Abstract
Objective
To explore the effect of 3-dimensional (3D) printing-assisted cognitive fusion on improvement of the positive rate in prostate biopsy.
Methods
From August to December 2014, 16 patients with suspected prostatic lesions detected by multiparametric magnetic resonance imaging (MRI) were included. Targeted prostate biopsy was performed with the use of prostate 3D reconstruction modeling, computer-simulated biopsy, 3D printing, and cognitive fusion biopsy. All patients had received 3.0 T multiparametric MRI before biopsy. The DICOM MRI files were imported to medical imaging processing software for 3D reconstruction modeling to generate a printable .stl file for 3D printing with use of transparent resin as raw material. We further performed a targeted 2- to 3-core biopsy at suspected lesions spotted on MRI.
Results
For the 16 patients in the present study, 3D modeling with cognitive fusion-based targeted biopsy was successfully performed. For a single patient, 1–2 lesions (average: 1.1 lesions) were discovered, followed by 2–6 cores (average: 2.4 cores) added as targeted biopsy. Systematic biopsies accounted for 192 cores in total, with a positive rate of 22.4%; targeted biopsies accounted for 39 cores in total, with a positive rate of 46.2%. Among these cases, 10 patients (62.5%) were diagnosed with prostate adenocarcinoma, in which seven were discovered by both systematic and targeted biopsy, one was diagnosed by systematic biopsy only, and two were diagnosed by targeted biopsy only. For systematic biopsy, Gleason score ranged from 6 to 8 (average: 7), while that for targeted biopsy ranged from 6 to 9 (average: 7.67). Among the seven patients that were diagnosed by both systematic and targeted biopsy, three (42.8%) were reported with a higher Gleason score in targeted therapy than in systematic biopsy.
Conclusion
3D printing-assisted cognitive fusion technique markedly promoted positive rate in prostate biopsy, and reduced missed detection in high-risk prostate cancer.
Keywords: Prostate cancer, Prostate biopsy, 3D printing
1. Introduction
Transrectal ultrasound (TRUS) guided prostate biopsy is the first choice in the diagnosis of prostate cancer [1]. However, the traditional method has difficulty in avoiding missed diagnosis, for as high as 22%–47% of prostate cancer are missed in the initial biopsy [2]. The standard TRUS guided prostate biopsy is mainly for sampling in the peripheral zone where the incidence of cancer is high, but this conventional approach is poor in sampling cancers at the anterior, midline, and apex of the prostate, leading to underdiagnosis of clinically significant diseases [3]. Magnetic resonance imaging (MRI) has higher sensitivity in finding clinically significant prostate cancer [4]. Functional MRI technique as dynamic contrast-enhancement (DCE) and diffusion weighted imaging (DWI) may provide more accurate space orientation on the basis of qualitative diagnosis. It has now become an important problem regarding the use of image positioning to guide prostate biopsy so as to effectively improve the biopsy positive rate in the early diagnosis of prostate cancer. MRI-TRUS fusion targeted biopsy and MRI-guided targeted biopsy are effective approaches to improve biopsy positive rate and avoid missed diagnosis of prostate cancer [5], [6], but both have higher requirement for hardware facilities, and need complicated skills in operation; therefore, it is rather difficult to apply these methods in conventional examination.
Currently, 3-dimensional (3D) printing technique is fast developing and has infiltrated into multiple industries including healthcare industry. Now its application in medical field is mainly in implant design, surgery simulation, skill training and others. There has not been much report from urinary surgery in this regard. This study explores 3D printing technique assisting cognitive fusion for design of prostate biopsy regimen, and evaluates its feasibility and efficacy in improvement of positive rate of prostate biopsy.
2. Patients and methods
2.1. Patients
This prospective study was conducted in the Changhai Hospital Affiliated to Second Military Medical University (Shanghai, China). The code of ethics was reviewed by the Institutional Review Board of Changhai Hospital and approval was obtained. Informed consents were obtained from patients eligible for this study, and any potential harms and benefits regarding to the study were elaborated. Study enrollment began in 2014.
2.2. Multi-parameter MRI examination
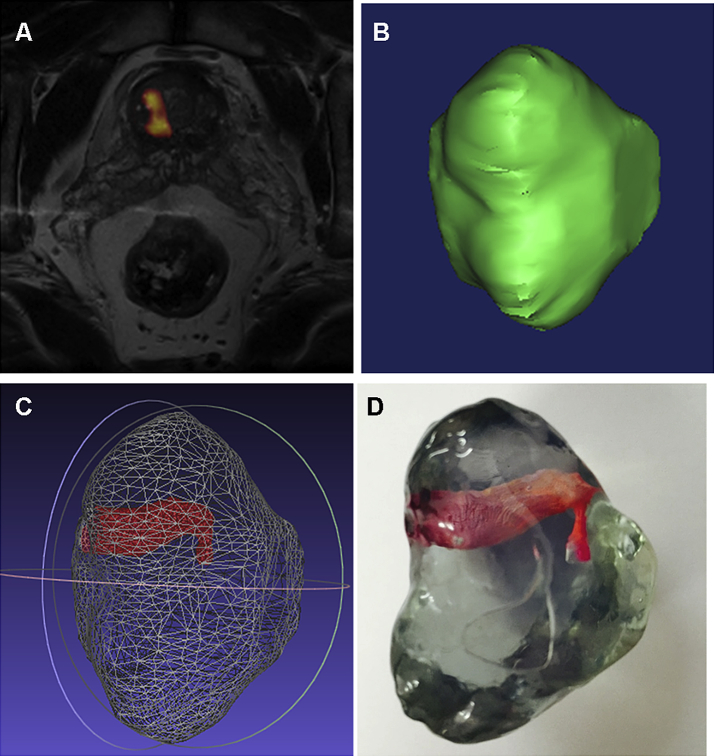
All patients had received 3.0 T multiparametric MRI (Siemens Magnetom Skyra, Germany) before biopsy. The scan sequence included T1 weighted, T2 weighted, DCE and DWI. Two radiologists identified and located lesions suspicious for cancer according to the MRI sequences (Fig. 1A). Both radiologists were blinded to pre-imaging serum prostate specific antigen (PSA) values and digital rectal examination (DRE) status.
Figure 1.
Prostate 3-dimensional (3D) model building and its printing based on multi-parametric magnetic resonance imaging (MRI). The patient was male, PSA 16.2 ng/mL, with history of one prior negative biopsy. (A) Comparison of T2 weighted image with dynamic condition for enhancement of image fusion, displaying the tumor location with an abnormal signal in the right side of the central lobe of the prostate; (B) MRI data introduced into medical image processing platform for 3D model building; (C) The .stl format file introduced into the software, indicating the special location of the tumor; (D) Transparent resin material used for 3D printing model, the spatial structure of the tumor shown by staining in later phase.
2.3. 3D reconstruction and 3D printing
Digital Imaging and Communications in Medicine (DICOM) format file of MRI was introduced into medical image processing software accordingly. Prostate and tumor images were introduced for 3D model reconstruction and smoothly processed to generate printable .stl format files (Fig. 1B,C). By means of SLA, RS-450, 3D printer, the .stl files were printed in accordance with a thickness of 0.1 mm. The printing material was transparent resin (Fig. 1D).
2.4. Systematic prostate biopsy
All patients received 12-core systematic prostate biopsy under TRUS guidance. The 12-core biopsy was performed on the basis of the traditional 6-core biopsy by adding three cores on both sides of the lateral peripheral zones.
2.5. Targeted biopsy under 3D printing assisted cognitive fusion
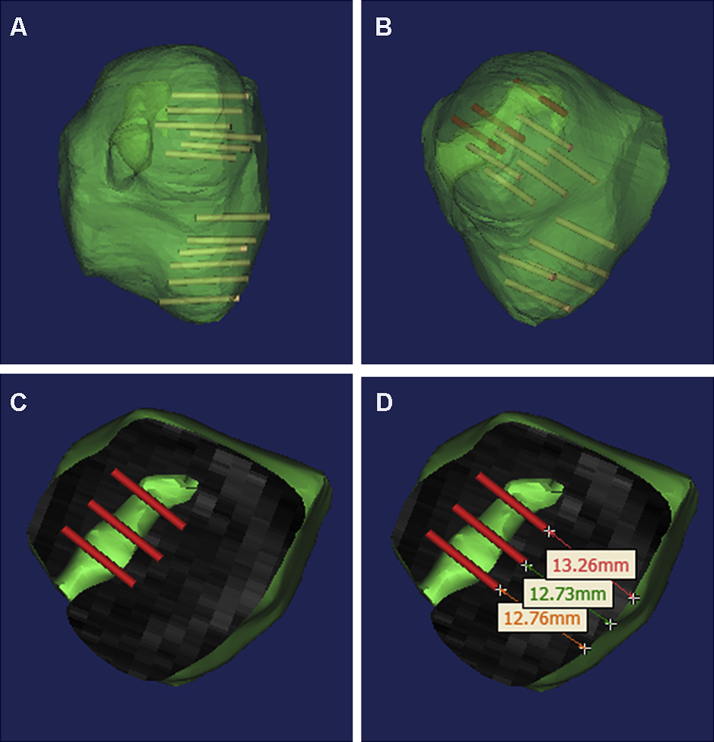
The suspected lesions found by multi-parametric MRI further underwent a targeted 2–3-core biopsy. Before biopsy, the location of the suspected focus in the prostate was determined according to the 3D reconstruction data, followed by computer simulation 12-needle systematic biopsy performed (Fig. 2A) to estimate whether the suspected focus could be detected in the course of biopsy. If the suspected focus was in the anterior, midline, and apex, because of the limitations of biopsy angle or biopsy depth, systematic biopsy might not be able to take samples. Then computer simulation of targeted biopsy procedures (Fig. 2B) should be done to select biopsy sections, needling angles and needling depth at triggering.
Figure 2.
Computer simulated prostate system and targeted biopsy. (A) Computer simulated transrectal 12-needle systematic biopsy, showing that the conventional biopsy scheme is unable to sample in the suspected area; (B) Computer simulated targeted biopsy on suspected area; (C) Selecting the sagittal plane on the right side of the central lobe as biopsy plane; (D) The biopsy needle penetrated through the prostate envelope for 12–14 mm, followed by triggering and sampling in the suspected area.
3. Results
From August to December, 2014, 16 patients (median age 64 years) successfully underwent 3D modeling with cognitive fusion-based targeted biopsy. Patient and biopsy characteristics are described in Table 1. Median PSA at biopsy was 14.95 ng/mL (range 1.11–33.35 ng/mL), and 14 of 16 (87.5%) patients had a negative DRE.
Table 1.
Patient demographics.
| Indice | Median | Range |
|---|---|---|
| Age (year) | 64 | 53–82 |
| PSA (ng/mL) | 14.95 | 1.11–33.35 |
| Prostate volume (mL) | 39 | 22–89 |
| PSA density (ng/mL2) | 0.373 | 0.028–0.744 |
| Lesions of suspicion on MRI | 1 | 1–2 |
| Targeted biopsy cores | 2 | 2–6 |
PSA, prostate specific antigen; MRI, magnetic resonance imaging.
For a single patient, one to two lesions (average: 1.1 lesions) were discovered, followed by 2–6 cores (average: 2.4 cores) added as targeted biopsy. Eight patients had suspected lesions in the peripheral zone, and the remaining eight had lesions in atypical zones such as the prostate apex and central gland. Systematic biopsies accounted for 192 cores in total, with a positive rate of 22.4%; targeted biopsies accounted for 39 cores in total, with a positive rate of 46.2%. No patient required hospitalization for fever or sepsis after biopsy.
Of the 16 patients, 10 patients (62.5%) were diagnosed with prostate adenocarcinoma (Table 2), in which seven were discovered by both systematic and targeted biopsy, one was diagnosed by systematic biopsy only, and two were diagnosed by targeted biopsy only. For systematic biopsy, Gleason score ranged from 6 to 8 (average: 7), while that for targeted biopsy ranged from 6 to 9 (average: 7.67).
Table 2.
Prostate cancer grades found by systematic and targeted biopsies.
| Method | Low grade (GS ≤ 6) | Intermediate grade (GS = 7) | High grade (GS 8–10) | Total (n) |
|---|---|---|---|---|
| Systematic biopsy | 2 | 4 | 2 | 8 |
| Targeted biopsy | 1 | 4 | 4 | 9 |
GS, Gleason score.
Among the seven patients that were diagnosed by both systematic and targeted biopsy, three (42.9%) were reported with a higher Gleason score in targeted therapy than in systematic biopsy.
4. Discussion
How to effectively avoid false negative results in biopsy is an important problem in the early diagnosis of prostate cancer. The development of MRI techniques provides more and more accurate localization diagnosis on the basis of its qualitative diagnosis. With rational use of imaging localization information, performing targeted biopsy on suspected cancer foci is an effective method to improve the positive rate of diagnosis. At present, fusion technique based on MRI-identified foci includes MRI/TRUS fusion, MRI/MRI fusion and cognitive fusion. Sonn et al. [5] utilized Artemis device to perform biopsy on 105 cases, in which PSA continued to rise after initial negative biopsy. By performing subsequent targeted biopsy with MRI/TRUS fusion on these cases, the positive rate was 34%. Of the positive targeted biopsy cases, 91% were of clinical significance (Gleason score ≥7), and that of systematic biopsy was 54%. Hoeks et al. [6] performed MR-guided biopsy on patients with elevated PSA and one or more previous negative TRUS biopsy sessions. In a total of 117 patients, cancer detection rate was 41%, and the majority of detected cancers were clinically significant (87%). The two methods are both able to improve the positive rate and avoid missed diagnosis of cancer in prostate biopsy, but requirements for image fusion device are high, which was inconvenient to operate, hence is not conducive to extended promotion on large scale.
In cognitive fusion, the operator selects suspected regions by reading the MRI image and then performing biopsy under TRUS guidance. Its efficacy is still in controversy. Puech et al. [7] believed that the result of targeted biopsy in terms of cognitive fusion is not obviously different from that of systematic biopsy in terms of MRI/TRUS fusion; Delongchamps et al. [8] thought that targeted biopsy by cognitive fusion did not have obvious advantage over systematic biopsy (p = 0.66). Cognitive fusion depends greatly on the operator's experience, which is easy and simple to handle but without accurate methods. Its efficacy and repeatability is relatively poor. Therefore, to improve cognitive fusion method and raise its efficacy in prostate biopsy is of high importance for the improvement of biopsy positive rate and avoidance of missed diagnosis of high-risk prostate cancer.
3D printing technique performs accurate modeling in terms of multi-parameter MRI localization diagnostic information that makes use of computer software simulated biopsy and objectively evaluates systematic biopsy capability in the diagnosis of the suspected areas. In conventional systematic biopsy, the needle is triggered the moment it touches the prostatic capsule. If the tumor is located at the tip of the prostate or close to the urethra or at other atypical areas, conventional systematic biopsy may have difficulty in sampling these suspected areas; therefore, an individualized biopsy plan can be worked out in terms of computer simulated needling angles and depths. For the patients in the present study, 3D print assisting cognitive fusion targeted biopsy avoided the missed diagnosis of two cases (20%), effectively improving the biopsy positive rate. Besides, of the seven patients found with cancer by both system and target biopsies, three (42.9%) were with higher points of Gleason score by targeted biopsy than by systematic biopsy; high-risk prostate cancer was effectively found. Two patients in this group were found with cancer only by targeted biopsy; both had a history of one prior negative prostate biopsy, multi-parametric MRI found suspected lesions in transition zone, thus it is clear that this technique is of marked significance in the diagnosis of cancer in non-peripheral zones.
3D printing technique can accurately reproduce 3D image, and application of transparent resin material can intuitively show the location, size and morphology of the tumor. Before biopsy, the operator can observe the 3D model of the tumor from multiple angles, thus evaluating the possibility of sampling by systematic biopsy. If the suspected focus is located in the peripheral zone, sampling can be done by systematic biopsy, for which the corresponding needle position for transrectal 12-needle systematic biopsy would be determined. In cases of non-peripheral zone and larger-sized cancers, it is impossible for the biopsy needle to sample in the suspected area that triggers the moment it touches the envelope of the prostate. The needing depth can thus be adjusted so as to break through the envelope and get close to the suspected area prior to triggering. Each suspected area can be further determined with 2–3 biopsies to avoid tumor omissions. In this study, the single needle positive rate for targeted biopsy was 46.2%, which was markedly higher than the 22.4% one for systematic biopsy.
The application of 3D printing technique effectively improves the efficacy of cognitive fusion, and avoids the drawback of depending too much on the operator's experience. It is of certain accuracy and repeatability, but there is still much room to be desired in this approach. Firstly, the prostate is a soft tissue organ, so MRI data image processing is more difficult than that for bone, teeth and other tissues. In the data modeling phase, adequate acknowledgment of pelvic anatomy is very much required. With the assistance of the image practitioner, only by being clear of the suspected area in MRI image, can one perform relatively accurate modeling of the prostate and the suspected focus. Secondly, prostate cancer is likely to be characterized by multiple foci, so multi-parametric MRI cannot find small-sized foci. Therefore, based on various fusions of multi-parametric MRI, targeted biopsy cannot take place of systematic biopsy completely. Development of targeted biopsy relies on advances in more sensitive and specific imaging technologies.
Currently, 3D printing technique is fast developing and integrating in multiple industries including healthcare industry. Its major application in the medical field is now involved in implant design, surgery simulation, training and others [9], [10]. There have been just a few 3D print applications in the urology field. Zhang et al. [11] reported research on 3D printing technique applied in the planning of renal tumor surgery and believed that it was of great significance for doctor's surgery planning and doctor-patient communication. With its development and the advent of new materials, this technology will surely be applied more extensively in the urology surgery field.
5. Conclusion
The development of new technologies and their cross-fusion with multi-discipline is an important driving force for medical development. In this study, we applied 3D printing technique assisting cognitive fusion in the early diagnosis of prostate cancer, which markedly improved the positive rate of biopsy and avoided missed diagnosis of high-risk prostate cancer. This technical operation proves to be easy and simple. The increased number of needling in targeted biopsy does not increase the incidence of complication. Its application and popularization will surely benefit more patients on a larger scale in the future.
Conflicts of interest
The authors declare no conflict of interest.
Footnotes
Peer review under responsibility of Shanghai Medical Association and SMMU.
References
- 1.Hodge K.K., McNeal J.E., Terris M.K., Stamey T.A. Random systematic versus directed ultrasound guided transrectal core biopsies of the prostate. J Urol. 1989;142:71–75. doi: 10.1016/s0022-5347(17)38664-0. [DOI] [PubMed] [Google Scholar]
- 2.Taira A.V., Merrick G.S., Galbreath R.W., Andreini H., Taubenslag W., Curtis R. Performance of transperineal template-guided mapping biopsy in detecting prostate cancer in the initial and repeat biopsy setting. Prostate Cancer Prostatic Dis. 2010;13:71–77. doi: 10.1038/pcan.2009.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moore C.M., Robertson N.L., Arsanious N., Middleton T., Villers A., Klotz L. Image-guided prostate biopsy using magnetic resonance imaging-derived targets: a systematic review. Eur Urol. 2013;63:125–140. doi: 10.1016/j.eururo.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 4.Puech P., Potiron E., Lemaitre L., Leroy X., Haber G.P., Crouzet S. Dynamic contrast-enhanced-magnetic resonance imaging evaluation of intraprostatic prostate cancer: correlation with radical prostatectomy specimens. Urology. 2009;74:1094–1099. doi: 10.1016/j.urology.2009.04.102. [DOI] [PubMed] [Google Scholar]
- 5.Sonn G.A., Chang E., Natarajan S., Margolis D.J., Macairan M., Lieu P. Value of targeted prostate biopsy using magnetic resonance-ultrasound fusion in men with prior negative biopsy and elevated prostate-specific antigen. Eur Urol. 2014;65:809–815. doi: 10.1016/j.eururo.2013.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoeks C.M., Schouten M.G., Bomers J.G., Hoogendoorn S.P., Hulsbergen-van de Kaa C.A., Hambrock T. Three-Tesla magnetic resonance-guided prostate biopsy in men with increased prostate-specific antigen and repeated, negative, random, systematic, transrectal ultrasound biopsies: detection of clinically significant prostate cancers. Eur Urol. 2012;62:902–909. doi: 10.1016/j.eururo.2012.01.047. [DOI] [PubMed] [Google Scholar]
- 7.Puech P., Rouviere O., Renard-Penna R., Villers A., Devos P., Colombel M. Prostate cancer diagnosis: multiparametric MR-targeted biopsy with cognitive and transrectal US-MR fusion guidance versus systematic biopsy–prospective multicenter study. Radiology. 2013;268:461–469. doi: 10.1148/radiol.13121501. [DOI] [PubMed] [Google Scholar]
- 8.Delongchamps N.B., Peyromaure M., Schull A., Beuvon F., Bouazza N., Flam T. Prebiopsy magnetic resonance imaging and prostate cancer detection: comparison of random and targeted biopsies. J Urol. 2013;189:493–499. doi: 10.1016/j.juro.2012.08.195. [DOI] [PubMed] [Google Scholar]
- 9.Cousley R.R., Turner M.J. Digital model planning and computerized fabrication of orthognathic surgery wafers. J Orthod. 2014;41:38–45. doi: 10.1179/1465313313Y.0000000075. [DOI] [PubMed] [Google Scholar]
- 10.Rohner D., Guijarro-Martinez R., Bucher P., Hammer B. Importance of patient-specific intraoperative guides in complex maxillofacial reconstruction. J Craniomaxillofac Surg. 2013;41:382–390. doi: 10.1016/j.jcms.2012.10.021. [DOI] [PubMed] [Google Scholar]
- 11.Zhang Y., Ge H.W., Li N.C., Yu C.F., Guo H.F., Jin S.H. Evaluation of three-dimensional printing for laparoscopic partial nephrectomy of renal tumors: a preliminary report. World J Urol. 2015 Apr 5 doi: 10.1007/s00345-015-1530-7. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]