Abstract
Objective
The goal of hypospadias repair is to achieve normal voiding and good penile cosmesis with minimal complications. Some urethroplasties deteriorate from childhood to adolescence and late stage failures have been reported. We report our experience with adult patients who have had a previous repair during childhood and present with a late complication.
Methods
We reviewed the records of 220 patients aged 15–39 years old with a history of hypospadias repair who presented to our clinic. Forty-five patients with chordee, 39 with urethral strictures, 11 urethral fistulae, five with hairy urethras, three with urethral diverticula, and 117 patients with an abnormal glans or subterminal meatus were repaired.
Results
Median follow-up was 14 months. Two patients had persistent chordee. Island skin flap urethroplasty afforded one patient with a urethral fistula and another with a recurrent urethral stricture, while the buccal mucosa group had one fistula which healed spontaneously and two recurrent strictures. For the patients undergoing glanular repairs, seven had dehiscence or breakdown of the repair. All other operations were successful.
Conclusion
Complications of childhood hypospadias repair may present later in life as some urethroplasties deteriorate with time. We now recommend to parents of children with repaired proximal hypospadias to come for follow-up as their child transitions to adolescence.
Keywords: Hypospadias, Adult, Adolescent, Failure, Complication
1. Introduction
Hypospadias repair in children aims at the creation of a straight penis, an adequate caliber neo-urethra, and a meatus at or near the tip of the glans penis. The goal is to achieve normal voiding and good penile cosmesis with minimal complications. Short-term follow-up reports indicate that 90% success rate can be accomplished with modern surgical techniques. However, some urethroplasties deteriorate from childhood to adolescence and late stage failures have been reported. A three-decade series from 1978 to 2009 by Prat et al. [1] found 4.6% of 820 patients required further revision in adolescence. A study of more than 5000 patients found a 9% secondary surgery rate for distal hypospadias repair and 32.2% for proximal hypospadias repairs [2].
Hypospadias repair in adults can be divided into three groups: the first group are primary cases, the second group include patients who have had a previous repair during childhood and present with a late complication (e.g., urethrocutaneous fistula, persistent curvature, urethral stricture, urethral diverticulum and poor cosmesis), and the third group are patients who have undergone several failed surgeries referred to as “hypospadias cripples”. Herein, we report on the management of 220 patients who fall in to the second group.
2. Materials and methods
We reviewed the records of 220 patients (15–39 years old) treated between 1981 and 2015. Seventy-two patients out of 220 had their primary surgery by us. Forty-five patients complained of penile curvature of whom 11 had urethral fistula. Their repairs were 16 patients with Nesbitt [3] procedure, 14 with Baskin [4] modification of midline stitch, and 15 patients with corporal dermal grafts (Fig. 1). One hundred and seventy-five patients presented with voiding abnormalities (straining, spraying or leakage and post void dripping) of whom 39 had urethral stricture, and 18 had mild-to-moderate chordee which was corrected in conjunction with the urethral repair. The length of urethral strictures varied between 2 and 12 cm (mean 7.5 cm). Earlier in the series their treatment was one-stage repair using an island local skin onlay flap in 14 patients. Subsequently a buccal mucosa onlay graft was used in 23 and mucosal inlay in two patients. All patients who underwent one-stage repair had an intact residual but narrow urethral plate. The curvature was due to subcutaneous scarring in 27/39 patients and was corrected by penile degloving and excision of scar tissues, and in 12 patients the curvature was corrected by dorsal tunica plication. Eleven patients who had had Lichen sclerosis (LS), underwent two-stage repair. In the first stage they underwent radical excision of the scarred tissues and placement of a neo-plate using a buccal mucosal graft harvested from the inner cheek (Fig. 2), 9–16 months later the graft was tubularized, however 2/11 patients underwent graft revision due to scarring. Five patients presented with hairy urethra of whom two presented with urinary retention due to stone formation. Transurethral laser depilation was tried in two patients but was ineffective, and we had to remove the hairy urethra and replace it with a one-stage buccal mucosal patch in three, and two-stage urethroplasty in the other two patients. Three patients had urethral diverticulum and underwent excision and trimming of the skin lining of the diverticulum and preservation of the peri-diverticular tissue to wrap around the constructed urethral tube (Fig. 3). One hundred and seventeen patients presented with abnormal glans penis and/or subterminal meatus and complained of urine spraying and/or aesthetic concerns (Fig. 4).
Figure 1.
Chordee. (A) Severe curvature with artificial erection after penile degloving. (B) Penis now straight after placement of a dermal graft.
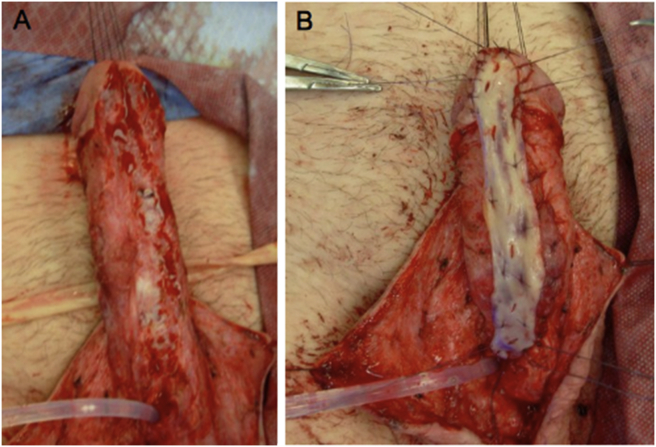
Figure 2.
Urethral stricture. (A) Excessive scar tissue from Lichen sclerosis causing stricture disease. (B) Buccal mucosa graft placement used during urethroplasty.
Figure 3.
Urethral diverticulum. (A) Dilated penile urethra due to diverticulum. (B) Opening of the urethra, followed by excision of diverticulum and simple closure.
Figure 4.
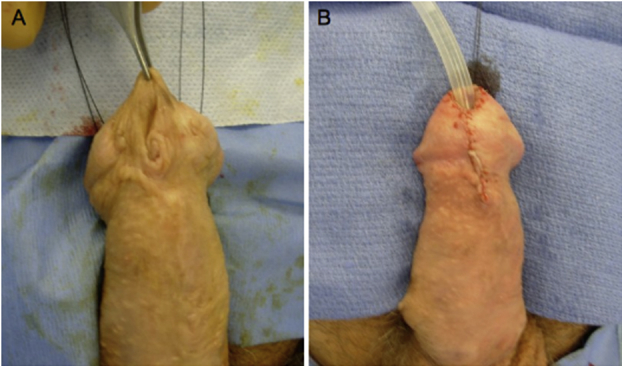
Recurrent hypospadias and meatal stenosis. (A) Patient presents for urine spraying, found to have subterminal meatus with abnormal contour. (B) Postoperative appearance after meatal advancement and glanuloplasty.
3. Results
Follow-up of 6–48 months (median 14 months) was recorded in 41/45 patients who had chordee repair; the penis was straight in 39/41, and improved in the other two patients (one had Nesbitt, and another had Baskin repairs), none had any sexual functional complaints. The other four patients were seen for few weeks postoperatively then lost to follow-up. All fistula repairs were successful. For urethral stricture disease, a successful outcome was defined as resolution of symptoms, patient observation of his urine flow for a minimum of 2 years and cystoscopic evaluation was performed in the first 29 patients at 6–12 months (but subsequently found to be unnecessary and cystoscopy was performed if the patient became symptomatic). Postoperative urethral calibration with an 18 Fr metal sound was performed in the majority of patients. The morbidity of island skin flaps were one case of fistula which was corrected and another case of recurrent stricture, who refused further treatment. For the buccal mucosa onlay and inlay group (25 patients), one developed a urethral fistula which healed spontaneously and two had recurrent stricture and are performing self-dilation. Surgical repair of the 11 patients with LS and the five hairy urethra was successful in 14/16 patients, but two were lost to follow-up. Urethral diverticulectomy was successful in all three patients.
Of the 117 patients there were 45 glans approximation procedure (GAP) repairs for coronal meatus, 59 meatal advancement and contouring for meatal irregularity, and 13 cosmetic repairs including glans sculpting. Early complications included glans dehiscence in 3/45 of the GAP repairs, break down of the repair in 4/59 of meatal advancement. Among the 117 patients, 89 patients were followed for a minimum of 6 months and 28 patients were seen in follow-up for few weeks only. All patients were satisfied with their surgical outcome.
4. Discussion
High success rates are reported in modern literature for studies involving hypospadias repair during childhood. Most of these studies have short follow-up times, and little information is known about these patients after sexual maturity. Hypospadias patients may anticipate ridicule by a partner and experience a poor image of their genitalia. Interestingly, older patients (≥6 years) who undergo primary repair are less satisfied and have a worse genital view than younger (<6 years) patients, and this is particularly apparent after puberty due to the changes in physical appearance with increased self awareness and sexual interest. When patients with hypospadias which was repaired in childhood grow into adulthood, they may experience delayed issues such as problems with urination, poor cosmetic appearance, psychologic issues, sexual dysfunction, and infertility [5]. Ejaculatory complaints seem to predominate in these patients [5]. Failed repairs are devastating to patients and families. Additionally, 12% of patients experience another failure after their second surgery/first revision. This includes 10% after one-stage repair and 16% after two-stage repair. The patient may need repair of complications such as urethral fistulae, meatal stenosis, urethral stricture, diverticula, persistent chordee, and a hairy urethra causing calculi, urinary retention, and urinary tract infections. With a median of five operations per patient (including patients with initial distal hypospadias), there are some patients that require frequent surgery and can experience up to 23 operations in their lifetime [6]. When complications occur, 64% are diagnosed by the first postoperative visit after tubularized incised plate (TIP) repair and 81% occur in the first year after repair. The median time for diagnosis of fistulae, meatal stenosis, strictures, and diverticula is 6 months and for glans dehiscence 2 months [7]. While it is difficult to assess the long-term success rates of hypospadias repair and revision as a young child, we know that late-stage failures and complications do occur and have been reported in the literature, with some studies suggesting 50% of patients eventually experience complications with 20% occurring more than 5 years after surgery [2].
Fistulae are one of the most frequent complications after hypospadias repair. Many of these cases can be managed by simple excision as opposed to formal urethroplasty. The same goes for urethral diverticula, which can be associated with distal obstruction. Chordee is caused by recurrent fibrosis secondary to previous repair or incomplete correction during repair as a child. This may interfere with sexual intercourse later in life. The degree of chordee will dictate the appropriate approach to correction [5]. Mild chordee (<30°) can be addressed by simple penile degloving and lysis of adhesions, Nesbit or Baskin plication procedures. More severe cases of chordee can be corrected by dermal grafting, which minimizes penile shortening at the expense of a planned two-stage repair [5]. Urethral stricture is usually diagnosed soon after the initial hypospadias repair, however, this can occur several decades later, with most of these patients between the ages of 17–40 years old [6], [7]. Stricture disease secondary to hypospadias is etiologically different from inflammatory/infectious or traumatic strictures, as the bulbospongiosum tissue is lacking, which may cause ischemia and tissue necrosis. Endoscopic internal urethrotomy does not achieve the success seen in other stricture etiologies but may be appropriate for short (<1 cm) urethral strictures seen early after hypospadias repair. When formal repair is planned, excision and primary anastomosis is appropriate for short strictures, while substitution urethroplasty is necessary for longer strictures. In the past, island skin flaps were used but are no longer the first option as hair growth within the neo-urethra causes calculus formation, urinary retention, and urinary tract infections. A patient may also present with these issues from a hairy urethra during their initial adult urologic follow-up years after hypospadias repair. Bladder mucosa was used for substitution, but patients experienced hypertrophy of mucosa when exposed to air causing meatal stenosis and a poor cosmetic appearance. Today, oral buccal mucosal using the inner cheek or lower lip as the donor site serve as the universally accepted best free graft due to ease of harvest, low donor site morbidity, and low urethroplasty complication rate. Repairs can usually be achieved in one-stage with a graft or flap placed in dorsal inlay, or ventral onlay fashion, and success rate has been found to be 86.7% (vs. 85.8% for penile skin flap substitution urethroplasty) [6]. Severe cases of scarred urethral plate or the presence of LS should be repaired in two stages after excision of all scar tissue. Penile skin coverage becomes an issue for patients with a history of multiple operations and excessive scar tissue as deficiency in available native skin increases the complexity of penile coverage. Z-plasty, rotational fasciomyocutaneous flaps, and split thickness skin grafts have been employed. The use of tissue expanders have the advantage of recruiting additional skin with similar distribution of androgen receptors, and can be helpful for coverage either alone or in combination with other techniques [8].
When patients present later in life with hypospadias complications, it is possible to achieve a good result as we were able to demonstrate. Successful revision outcomes for adolescents and adults found in the literature range from 65% to 91% [9]. Barbagli et al. [9] found a success rates of 88% in 760 patients with a failed hypospadias repair corrected in one stage, and 84% in 416 patients corrected with staged repair.
This study is limited by its retrospective manner, not having complete access to records of prior hypospadias repairs, and inability to determine late complication rates after hypospadias repair due to problems with follow-up of patients as they grow up and move away or were followed up with adult urologists for ongoing issues. However, this study has shown that having a knowledge of both pediatric disease combined with ongoing age-related issues as patients grow into adulthood can offer proper care for hypospadias patients. Efforts to improve transitional care in urology are necessary for appropriate management of these patients, and awareness of this issue is growing.
5. Conclusion
Complications of childhood hypospadias repair may present later in life as some urethroplasties deteriorate with time. Urethral strictures may develop and recurrent curvature may recur after many years. Furthermore esthetics and spraying from irregular or sub-terminal meatus acquire greater importance during adolescence. We now recommend to parents of children with repaired proximal hypospadias to come for follow-up as their child transitions to adolescence.
Conflicts of interest
The authors declare no conflict of interest.
Footnotes
Peer review under responsibility of Second Military Medical University.
References
- 1.Prat D., Natasha A., Polak A., Koulikov D., Prat O., Zilberman M. Surgical outcome of different types of primary hypospadias repair during three decades in a single center. Urology. 2012;79:1350–1353. doi: 10.1016/j.urology.2011.11.085. [DOI] [PubMed] [Google Scholar]
- 2.Lee O.T., Durbin-Johnson B., Kurzrock E.A. Predictors of secondary surgery after hypospadias repair; a population based analysis of 5000 patients. J Urol. 2013;190:251–255. doi: 10.1016/j.juro.2013.01.091. [DOI] [PubMed] [Google Scholar]
- 3.Nesbit R.M. Operation for correction of distal penile curvature with and without hypospadias. J Urol. 1967;7:720–722. doi: 10.1016/S0022-5347(17)63105-7. [DOI] [PubMed] [Google Scholar]
- 4.Baskin L.S., Erol A., Li Y.W., Cunha G.R. Anatomical studies of hypospadias. J Urol. 1998;160:108–115. doi: 10.1097/00005392-199809020-00039. [DOI] [PubMed] [Google Scholar]
- 5.Cambareri G.M., Hanna M.K. Approach to the adult hypospadias patient. In: Wood H.M., Wood D., editors. Transition and lifelong care in congenital urology, current clinical urology. Springer International Publishing; Switzerland: 2015. pp. 35–42. [Google Scholar]
- 6.Hanna M.K., Cambareri G.M. The adult hypospadias patient: technical challenges in adulthood. In: Wood H.M., Wood D., editors. Transition and lifelong care in congenital urology, current clinical urology. Springer International Publishing; Switzerland: 2015. pp. 77–96. [Google Scholar]
- 7.Snodgrass W., Villanueva C., Bush N.C. Duration of follow-up to diagnose hypospadias urethroplasty complications. J Ped Urol. 2014;10:208–211. doi: 10.1016/j.jpurol.2013.11.011. [DOI] [PubMed] [Google Scholar]
- 8.Fam M., Hanna M.K. Presentation at the society for pediatric urology, AUA meeting. San Diego. 2016. Resurfacing the penis in 215 hypospadias cripples. [Google Scholar]
- 9.Barbagli G., Perovic S., Djinovic R., Sansalone S., Lazzeri M. Retrospective descriptive analysis of 1,176 patients with failed hypospadias repair. J Urol. 2010;183:207–211. doi: 10.1016/j.juro.2009.08.153. [DOI] [PubMed] [Google Scholar]