Abstract
Objective
With today's modern imaging modalities, patients diagnosed with renal cell carcinoma (RCC) rarely present symptomatically. In some cases, however, they can develop paraneoplastic syndromes with associated symptoms. To date, only three cases of RCC presenting with chronic dry cough have been reported. We describe six patients who presented with cough that improved following radical nephrectomy.
Methods
A retrospective review of patients undergoing partial or radical nephrectomy for renal masses between January 2015 and March 2016 was performed, and patients presenting with a cough were examined.
Results
Six patients presented with chronic cough and were discovered to have a large renal mass. Postoperative spontaneous resolution of cough was noted in all but one patient, in whom coughing was reduced and limited to the mornings. Cough duration ranged from 3 months to just over a year. All patients were treated with radical nephrectomy, which was cytoreductive in four patients. Average tumor size was 10.9 cm (SD = 2.2 cm). Five of the tumors had clear cell pathology, and every tumor was Fuhrman grade IV, unifocal, and demonstrated necrosis. Sarcomatoid features were reported in four of the tumors.
Conclusion
Our study presents the largest series of patients with RCC who presented with a chronic cough that was significantly improved following radical nephrectomy. We believe the cause of cough is multifactorial and further investigation is needed to clearly elucidate the etiology.
Keywords: Renal cell carcinoma, Paraneoplastic syndrome, Cough, Mass effect, Cytokines, Renin-angiotensin system
1. Introduction
Renal cell carcinoma (RCC) is often asymptomatic, with an increasing number of patients being diagnosed incidentally thanks in large part to increased utilization of abdominal imaging [1]. When the disease does present symptomatically, however, RCC has variable clinical symptoms, commonly including hematuria, flank pain, fever, and weight loss. It is estimated that 10%–40% of patients develop paraneoplastic syndromes, including metabolic, hepatic, and hematologic syndromes [2]. Although the lungs are a common site of metastasis in patients with RCC, respiratory paraneoplastic syndromes are rare, with only three cases of RCC presenting with cough having been reported in the literature [3], [4], [5]. No clear explanation for these coughs has been elucidated; however, mass effect causing diaphragmatic irritation as well as paraneoplastic cytokines or growth factors have been hypothesized as possible causes. We present six patients, all of whom presented with cough that improved following radical nephrectomy.
2. Materials and methods
Following Institutional Review Board approval, data were prospectively collected from patients undergoing partial or radical nephrectomy for renal masses between January 2015 and March 2016 from a high volume tertiary care center. Patient demographics, presenting symptoms, preoperative lab values, surgical approach (open vs. laparoscopic), laterality, tumor pathology (size, histology, Fuhrman grade, pathologic stage, histological features, and focality), and postoperative follow-up were evaluated. Patients under the age of 18 years and those with no history of cough were excluded. All patients had more than 3 months of postoperative surveillance.
Descriptive statistics are presented as counts and percentages for categorical variables and as means and standard deviations (SD) for continuous variables. All calculations were performed using SPSS, v24.0 (IBM, Chicago, IL, USA).
3. Results
3.1. Patient and disease characteristics
Six patients all presenting with a chief complaint of chronic dry cough and subsequently found to have large renal mass were identified. Postoperative spontaneous resolution of cough was noted in all but one patient, in whom coughing persisted but was significantly reduced and limited only to the mornings.
Baseline patient and disease characteristics are presented in Table 1. Mean age was 53.3 years (SD = 8.1 years), and five of the patients were male. Only one patient presented with flank pain and fever; the remaining patients reported weight loss averaging 10.5 kg (SD = 6.4 kg). Cough duration ranged from 3 months to just over a year. Workup for cough included a CT scan of the chest and abdomen in five of the patients, which revealed a renal mass in each case; the final patient had been taking prednisone intermittently for several months, and his mass was not discovered until he presented with flank pain and fever.
Table 1.
Baseline patient and disease characteristics.
| Characteristics | Values |
|---|---|
| Age (year)a | 53.3 ± 8.1 |
| Genderb | |
| Male | 5 (83) |
| Female | 1 (17) |
| Presenting symptomb | |
| Flank pain | 1 (17) |
| Fever | 1 (17) |
| Weight loss | 5 (83) |
| Cough | 6 (100) |
| Weight loss (kg)a | 10.5 ± 6.4 |
| Duration of cough (month)a | 5.6 ± 4.1 |
| Nephrectomy typeb | |
| Radical | 6 (100) |
| Cytoreductive | 4 (67) |
| Surgical approachb | |
| Open | 1 (17) |
| Laparoscopic | 5 (83) |
| Preoperative lab valuea | |
| Hemoglobin (g/L) | 101 ± 19 |
| Total serum calcium (mg/L) | 97 ± 8 |
| Alkaline phosphatase (U/L) | 145.0 ± 69.5 |
| Follow-up (month)a | 7.8 ± 3.4 |
Values are presented as mean ± SD.
Values are presented as n (%).
All patients were treated with radical nephrectomy, and the operation was cytoreductive in four cases. Two patients had pulmonary nodules concerning for metastasis at the time of nephrectomy, one patient had mediastinal adenopathy, and another patient had periaortic adenopathy. Each nephrectomy began laparoscopically, but one needed to be converted to open following an intraoperative complication of hemorrhage leading to hypotension.
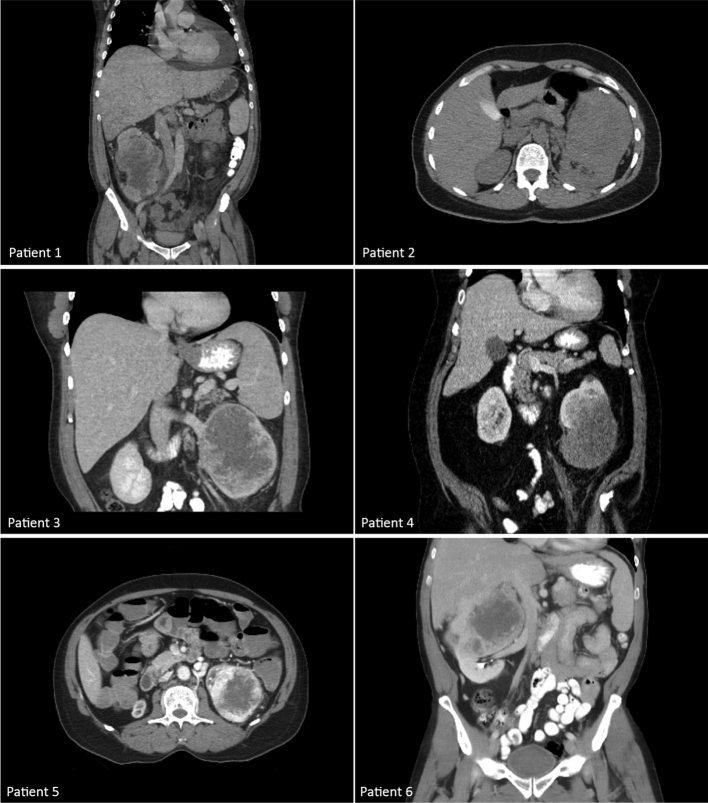
Table 2 summarizes tumor characteristics found on surgical pathology. Average tumor size was 10.9 cm (SD = 2.2 cm). Fig. 1 shows preoperative CT scans for each patient. Tumors were clear cell in five of the cases; one was unclassified due to mixed morphologic and immunohistochemical features. Every tumor was Fuhrman grade IV, unifocal, and demonstrated necrosis. Sarcomatoid features were observed in four of the tumors.
Table 2.
Tumor characteristics found on surgical pathology.
| Characteristics | Values |
|---|---|
| Tumor size (cm)a | 10.9 ± 2.2 |
| Tumor histologyb | |
| Clear cell | 5 (83) |
| Unclassified | 1 (17) |
| Fuhrman gradeb | |
| IV | 6 (100) |
| Tumor stageb | |
| pT2a | 1 (17) |
| pT2b | 1 (17) |
| pT3a | 3 (50) |
| pT4 | 1 (17) |
| Histologic featureb | |
| Positive surgical margin | 0 (0) |
| Sarcomatoid feature | 4 (67) |
| Necrosis | 6 (100) |
| Perinephric fat invasion | 2 (33) |
| Sinus fat invasion | 3 (50) |
| Renal vein invasion | 2 (33) |
| Lymphovascular invasion | 2 (33) |
| Tumor focalityb | |
| Unifocal | 6 (100) |
| Tumor sideb | |
| Right | 2 (33) |
| Left | 4 (67) |
Values are presented as mean ± SD.
Values are presented as n (%).
Figure 1.
CT scans of renal masses prior to nephrectomy.
3.2. Follow-up
The average follow-up time was 7.8 months (SD = 3.4 months). Five out of six patients remain completely free of cough to date. Two of the patients are recovering well and now on surveillance, with no evidence of local recurrence or metastasis. They will continue to receive yearly imaging of the chest, abdomen, and pelvis.
In one patient, two new lesions, sized 2 mm and 6 mm, were seen in an MRI of the brain 4 months after nephrectomy. He underwent stereotactic radiation to his brain as well as whole brain radiation therapy. He is currently undergoing chemotherapy with axitinib for his metastatic RCC. A recent CT scan showed a decrease in lung and pleural-based metastasis with no change in the size of a metastatic growth in the retroperitoneum.
Another patient who had mediastinal adenopathy at the time of surgery had a subsequent biopsy 1 month after nephrectomy, which revealed metastatic RCC. This patient elected treatment with interleukin-2 therapy.
A PET/CT scan was performed just over 1 month following another patient's nephrectomy, revealing metastasis to his right femur and spine as well as the presence of adenopathy in his supraclavicular and axillary lymph nodes. Two months following this, he underwent stereotactic body radiation therapy for his spine and femur. Follow-up MRI scans reveal radiographic partial regression of the metastasis in his spine.
Finally, one patient, taking enalapril for hypertension following nephrectomy, still suffered from a mild cough, although significantly reduced. He experienced clinical progression of disease with development of large pleural effusions; biopsies from the pleural surface revealed presence of clear cell carcinoma. This patient died from complications related to metastasis.
4. Discussion
Paraneoplastic syndromes associated with RCC can range widely in their presentation. The six cases described above represent unusual instances of RCC, with only three similar cases of patients presenting with a chronic cough having been previously reported in the literature [3], [4], [5]. In all six cases, evaluation of the cough led to the diagnosis of a renal mass. While the mechanism of the coughing is not fully understood, it is clear that tumor removal significantly improved this presenting symptom in each patient as evidenced by complete resolution in all but one patient, who had significant improvement.
One explanation for the coughing may be the mass effect of these large tumors. Presence of a large mass may have led to irritation of the diaphragm, causing a reflexive cough alleviated only by removal of the tumor [6]. In the six cases in our retrospective review, each of the carcinomas was relatively large, ranging from 8.5 cm to 14.0 cm. In none of the cases, however, was there direct extension into the diaphragm. Historically, prior to the advent of axial imaging, most renal tumors were detected at a large size. If mass effect was the primary cause, one would expect many more cases to have been reported in the literature.
Fujikawa et al. [3] described a patient with a 15 cm renal mass whose coughing was dramatically reduced following embolization but prior to nephrectomy. In this instance, mass effect did not appear to have been the cause of the cough. This case, as well as the paucity of coughing as a presenting symptom in individuals with renal cancer, points to other potential causes.
RCC is known to cause several paraneoplastic syndromes, from hepatic dysfunction to electrolyte abnormalities to anemia [2]. The etiology of some of the most common syndromes has been elucidated. Interleukin-6, for example, is a cytokine produced by RCCs that has been linked to higher serum C-reactive protein and haptoglobin as well as platelet, polymorphonuclear neutrophil, and monocyte counts [7], [8]. Cytokines or growth factors produced by tumor cells or the immune system have been shown to produce a cough; indeed, prostaglandins secreted by RCCs, specifically prostaglandin E2, have been shown to act upon the cough reflex [9]. As such, it is conceivable that a factor produced by these cancers may have led to a paraneoplastic syndrome in the form of a cough. Moreover, as 67% of our nephrectomies were cytoreductive with synchronous lesions, a clinically significant reduction in biochemical substrates may also play a role in the abatement of the cough. Interestingly, in one of our patients, the cough which initially abated after nephrectomy returned 1 year later and correlated with appearance of new metastasis. Institution of axitinib therapy resulted in suppression of the cough as well as a reduction in the size of his lung and pleural-based metastasis.
Finally, alterations in the renin-angiotensin system may be another area of investigation. It is widely known that angiotensin-converting enzyme inhibitors prevent the breakdown of bradykinin, leading to cough as a potential side effect. Increased bradykinin levels may be due to alterations in the renin-angiotensin system, leading to the paraneoplastic cough, but further investigation is necessary to validate this mechanism.
Without a complete set of lab values for each patient, we can only hypothesize why they all presented with the cough. It is important to note, however, that our six patients each had large tumors, and every tumor was Fuhrman grade IV and demonstrated necrosis on surgical pathology, well-known characteristics associated with a poor prognosis. In all but one case, cough resolved completely following nephrectomy. Despite these similarities, multiple pathophysiological mechanisms may be responsible for this paraneoplastic syndrome.
5. Conclusion
Chronic dry cough is a known paraneoplastic syndrome in patients with RCC. This is the largest collection of patients who presented with this symptom. Further investigation is needed to elucidate the cause or causes of the cough. Patients may be counselled that this symptom will likely improve significantly following radical nephrectomy, even if cytoreductive in nature.
Conflicts of interest
The authors declare no conflict of interest.
Footnotes
Peer review under responsibility of Second Military Medical University.
References
- 1.Chow W.H., Devesa S.S., Warren J.L., Fraumeni J.F. Rising incidence of renal cell cancer in the United States. JAMA. 1999;281:1628–1631. doi: 10.1001/jama.281.17.1628. [DOI] [PubMed] [Google Scholar]
- 2.Palapattu G.S., Kriso B., Rajfer J. Paraneoplastic syndromes in urologic malignancy: the many faces of renal cell carcinoma. Rev Urol. 2002;4:163–170. [PMC free article] [PubMed] [Google Scholar]
- 3.Fujikawa A., Daidoh Y., Taoka Y., Nakamura S. Immediate improvement of a persistent cough after tumor embolization for renal cell carcinoma–a rare manifestation of paraneoplastic syndrome. Scand J Urol Nephrol. 2002;36:393–395. doi: 10.1080/003655902320783962. [DOI] [PubMed] [Google Scholar]
- 4.Okubo Y., Yonese J., Kawakami S., Yamamoto S., Komai Y., Takeshita H. Obstinate cough as a sole presenting symptom of non-metastatic renal cell carcinoma. Int J Urol. 2007;14:854–855. doi: 10.1111/j.1442-2042.2007.01832.x. [DOI] [PubMed] [Google Scholar]
- 5.Tatzel S., Sener A. Persistent dry cough: an unusual presentation of renal cell carcinoma. CMAJ. 2014;186:136. doi: 10.1503/cmaj.130355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chung K.F., Pavord I.D. Prevalence, pathogenesis, and causes of chronic cough. Lancet. 2008;371:1364–1374. doi: 10.1016/S0140-6736(08)60595-4. [DOI] [PubMed] [Google Scholar]
- 7.Blay J.Y., Rossi J.F., Wjdenes J., Menetrier-Caux C., Schemann S., Negrier S. Role of interleukin-6 in the paraneoplastic inflammatory syndrome associated with renal-cell carcinoma. Int J Cancer. 1997;72:424–430. doi: 10.1002/(sici)1097-0215(19970729)72:3<424::aid-ijc9>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 8.Walther M.M., Johnson B., Culley D., Shah R., Weber J., Venzon D. Serum interleukin-6 levels in metastatic renal cell carcinoma before treatment with interleukin-2 correlates with paraneoplastic syndromes but not patient survival. J Urol. 1998;159:718–722. [PubMed] [Google Scholar]
- 9.Maher S.A., Birrell M.A., Belvisi M.G. Prostaglandin E2 mediates cough via the EP3 receptor: implications for future disease therapy. Am J Respir Crit Care Med. 2009;180:923–928. doi: 10.1164/rccm.200903-0388OC. [DOI] [PMC free article] [PubMed] [Google Scholar]