Abstract
The last 20 years have produced developments in the treatment for patients with non-obstructive azoospermia (NOA) who were once considered to be infertile. The combination of intracytoplasmic sperm injection together with various testicular sperm retrieval techniques, including conventional testicular sperm extraction (TESE), microdissection TESE (micro-TESE) and fine needle aspiration (FNA), have revolutionized treatment for these men. In men with NOA, isolated regions of spermatogenesis within the testis are common. The goal for all types of sperm retrieval procedures is locating the focal region(s) of spermatogenesis, and harvesting the sperm for assisted reproduction. This review article explores the surgical management of men with NOA and describes all techniques that can be used for testicular sperm retrieval. A PubMed search was conducted using the key words: “sperm extraction”, “NOA”, “testicular FNA”, “testicular mapping”, “TESE”, and “testicular biopsy”. All articles were reviewed. Articles were included if they provided data on sperm retrieval rates. The methods for performing sperm retrieval rates and outcomes of the various techniques are outlined. Micro-TESE has a higher sperm retrieval rates with fewer postoperative complications and negative effects on testicular function compared with conventional TESE.
Keywords: Non-obstructive azoospermia, Microdissection testicular sperm extraction, Fine needle aspiration, Sperm retrieval
1. Introduction
Approximately 10% of infertile men have non-obstructive azoospermia (NOA) and 60% of azoospermic men are diagnosed with NOA [1]. Dramatic advances in the last 20 years have been made in treatment options of NOA. In the past, the only options for treating men with NOA were donor insemination or adoption. The theoretical basis for attempting to retrieve spermatozoa from the testes in men with azoospermia is based on early histological studies that noted spermatids in infertile men [2]. The testes of infertile men have a mixed histological pattern of focal areas of complete spermatogenic development in a background of germinal cell aplasia [3]. The development of intracytoplasmic sperm injection (ICSI) paired with the practicality of retrieving viable sperm from the testes of NOA patients led to the development of fertility treatments for these patients [4].
There are several etiologies for testicular failure that leads to NOA, including genetic disorders (e.g., sex chromosome abnormalities, translocations or Y chromosome microdeletions), cryptorchidism, radiation and/or gonadal toxins. Despite the different causes for testicular failure, the goal for sperm retrieval is always finding the focal area of spermatogenesis. There are several approaches for sperm retrieval including fine needle aspiration (FNA), percutaneous testicular biopsy, open testicular biopsy (testicular sperm extraction (TESE), which includes multiple TESE), and microdissection TESE (micro-TESE). This review article will describe the technical aspects of testicular sperm retrieval and highlight the sperm retrieval rates (SRR) and outcomes of these procedures.
2. Evidence acquisition
A PubMed search was conducted on February 15 2014 using key words: “sperm extraction”, “non-obstructive azoospermia”, “testicular fine needle aspiration”, “testicular mapping”, “testicular sperm extraction”, “testicular biopsy”. English language articles were reviewed for inclusion. Articles were included if they provided data on SRR.
3. Evidence synthesis
3.1. Indication for surgery
In azoospermia, sperm retrieval is possible through both open and percutaneous surgical approaches. In obstructive azoospermia, sperm is usually harvested from the epididymis. Testicular sperm extraction is reserved for when epididymal sperm extraction fails, and it is the only option for sperm retrieval in men with NOA.
3.2. Preoperative preparation
To confirm the diagnosis of azoospermia, the semen sample should be centrifuged and the pellet should be examined under the microscope, up to 35% of men who were diagnosed with NOA may in fact have sperm in the ejaculate [5]. A thorough history and physical examination should be performed on all men with NOA. In addition, hormonal evaluation and genetic testing should be offered, specifically karyotype analysis and Y microdeletion. On physical examination, men with NOA have small testes and flat non-indurated epididymides. On hormonal testing, elevated follicle stimulating hormone (FSH) greater than 7.0 mIU/mL is common and variable levels of serum testosterone (T) are seen. The etiology of NOA will be elucidated in up to 17% of men with genetic testing [6]. Genetic testing also provides prognostic information for counseling patients about their prognosis and the possibility of passing a genetic defect to their offspring if they proceed with in vitro fertilization. For instance, men with the AZFc deletion or Klinefelter's Syndrome have good prognosis. Men with complete AZFa or AZFb have little to no chance of sperm retrieval [7]. Men with AZFc deletion should be counseled about passing on the genetic defect to their offspring.
3.3. Prior to surgical intervention
Optimization of spermatogenesis prior to sperm retrieval should be attempted in couples where the female age permits. Simple changes in life style habits such as smoking cessation is advised for the male partner might improve their fertility potential. Medical treatment is effective and recommended for men with hypogonadotropic hypogonadism; therefore, it will often obviate the need for sperm retrieval surgery.
Hormonal manipulation has a role in increasing endogenous production of testosterone and normalizing the testosterone/estrogen ratio in men with clear hypogonadism. Hormonal therapy includes clomiphene citrate, aromatase inhibitors, and human chorionic gonadotropin [8]. Klinefelter's Syndrome patients with a low serum T, which increases to greater than 250 ng/dL with medical therapy, have a higher SRR with micro-TESE [9]. Selective estrogen receptors modulators (SERMs) have been shown to be associated with improving sperm production in men with NOA; however, well-designed trials demonstrating its benefit are lacking [10]. Men with NOA and testicular histology showing hypospermatogenesis [11], men who failed initial micro-TESE but before a repeat micro-TESE [12], might benefit from a trial of gonadotropins. Additionally, patients diagnosed with NOA and hypospermatogenesis on histologic examination and received gonadotropins have better SRR even when selective estrogen receptors modulators therapy fails to raise testosterone [13]. Patients with NOA may benefit from clomiphene with normal T.
In a study by Pavlovich et al. [14] men with severe male infertility were characterized as having a T to estradiol (E) ratio of 6.9, whereas men with normal spermatogenesis had a mean T/E ratio of 14.5. Therefore, 10, is proposed as the lower limit of normal T/E ratios in men. Clinical studies of aromatase inhibitors have focused on men with defective spermatogenesis associated with low serum T levels and abnormal T/E ratios. Most of the studies focused on men who had abnormal T/E ratio and it is difficult to draw any conclusion on the use of aromatase inhibitors in men with normal ratio.
The benefit of varicocelectomy in NOA prior to sperm retrieval is limited. Varicocelectomy in patients with NOA resulted in less than 10% that had adequate sperm in the ejaculate obviating the need for subsequent TESE [15]. A single diagnostic biopsy provides a very limited evaluation of the testicle and does not predict SRR because of known heterogeneity of spermatogenic patterns in NOA. Therefore, negative biopsies should be interpreted with caution and patients with NOA may need repeat surgical sperm retrieval [16].
3.4. Percutaneous sperm retrieval
Percutaneous testicular aspiration or biopsy can be performed in the office under local anesthesia, which is less invasive than an open surgical procedure and is most useful for men with obstructive azoospermia. Complications of percutaneous testicular aspiration include intratesticular bleeding and scar tissue. Needle aspiration and biopsy are effective in providing quality sperm for in vitro fertilization/ICSI in men with obstructive azoospermia [17].
3.4.1. FNA
FNA is a blind needle insertion through scrotal skin into the testicle, ideally under local anesthesia in an office setting. There are technical variations in the needle caliber and number of samples taken with the goal of minimizing complications and optimizing SRR.
FNA is begun by preparing and draping the skin with non-betadine solution. A cord block is performed by injecting 10 mL of local anesthesia into the spermatic cord, the region of the vas and the scrotal skin where the biopsy needle will pass with a 25-gauge needle. The testis is held securely maintaining constant fixed position relative to the scrotal skin. To perform an FNA, percutaneously puncture the testicular parenchyma with aspiration of tissue and fluid using a fine needle, for example a 23 gauge needle. Pull the syringe plunger to create negative pressure while moving the tip of the needle in and out of the testis; the stroke size is approximately 8–10 mm in an oblique plane, thereby, disrupting the seminiferous tubules and sampling different testicular areas. Maintain suction while the needle is withdrawn to remove small segments of seminiferous tubules. Expel the tissue fragments by flushing the needle with sperm wash medium. The sample is sent to the andrology lab, and a sample is assessed by Papanicolaou stain.
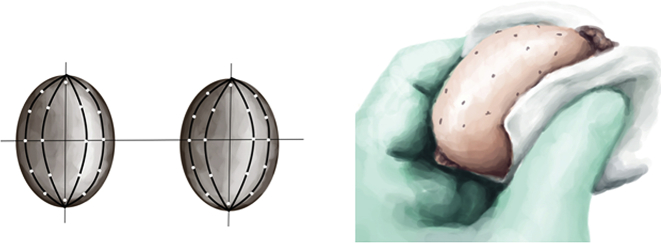
FNA was first described by Obrant et al. [18] in 1965 in the human testis and the technique has been modified by many to optimize its efficacy. Turek et al. [19] described systematic and geographic mapping of the testicle using FNA for the presence or absence of mature spermatozoa. Using a template, aspiration sites are marked on the scrotal skin 5 mm apart (Fig. 1). After the puncture pressure is applied to the puncture sites to ensure hemostasis. To map the sperm production, the testicular biopsy procedure is repeated in several areas. If insufficient sperm are found, the procedure is performed on the contralateral testis. In most men with NOA, mapping the testis is of greater value as it helps to direct subsequent open surgical biopsies. Postoperatively the patient is advised to use scrotal supports and ice packs for comfort. The site(s) where sperm are located on FNA are noted for subsequent open sperm retrieval. The number of aspiration sites ranges depends on the testicular volume.
Figure 1.
Schematic presentation of the systematic and geographic mapping of the testicle in FNA.
3.4.2. Complications and outcomes
The needle puncture may cause epididymal or vascular injury. This risk is higher in men with a history of scrotal surgery and scar tissue. Testicular hematoma and post biopsy fibrosis are also complications after the procedure. FNA pathology has a high correlation with testicular histological patterns. Several controlled studies comparing FNA with open testicular biopsy in NOA patients have suggested that open biopsies have a better chance of finding rare foci of testicular spermatozoa present within these poorly functioning gonads and of harvesting sufficient numbers of sperm for ICSI [20].
FNA correlates to testicular histology about 90% of the time. Sperm retrieval rates via TESE by histology are 14%–40% for Sertoli cell only, 70%–100% for hypospermatogenesis, 40%–75% for maturation arrest, and 20%–30% for tubular sclerosis. Sperm retrieval rates using 7-8 puncture sites in FNA is 25%–47%. SRR in one biopsy site by TESE is 41%–46%. SRR in 14–21 puncture sites utilizing FNA are 52%–58%. SRR via TESE using more than two sites yields 41%–60%. TESE is required 80% of the time after FNA mapping. The overall SRR by sample weight is 49.5% [20].
3.5. Open surgical approach
There are various sperm retrieval techniques described for men with NOA. General, spinal, or local anesthesia may be used. Perioperative antibiotics may be used in men with prior scrotal surgery or those with higher than average risk of forming a hematoma. Shave the scrotum and prepare the area with a non-betadine scrub and drape in standard sterile fashion. A median raphe incision gives ready access to both sides of the scrotum unless the testes are fixed in position high in the scrotum. The incision is extended through the dartos fibers to the tunica. The tunica vaginalis is then carefully opened allowing the epididymis and the testicle to be delivered. Microdissection of the tunica vaginalis from the testicle may be necessary in patients with a prior history of scrotal or testicular surgery as the tunica may be matted to the testicle. Proceed with either TESE or micro-TESE.
3.5.1. Open testicular biopsy and sperm extraction
Open testicular biopsy is utilized for both diagnosis and sperm retrieval. There are two methods of performing a conventional TESE. One can obtain a large quantity of seminiferous tubules through a single incision in the tunica albuginea. Alternatively, one may obtain samples through multiple biopsies via many small incisions in the tunica albuginea.
It is thought that single-site TESE will sample the multi-focal areas of spermatogenesis that is distributed throughout the testis. For this method, make a 5 mm transverse incision through the tunica albuginea with a small blade scalpel, avoiding blood vessels (Fig. 2).
Figure 2.
Open testicular biopsy. After the testicle is delivered and inspected, the tunica albuginea is incised about 5 mm transversely with a No. 11 blade scalpel avoiding any blood vessels, then gently squeezing the testicle and the protruding seminiferous tubules are excised using iris scissors.
Next gently squeeze the testis and excise the seminiferous tubules that protrude with iris scissors. Limit the amount of seminiferous tubules excised to about 50–100 mg as most of these patients have testicular dysfunction. Place the sample immediately in sperm wash medium. Examine the wet preparation intraoperatively with a phase contrast microscope to assess for the presence of sperm. Close the tunica albuginea with a continuous 5-0 monofilament polypropylene or nylon suture.
In the multiple biopsy technique, one or both testicles are delivered and avascular regions of the testicle are sequentially sampled through 5 mm incisions. Use the operating microscope to identify large subcapsular testicular vessels in the space between the tunica albuginea and testicular tissue. Transverse incisions minimize the risk of subcapsular hematomas. A No. 11 blade is used to make a 5 mm transverse incision in the tunica albuginea and then gentle testicular pressure is used to extrude seminiferous tubules, which are transected with fine surgical scissors. The specimens should be sequentially examined with a wet preparation, thus, ending the procedure when sperm are located. The biopsy site should be closed with a continuous 5-0 monofilament polypropylene or nylon suture.
3.5.2. Microdissection TESE
The use of the operating microscope at 15 × –20 × power allows for the identification of seminiferous tubules that are most likely to contain sperm. In 1999, Schlegel [3] observed qualitative differences in seminiferous tubules while performing conventional TESE under optical magnification. Quantitative analysis demonstrated that spermatozoa were present in larger tubules, but not in smaller or sclerotic ones. Harvesting larger tubules decreases the amount of testicular tissue that needs to be removed by 70-fold [7].
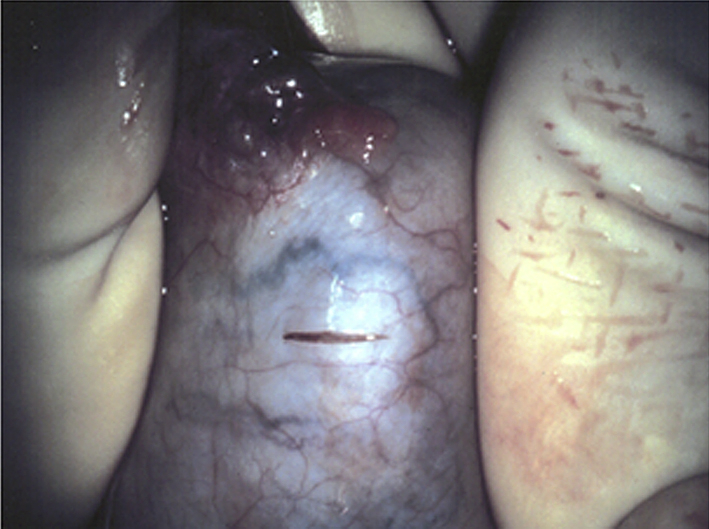
Operate first on the larger testicle or if both are equal in size, the right testicle. After the testicle is delivered, use optical magnification 6 × –8 × power to visualize blood vessels under the surface of the tunica albuginea and thereby incise an avascular region. Make a wide transverse incision in an equatorial plane along the midportion with an ophthalmic (miro) knife. This facilitates adequate exposure of seminiferous tubules, in this physiological approach, and the centrifugal vessels, which run parallel to the tubules and septae. In contrast, a small incision limits exposure and can adversely affect the surgeon's ability to visualize and control any bleeding. Longitudinal incisions, while possible, will disrupt the primary testicular blood supply that wraps around the posterior and lower pole sections of the testis if the testis is opened enough to expose all seminiferous tubules. Secure the edge of the cut tunica and seminiferous tubules together, using fine small hemostats. This limits the risk of separation during the procedure and facilitates exposure and dissection within the tissue. Open the testicle with gentle pressure.
All seminiferous tubules must be examined to identify small foci of spermatogenesis. The seminiferous tubules are highly coiled within very fine septae. The dissection should be carried out between tubules to allow access to deeper sections of the seminiferous tubules (Fig. 3). The space between the tubules and the tunica is highly vascular, so bleeding that would be very difficult to control can occur if there is separation of tissue from the tunica albuginea and/or if there is dissection in this plane. To prevent separation of seminiferous tubules from their blood supply and thereby devascularize the seminiferous tubules, avoid excessive force during the dissection. Postoperative bleeding and hematoma formation after micro-TESE can lead to scarring within the testis after surgery. Careful dissection and meticulous hemostasis after the procedure will minimize complications. Microdissection continues as an interactive procedure until sperm are found or all regions of both testes have been examined. Typically, small samples of 2–10 mg are obtained, which is far less than the 50–75 mg removed with conventional TESE [3]. If sperm are not found in one testicle, repeat the process in the contralateral testicle. Once adequate sperm are found, hemostasis is attained using bipolar cautery. The tunica albuginea of the bivalved testicle is brought together with a series of small fine hemostats and the testicle is closed with running 5-0 non-absorbable monofilament suture under magnification, avoiding laceration of the sub-tunical vessels.
Figure 3.

Bivalved testis. Wide exposure of seminiferous tubules and the centrifugal vessels running parallel to the tubules and septae. Small hemostats are used to secure the edge of the cut tunica and seminiferous tubules together, limiting the risk of separation during the procedure and facilitating exposure and dissection.
3.5.3. Sperm and tissue processing
Sperm production occurs within the seminiferous tubules; therefore, mechanical processing of the samples in the operating room is essential to identify sperm in these tissues. The processing involves cutting tissue samples then passing the resulting suspension through a fine (i.e., 24 gauge) angiocatheter, thus, facilitating the release of sperm from the tubules. This processing increases the yield of testicular sperm on intraoperative wet preparation analysis up to 300-fold [21]. Once sperm are found on wet mount, the procedure can be terminated. Sperm are not always identified on the wet preparation analysis in the operating room. The samples are sent to a laboratory for enzymatic treatment for tubule digestion to search for viable sperm, although this has a relatively low success rate that ranges between 7% and 25% [22]. Once the tunica albuginea is closed and the testis is returned to the scrotum in its proper anatomic orientation, close the richly vascularized tunica vaginalis with a running 5-0 absorbable suture, which is then followed by dartos and skin closure.
3.5.4. TESE and micro-TESE complications and outcomes
The testicular anatomy and vascular supply must be respected otherwise TESE or micro-TESE may lead to compromise of testicular blood flow. The testicular blood flow may be compromised from interference of the vascular supply or from bleeding enclosed within the tunica albuginea leading to an increased intratesticular pressure. Postoperative ultrasound shows fewer acute and chronic changes in patients undergoing micro-TESE. Postoperative ultrasound on men who underwent TESE showed up to 80% of men had sonographic evidence of structural changes or intratesticular hematoma [23]. The prevalence of sonographic changes consistent with fibrosis 6 months after surgery was 3.3% after micro-TESE compared to 30% after TESE [24]. Testicular vessels run under the tunica; optical magnification can identify and allow one to avoid transecting the sub-tunical vessels during initial incision. Meticulous hemostasis during and after sperm retrieval helps prevent hematoma formation. Bipolar cautery should be used to avoid heat injury.
Functional evaluation of the testicle after micro-TESE showed a decrease in the serum testosterone concentrations by 20% at 3–6 months, followed by rebound to 95% of the pre-TESE testosterone levels at 18 months postoperatively [25]. Micro-TESE has the lowest complication rates of all testicular sperm retrieval procedures [23]. As with all surgical procedures, risks include infection, bleeding, and postoperative pain.
TESE with multiple biopsies has a better SRR than both single biopsy TESE and multiple FNAs, especially in cases of Sertoli cell only (SCO) syndrome and maturation arrest [23]. In retrospective studies, conventional TESE for NOA have an SRR of 16.7% compared to micro-TESE in NOA with an SRR of 44.6% [26]. Retrospective studies with a controlled comparison show an SRR of 62% for micro-TESE vs. 45% in TESE. The treatment of choice is becoming micro-TESE combined with ICSI for certain subsets of men diagnosed with NOA who want biological offspring. The results for TESE and micro-TESE for men with NOA, including those with Klinefelter's Syndrome, cryptorchidism, prior history of chemotherapy and Y chromosome (AZFc) microdeletions, are summarized below [3], [9], [27].
Overall SRR via micro-TESE cycle ranges from 56% to 62%. After chemotherapy SRR via micro-TESE decreases to 37%–85%. Patients with Klinefelter's syndrome have SRR of 65%–70% using micro-TESE. Patients with a history of cryptorchidism have SRR of 55%–74% utilizing micro-TESE [3], [9], [27]. According to the published evidence, men with SCO syndrome had SRR with micro-TESE of 40%, those with maturation arrest had SRR of 36% with micro-TESE, and those with hypospermatogenesis had SRR of 75% with micro-TESE [28]. Tournaye et al. [29] reported the SRR in TESE to be 84% with incomplete germ-cell aplasia and maturation arrest (MA) as opposed to SRR of 76% in patients with complete germ-cell aplasia or MA.
Tournaye et al. [29] reported TESE overall fertilization rate of 57.8%, with the fertilization rate lower in couples with germ-cell aplasia and MA. Fifty-five percent of normally fertilized oocytes developed into embryos, and overall pregnancy rates of 36.3% per TESE procedure. Bryson et al. [30] reported overall SRR of 56% in micro-TESE with respective clinical pregnancy and live birth rates of 55.2% and 47.2% in patients with testicular volume of <2 mL; 50.0% and 43.0% in men with testicular volumes of 2–10 mL; 47.0% and 42.2% in men with testicular volume of 10 mL or greater. Raheem et al. [31] reported overall clinical pregnancy rate of 32% in men with NOA and live birth rate of 20% after testicular sperm extraction (most patients in this series had TESE). The clinical pregnancy rate was higher for normal spermatogenesis groups (50%) compared to hypospermatogenesis (30%) and MA (25%) versus SCO (33%).
4. Conclusion
Micro-TESE has a higher SRR with fewer postoperative complications and negative effects on testicular function compared with conventional TESE.
Conflicts of interest
The authors declare no conflict of interest.
Footnotes
Peer review under responsibility of Chinese Urological Association and SMMU.
References
- 1.Jarow J.P., Espeland M.A., Lipshultz L.I. Evaluation of the azoospermic patient. J Urol. 1989;142:62–65. doi: 10.1016/s0022-5347(17)38662-7. [DOI] [PubMed] [Google Scholar]
- 2.Zukerman Z., Rodriguez-Rigau L.J., Weiss D.B., Chowdhury A.K., Smith K.D., Steinberger E. Quantitative analysis of the seminiferous epithelium in human testicular biopsies, and the relation of spermatogenesis to sperm density. Fertil Steril. 1978;30:448–455. doi: 10.1016/s0015-0282(16)43581-8. [DOI] [PubMed] [Google Scholar]
- 3.Schlegel P.N. Testicular sperm extraction: microdissection improves sperm yield with minimal tissue excision. Hum Reprod. 1999;14:131–135. doi: 10.1093/humrep/14.1.131. [DOI] [PubMed] [Google Scholar]
- 4.Palermo G., Joris H., Devroey P., Van Steirteghem A.C. Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet. 1992;340:17–18. doi: 10.1016/0140-6736(92)92425-f. [DOI] [PubMed] [Google Scholar]
- 5.Ron-El R., Strassburger D., Friedler S., Komarovski D., Bern O., Soffer Y. Extended sperm preparation: an alternative to testicular sperm extraction in non-obstructive azoospermia. Hum Reprod. 1997;12:1222–1226. doi: 10.1093/humrep/12.6.1222. [DOI] [PubMed] [Google Scholar]
- 6.Rucker G.B., Mielnik A., King P., Goldstein M., Schlegel P.N. Preoperative screening for genetic abnormalities in men with nonobstructive azoospermia before testicular sperm extraction. J Urol. 1998;160:2068–2071. doi: 10.1097/00005392-199812010-00034. [DOI] [PubMed] [Google Scholar]
- 7.Schlegel P.N. Nonobstructive azoospermia: a revolutionary surgical approach and results. Semin Reprod Med. 2009;27:165–170. doi: 10.1055/s-0029-1202305. [DOI] [PubMed] [Google Scholar]
- 8.Raman J.D., Schlegel P.N. Aromatase inhibitors for male infertility. J Urol. 2002;167:624–629. doi: 10.1016/S0022-5347(01)69099-2. [DOI] [PubMed] [Google Scholar]
- 9.Ramasamy R., Ricci J.A., Palermo G.D., Gosden L.V., Rosenwaks Z., Schlegel P.N. Successful fertility treatment for Klinefelter's syndrome. J Urol. 2009;182:1108–1113. doi: 10.1016/j.juro.2009.05.019. [DOI] [PubMed] [Google Scholar]
- 10.Reifsnyder J.E., Ramasamy R., Husseini J., Schlegel P.N. Role of optimizing testosterone before microdissection testicular sperm extraction in men with nonobstructive azoospermia. J Urol. 2012;188:532–536. doi: 10.1016/j.juro.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 11.Aydos K., Unlu C., Demirel L.C., Evirgen O., Tolunay O. The effect of pure FSH administration in non-obstructive azoospermic men on testicular sperm retrieval. Eur J Obstet Gynecol Reprod Biol. 2003;108:54–58. doi: 10.1016/s0301-2115(02)00412-8. [DOI] [PubMed] [Google Scholar]
- 12.Shiraishi K., Ohmi C., Shimabukuro T., Matsuyama H. Human chorionic gonadotrophin treatment prior to microdissection testicular sperm extraction in non-obstructive azoospermia. Hum Reprod. 2012;27:331–339. doi: 10.1093/humrep/der404. [DOI] [PubMed] [Google Scholar]
- 13.Hussein A., Ozgok Y., Ross L., Rao P., Niederberger C. Optimization of spermatogenesis-regulating hormones in patients with non-obstructive azoospermia and its impact on sperm retrieval: a multicentre study. BJU Int. 2013;111:E110–E114. doi: 10.1111/j.1464-410X.2012.11485.x. [DOI] [PubMed] [Google Scholar]
- 14.Pavlovich C.P., King P., Goldstein M., Schlegel P.N. Evidence of a treatable endocrinopathy in infertile men. J Urol. 2001;165:837–841. [PubMed] [Google Scholar]
- 15.Schlegel P.N., Kaufmann J. Role of varicocelectomy in men with nonobstructive azoospermia. Fertil Steril. 2004;81:1585–1588. doi: 10.1016/j.fertnstert.2003.10.036. [DOI] [PubMed] [Google Scholar]
- 16.Ramasamy R., Schlegel P.N. Microdissection testicular sperm extraction: effect of prior biopsy on success of sperm retrieval. J Urol. 2007;177:1447–1449. doi: 10.1016/j.juro.2006.11.039. [DOI] [PubMed] [Google Scholar]
- 17.Kahraman S., Ozgür S., Alataş C., Aksoy S., Taşdemir M., Nuhoğlu A. Fertility with testicular sperm extraction and intracytoplasmic sperm injection in non-obstructive azoospermic men. Hum Reprod. 1996;11:756–760. doi: 10.1093/oxfordjournals.humrep.a019249. [DOI] [PubMed] [Google Scholar]
- 18.Obrant K.O., Persson P.S. [Cytological study of the testis by aspiration biopsy in the evaluation of fertility] [Article in German] Urol Int. 1965;20:176–189. doi: 10.1159/000279375. [DOI] [PubMed] [Google Scholar]
- 19.Turek P.J., Cha I., Ljung B.M. Systematic fine-needle aspiration of the testis: correlation to biopsy and results of organ “mapping” for mature sperm in azoospermic men. Urology. 1997;49:743–748. doi: 10.1016/S0090-4295(97)00154-4. [DOI] [PubMed] [Google Scholar]
- 20.Rosenlund B., Kvist U., Ploen L., Rozell B.L., Sjoblom P., Hillensjo T. A comparison between open and percutaneous needle biopsies in men with azoospermia. Hum Reprod. 1998;13:1266–1271. doi: 10.1093/humrep/13.5.1266. [DOI] [PubMed] [Google Scholar]
- 21.Ostad M., Liotta D., Ye Z., Schlegel P.N. Testicular sperm extraction for nonobstructive azoospermia: results of a multibiopsy approach with optimized tissue dispersion. Urology. 1998;52:692–696. doi: 10.1016/s0090-4295(98)00322-7. [DOI] [PubMed] [Google Scholar]
- 22.Aydos K., Demirel L.C., Baltaci V., Unlu C. Enzymatic digestion plus mechanical searching improves testicular sperm retrieval in non-obstructive azoospermia cases. Eur J Obstet Gynecol Reprod Biol. 2005;120:80–86. doi: 10.1016/j.ejogrb.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 23.Donoso P., Tournaye H., Devroey P. Which is the best sperm retrieval technique for non-obstructive azoospermia? A systematic review. Hum Reprod Update. 2007;13:539–549. doi: 10.1093/humupd/dmm029. [DOI] [PubMed] [Google Scholar]
- 24.Amer M., Ateyah A., Hany R., Zohdy W. Prospective comparative study between microsurgical and conventional testicular sperm extraction in non-obstructive azoospermia: follow-up by serial ultrasound examinations. Hum Reprod. 2000;15:653–656. doi: 10.1093/humrep/15.3.653. [DOI] [PubMed] [Google Scholar]
- 25.Ramasamy R., Yagan N., Schlegel P.N. Structural and functional changes to the testis after conventional versus microdissection testicular sperm extraction. Urology. 2005;65:1190–1194. doi: 10.1016/j.urology.2004.12.059. [DOI] [PubMed] [Google Scholar]
- 26.Okada H., Dobashi M., Yamazaki T., Hara I., Fujisawa M., Arakawa S. Conventional versus microdissection testicular sperm extraction for nonobstructive azoospermia. J Urol. 2002;168:1063–1067. doi: 10.1016/S0022-5347(05)64575-2. [DOI] [PubMed] [Google Scholar]
- 27.Dabaja A.A., Schlegel P.N. Microdissection testicular sperm extraction: an update. Asian J Androl. 2013;15:35–39. doi: 10.1038/aja.2012.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kalsi J.S., Shah P., Thum Y., Muneer A., Ralph D.J., Minhas S. Salvage mico-dissection testicular sperm extraction; outcome in men with non obstructive azoospermia with previous failed sperm retrievals. BJU Int. 2014 Sep 15 doi: 10.1111/bju.12932. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 29.Tournaye H., Liu J., Nagy P.Z., Camus M., Goossens A., Silber S. Correlation between testicular histology and outcome after intracytoplasmic sperm injection using testicular spermatozoa. Hum Reprod. 1996;11:127–132. doi: 10.1093/oxfordjournals.humrep.a019004. [DOI] [PubMed] [Google Scholar]
- 30.Bryson C.F., Ramasamy R., Sheehan M., Palermo G.D., Rosenwaks Z., Schlegel P.N. Severe testicular atrophy does not affect the success of microdissection testicular sperm extraction. J Urol. 2014;191:175–178. doi: 10.1016/j.juro.2013.07.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Raheem A.A., Rushwan N., Garaffa G., Zacharakis E., Doshi A., Heath C. Factors influencing intracytoplasmic sperm injection (ICSI) outcome in men with azoospermia. BJU Int. 2013;112:258–264. doi: 10.1111/j.1464-410X.2012.11714.x. [DOI] [PubMed] [Google Scholar]