Abstract
Aim and Objectives:
The aim of the study was to assess the knowledge of dental laboratory technicians regarding infection control and modes of infection control employed by them.
Settings and Design:
A self-assessment questionnaire-based survey was carried out among dental technicians to assess the knowledge and practice of infection control in dental laboratories.
Materials and Methods:
Survey instrument containing 16 questions were randomly distributed to 70 dental colleges of North India regarding knowledge of infection control methods and infection control practised in laboratories. Data were collected and analyzed.
Results:
The response showed that 30.76% of dental technicians receive 30–50 or more than 50 impressions in a week. About 96.15% of the technicians used a plastic bag to carry impressions. Twenty-five percent of the dental technicians were aware of infection control protocol. Fifty-five percent of the technicians received impressions while wearing gloves and 61.53% of the institutes had a separate receiving area. Nearly 71.15% of the technicians communicate with the doctor regarding the disinfection of impression received in the laboratory. Almost 30.76% of the dental technicians disinfect all the impressions and 67.30% technicians use immersion for disinfection of impressions. Only 38.46% responded that they immerse impressions for 10 min for disinfection. About 73.07% use gloves, 90.38% use mouth masks, 57.69% wear eye shields, and 88.46% wear aprons while working. Nearly 78.84% of the technicians received vaccination against hepatitis B virus. Almost 69.23% of the technicians change pumice slurry after regular intervals, and 75% do not add any disinfectant. Nearly 59.61% of technicians disinfect the prostheses before sending it to the clinic, and 42.30% disinfect them by immersion technique. About disposal of waste, 80.76% said that they dispose the waste properly.
Conclusion:
To summarize, most of the technicians were not aware of basic infection control protocols.
Keywords: Dental institutes, infection control, laboratory technicians, survey
INTRODUCTION
Infection control is an imperative issue in the dental practice. It is reported that 1 ml of saliva sample from the mouth of an average healthy person contains about 750 million microorganisms; therefore, it is one of the most discussed topics in dentistry and has become an integral part of the practice that dental health workers no longer question its necessity.[1]
Dentistry is predominantly a field of surgery, involving exposure to saliva/blood and other potentially infectious materials, and therefore, requires a high standard of infection control and safety in controlling cross-contamination and occupational exposures to blood- and saliva-borne diseases. Dental care professionals are at an increased risk of cross infections while treating patients. However, in contrast to the dental treatment rooms and surgical operatories where infection control measures are rigidly recommended, the dental laboratories are often overlooked. This constitutes a threat to the safety of dental technicians, who may acquire pathogenic microorganisms from contaminated impressions, prosthesis, and/or by improper handling of clinical materials after arrival at the dental laboratory.
The principal route of transmission of infection from the patient to the dental technician is through these materials as they are in direct contact with patient's mouth, saliva, and possibly blood. It has been documented that dental personnel have a 5–10-fold chance of acquiring hepatitis B infection than the general population.[2] In 1987, the Centers for Disease Control and Prevention (CDC) developed universal precautions to help protect both health-care workers (HCWs) and patients from infection with blood-borne pathogens in health-care settings. Similarly, to address the cross-contamination concerns, the American Dental Association (ADA) also issued guidelines for disinfection in 1988, 1991, and 1996.
Although a lot of guidelines have been issued and revised from time to time, regrettably hygiene in many dental laboratories continues to be substandard which suggests the need for more stringent control measures. It is important to evaluate the knowledge of dental technicians regarding the disinfection and personal protection along with their motivation for the implementation of same. Therefore, this study was aimed to assess the knowledge, attitude, and behavior of dental technicians toward infection control and infection control practised by them in dental laboratories in various dental colleges of North India.
MATERIALS AND METHODS
Infection control forms an important part of practice for all health-care professions and remains one of the most cost-beneficial interventions available. The British dental association stated that “infection control is a core element of dental practice,”[3] and these recommendations are applicable to all levels and fields of dentistry for all persons involved in providing dental care directly or indirectly including dentists, dental assistants, dental nurses, dental technicians, students, trainees, and volunteers.[4]
Study design
This study was conducted as a descriptive survey of dental laboratories in dental colleges of North India after obtaining clearance from the ethical committee. Informed consent was obtained from technicians before the commencement of survey. Data were collected during August 2012 to November 2012. The states included in the study were Jammu and Kashmir, Himachal Pradesh, Punjab, Haryana, Chandigarh, Delhi and NCR, and a part of Rajasthan and Uttar Pradesh.
Sample size calculation
Sample size is calculated by formula n = Z2 P (1 − P)/d2
Where Z is 19.6 at 95% confidence interval and P= 32.0% awareness according to our pilot study and precision of our study was 9%.
Questionnaire
A self-administered questionnaire containing seven closed-ended and nine open-ended questions [Table 1] had been designed. The questionnaire asked respondents regarding their attitude and knowledge of infection control measures: use of gloves, protective eyeglasses, receiving of impression in laboratory, disinfection of impression, etc. The survey instrument had been pilot studied through questionnaire with three dental technicians and 18 postgraduate students from the Department of Prosthodontics. Responses from the pilot study were analyzed to assess the clarity and relevance of questions. Necessary modifications were carried out on the feedback from pilot test participants. The Cronbach's alpha was calculated using the SPSS (version 16) for windows (SPSS Inc., Chicago, IL, USA) for the validation of the questionnaire. The Cronbach's alpha value was found to be 0.80 which was satisfactory.
Table 1.
Questionnaire for response to infection control
The questionnaire was randomly distributed to laboratory technicians in 70 Dental Institutes of North India. Participants were given no time limit to fill questionnaire (in days) so as to reduce induced error.
RESULTS
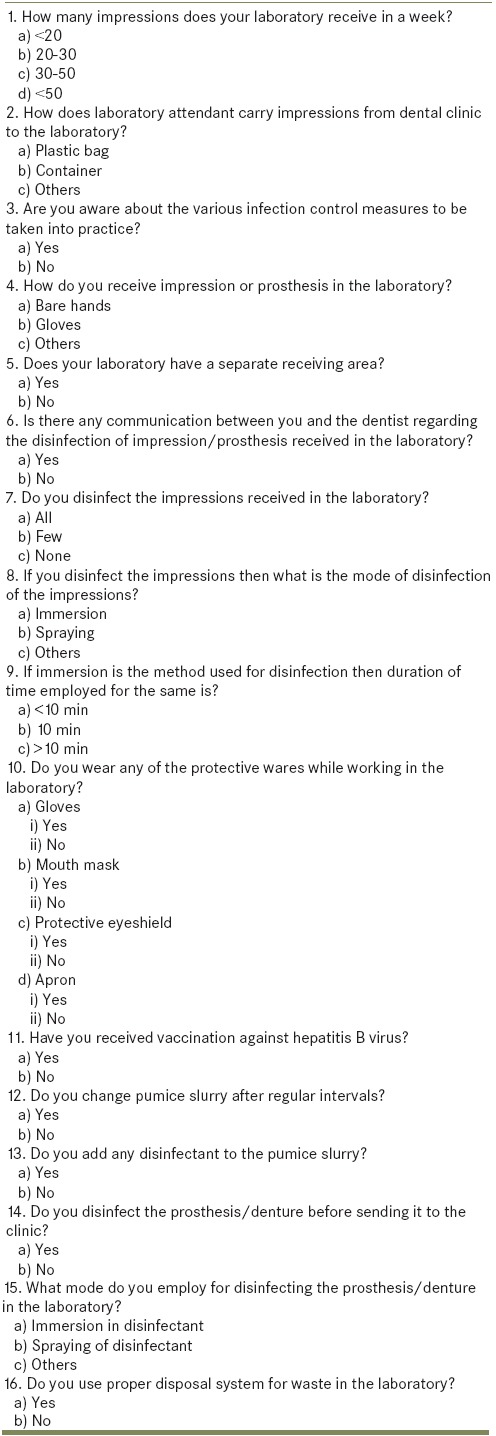
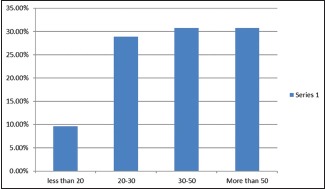
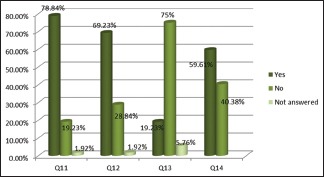
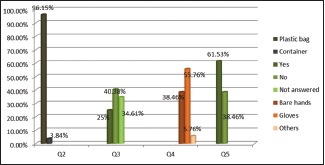
Out of 70 dental institutes contacted, 52 responded to the survey and 2 technicians from each institute were participated. The operatory area was properly ventilated and adequate water drainage in the laboratories. The obtained data were analyzed, and results have been presented with graphical presentation for ease of understanding [Graphs 1–5]. The response showed that most of the dental technicians receive 30–50 (30.76%) or more than 50 impressions (30.76%) in a week [Graph 1]. Most of the laboratory attendants carry impressions in plastic bag (96.15%) to the laboratory [Graph 2]. Only 25% of the dental technicians said that they are aware of infection control protocol [Graph 2]. Fifty-five percent of the technicians told that they receive impressions while wearing gloves [Graph 2]. About 61.53% of the institutes had a separate receiving area in the laboratories [Graph 2]. Nearly 71.15% of the technicians said that they communicate with the doctor regarding the disinfection of impression/prosthesis received in the laboratory [Graph 3]. Only 30.76% of the dental technicians responded that they disinfect all the impressions. Immersion was the method used for disinfection of impressions by the maximum technicians (67.30%) [Graph 3]. Most of them (38.46%) responded that they immerse impressions for 10 min for disinfection [Graph 3]. Regarding protective wears 73.07% said that they use gloves, 90.38% said that they use mouth masks, 57.69% told that they wear eye shields, and 88.46% said that they wear aprons while working [Graph 4]. Most of the technicians received vaccination against hepatitis B virus (HBV) (78.84%) [Graph 5]. Majority of the technicians (69.23%) stated that they change pumice slurry after regular intervals and 75% said that they do not add any disinfectant [Graph 5]. About 59.61% of technicians said that they disinfect the prosthesis/denture before sending it to the clinic [Graph 5]. Most of them (42.30%) disinfect them by immersion technique [Graph 6]. About disposal of waste, 80.76% said that they dispose the waste properly [Graph 6].
Graph 1.
Response to the Question 1: How many impressions does your laboratory receive in a week?
Graph 5.
Response to Question 11: Have you received vaccination against hepatitis B virus? Question 12: Do you change pumice slurry after regular intervals? Question 13: Do you add any disinfectant to the pumice slurry? Question 14: Do you disinfect the prosthesis/denture before sending it to the clinic?
Graph 2.
Response to Question 2: How does laboratory attendant carry impressions from dental clinic to the laboratory? Question 3: Are you aware about the various infection control measures to be taken into practice? Question 4: How do you receive impression or prosthesis in the laboratory? Question 5: Does your laboratory have a separate receiving area?
Graph 3.
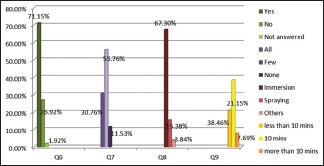
Response to Question 6: Is there any communication between you and the dentist regarding the disinfection of impression/prosthesis received in the laboratory? Question 7: Do you disinfect the impressions received in the laboratory? Question 8: If you disinfect the impressions then what is the mode of disinfection of the impressions? Question 9: If immersion is the method used for disinfection then the duration of time employed for the same is?
Graph 4.
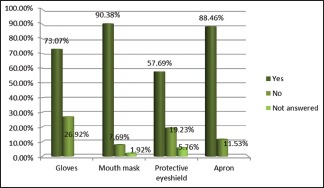
Response to Question 10: Regarding the use of protective wares while working in the laboratory?
Graph 6.
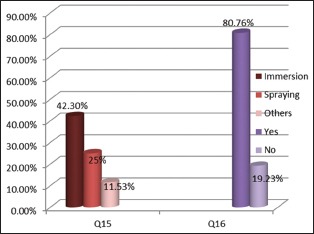
Response to Question 15: What mode do you employ for disinfecting the prosthesis/denture in the laboratory? Question 16: Do you use proper disposal system for waste in the laboratory?
DISCUSSION
In prosthodontics, objects potentially contaminated with pathogenic microorganisms are transported between dental laboratory and the dental clinic. A number of bacteria, fungi, and viruses present in the prosthodontic environment have been linked to debilitating and life-threatening diseases. Although the goals are oriented toward disease prevention, reduction in potential risks of disease spread is only practical.[4] On literature review, the prevalence of occupational hazard in dental technicians is found to be 15.4%.[5]
In this study, observation of various infection control measures in laboratories of Dental Institutes of North India has been done. On enquiring on the method of carrying an impression from the clinics to the laboratory by the attendant, 96.15% of the dental technicians told that they received impressions in plastic bags while 3.84% said that they received it in a container. The Occupational Safety and Health Administration (OSHA) has given specifications for handling and transporting specimens of blood contaminated or other potentially infectious materials. According to it, “potentially infectious materials shall be placed in a container which prevents leakage. Labeling or color coding is required when such specimens/containers leave the facility.”
Regarding awareness about the various infection control measures to be taken into practice, only 25% of technicians said that they were aware of it. Al-Kheraif and Mobarak[6] did a survey on infection control practice in private dental laboratories in Riyadh and found that 87.5% of the respondents were unaware and did not follow any infection control procedure. They suggested that it should be mandatory to provide formal infection control courses for the dental technicians in the dental institutes either as a part of their training or before the appointment in the institutes. Furthermore, they should be motivated to follow a single set of standard precautions assuming every patient as a source of infection.
About 55.76% of the dental technicians reported that they receive impressions while wearing gloves. Bhat et al.[7] assessed that barrier system must be followed routinely in the laboratory. Disposable gloves should always be used. The gloves should be disposed off appropriately after each use. Hands should be washed before and after removing gloves.
On enquiring on the separate receiving area for impression/prostheses, 61.53% of the dental technician responded that they have separate receiving areas in their laboratories. Kaul et al.,[8] in their study, evaluated that use of strict zoning areas within the laboratory is essential. Regarding communication between technicians and the doctor about the disinfection of impression/prosthesis received in the laboratory, 71.15% of the dental technicians answered that they communicate with doctors. Kohli and Puttaiah[4] in their book on infection control in dentistry mentioned that there should be adequate communications between the dental laboratory and the dentist about decontamination of items that have been shipped (must have a label stating whether it was disinfected and with which disinfectant).
About the disinfection of the impressions received in the laboratory, only 30.76% of dental technicians responded that they disinfect all the impressions they receive from clinics. The results showed that there is a lack of commitment of technicians toward disinfection of impressions. Marya et al.[9] said that an impression, if not disinfected, can cross contaminate the entire laboratory area, allowing microorganisms to travel back and forth from the laboratory to the clinical area. Thus, it is essential for the laboratory technicians to disinfect all the impressions just to assure their own protection from infection.
Regarding the method used for the disinfection of impressions, 67.30% of dental technicians answered immersion as the method of choice while 15.38% answered spraying. Ngpal and Chaudhary[10] and Kaul et al.[8] stated that immersion method is preferred over the spraying as it assures constant contact of disinfectant with all surfaces of the impression. They advocated disinfection of all the impressions with an acceptable disinfectant either with spraying or immersion.
Nearly 38.46% of dental technicians answered that they immerse impressions for 10 min, 21.15% responded that they immerse impressions for <10 min while 7.69% answered that they immerse impressions for more than 10 min in a disinfectant. The results revealed that technicians were not aware of the actual time duration for which disinfection has to be done and they were not following any standard protocol of disinfecting impressions. Kugel et al.[11] said that most of dentists and laboratories disinfect impressions for longer than recommended durations. The ideal time duration for disinfection of the impression was 10 min. The ADA recommended the use of ADA accepted disinfectant that requires no more than 30 min for disinfection.
Regarding the use of personal protective equipment (PPE) while working in the laboratory, 73.07% of dental technicians said that they wear gloves while 90.38% of dental technicians answered that they wear mouth masks. Furthermore, 88.46% of the dental technicians told that they wear aprons, and only 59.61% of the dental technicians answered that they use eye shield while working in laboratory. Primary PPE (protective eyewear and face shields) used in oral health-care settings includes gloves, surgical masks, protective eyewear, face shields, and protective clothing. All PPEs should be removed before dental health-care providers leave patient-care area. Reusable PPE should be cleaned with soap and water when visibly soiled, according to the manufacturer's directions. Wearing gloves, surgical masks, protective eyewear, and protective clothing in specified circumstances to reduce the risk of exposures to saliva/blood borne pathogens were mandated by OSHA.[12]
On enquiring about whether they have received vaccination against HBV, 78.84% of dental technicians said that they have received it. The immunization against HBV forms the main disciple against infection control and personal protection. Almost all of the studies regarding infection control advocated the immunization of dentist as well as his team including technicians. In 1987, the Center for Disease Control and Prevention[13] developed universal precautions to help protect both HCWs and patients from infection with blood-borne pathogens in health-care settings.
Regarding change of pumice slurry after regular intervals, 69.23% of dental technicians said that they change pumice slurry on regular intervals in their dental laboratories. The US Army Dental Care System[14] said that pumice solution should be made by suspending the pumice in tincture of green soap or other surfactant and adding an effective disinfectant solution to the mix. The pumice must be changed daily, and the machines must be disinfected on a regular basis.
Regarding addition of disinfectant to the pumice slurry, only 19.23% of dental technicians said that they add disinfectant to it. Firoozeh et al.[15] said that pumice used in prostheses polishing could be a potential source of contamination to dental laboratory technicians when considering the wide variety of microorganisms in saliva and blood of patients. They promoted the use of sterile pumice or association of disinfectants to the pumice (0.2% chlorhexidine gluconate or 5% hypochlorite sodium). They also recommend a daily change of polishing paste.
Regarding disinfection of prostheses/denture before sending them to the clinic, 59.61% of dental technicians answered that they disinfect prostheses/denture before sending it to clinics. Runnells[16] in his overview of infection control in dental practice stated that all prostheses should be carefully rinsed under running water, cleaned off debris, and disinfected in an Environmental Protection Agency registered and ADA accepted disinfectant, and only then, it should be sent in a properly sealed and labelled plastic bag from laboratory to the clinics.
On enquiring on mode of employment for disinfecting the prostheses/denture in the laboratory, 42.30% of dental technicians said that they use immersion as a method of choice while 25% answered spraying method. Regarding disposal system for waste in the laboratory, 80.76% of dental technicians answered that they use proper waste disposal system in laboratories. Kohli and Puttaiah[4] in their text book on infection control mentioned that, while protecting the patient and the care provider, a lot of medical waste is generated. With respect to dentistry, waste can be classified as - regulated waste and nonregulated waste. The clinics should have a contract with a professional waste management company that regularly removes the hazardous waste from the clinic. Chemical wastes should not be poured down the drain as they pose a grave environmental hazard.
Further studies are required covering maximum laboratories of the dental institutes in India, dental laboratories in private sectors as well as laboratories associated with dental clinics to get a better picture regarding various infection control measures taken by dental laboratories so that the area or aspect most ignored can be fetched and worked on.
CONCLUSION
Within the limitations of the current study, we concluded that most of the dental technicians were not aware of the basic infection control protocols. A single set of standard precautions in accordance with the CDC and OSHA guidelines should be mandatory for all the dental laboratories. It is therefore essential that the foregoing outline of a workable laboratory infection control policy should be implemented.
Limitations of study
The questionnaire does not include questions regarding disinfection of articulator, facebow, and trimmer which are used in dental laboratories. Further study should be planned including more objective questions pertaining to exact knowledge of technicians.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Notle WA. Oral Microbiology with Basic Microbiology and Immunology. 4th ed. CV mosby, St Louis, Missouri: The CV Mosby Company; 1982. p. 55. [Google Scholar]
- 2.Miller CH. Infection control. Dent Clin North Am. 1996;40:437–56. [PubMed] [Google Scholar]
- 3.Kahn RC, Lancaster MV, Kate W., Jr The microbiologic cross-contamination of dental prostheses. J Prosthet Dent. 1982;47:556–9. doi: 10.1016/0022-3913(82)90309-2. [DOI] [PubMed] [Google Scholar]
- 4.Kohli A, Puttaiah R. Infection Control & Occupational Safety Recommendations for Oral Health Professionals. 1st ed. New Delhi: Dental Council of India; 2007. pp. 2–14. [Google Scholar]
- 5.Choel L, Grocgogeat B, Bourgeois D, Descotes J. Occupational toxic risks in dental laboratory technicians. J Environ Med. 1999;1:307–14. [Google Scholar]
- 6.Al-Kheraif AA, Mobarak FA. Infection control practice in private dental laboratories in Riyadh. Saudi Dent J. 2008;20:162–9. [Google Scholar]
- 7.Bhat VS, Shetty MS, Shenoy KK. Infection control in the prosthodontic laboratory. J Indian Prosthodont Soc. 2007;7:62–5. [Google Scholar]
- 8.Kaul R, Purra AR, Farooq R, Khatteb SU, Ahmad F, Parvez PA. Infection control in dental laboratories - A review. Int J Clin Cases Investig. 2012;4:19–32. [Google Scholar]
- 9.Marya CM, Shukla P, Dahiya V, Jnaneswar A. Current status of disinfection of dental impressions in Indian dental colleges: A cause of concern. J Infect Dev Ctries. 2011;5:776–80. doi: 10.3855/jidc.1652. [DOI] [PubMed] [Google Scholar]
- 10.Ngpal A, Chaudhary V. Infection control in prosthodontics. Indian J Dent Sci. 2010;2:5–10. [Google Scholar]
- 11.Kugel G, Perry RD, Ferrari M, Lalicata P. Disinfection and communication practices: A survey of U.S. dental laboratories. J Am Dent Assoc. 2000;131:786–92. doi: 10.14219/jada.archive.2000.0278. [DOI] [PubMed] [Google Scholar]
- 12.Washington, DC: OSHA Instruction CPL2-244B; 1990. Occupational Safety and Health Administration. Enforcement of Procedures for Occupational Exposure to HBV & HIV. [Google Scholar]
- 13.Centers for Disease Control. Guidelines for Infection Control in Dental Health Care Settings-2003. [Last accessed on 2017 Jul 19];MMWR. 2003 52(RR-17):1–66. 2003. Available from: http://www.cdc.gov/mmwr/PDF/rr/rr5217.pdf . [Google Scholar]
- 14.Washington, DC: Technical Bulletin; 1995. Headquarters Department of the Army. Disinfection and Sterilization of Dental Instruments and Materials; pp. 1–12. [Google Scholar]
- 15.Firoozeh F, Zibaei M, Zendedel A, Rashidipour H, Kamran A. Microbial contamination of pumice used in dental laboratories. Healthc Low Resour Settings. 2013;1:18–21. [Google Scholar]
- 16.Runnells RR. An overview of infection control in dental practice. J Prosthet Dent. 1988;59:625–9. doi: 10.1016/0022-3913(88)90083-2. [DOI] [PubMed] [Google Scholar]


