Abstract
Purpose:
The purpose of this study was to evaluate the effect of incisal butt joint and incisal overlap design on the fracture resistance of ceramic veneers under two different loading conditions, i.e., 125° and 60° representing protrusive and intercuspal movements, respectively.
Materials and Methods:
Thirty-two maxillary central incisors were divided into two groups of sixteen specimens each and were prepared with incisal butt joint and incisal overlap design. Ceramic veneers were fabricated and cemented. Both the groups were further divided and mechanical testing to evaluate the fracture resistance were done using the universal testing machine. The values were recorded in Newton along with the assessment of the failure mode of both veneer and the tooth.
Results:
Unpaired t-test showed a significant difference (P < 0.05) with butt joint design having higher fracture resistance than palatal overlap design with the mean value of 409.50N at 60° angle and 473.37N at 125° angle. Paired t-test depicted a significant difference for both the designs at 125° than at 60° angle (P < 0.05). Chi-square analysis showed more number of intact veneers with butt joint design; however, there was no significant difference (P > 0.05). Failure mode of teeth showed more number of coronal fracture followed by cervical fracture and root fracture, but there was no significant difference between the two groups (P > 0.05).
Conclusion:
Butt joint design had higher fracture resistance than palatal overlap design. Under functional loads for both designs, fracture resistance was higher at 125° than at 60° angle.
Keywords: Ceramic veneers, incisal butt joint, incisal overlap
INTRODUCTION
The restoration of unesthetic anterior teeth has always been a challenge to a dentist. With the increased demand and patient awareness, the use of ceramic laminate veneers to restore unesthetic teeth has increased. However, the longevity of ceramic veneer has always been questioned because of the multiple stresses they are subjected to.
The various factors which could affect the long-term prognosis of ceramic veneers include careful case selection, tooth surface, preparation design, ceramic thickness, laboratory veneer fabrication, material used for cementation, and functional and parafunctional activities.
Among all the factors affecting the success rate, preparation design is one of the most controversial aspects. There are four preparation designs for veneers. Window and feather edge design does not involve incisal edge whereas butt joint and incisal overlap design involve the incisal edge.
The occlusal load is another important factor influencing the long-term success of ceramic veneers. Hence, the direction of load application during testing has a significant effect on the result.
In the past, various studies have been performed to evaluate the fracture resistance of ceramic veneer with different preparations designs, but none has correlated them with functional movements. The goal of this study was to evaluate the effect of two most preferred preparation designs, i.e., butt joint design and palatal overlap design with 2 mm incisal reduction on the fracture resistance of ceramic veneers by loading them under conditions simulating functional movements, i.e., 125° and 60° representing protrusive and intercuspal movements, respectively, and assessing their mode of failure.
MATERIALS AND METHODS
Thirty-two extracted intact maxillary central incisors with approximately similar anatomic crown length, and mesiodistal width were selected. They were mounted individually in a custom made metallic mould with self-polymerizing acrylic resin (DPI) with the long axis parallel to the center of the mould using Ney Surveyor (Unident).
The teeth were then divided into two groups as follows: Group A and Group B with sixteen teeth each for two different preparation designs, i.e., butt joint design and incisal overlap design, respectively [Figure 1]. Group A was further divided into subgroup, 1A and 2A for loading at 60° and 125° respectively. Similarly, Group B was divided into subgroup 1B and 2B for loading at 60° and 125°, respectively [Figure 2].
Figure 1.
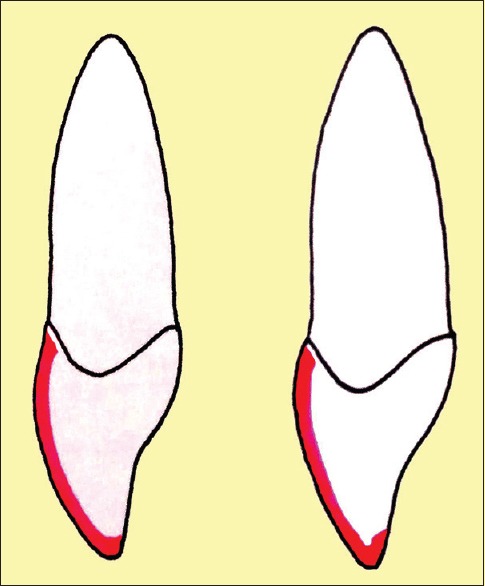
Line diagram showing butt joint and incisal overlap design
Figure 2.
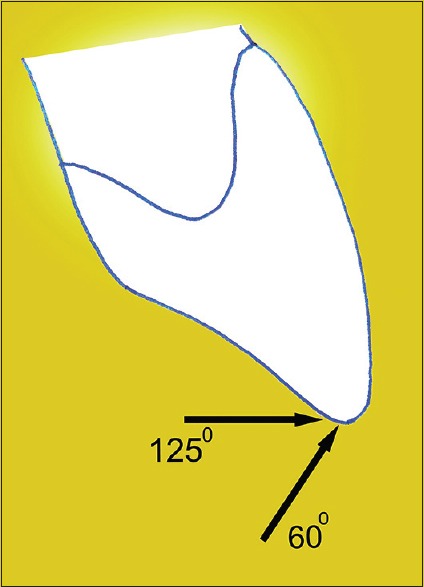
Line diagram representing loading at 60° and 125° angle
Preparation of the teeth
Reduction of 0.5 mm was done on the facial surface using the round end tapered diamond bur. It was continued into the proximal area and stopped short of breaking the contact. The incisal edge was reduced by 2 mm. Lingual reduction was done only in Group B where the lingual finish line was created 1 mm away from the incisal edge with the round-end tapered diamond bur with its end forming a slight chamfer 0.5 mm deep. The cervical preparation ended 1 mm incisal to the cement-enamel junction, and chamfer finish line was given.
Impression making
A custom tray was fabricated with perforations to make the impression of the prepared tooth. Tray adhesive (VPS tray adhesive, 3M ESPE) was applied on the tray, and then putty consistency of polyvinyl siloxane impression material (Flexceed, GC) was loaded in the custom tray, and light body impression material (Flexceed, GC) was applied on the tooth. The loaded tray was placed on the acrylic block, and a single-step impression was made. All the impressions were then poured in die stone.
Fabrication of ceramic veneer
After recovering stone dies from the impression, wax patterns (Crown wax, Renfert) were fabricated on each sample followed by investment using phosphate-bonded investment material (Interdent, Italy).
The investment ring, IPS Empress Esthetic Ingot, and IPS Empress Alox plunger were then placed inside the preheating furnace (Unident), the temperature of which was maintained at 850°C (1562 F) for 60 min.
Once the preheating cycle was completed, the hot IPS Empress Esthetic ingot and hot Alox plunger were placed into the hot investment ring. The completed investment ring was placed central to the ceramic press furnace (EP600 Combi; Ivoclar Vivadent), and the press program for the IPS Empress Esthetic was started.
On completion, the investment ring was placed on the cooling grid for approximately 60 min. After this, divestment was done followed by finishing of the copings. The thickness of the copings was kept 0.3 mm which was checked using the Iwanson gauge (GDC).
Thereafter, layering and glazing procedures were carried out using IPS Empress Esthetic layering material (Ivoclar Vivadent) and IPS Empress Universal glaze (Ivoclar Vivadent), respectively, according to the manufacturer recommended protocol in the ceramic furnace (Programat P300, Ivoclar Vivadent) to get the final thickness of 0.5 mm.
Cementation of veneer
The intaglio surface of veneers was etched with 4.5% hydrofluoric acid (IPS Ceramic Etching gel, Ivoclar Vivadent) for 60 s. They were washed thoroughly with water for 30 s and then dried using compressed air. A single component silane coupling agent (Monobond N, Ivoclar Vivadent) was applied to the etched veneer surface in a thin coat with a brush and allowed to react for 60 s.
The prepared tooth was etched using 37% phosphoric acid (Eco-Etch Etching Gel, Ivoclar Vivadent) for 15 s. It was followed by washing, drying, and application of bonding agent (Tetric N-Bond total etch dental adhesive by Ivoclar Vivadent).
Dual-/light-curing luting composite system (Variolink N, Ivoclar Vivadent) was used for the adhesive luting of ceramic. A thin layer of resin cement was applied to the center of the intaglio surface of the veneer. It was then seated on the prepared tooth with light finger pressure and then light cured from facial, palatal, and incisal surfaces for 40 s.
Mechanical testing of specimens
Fracture resistance test was performed using a universal testing machine (Autograph, Ag-Is, Shimadzu). Specimens from subgroup 1A and subgroup 1B were placed in a custom made mounting jig that allowed the specimen to be loaded at 60° to the long axis of the tooth [Figure 3].
Figure 3.
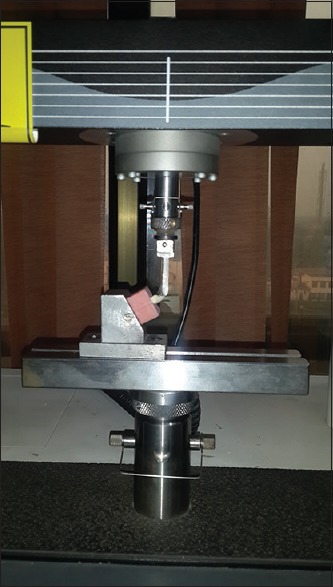
Loading of the tooth at 60° angle
Similarly, the specimens from subgroup 2A and subgroup 2B were placed in the mounting jig that allowed the specimen to be loaded at 125° to the long axis of the tooth [Figure 4].
Figure 4.
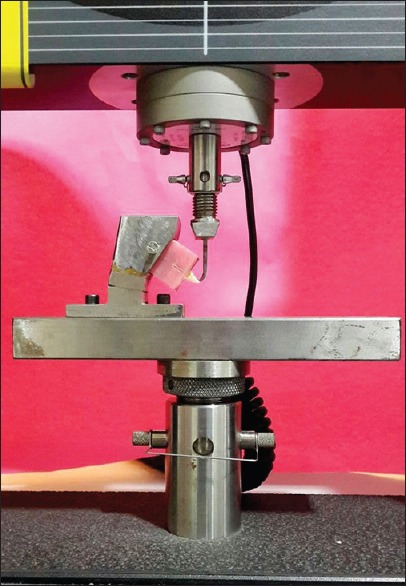
Loading of the tooth at 125° angle
Load was applied at a crosshead speed of 1.0 mm/min. Maximum load to produce fracture for each specimen was recorded in Newton. In addition, the mode of failure was macroscopically assessed for both tooth and veneer after specimen testing [Figures 5 and 6].
Figure 5.

Failure mode of veneer showing intact and fractured veneer
Figure 6.

Failure mode of tooth showing intact tooth, coronal fracture, cervical fracture, and root fracture
Statistical analysis
The data collected was subjected to unpaired or independent t-test for the comparison of mean fracture load values between the two groups and paired t-test or dependent t-test for comparison of mean values obtained from the same group. Chi-square test was used to assess the failure mode frequency.
RESULTS
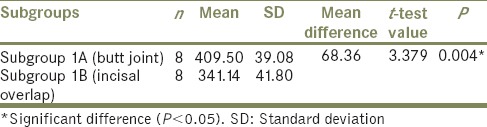
Unpaired t-test [Table 1] used to compare the mean load value at 60° angle between subgroup 1A and subgroup 1B showed a significant difference between the two subgroups. The mean fracture load value at 60° angle was found to be significantly more (P < 0.05) among butt joint design (mean = 409.50) as compared to the incisal overlap design (mean = 341.14).
Table 1.
Unpaired t-test for fracture load values (in newtons) of specimens loaded at 60° angle
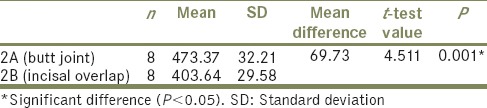
The mean load value at 125° angle [Table 2] was found to be significantly more (P < 0.05) in subgroup 2A (mean = 473.37) as compared to subgroup 2B (mean = 403.64).
Table 2.
Unpaired t-test for fracture load values (in newtons) of specimens loaded at 125° angle
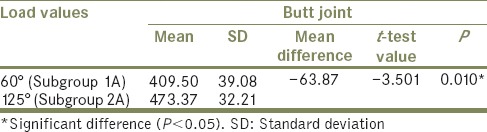
The comparison of mean load values between the specimens of butt joint design at 60° angle and at 125° angle (in Newton) was done using the Paired t-test [Table 3]. It was seen that the load values increased significantly from 60° to 125° angle.
Table 3.
Paired t-test for comparison of mean load values (in newtons) of butt joint design at 60° and 125° angle
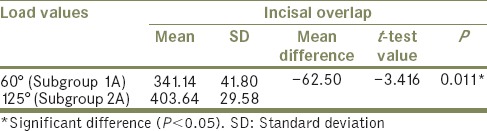
The comparison of mean load values between the specimens of incisal overlap design at 60° angle and at 125° angle (in Newton) also showed significant difference (P < 0.05) between 60° and at 125° angle [Table 4]. Thus, mean load values in both butt joint and incisal overlap design were higher at 125° (protrusive) than at 60° (intercuspal/tearing) angle.
Table 4.
Paired t-test for comparison of mean load values (in newtons) of incisal overlap design at 60° and 125° angle
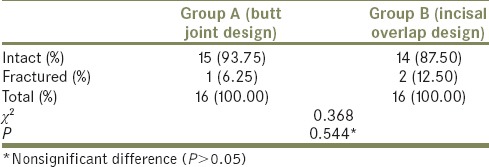
The frequency of failure mode of veneers for Group A and Group B was assessed using Chi-square test [Table 5]. The fractured veneer was found to be more among Group B (12.50%) than in Group A (6.25%). In Group A, 93.75% veneers remained intact whereas in Group B, 87.50% veneers remained intact; however, there was no significant difference (P > 0.05) between the two groups.
Table 5.
Chi-square test to compare the failure modality of veneers with butt joint and incisal overlap design
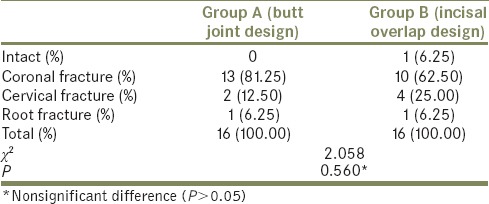
Chi-square test analysis to assess the frequency of failure mode of teeth for Group A and Group B [Table 6] showed more coronal fracture in Group A (81.25%) than in Group B (62.50%) whereas cervical fracture was found to be more in Group B (25%) than in Group A (12.50%). The frequency of root fracture was similar in both the Groups, i.e., 6.25%. Overall, there was no significant difference (P < 0.05) between the two groups.
Table 6.
Chi-square test to compare the failure modality of teeth with butt joint and incisal overlap design
DISCUSSION
Till the advent of porcelain veneers, enhancing the esthetic quality of an existing dentition with conventional prosthodontic procedures-like full crowns has either challenged the biology of the vital tooth or has compromised the esthetics. During the last decade, due to growing patient demand for esthetics and conservative restoration, use of porcelain veneer has become a widespread and successful technique for restoring discolored, worn, malformed, or fractured teeth.[1,2] During the functional jaw movements, stresses concentrate at the incisal edge, and the palatal concavity as the design of these areas do not permit solid presence of dentin but the cervical, midfacial, and cingulum regions resist the stresses better due to the solid support provided by dentin.[3] Therefore, the tooth preparation design plays a vital role in affecting the longevity of the veneer.
The present study was undertaken to evaluate the effect of butt joint design and palatal overlap design with 2 mm incisal reduction on the fracture resistance of porcelain veneers by loading them under conditions simulating functional movements, i.e., 125° and 60° representing protrusive and intercuspal movements, respectively, and assessing their mode of failure.
Maxillary central incisors were selected in the present study as they are the most commonly restored teeth with laminate veneers.[2] Even though standardization of human teeth is difficult, these teeth were preferred as artificial teeth, or bovine teeth differ from human teeth in elasticity, bonding properties, and strength.[4]
After mounting and division of the groups, standardized technique was followed to reduce the facial surface by 0.5 mm. Incisal edge for both the designs was reduced 2 mm as according to Akoǧlu and Gemalmaz[5] veneers with 2 mm incisal reduction exhibit fracture resistance similar to natural tooth. The cervical preparation for both the groups ended 1 mm incisal to the cementoenamel junction, and a chamfer finish line was given. This finish line was chosen over butt finish line as according to Al-Huwaizi[6] this finish line configuration better distributes the stresses exerted by masticatory forces.
Following fabrication and cementation of veneers, mechanical testing of all the specimens was done in the universal testing machine. As the direction of applied load during functional movements, such as chewing and swallowing, has a significant effect on the survival rate of veneer, two loading angles (60° and 125°) which represent load applied during tearing/intercuspal and protrusive position were chosen in the present study.[7,8]
A customized plunger was used to apply load at a crosshead speed of 1.0 mm/min on the incisal edge of each specimen. This loading area was chosen as our study required total force to be applied on the veneer which was necessary to evaluate the fracture resistance of veneer. Maximum load to produce fracture for each specimen was recorded in Newton along with the assessment of failure mode of both veneer and the tooth.
In comparison, failure load values of veneer restored teeth in the present study were higher than those reported by Khatib et al.,[2] and lower than those reported by Prasanth et al.[9] and Mirra and Mahalawy[10] but the results from the previous studies cannot be compared directly to the present study due to different test parameters used in these studies, such as different region and direction of applied load during the load to fracture test, use of different ceramic material for tooth restoration, and different cement for cementation of the specimens.
Results of the study showed higher fracture load value for butt joint design compared to palatal overlap design at both 60° and 125° angle. According to Castelnuovo et al.,[11] butt joint design preserves the peripheral enamel layer around all the margins, especially at the palatal surface which helps in counteracting shear stresses better, enhances tooth-ceramic bonding, and eliminates microleakage at the palatal tooth-restoration interface. With this design, the risk of fracture of thin, unsupported palatal ledges of ceramic is controlled. Palatal overlap design on the other hand creates a thin extension of ceramic in the area known to exhibit maximum tensile stress, i.e., in the palatal concavity leading to failure.[11] A study conducted by Prasanth et al.[9] also revealed that in situations which demanded incisal reduction, incisal butt joint design is the design of choice. They concluded that incisal overlap with palatal chamfer design offer neither clinical nor mechanical advantages.
Fracture load values were higher at 125° angle than at 60° angle for both butt joint design and incisal overlap design depicting that more force was required to fracture the specimen at 125° angle. According to Gibbs and et al.,[12] intercuspal position is of prime importance during functional movements such as chewing and swallowing. It is in this position that the forces generated are highest and strongest while the forces produced during eccentric contacts during functional movements are fairly low and short acting. Clinically, intercuspal forces are strong, and thus in our study, specimens fractured at low fracture load value at this angle. At 125° angle, which simulated eccentric position, i.e., protrusive position, more fracture load value was required to fracture the specimen owing to the low-force value generated clinically at this position.
The failure mode analysis showed a predominance of tooth fracture without the involvement of the ceramic veneer. A possible reason for this failure mode could be that human masticatory forces for maxillary anterior teeth have been reported to be maximum of 130 N,[13] and in the present study, load to failure was high enough to exceed the proportional limit of the tooth. In addition, there occurs difference in the elastic modulus of the teeth after extraction procedure and storage compared to in vivo conditions.[4,14] Therefore, reproducing failure modes as seen in clinical condition during functioning could be an area of improvement for the future studies. Another reason for less veneer fracture and no debonding could be related to the excellent adhesion achieved between both the resin cement-ceramic interface and the resin cement-dental substrate interface. Alghazzawi et al.[14] reported that the direction of loading, preparation design, and laminate veneer material affect the failure mode of laminate veneers. Thus, these parameters could have affected the failure mode of our study.
In the past, different loading angles have been used to test the fracture resistance of the ceramic veneers with different designs. Some authors have loaded the veneers in a direction parallel to the long axis of the tooth (0°)[9] to study the effect of vertical component of incising force but according to Castelnuovo et al.,[11] stresses that affect maxillary veneers during mastication and protrusive excursions are not directed in this direction. Others have loaded them at 135° in accordance with the orthognathic interincisal angle,[2,14] but they did not correlate them with functional movements as done in the present study. In addition, no comparison was made to assess fracture resistance at centric and eccentric forces on veneer. The comparison between these two forces is essential to select the preparation design that would best resist the forces during centric and eccentric movements of the mandible. Few authors have also loaded the veneers at 90° to the long axis of the tooth[5,11,13] to test the effect of horizontal component of force, but none has correlated them with functional movements. This study is different from the past, as in this study both centric and eccentric movements, i.e., functional movements that could result in the failure of veneers were taken into consideration. The direction of loading during in vitro studies has significant effect on the results and as the functional movement of chewing and swallowing mainly require intercuspal movement,[12] angle simulating this movement was choosen for this study and compared to the protrusive (eccentric) loading angle. Loading angles-simulating functional movements, i.e., 60° angle for intercuspal or tearing movement and 125° for protrusive movement were used by Zarone et al.[7] and Li et al.,[8] but they conducted three-dimensional finite element study on laminate veneers. In the present study, in vitro fracture load test was carried out at these two loading angles using the universal testing machine.
There are several limitations to this study. Extracted human maxillary incisors were used which vary in age and quality making standardization of the bonded interface among the specimens difficult. There was no inclusion of the factors of the periodontal ligament. The material used to embed the teeth was acrylic resin which presented different biomechanical situation from the oral cavity and did not simulate the clinical condition.
Finger pressure was used to place the restoration which was not standardized; however, this technique is clinically applicable. Thermocycling, with changing temperatures, was not performed which otherwise could have affected the fracture resistance value.
Therefore, the influence of the above-mentioned parameters should be considered in the future research as they may affect the fracture resistance values and the failure modality of the specimens.
The study could have been improved by increasing the number of specimens used for testing. This would have given more precise results. The use of artificial periodontal membrane to more closely simulate the clinical condition would be better as abutment mobility is a decisive clinical factor for the evaluation of failure load.[4]
CONCLUSION
Within the limitation of this study, it was concluded that as follows:
Butt joint design with 2 mm incisal reduction without palatal chamfer showed higher fracture resistance for ceramic veneers than palatal overlap design
Fracture resistance of ceramic veneers under functional loads for both butt joint and incisal overlap design was higher at 125° than at 60° angle
Based on the result of the present study, the most effective preparation design recommended for ceramic veneers in case incisal coverage is required is butt joint design.
Although butt joint design gave the most favorable result in terms of fracture load values, it still depends on the clinical situation of the tooth to decide the best design of preparation to be adopted.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bulbule NS, Motwani BK, Tunkiwala A, Pakhan AJ. Esthetic rehabilitation with laminate veneers. J Indian Prosthodont Soc. 2006;6:101–4. [Google Scholar]
- 2.Khatib D, Katamish H, Ibrahim AS. Fracture load of two CAD/CAM ceramic veneers with different preparation designs. Cairo Dent J. 2009;25:425–32. [Google Scholar]
- 3.Magne P, Versluis A, Douglas WH. Rationalization of incisor shape: Experimental-numerical analysis. J Prosthet Dent. 1999;81:345–55. doi: 10.1016/s0022-3913(99)70279-9. [DOI] [PubMed] [Google Scholar]
- 4.Stappert CF, Ozden U, Gerds T, Strub JR. Longevity and failure load of ceramic veneers with different preparation designs after exposure to masticatory simulation. J Prosthet Dent. 2005;94:132–9. doi: 10.1016/j.prosdent.2005.05.023. [DOI] [PubMed] [Google Scholar]
- 5.Akoǧlu B, Gemalmaz D. Fracture resistance of ceramic veneers with different preparation designs. J Prosthodont. 2011;20:380–4. doi: 10.1111/j.1532-849X.2011.00728.x. [DOI] [PubMed] [Google Scholar]
- 6.Al-Huwaizi HF. A finite element analysis of the effect of different margin designs and loading positions on stress concentration in porcelain veneers. J Coll Dent. 2005;17:8–12. [Google Scholar]
- 7.Zarone F, Apicella D, Sorrentino R, Ferro V, Aversa R, Apicella A, et al. Influence of tooth preparation design on the stress distribution in maxillary central incisors restored by means of alumina porcelain veneers: A 3D-finite element analysis. Dent Mater. 2005;21:1178–88. doi: 10.1016/j.dental.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 8.Li Z, Yang Z, Zuo L, Meng Y. A three-dimensional finite element study on anterior laminate veneers with different incisal preparations. J Prosthet Dent. 2014;112:325–33. doi: 10.1016/j.prosdent.2013.09.023. [DOI] [PubMed] [Google Scholar]
- 9.Prasanth V, Harshkumar K, Lylajam S, Chandrasekharan NK, Sreelal T. Relation between fracture load and tooth preparation of ceramic veneers - An in vitro study. Health Sci. 2013;2:1–11. [Google Scholar]
- 10.Mirra AE, Mahalawy SE. Fracture strength and microleakage of laminate veneers. Cairo Dent J. 2009;25:245–54. [Google Scholar]
- 11.Castelnuovo J, Tjan AH, Phillips K, Nicholls JI, Kois JC. Fracture load and mode of failure of ceramic veneers with different preparations. J Prosthet Dent. 2000;83:171–80. doi: 10.1016/s0022-3913(00)80009-8. [DOI] [PubMed] [Google Scholar]
- 12.Gibbs CH, Mahan PE, Lundeen HC, Brehnan K, Walsh EK, Holbrook WB, et al. Occlusal forces during chewing and swallowing as measured by sound transmission. J Prosthet Dent. 1981;46:443–9. doi: 10.1016/0022-3913(81)90455-8. [DOI] [PubMed] [Google Scholar]
- 13.Schmidt KK, Chiayabutr Y, Phillips KM, Kois JC. Influence of preparation design and existing condition of tooth structure on load to failure of ceramic laminate veneers. J Prosthet Dent. 2011;105:374–82. doi: 10.1016/S0022-3913(11)60077-2. [DOI] [PubMed] [Google Scholar]
- 14.Alghazzawi TF, Lemons J, Liu PR, Essig ME, Janowski GM. The failure load of CAD/CAM generated zirconia and glass-ceramic laminate veneers with different preparation designs. J Prosthet Dent. 2012;108:386–93. doi: 10.1016/S0022-3913(12)60198-X. [DOI] [PubMed] [Google Scholar]


