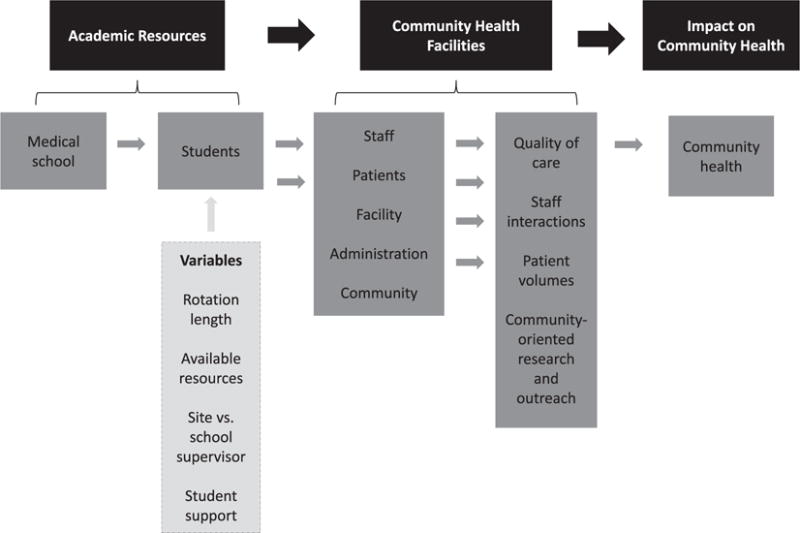
Common framework linking academic activity to impact on health facilities. This framework describes how, theoretically, components of academic resources influence community health facilities and ultimately contribute to improved community health. Academic resources consist of medical schools and students. Community health facilities consist of staff, patients, facilities, administration, and communities. These facility components influence patient care, the care environment, and the ability of the facility to engage in community-oriented outreach. Ultimately, the academic resources and community health facility resources converge to influence health outcomes.
Method
Members of MEPI’s CBE TWG conducted a study involving 11 MEPI schools (see List 1).22 This report focuses on a qualitative analysis of key informant interviews and provides a descriptive summary of survey findings, which illustrate study site characteristics and student activities. Our study team included faculty from George Washington University (GWU), which served as the coordinating center for MEPI; regional experts in CBE; and representatives from each MEPI-funded medical school, who were appointed by the relevant principal investigator. Z.T. led the study team in close consultation with study team members from GWU and from the CBE TWG who have relevant expertise in qualitative research and decentralized training (S.v.S., I.C., S.P., K.T., and S.B.). In addition, all of the authors contributed to the study design and collectively determined the data collection approach and the type of data collected to ensure both relevance and feasibility in each of their contexts. The study team members who initially coded and analyzed the data were Z.T., S.P., and K.T., who were all part of the GWU coordinating center and had no formal affiliation with any participating sites. The GWU Office of Human Research deemed the study to be exempt from human subjects research requirements. Approval from the institutional review boards (IRBs) at three of the 11 schools was covered by the approval obtained for evaluation of their respective MEPI parent programs. The remaining 8 schools obtained approval specifically for the study from local authorities (institutional IRB and/or ministry of health).
List 1. The 11 Schools Participating in the Medical Education Partnership Initiative Community-Based Education Study, 2015–2016.
Ethiopia
Addis Ababa University
Uganda
Makerere University
Mozambique
Universidade Eduardo Mondlane
South Africa
University of KwaZulu Natal
Stellenbosch University
Zambia
University of Zambia
Tanzania
Kilimanjaro Christian Medical University College
Botswana
University of Botswana
Nigeria
University of Ibadan
Kenya
University of Nairobi
Zimbabwe
University of Zimbabwe
Sites and respondents
Representatives from the 11 schools each identified two health facilities where undergraduate medical students were assigned to provide facility-based clinical care. The number of sites was based on the feasibility of each school to assign internal resources for data collection. The clinical training sites were purposefully selected in terms of setting (each school identified one rural and one peri-urban/urban site), actors (undergraduate medical students), and events (a site for medical student clinical rotations). The inclusion of rural, peri-urban, and urban sites ensured a diversity of clinical training sites. Peri-urban was defined as around a city or town.23 We identified and interviewed three facility staff at each site (key informants), who met the following criteria: (1) the health facility manager responsible for day-to-day operations; (2) a clinical supervisor who was a health care provider and engaged in direct clinical oversight of medical students; and (3) a health care provider who did not directly supervise students. If more than one staff member qualified for one of the three roles, then key informants were identified through convenience sampling based on availability.
Data collection and analysis
The team administered a common data collection tool (a semistructured interview guide; see Supplemental Digital Appendix 1 at http://links.lww.com/ACADMED/A492) at all sites. The guide also included a brief quantitative survey to document the scope of services provided and student activities at each site. This report presents the results from qualitative data analysis along with a description of the quantitative survey findings. The interview guide and data collection process were pretested at the Abosa Health Center, within Addis Ababa University’s rural training sites in January 2015. Revisions to the interview guide were made based on the lessons learned from this pilot site.
Study team members from each school received training via Skype on using the interview guide for qualitative research and were responsible for then conducting interviews at their respective CBE sites. Data were collected between March 2015 and February 2016 depending on in-country factors such as duration of the IRB approval process and participants’ availability. Most key informants were interviewed in person at the health facility where they worked; however, a few interviews were conducted by phone when meeting in person was not possible. Written consent was obtained from all interviewees. Interviews lasted 50 to 55 minutes and were audio recorded and transcribed by the study team representative at each school. Nine schools conducted interviews in English. For the remaining two universities, interviews were in some instances conducted in Setswana (at University of Botswana) and Afrikaans (at Stellenbosch University). A qualified translator translated the transcripts, and interviewers then reviewed the final translated transcripts before analysis.
Transcribed interviews were returned to the MEPI coordinating center, where all the transcripts were securely stored and only accessed by Z.T., S.P., and K.T. Data were initially analyzed by these three researchers using NVivo 10 (QSR International, Melbourne, Victoria, Australia), qualitative research software. To analyze the text, a directed approach to content analysis that aims to “validate or conceptually extend” an existing framework was used.24 To guide the analysis, an initial codebook was developed by Z.T. and S.P. based on the common framework developed by the study team (Figure 1). Data were first categorized using the framework codes, and then an inductive approach was used to code according to the emerging themes. Each transcript was coded twice. To address reflexivity, the researchers met intermittently to discuss emerging themes and agree on additional codes.25 To establish validity of findings, a matrix was created in Microsoft Excel (Microsoft Corporation, Redmond, Washington) which provided a visual summary of major themes and subthemes along with school summaries, which demonstrated how data from each school were coded. School representatives then reviewed these summaries and reported their feedback. Z.T., S.v.S., I.C., S.P., and K.T. led the final manuscript preparation, with the remaining authors involved in writing, reviewing, and revising. Data from the quantitative survey were compiled and tabulated in Microsoft Excel.
Results
A total of 61 interviews were conducted from 21 sites. One urban site selected did not meet criteria and was not included in the analysis. At two sites there were only two individuals who met the criteria for key informants. The data presented include descriptions of the clinical sites (Table 1) and activities students engage in (Table 2), and a list of themes with illustrative quotes derived from interviews (Table 3). The majority of the clinical sites studied had fewer than 20 physicians, and just over half were either urban or peri-urban. Half were funded by their respective governments, while the remainder were private, faith based, or a combination. All facilities had overnight beds, and all sites provided a range of clinical services including acute care, obstetrics, pediatrics, family planning, HIV care, and tuberculosis care. The majority of sites employed nonphysician providers including midwives (21 sites), nurses (21 sites), pharmacists (20 sites), and lab technologists (13 sites).
Table 1.
Characteristics of 21 Decentralized Clinical Training Sites From 11 Medical Education Partnership Initiative–Funded Schoolsa in Sub-Saharan Africa, 2015–2016
| Characteristic | No. (%) |
|---|---|
| Facility type | |
| Urban | 5 (24) |
| Peri-urban | 7 (33) |
| Rural | 9 (43) |
| Level of care provided | |
| District only | 12 (57) |
| Community only | 3 (14) |
| Multiple typesb | 6 (29) |
| Overnight beds | |
| Yes | 21 (100) |
| Ambulatory clinic | |
| Yes | 20 (95) |
| No | 1 (5) |
| Patients seen in ambulatory/outpatient clinicc | |
| ≤ 100 per day | 7 (33) |
| 101–270 per day | 10 (48) |
| > 270 per day | 1 (5) |
| Health services provided | |
| General acute care | 21 (100) |
| Obstetrics | 21 (100) |
| Child health | 21 (100) |
| HIV care | 21 (100) |
| Family planning | 21 (100) |
| Tuberculous care | 19 (90) |
| Mental health | 16 (76) |
| Other specialty servicesd | 2 (10) |
| Cadres of providers at site | |
| Doctors | 19 (90) |
| Nurses | 21 (100) |
| Pharmacists | 20 (95) |
| Midwives | 21 (100) |
| Lab techs/scientist | 13 (62) |
| Health/clinical officer | 7 (33) |
| Othere | 18 (86) |
| Number of doctors | |
| ≤ 20 | 13 (62) |
| 21–42 | 6 (29) |
| Not applicable (Addis Ababa sites) | 2 (10) |
| Number of nursesf | |
| ≤ 50 | 11 (52) |
| 51–100 | 2 (10) |
| 101–200 | 3 (14) |
| 201–285 | 2 (10) |
| ≥ 286 | 1 (5) |
| Funding sources | |
| Government only | 10 (48) |
| Faith-based only | 1 (5) |
| Multiple sourcesg | 10 (48) |
For a complete list of participating schools, see List 1.
Various combinations of district, community, and national.
Variable does not sum to 21 because one site in Mozambique does not have an ambulatory/outpatient clinic. Both sites from Kwazulu-Natal are missing data.
Oncology, specialties in maxillo-facial surgery, otolaryngology, general surgery, anesthesiology, physiotherapy, occupational health, dietetics, and nutrition.
Lay counselors, health education assistants, medical record clerks, health auxiliaries, nurse orderlies, social workers, nurse auxiliaries, physiotherapists, community health extension workers, community health workers, speech therapists, dieticians, occupational therapists, dentists, pharmaceutical technologists, pharmaceutical technicians, nutritionists, dispensers, volunteers, pharmacy techs, rehab therapists, radiologists, rehabilitation techs, nurse aides, anesthetists, counselors, social workers, psychiatrists, radiographers, speech/language/healing therapists, audiologists, clinical psychologists.
Missing data for both Kwazulu-Natal sites.
Includes mix of government, faith-based organizations, nongovernmental organizations, United States Agency for International Development, private partners, and/or development partners.
Table 2.
Characteristics of Student Experiences at 21 Decentralized Clinical Training Sites From 11 Medical Education Partnership Initiative–Funded Schoolsa in Sub-Saharan Africa, 2015–2016
| Characteristic | No. (%) |
|---|---|
| Type of students coming to the facility | |
| Medical | 20 (95) |
| Pharmacy | 3 (14) |
| Lab technology | 3 (14) |
| Nursing | 14 (67) |
| Health extension | 4 (19) |
| Officers (clinical, etc.) | 6 (29) |
| Otherb | 16 (76) |
| Number of students (medical) at oncec | |
| 1–25 | 18 (86) |
| 26–50 | 2 (10) |
| Duration of student rotation | |
| 2–4 weeks | 5 (24) |
| 6 weeks | 5 (24) |
| 8 weeks | 8 (38) |
| 12 weeks | 1 (5) |
| 44 weeks | 1 (5) |
| Variousd | 1 (5) |
| Number of weeks with no students | |
| 0–8 weeks | 11 (52) |
| 9–12 weeks | 3 (14) |
| 12–24 weeks | 1 (5) |
| 24–46 weeks | 5 (24) |
| Othere | 1 (5) |
| Formal curriculum | |
| Yes | 16 (76) |
| No | 5 (24) |
| Formal medical student rotation agreement | |
| Yes | 10 (48) |
| No | 11 (52) |
| Specific learning objectives | |
| Yes | 21 (100) |
| Activities students participate in | |
| Ambulatory clinical care | 20 (95) |
| Inpatient clinical care | 18 (86) |
| Research | 16 (76) |
| Preventive health care/health promotion | 18 (86) |
| Community outreach | 19 (90) |
| Supervision of lower-level students | 6 (29) |
| Quality improvement projects | 8 (38) |
| Health facility administrative meetings | 13 (62) |
| Laboratory activities | 15 (71) |
| Otherf | 5 (24) |
| Supervisor affiliation | |
| Health facility only | 5 (24) |
| Medical school only | 0 (0) |
| Health facility and medical school | 16 (76) |
For a complete list of participating schools, see List 1.
Midwifery, paramedic students, health auxiliaries, phlebotomy students, vaccination programs, nutritionists, occupational therapy (elective), physiotherapy (elective), allied health professionals, speech, clinical associates—electives and practicals, social work, lab, pharmaceutical technologists, radiographers, emergency medical technicians, nutrition, dental, pharmacy technicians, statistics, health system management, medical records, laboratory students, and nonspecific types.
Missing data for one site in Zambia.
For one Kilimanjaro Christian Medical College (KCMC) site: out-of-country students—3–6 months, KCMC students—2 months.
One site in Zimbabwe reported “greater part of the year as students are there at intervals.”
Pharmacy, antenatal care, delivery, assisting in operations (lumbar puncture and ascitic fluid tap), theater, coding patients, and registering patients.
Table 3.
Themes and Illustrative Quotations From Interviews with Key Informants at 21 Decentralized Clinical Training Sites From 11 Medical Education Partnership Initiative–Funded Schoolsa in Sub-Saharan Africa, 2015–2016
| Theme | Illustrative quotations (country) |
|---|---|
| Impact on health facility | “When they [students] were not coming, the community felt this hospital [would] fold up, but now their presence gives the community a better perspective of the hospital again.” (Nigeria) “Most government facilities are understaffed so when you receive these students they boost us and our productivity will be high.” (Uganda) “It has really been a challenge to us, a great one for that matter. Accommodation, mattresses, beds, lighting (electricity was not too good, we had to get a power-generating set for them), water storage containers like tanks are some of what is required. Yeah, it is important that we mention the issue of accommodation for them. It does not cost us much but it costs some time at least. Sometimes we may have to feed them, though we are quite happy to do that compared to what the students contribute.” (Nigeria) “They were challenges in the fact that certain basic tests were lacking. So you find that this does not provide a very comprehensive teaching. So through those feedbacks we have been able to improve the lab, actually, the lab is very much improved. Quite a number of tests that were not available we had to make sure that either the reagents are available or the equipment is bought or replaced.” (Kenya) “Because of the students we have been able to get a pathologist, we have been able to get an ophthalmologist, we have been able to get [an] extra gynecologist, [an] extra physician, and we are soon going to get an ENT surgeon.” (Kenya) “They ask so many questions on the round—for example, you prescribe a paracetamol to a patient, the students would like to know why you chose this paracetamol and not the other painkillers. Therefore you can see it is good on our part, to be challenged.” (Tanzania) “Their supervisors also help us in our work. There are cases—for example, urology—which are not done here much, but if they are around then services like surgery can be done. So that is another advantage we get from students.” (Tanzania) “And generally they follow up patients in the ward and that has had an impact on the outcome of the care to the children. So that has reduced the time spent in the ward, and it has also reduced the workload because there are more hands that can be used in service delivery now that they are here.” (Kenya) |
| Impact on staff | “The facility becomes a more academic facility. I have been to hospitals where that has been far behind, where I have felt I am not going anywhere in life. I am not learning anything new. But with students you are always learning something new, and you yourself feel that you have to equip yourself better all the time.” (South Africa) “Supervisors sharpen their knowledge and skills in preparation for effective supervision of students.” (Zimbabwe) “When the students are around, they are demanding, they have questions, they want answers, they want to be taught, they want to be shown bedside, you know, examinations and so on. So it puts people on their toes.” (South Africa) “The fact that there is discussion among them and there are also instructors that ask questions, stimulates me to read more and know about the services I am providing. I also listen to the discussions and interactions among students and their instructors, and I also learn from their discussions. All these contribute positively to my job satisfaction.” (Ethiopia) “I would say that it contributes a lot to my job satisfaction. I am happy, I enjoy teaching them and helping them to learn new things and to understand the principles and practice of community medicine.” (Nigeria) “Their job satisfaction is affected positively, as there is academic stimulation for all clinicians. They tend to refresh and update their clinical knowledge. They are also motivated to study so that they can effectively teach and guide students.” (Botswana) “There are times they come with ideas, sometimes they would tell us to say in (the university hospital) this is done in such a way. And then maybe the doctors will confirm and then we learn more from them. So I think it’s something both ways—we teach them a few things and we also learn from them and they also learn from here.” (Zambia) (“Personally it’s okay and I enjoy teaching because it keeps me updated and I add new knowledge through revising. Let me tell [you], before you teach these students you have to research and come when prepared.” (Uganda) |
| Impact on quality of care | “And if you look at the outcomes, particularly in obstetric care, we used to have more maternal deaths. I can tell you, previously we used to have tens of maternal deaths in one year. After that, with the program and many other things … we have reduced that to less than five in the last one year. So it is … the interplay of more than just the students but I can tell you that the student and the interaction from the university has really had a role in the whole … picture.” (Kenya) “We’ve identified there is a gap in the management of diarrhea. So they actually took up, they did a situation analysis on the care we do give all the way from the outpatient to the inpatient and they came up with recommendations on what we had need [for], such as the ORT corner in the outpatient [ward] … and actually assisted us to start an ORT corner in the ward.” (Kenya) “In terms of health services quality, as the students and their teachers are nearer to medical science compared to health center staff, they come with updated knowledge and skills in dealing with patients and in streamlining the services in the health center.” (Ethiopia) “And especially the home visit aspect.… Actually all our patients do have social issues contributing actually to these illnesses. Yeah, so that’s one aspect I felt the students really, really added. Because then when they do go looking into the social aspects, bringing them back to us, even [following] up [with] these patients post discharge, which we may not have done as thoroughly. Then we’ve been able to provide a more holistic care, you know, for those particular patients that they followed up [with].” (Kenya) |
| Impact on patients and communities | “There will be patients that are saying, no I don’t want to be seen by the students, I’d rather be seen by the doctor, which is totally fine, but it has not been the majority of the patients.” (South Africa) “To me it has improved because [the] ratio [of patients] to doctors reduces during this period when students are there. Reduction in waiting time positively affects quality of health care.” (Uganda) “They often do home visits for the patients and then they obviously spend more time with a patient than what we do. I think the patients appreciate this and I think also the home visits.” (South Africa) “Our community has benefited a lot from students especially during sensitizations carried out in the community. Sanitation, hygiene, and nutrition levels have improved in our community.” (Uganda) “In addition, during their community visits students bring services near to people and by doing so they encourage them to seek medical care. This [is] true and evident on the day when students visit the community, the following day you see more patients coming in to seek care.” (Uganda) “To me they positively benefit in reduction in waiting time, students go [the] extra mile to visit [patients] in their villages and give health talks to community members in general.” (Uganda) “Within the community health discipline, students undertake situational health diagnosis, which include[s] the study of the main pathologies existing in the health center, the causes, and the respective clinical history. They also analyze the main risk and vulnerability factors, against the community lifestyle, genetic aspects of the community members, administrative organization of the center and the national system of health, as well as the community environment.” (Mozambique) |
Abbreviations: ENT indicates otolaryngology; ORT, oral rehydration therapy.
For a complete list of participating schools, see List 1.
Students engaged in a spectrum of clinical services including ambulatory care, inpatient clinical care, and laboratory activities. The most common activity students participated in was ambulatory clinical care. Students in more than half of the sites engaged in facility administrative meetings, preventive health and health promotion activities, community outreach activities, and/or research. Students at 16 sites were supervised by both staff affiliated with the health facility and faculty from the medical school. Rotations ranged from 2 to 44 weeks (11 months), and the number of medical students attending a site at one time ranged from 1 to 50. Some rotations were established as early as the 1970s, while others were relatively new.
Impact on staff
A common theme reported was the positive impact students had on staff by providing clinical care, reducing workload, and motivating academic engagement. Many informants commented that they missed students when they were absent, especially where facilities were short-staffed. Students were described as extra helping hands and were valued by staff for taking thorough histories, facilitating ancillary services, and shortening patients’ waiting time. Two sites mentioned that students provided critical support in the maternity ward:
We are only 3 people handling over 40 expectant mothers during antenatal days. So our workload is heavy. When students come they help us and simplify our life (Uganda, urban site).
Another two indicated that students were helpful at triaging patients in the emergency room, with one saying:
Here we have a lot of cases of road traffic accidents. They are very helpful in triaging [when we delegate] roles to them like taking vital signs (Nigeria, peri-urban site).
Staff reported that students motivated them to reflect on clinical questions and influenced other cadres of providers either by facilitating teaching sessions or by inspiring them to read more. Most staff indicated that working with students stimulated them to improve their knowledge in advance of teaching, and informants described a sense of responsibility and desire to be a good example:
It’s always good to have students. You have an opportunity to teach them and you have [an] opportunity to learn from them as well. We must acknowledge that we learn from the student as well. It keeps you up-to-date. You want to be up-to-date so that when you are discussing with the student you are not seen like an outdated clinician (Botswana, urban site).
Staff reported increased motivation to engage in research and said that hosting students had increased research activity at their site. One staff member said,
We are reading more, researching more because you have the students coming and asking very difficult questions (Kenya, urban site).
At one site, students ran daily teaching sessions with the nurses. An informant at another site described how improving library facilities for medical students also meant that medical officers had better resources to address clinical questions.
Impact on health facilities
Students contributed to an improved work environment, staffing, and health facility reputation. Many staff reported that having students at their facility created a more dynamic and energized environment. Students created a greater pool of providers staffing the facility, and in some cases the need for adequate supervision allowed facilities to advocate successfully to governments for posting of additional specialists. One site reported,
Because of the students we have been able to get a pathologist …, an ophthalmologist, we have been able to get [an] extra gynecologist, [an] extra physician, and we are soon going to get an ENT surgeon (Kenya, urban site).
The transformation into a teaching facility also improved long-term recruitment, as students at some facilities returned for work after graduation. Several sites reported that being a training institution resulted in increased community utilization of services.
For clinical sites where specialists from the medical school provided supervision to students, visiting faculty often taught local staff and helped them to manage difficult cases. They participated directly in clinical care, providing consultations for patients who otherwise would have to travel some distance for specialist appointments. Staff from one site reported:
… Supervisors also help us in our work. There are cases—for example, urology—which are not done here much, but if they are around then services like surgery can be done (Tanzania, rural site).
Staff from one site indicated that visiting faculty even helped local staff by taking overnight call.
Respondents mentioned some challenges, mostly reflecting the need for resources to support students and their learning. Student welfare was a pressing issue at most sites, including provision of student accommodation, meals, and medical care. Interviewees reported higher rates of consumption of supplies such as gloves and masks. While some universities provided extra supplies for students, some sites ran out, and others requested more supplies from governments. In Botswana, staff reported:
When students are here, they use a lot of the consumables like gloves. They also use more of the aprons and gowns which will result in washing and laundry of these outfits (Botswana, urban site).
Consistent Internet access for students was a challenge because of poor connectivity or lack of electricity. Space for student learning was sometimes limited, which some sites addressed by sharing boardrooms for learning and administrative purposes.
Impact on quality of care
Informants reported that academic activities improved quality of care. They stated that when students asked questions about clinical cases or treatment plans, staff felt accountable and obligated to revisit their reference materials. One respondent from Zimbabwe said,
It affects the quality of care positively. Supervisors have to refresh, update, and [keep] on learning in order to supervise effectively (Zimbabwe, rural site).
Students also reportedly improved quality of care by presenting evidence-based approaches to clinical cases, conducting quality improvement activities, and stimulating locally relevant research. Many sites indicated that students’ quality improvement projects resulted in sustained changes to workflow, improved patients’ experiences, and increased efficiency of care. One site reported:
The number one advantage of having students is it creates a very conducive learning environment for both the students and the permanent staff. It has made an improvement in the quality of care.… It has challenged the hospital to embark on continuous improvement for the purpose of maintaining the standards (Kenya, urban site).
Another site in South Africa described how students mapped the flow of emergency room patients, posting a “visual for patients to understand the process.” In Ethiopia, one staff member shared that the
students and their teachers are nearer to medical science compared to health center staff, they come with updated knowledge and skills in dealing with patients and in streamlining the services in the health center (Ethiopia, rural site).
Many staff reported that students improved the thoroughness of care by taking extra time with patients, resulting in more detailed histories (especially social histories), leading to more accurate diagnoses or appropriate treatments. One provider described how he had a limited understanding of night shelters until his students followed up with a patient at a shelter and reported back to him that there were a number of medical resources and services that could be accessed.
Some sites reported improvements in health indicators. Respondents from one site where students rotated in obstetrics described how academic resources played a key role in reducing maternal mortality:
Previously we used to have tens of maternal deaths in one year. After that, with the program and many other things … we have reduced that to less than five in the last one year. So it is … the interplay of more than just the students but I can tell you that the student and the interaction from the university has really had a role in the whole … picture (Kenya, urban site).
Staff from another site, where students completed pediatric rotations, indicated that there were fewer deaths, transfers, and complaints from patients since students started coming, and that HIV testing rates at the facility rose from just over 60% to over 90% as a result of student research on HIV.
Impact on patients
Respondents perceived that students’ interactions with patients resulted in better experiences at the health facility. Several felt that patients considered students to be more compassionate and polite, and sometimes patients felt more comfortable talking with students than with facility staff. They noted students’ thorough history taking and physical examinations, observing that patients appreciated the increased attention. Two sites mentioned that when students were from that community, they became role models for other young people. At a few sites, however, respondents indicated some patients’ discomfort with students, preferring not to be seen by them. Staff from sites where large groups of students rotated together commented that patients were shy to be seen by such large groups and might not disclose all aspects of their history to them.
A somewhat mixed picture emerged regarding students’ impact on patient waiting time. Some respondents indicated that waiting times increased because of the time required to teach students, while others reported that waiting time decreased because students were able to start the history taking and examination before supervisors could attend to the patient. For example, in Zambia one respondent said,
I think it takes longer because the students … are learning and they need more of their time to make an assessment whereas the qualified staff, I think they have been through that routine and you know they are quick to see the patients and clear them on time (Zambia, urban site).
On the other hand, in Uganda one respondent gave a different perspective:
Patients are affected positively, they even love to see students around simply because they speed up the process of getting treatment. At least when they [are] around at every department/unit there is [a] health worker attending to patients (Uganda, rural site).
Impact on communities
Students often impacted communities through nonclinical activities, including health promotion, community health interventions, and home visits. Some students provided health education in the facility itself, while at other sites they did so in the community. One respondent described how students
offer health education and promotion talks to patients in the mornings before they are seen by the health care team (Botswana, urban site).
Another informant described student-created educational videos, which were played for patients while they waited to be seen. In the community, students participated in vaccination, deworming, community-based cervical cancer screening, or contact tracing for adults diagnosed with infectious diseases. Informants at one site described a comprehensive community outreach program, which included community diagnosis and medical services (consultations, investigations, treatment plans) provided free of charge by supervised students. At another, students participated as trainers at government-organized community health promotion meetings.
Staff from a number of sites noted that home visits by students were particularly valued by both staff at the facility and by patients. These visits involved health promotion and preventive care and were seen to be important in terms of assessment of patients in communities. One respondent from Kenya described how
All our patients do have social issues contributing actually to these illnesses … that’s one aspect I felt the students really, really added. Because then when they do go looking into the social aspects, bringing them back to us, even [following] up [with] these patients post discharge, which we may not have done as thoroughly. Then we’ve been able to provide a more holistic care (Kenya, urban site).
Discussion
The Lancet Commission that examined health professions education for the 21st century called for transforming education and the health systems, emphasizing the interdependence between these two domains.26 This study suggests that such interdependence can be mutually beneficial across multiple levels—for individuals (staff, students, patients), communities, and the health system within which they are situated, exemplifying the symbiotic model of medical education proposed by Worley.27 Across 21 sites in 10 countries, despite diverse health systems and training models, informants in this study saw students as a valuable resource. For staff at clinical sites, students reduced workload and extended facility services, rather than being a burden. Staff reported that students created livelier, engaging environments, bringing both academic rigor and hands-on support to facilities. Students seemed to transform the environment at the health facility, not just for those they directly work with but for all cadres of providers. Staff spoke positively about working with students despite the additional time required to supervise them, illustrating that nonfinancial incentives can contribute to job satisfaction. This supports prior evidence that establishing enabling environments can increase health worker satisfaction and perhaps retention even in rural and remote areas.28
It is difficult to link medical education directly with improvement in health outcomes, yet this study reveals several ways in which medical students appear to improve quality of care. Our findings support prior studies that suggest that medical students can change clinical supervisors’ practice by increasing inquiry and accountability, both of which are particularly relevant as health care increasingly relies on compliance with guidelines, checklists, and keeping up with evidence-based practice.22,29 These findings are especially relevant in low-resource settings where students can provide cost-effective improvements to quality of care.
What our study does not elucidate are the models of clinical training that are of best value to health facilities. Do longer rotations, more advanced students, or certain-sized facilities optimize student contribution? Convincing stakeholders (such as ministries of health or finance) to share the costs incurred and to provide adequate resources for training will likely require quantification of benefits and demonstration of measurable return on investment. Further research should consider how to optimize improvements to the health system while most efficiently using clinical resources, teaching time, and logistics.
As medical schools expand to meet Africa’s acute need for physicians, there are reports of crowding at tertiary health facilities, sometimes describing dozens of students around one patient bed. Expansion is forcing schools to look to nontertiary health facilities as student training sites. There are, of course, also strong pedagogical and philosophical reasons for decentralized training. However, training costs money, and commensurate additional financial resources are unlikely to be available to medical schools through traditional funding sources. Our study suggests a cost–benefit relationship that, while not quantified, can be qualitatively described. Education expenditures are typically considered long-term investments, but this study suggests that even in the short term, students add value to the health service environment. Linking investments in training programs to short-term improvements in health services provides a new narrative for academia to mobilize resources and bring new funders and stakeholders to the conversation of health workforce expansion.
Study limitations
Some methodological limitations should be considered when interpreting this study’s results. Conducting the study across 10 countries required engaging school representatives in multiple roles. While no TWG members were staff members at any of the sites, there may have been bias in site selection. Although all study team members were trained to conduct interviews, there may have been local variances in how the interviews were conducted and translated. Only four sites reported conducting the interviews in their local languages, but questions and responses from these interviews might have been affected during translation. Convenience sampling of both study sites and respondents may have introduced a selection bias favoring those sites that are more closely engaged with the medical school, and thus findings may not be generalizable to all such training sites. To curtail the researchers’ biases and to ensure credibility of the findings, a flexible yet rigorous analytical process was followed by using measures such as peer debriefing, prolonged immersion with content, triangulation of findings by interviewing three different persons at the same clinical site, and clarifying themes with all interviewers. Also, direct quotes from the interviews are included to present an undiluted narrative of the participants’ perspectives.
Conclusions
MEPI was a seminal investment in medical education, providing a unique opportunity to observe education models across the Sub-Saharan African region and to understand the impact of education on health systems. This study represents a capstone project of the MEPI community, which brought together investigators from 10 countries. It is, to our knowledge, the first multicountry study examining the value that undergraduate medical students bring to clinical health facilities and makes an important contribution to the medical education literature. As we strive to meet ambitious health workforce goals, this study suggests valuable synergies between health care delivery and education.
Students bring rigor, intellectual curiosity, and accountability to the health service setting; support overburdened staff by contributing to a more enabling and stimulating work environment; enhance the quality of the patient experience; and contribute to overall quality of care. As medical schools expand, especially in low-resource settings, mobilizing new and existing resources for decentralized clinical training could transform health facilities into vibrant service and learning environments.
Supplementary Material
Acknowledgments
The authors acknowledge the United States Government, the President’s Emergency Plan for AIDS Relief, the National Institutes of Health (NIH), the Health Resources and Services Administration (HRSA), George Washington University, the Africa Centre for Global Health and Social Transformation, and the schools that participated in this study. The authors wish to particularly acknowledge the principal investigators of the Medical Education Partnership Initiative (MEPI) grant who supported this study.
Funding/Support: Though there was no direct funding for this work, the team of authors came together through their work and association with MEPI. All the schools involved are recipients of MEPI funding. The Office of the U.S. Global AIDS Coordinator, the NIH, and HRSA funded MEPI but did not contribute to the work reported here.
Footnotes
Editor’s Note: This New Conversations contribution is part of the journal’s ongoing conversation on global health professions education—how ideas, experiences, approaches, and even resources can be shared across borders and across cultures to advance health professions education around the globe.
To read other New Conversations pieces and to contribute, browse the New Conversations collection on the journal’s Web site (http://journals.lww.com/academicmedicine/pages/collectiondetails.aspx?TopicalCollectionId=53), follow the discussion on AM Rounds (academicmedicineblog.org) and Twitter (@AcadMedJournal using #AcMedConversations), and submit manuscripts using the article type “New Conversations” (see Dr. Sklar’s and Dr. Weinstein’s May 2016 editorials for submission instructions and for more information about this feature).
Supplemental digital content for this article is available at http://links.lww.com/ACADMED/A492.
Other disclosures: None reported.
Ethical approval: This project was reviewed by the ethical review boards at all participating institutions. It received approval from the following bodies: Stellenbosch University Health Research Ethics Committee; University of Ibadan/University College Hospital Ethics’ Committee; Institutional Health Research Ethical Committee, Jos University Teaching Hospital; Joint Research Ethics Committee for the University of Zimbabwe College of Health Sciences and the Parirenyatwa Group of Hospitals; Makerere University College of Health Sciences School of Biomedical Sciences Research and Ethics Committee (also registered with Uganda National Council for Science and Technology and received permission from Kampala City Council); Health Research Development Committee, Health Research Unit, Ministry of Health and Wellness, and University of Botswana Institutional Review Board; Mahalapye District Hospital Ethics Committee; Letsholathebe Memorial Hospital Ethics Committee; the Eduardo Mondlane University Institutional Review Board; Jeremias–UEM COMISSÃO DE BIOÉTICA PÁRA SAÚDE; and the University of Kwazulu Natal Biomedical Research Ethics Committee. It received exemption from the following bodies: Office of Human Research–George Washington University and University of Zambia Biomedical Research Ethics Committee. This research was covered under the ethical approval granted for the larger MEPI project by the following bodies: College of Health Sciences, Addis Ababa University Institutional Review Board; Kenyatta National Hospital/University of Nairobi Ethics and Research Committee; and Kilimanjaro Christian Medical University Research Ethics and Review Committee.
Contributor Information
Zohray Talib, Associate professor of medicine and of health policy, George Washington University School of Medicine and Health Sciences, Washington, DC.
Susan van Schalkwyk, Professor of health professions education and director, Center for Health Professions Education, Faculty of Medicine and Health Sciences, Stellenbosch University, Stellenbosch, South Africa.
Ian Couper, Director, Ukwanda Center for Rural Health, Faculty of Medicine and Health Sciences, Stellenbosch University, Stellenbosch, South Africa.
Swaha Pattanaik, Doctoral student, Community Health Behavior and Education, Georgia Southern University, Statesboro, Georgia.
Khadija Turay, Senior research associate, Department of Health Policy, George Washington University, Washington, DC, at the time of this study.
Atiene S. Sagay, Professor of obstetrics and gynecology and honorary consultant obstetrician and gynecologist, University of Jos/Jos University Teaching Hospital, Jos, Nigeria.
Rhona Baingana, Lecturer, Department of Biochemistry, Makerere University, Kampala, Uganda.
Sarah Baird, Associate professor of global health and economics, Department of Global Health, George Washington University, Washington, DC.
Bernhard Gaede, Head, Department of Family Medicine, University of Kwazulu Natal, Durban, South Africa.
Jehu Iputo, Head, Department of Medical Education, Walter Sisulu University, Mthatha, Eastern Cape, South Africa.
Minnie Kibore, Pediatrician and public health specialist, University of Nairobi, Nairobi, Kenya.
Rachel Manongi, Senior lecturer, Department of Community Health, Kilimanjaro Christian Medical Center, Moshi, Tanzania.
Antony Matsika, Administrator, University of Zimbabwe College of Health Sciences-Novel Education Clinical Trainees & Researchers Program, Harare, Zimbabwe.
Mpho Mogodi, Lecturer, Department of Medical Education, Faculty of Medicine, University of Botswana, Gaborone, Botswana.
Jeremais Ramucesse, Assistant professor, Department of Community Health, Faculty of Medicine, Eduardo Mondlane University, and government advisor, Health Policies, Maputo, Mozambique.
Heather Ross, Senior proposal writer, IntraHealth International, and adjunct professor, Department of Global Health, George Washington University, Washington, DC.
Moses Simuyeba, Lecturer, School of Public Health, University of Zambia, Lusaka, Zambia.
Damen Haile-Mariam, Professor, School of Public Health, Addis Ababa University, Addis Ababa, Ethiopia.
References
- 1.World Health Organization. Global Strategy on Human Resources for Health: Workforce 2030. Geneva, Switzerland: World Health Organization; 2016. http://who.int/hrh/resources/globstrathrh-2030/en/. Accessed August 25, 2017. [Google Scholar]
- 2.Mullan F, Frehywot S, Omaswa F, et al. Medical schools in Sub-Saharan Africa. Lancet. 2011;377:1113–1121. doi: 10.1016/S0140-6736(10)61961-7. [DOI] [PubMed] [Google Scholar]
- 3.Talib ZM, Baingana RK, Sagay AS, Van Schalkwyk SC, Mehtsun S, Kiguli-Malwadde E. Investing in community-based education to improve the quality, quantity, and retention of physicians in three African countries. Educ Health (Abingdon) 2013;26:109–114. doi: 10.4103/1357-6283.120703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mariam DH, Sagay AS, Arubaku W, et al. Community-based education programs in Africa: Faculty experience within the Medical Education Partnership Initiative (MEPI) network. Acad Med. 2014;89(8 suppl):S50–S54. doi: 10.1097/ACM.0000000000000330. [DOI] [PubMed] [Google Scholar]
- 5.Birden HH, Wilson I. Rural placements are effective for teaching medicine in Australia: Evaluation of a cohort of students studying in rural placements. Rural Remote Health. 2012;12:2167. [PubMed] [Google Scholar]
- 6.Hirsh D, Walters L, Poncelet AN. Better learning, better doctors, better delivery system: Possibilities from a case study of longitudinal integrated clerkships. Med Teach. 2012;34:548–554. doi: 10.3109/0142159X.2012.696745. [DOI] [PubMed] [Google Scholar]
- 7.Couper ID, Worley PS. Meeting the challenges of training more medical students: Lessons from Flinders University’s distributed medical education program. Med J Aust. 2010;193:34–36. doi: 10.5694/j.1326-5377.2010.tb03738.x. [DOI] [PubMed] [Google Scholar]
- 8.Walters LK, Worley PS, Mugford BV. Parallel Rural Community Curriculum: Is it a transferable model? Rural Remote Health. 2003;3:236. [PubMed] [Google Scholar]
- 9.World Health Organization. Transforming and Scaling Up Health Professionals’ Education and Training. Geneva, Switzerland: World Health Organization; 2013. http://apps.who.int/iris/bitstream/10665/93635/1/9789241506502_eng.pdf. Accessed August 25, 2017. [Google Scholar]
- 10.Worley P, Prideaux D, Strasser R, Magarey A, March R. Empirical evidence for symbiotic medical education: A comparative analysis of community and tertiary-based programmes. Med Educ. 2006;40:109–116. doi: 10.1111/j.1365-2929.2005.02366.x. [DOI] [PubMed] [Google Scholar]
- 11.Couper I, Worley PS, Strasser R. Rural longitudinal integrated clerkships: Lessons from two programs on different continents. Rural Remote Health. 2011;11:1665. [PubMed] [Google Scholar]
- 12.Van Schalkwyk SC, Bezuidenhout J, De Villiers MR. Understanding rural clinical learning spaces: Being and becoming a doctor. Med Teach. 2015;37:589–594. doi: 10.3109/0142159X.2014.956064. [DOI] [PubMed] [Google Scholar]
- 13.Worley P, Couper I, Strasser R, et al. Consortium of Longitudinal Integrated Clerkships (CLIC) Research Collaborative. A typology of longitudinal integrated clerkships. Med Educ. 2016;50:922–932. doi: 10.1111/medu.13084. [DOI] [PubMed] [Google Scholar]
- 14.Blitz J, Bezuidenhout J, Conradie H, de Villiers M, van Schalkwyk S. “I felt colonised”: Emerging clinical teachers on a new rural teaching platform. Rural Remote Health. 2014;14:2511. [PubMed] [Google Scholar]
- 15.Van Schalkwyk SC, Bezuidenhout J, Conradie HH, et al. “Going rural”: Driving change through a rural medical education innovation. Rural Remote Health. 2014;14:2493. [PubMed] [Google Scholar]
- 16.Mullan F, Frehywot S, Omaswa F, et al. The Medical Education Partnership Initiative: PEPFAR’s effort to boost health worker education to strengthen health systems. Health Aff (Millwood) 2012;31:1561–1572. doi: 10.1377/hlthaff.2012.0219. [DOI] [PubMed] [Google Scholar]
- 17.Sullivan GM, Sargeant J. Qualities of qualitative research: Part I. J Grad Med Educ. 2011;3:449–452. doi: 10.4300/JGME-D-11-00221.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smucny J, Beatty P, Grant W, Dennison T, Wolff LT. An evaluation of the Rural Medical Education Program of the State University of New York Upstate Medical University, 1990–2003. Acad Med. 2005;80:733–738. doi: 10.1097/00001888-200508000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Daly M, Perkins D, Kumar K, Roberts C, Moore M. What factors in rural and remote extended clinical placements may contribute to preparedness for practice from the perspective of students and clinicians? Med Teach. 2013;35:900–907. doi: 10.3109/0142159X.2013.820274. [DOI] [PubMed] [Google Scholar]
- 20.McGaghie WC, Bordage G, Shea JA. Problem statement, conceptual framework, and research question. Acad Med. 2001;76:923–924. [Google Scholar]
- 21.Ringsted C, Hodges B, Scherpbier A. “The research compass”: An introduction to research in medical education: AMEE guide no. 56. Med Teach. 2011;33:695–709. doi: 10.3109/0142159X.2011.595436. [DOI] [PubMed] [Google Scholar]
- 22.Atuyambe LM, Baingana RK, Kibira SP, et al. Undergraduate students’ contributions to health service delivery through community-based education: A qualitative study by the MESAU Consortium in Uganda. BMC Med Educ. 2016;16:123. doi: 10.1186/s12909-016-0626-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Merriam-Webster. Peri-urban. https://www.merriam-webster.com/dictionary/peri–urban. Accessed August 25, 2017.
- 24.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 25.Hennink MM, Kaiser BN, Marconi VC. Code saturation versus meaning saturation: How many interviews are enough? Qual Health Res. 2017;27:591–608. doi: 10.1177/1049732316665344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376:1923–1958. doi: 10.1016/S0140-6736(10)61854-5. [DOI] [PubMed] [Google Scholar]
- 27.Worley P. Relationships: A new way to analyse community-based medical education? (Part one) Educ Health (Abingdon) 2002;15:117–128. doi: 10.1080/13576280210133062. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization. Global Policy Recommendations. Geneva, Switzerland: World Health Organization; 2010. Increasing Access to Health Workers in Remote and Rural Areas Through Improved Retention. http://apps.who.int/iris/bitstream/10665/44369/1/9789241564014_eng.pdf. Accessed August 25, 2017. [PubMed] [Google Scholar]
- 29.Kamien M. Can first-year medical students contribute to better care for patients with a chronic disease? Med Educ. 1990;24:23–26. doi: 10.1111/j.1365-2923.1990.tb02432.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


