Abstract
Purpose:
The purpose of this within-subject crossover clinical trial was to compare and evaluate the chewing efficiency, masticatory bite force, and patient satisfaction with conventional dentures and two implant-retained mandible overdentures after 4 weeks of usage.
Method:
This within-subject crossover clinical trial was carried out in the Department of Prosthodontics in K.D Dental College and Hospital. A total 15 patients were selected for the study. To report the changes in chewing efficiency by chewing 6gms of peanuts with 40 chewing strokes and comparing the particle size of the chewed material between two implant retained mandibular overdenture with that of conventional denture using micro vu excel gantry type visual measurement machine. To report changes in masticatory bite force after transition of conventional complete denture patient to implant retained overdenture after using the prosthesis for four weeks each and recorded by digital transducer. To assess the patient satisfaction after transition of conventional complete denture patient to implant retained mandibular overdenture with help of OHIP edent patient satisfaction questionnaire.
Results:
The chewing efficiency for implant retained overdenture increased significantly than that of conventional denture. The particle size decreased to 76.34% for implant supported overdenture than that of conventional denture. The chewing strokes required by conventional denture was 69 strokes and that by implant supported overdenture which was 40 strokes to get the same mean particle size. The patients satisfaction after receiving the implant retained overdenture was significantly higher than that of complete denture.
Conclusion:
The provision of two mandibular implants significantly improves measures of oral function and better quality of life for edentulous patients.
Keywords: Chewing efficiency, implant overdentures, masticatory bite force, patient satisfaction
INTRODUCTION
Complete edentulism is associated with decreased masticatory function, as well as unfavorable esthetics due to loss of support for the facial musculature, decreased vertical dimension, and speech impairment. The conventional method for treating edentulism patients is to rehabilitate them with conventional complete dentures. However, denture must be adjusted overtime to compensate for progressive tissue changes associated with denture wearing. Patients who wear conventional dentures often complain about the instability of the prosthesis, particularly the mandibular denture. Denture instability leads to a feeling of insecurity, inefficient mastication, and overall dissatisfaction with the prosthesis. Advances in implant dentistry have allowed a shift from conventional complete denture to implant-supported overdenture for oral rehabilitation of edentulism patients.[1] The McGill consensus statement in 2002 and some other studies state that the mandibular implant overdentures should be the first treatment of choice for edentulous patients. Implant-retained overdentures have many advantages over conventional complete dentures as chewing efficiency, masticatory bite force, and general patient satisfaction improves tremendously.[2]
Chewing replaces the body's nutrients, thereby facilitating the maintenance of the body composition. Mastication is the first step and consists of a rhythmic separation and apposition of the jaws and involves biophysical and biochemical processes. Although data on the importance of chewing on various stages of digestion are limited, it has been concluded that the chewing efficiency as low as 25% is adequate for complete digestion of food. Patients do not, however, compensate for a smaller number of teeth by more prolonged or a larger number of chewing strokes; they merely swallow large food particles. Nevertheless, loss of teeth can lead to a diminished chewing efficiency, and there is evidence of restricted dietary choice with resultant systemic effects. Clinical experience suggests a relationship between the quality of prosthetic service and denture wearers chewing performance. Dentures move during mastication because of dislodging forces of the surrounding musculature. These movements manifest themselves as displacing, lifting, sliding, tilting, or rotating of the prosthesis. Mandibular implant overdenture helps in better stability, support, and retention which reduces the denture movements and furthermore helps in achieving better chewing efficiency and masticatory bite force. The masticatory performance is reduced to one-fourth to one seventh of the performance of dentate subjects, depending on age and type of food. Thus, denture wearers need seven times more masticatory cycles to reduce food to half of its original size.[3,4] Reported masticatory bite forces using complete denture is much smaller than those produced by natural dentition which is of the order of 200 N. Although maximum bite forces of 60–80 N have been reported for complete dentures and 150–170 N for implant-supported overdenture.[4,5]
In the current study, the image analysis of the finest chewed particles and the micro measurements were accomplished by Micro Vu excel gantry type visual measurement machine (VMM). The grid system of the machine resulted in achieving a very high accuracy ranging from 2–5 μ. The simplicity of the design of the machine and the Inspec software (Micro vu) made it highly reliable, efficient, easy to use, and inspect even the finest of particle sizes for micro measurements. The transducer bite force device was used for the measurements of masticatory bite force and Oral Health impact profile for Edentulous Patient (OHIP-edent) index for the evaluation of patient satisfaction.
The purpose of this within-subject crossover clinical trial was to compare and evaluate the chewing efficiency, masticatory bite force, and patient satisfaction with conventional dentures and two implant-retained mandible overdentures after 4 weeks of usage.
MATERIALS AND METHODS
This within-subject crossover clinical trial was carried out in the Department of prosthodontics in K.D dental College and hospital. A total 15 patients were selected for the study. Three patients were excluded from the study as they did not report for data collection [Figure 1 and Schematic Chart 1].
Figure 1.
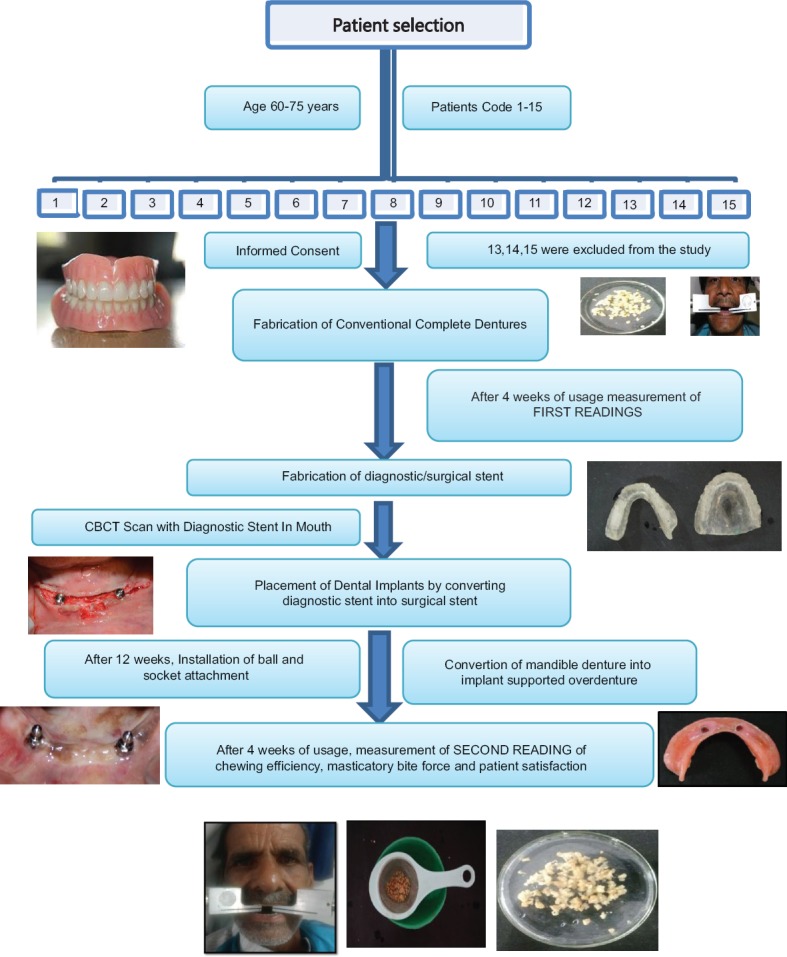
Schematic presentation of methodology
Schematic Chart 1.
Inclusion and exclusion criteria for subjects
Fabrication of conventional complete denture
A set of maxillary and mandibular complete dentures were made following the standard protocols. The retention, stability, esthetics, phonetics, jaw relation, and occlusion were confirmed. Patients were recalled after 24 h for postinsertion checkup. Patients were recalled after 4 weeks for measurement of chewing efficiency, masticatory bite force, and to record patient satisfaction in the questionnaire.
Fabrication of surgical stent
Fabrication of surgical stent involved duplication of existing mandibular complete denture. This duplicated mandibular denture was used as a radiographic stent during cone beam computed tomography (CBCT) scan. The conventional denture was duplicated in duplicating flask. The 2 mm diameter metal balls were placed at the desired location of each implant fixture at canine region (BandD region). The negative impression of the dentures in duplicating flask was filled with clear acrylic heat cure resin. The information was transferred to the stent, thereby replacing ball markers with cannula to orient the pilot drill, thus converting the diagnostic stent to surgical stent.
Placement of dental implants
The implant type chosen was Adin implant grade V titanium with rough microtextured surface treatment and single-threaded tapering design. Patients were advised to use the complete dentures for 12 weeks till the time of loading. Patients were referred for CBCT, and routine blood investigations were prescribed. According to the Centers for Disease Control and Prevention guidelines, single dose of prophylactic antibiotic was given orally 1 h before the surgery. Local infiltration was administered with lignocaine 2% with 1:100,000 adrenalin.
A crestal incision was made, and full thickness mucoperiosteal flap was raised both on the labial and lingual aspects to enable adequate visualization of the lingual aspect of the mandible and to evenly divide the available keratinized tissue. The surgical stent was placed in the patient's mouth, and pilot drill was used at osteotomy site (BandD region) to mark a purchase point to avoid slippage of the surgical drills. The paralleling pins were placed to assess the angulations of the osteotomy. These paralleling pins were then removed, and progressive drills were used in order, and osteotomy was completed. The implant of the selected diameter was inserted into the osteotomy site using the torque wrench. A cover screw was then tightened on the implants, and flaps were approximated with interrupted sutures. The patient was recalled after 1 week for removal the of sutures and postoperative checkup.
Installation of ball and socket attachments
The patients were recalled for second-stage surgery after 12 weeks of implant placement. The site was reopened at the bilateral canine region, and healing cap was placed. After 1 week, the healing caps were removed, and the ball and socket attachments were placed and tightened to 35–40 Ncm. Nylon caps and metal housing were incorporated at the predetermined site on intaglio surface of mandibular denture by standard technique. Patients were recalled after 4 weeks of usage of mandibular overdenture for the evaluation of chewing efficiency, masticatory bite force, and evaluating the patient satisfaction questionnaire with the implant-retained overdenture.
Measurement of chewing efficiency
The method for the evaluation of chewing efficiency was same for conventional complete denture and implant-retained overdenture. The test food selected for the study was peanuts because it is homogenous, inexpensive, and it also offers moderate resistance to chewing.[6,7] The chewing efficiency was evaluated in a series of chewing tests. During each test, the patient was requested to chew 6 g of peanuts with forty chewing strokes, trying not to swallow any fragments. The patient was then asked to spit out the remaining fragments in a bowl covered with special sieve. Subsequently, the patients were asked to remove their dentures in a bowl. The food particles sticking to the dentures were rinsed off with water and collected in the same bowl. The particles remaining in the oral cavity were collected, and the patients were asked to rinse their mouth with water in the same bowl. All the chewed materials were then carefully collected in the sieve and transferred into petridish which was kept in the incubator at 37°C temperature for 48 h. The chewed material in petridish was placed on the vibration table, running for 60 s with the maximal vibration amplitude. The clusters got sorted in vibrator, and the finest particle size got dispersed separately in the petridish.
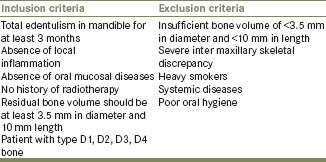
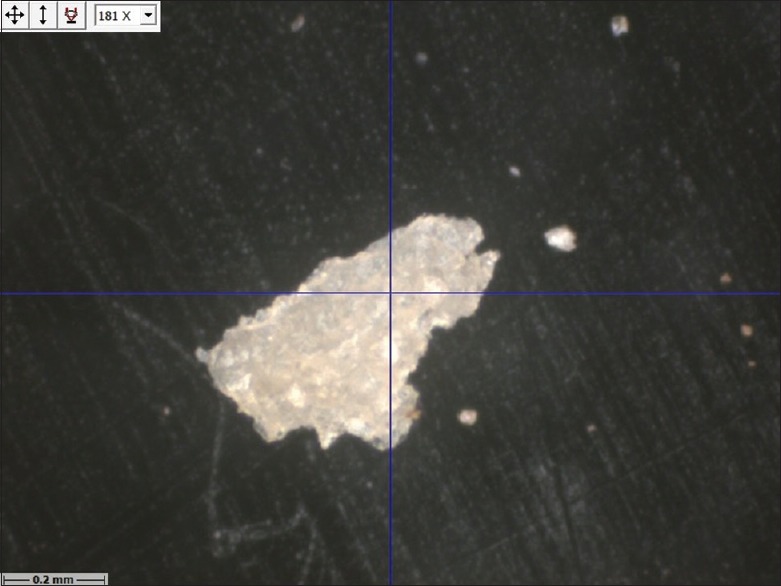
The excel type gantry VMM was employed for micro measurements of finest chewed particles as it provides a unique method of visual measurement. Ten finest chewed particles of each patient from conventional complete denture and implant-retained overdenture were selected for examination. The finest particles were selected by efficient grid system of VMM machine which measures up to 2–4 μm. Chewed material was placed on the bed/stage. The standard macro ring light was used for illumination; the axial light was used to focus the particles and profile light available below the stage was used to inspect the particle sizes and finest particles visible were selected and inspected on the InSpec software.
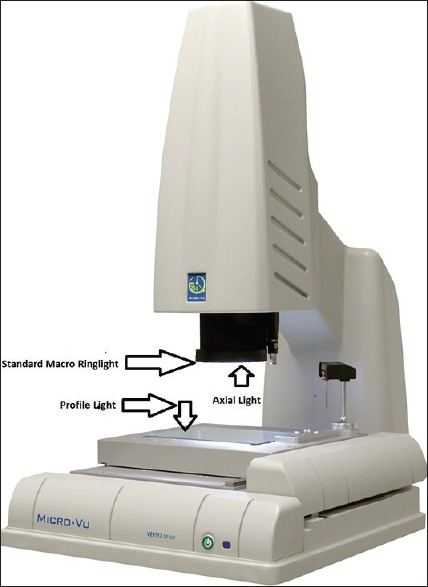
Once, single particle was selected on InSpec software, and the image analysis was done in x, y, and z direction. Two readings were recorded of the particle in vertical and horizontal axis. From top to bottom; the measurement was marked as L (length) and from the right to left; it was marked as W (width). The readings were recorded in micrometers. These measurements (L × W) were multiplied for each finest chewed particle and an average value of ten particles was taken for each patient for conventional denture and implant-retained overdenture. The chewing efficiency was recorded after 4 weeks of usage conventional complete dentures and after 4 weeks of usage of implant-retained overdentures, respectively [Figures 2–15 and Schematic Chart 2].
Figure 2.

Peanuts 6 g on weighing scale
Figure 15.
Micro-Vu: Three types of lights
Schematic Chart 2.
Chewed particle dimensions for conventional denture and implant-supported overdenture for each patient
Figure 3.

Peanuts before chewing
Figure 4.

Rinsed chew material in bowl with dentures
Figure 5.

Chewed material collected in sieves
Figure 6.

Collection of chew material in petridish
Figure 7.

Chewed material (conventional denture)
Figure 8.
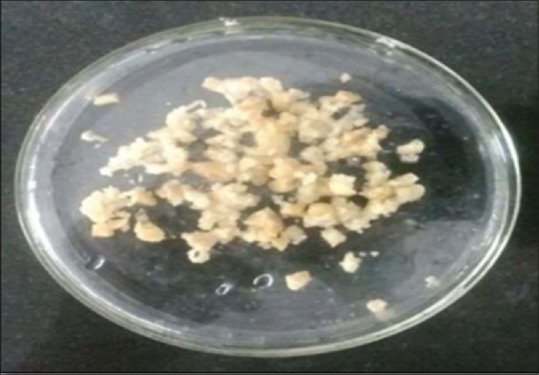
Chewed material (overdenture)
Figure 9.
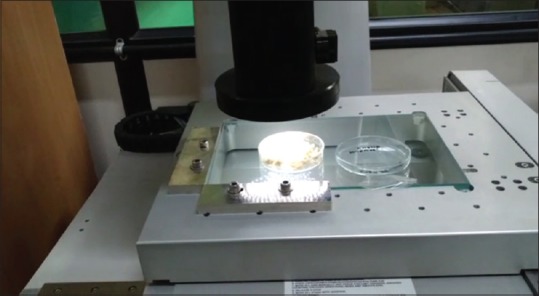
Inspection of finest chew particle size under Micro Vu visual measurement machine
Figure 10.
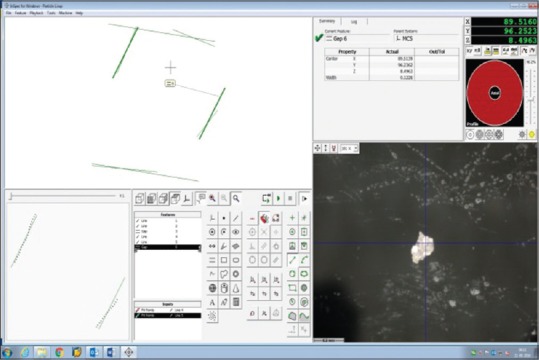
Measurement of finest chew particles with InSpec software
Figure 11.
Particle size after chewing with conventional denture
Figure 12.
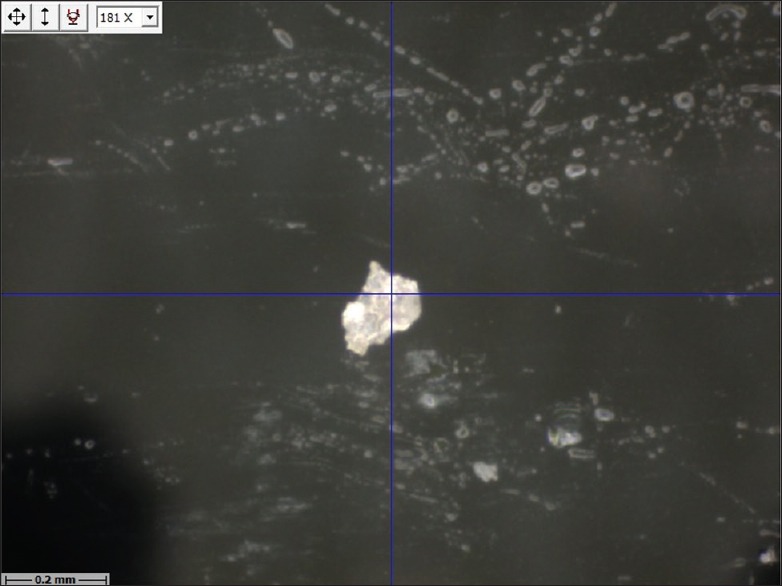
Particle size after chewing with implant supported denture
Figure 13.

Micro-Vu: Excel gantry type visual measurement machine
Figure 14.

Macro ring light
Measurement of masticatory bite force
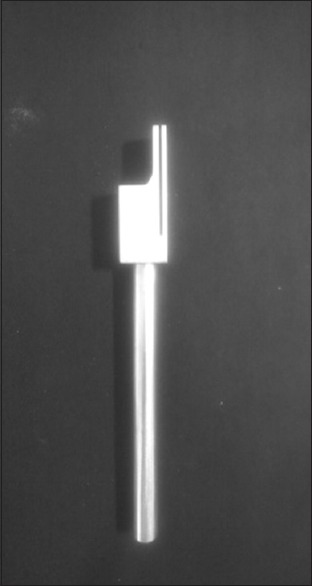
After 4 weeks of usage of conventional complete denture, the first reading for maximal bite force was recorded. After 4 weeks of usage of the implant-retained overdenture, second reading was recorded. Masticatory bite force records were taken with a transducer bite force gauge with a 1000 N capacity which was adapted to the mouth. The apparatus had a “set-zero” key, which allowed the exact control of the values obtained and also “peak” registers, that facilitates the record of the maximal force. It consisted of a bite fork over which the force to be measured was applied. The high-precision charge cell and electronic indicator force circuit and a digital display helped transfer data to Microsoft Excel sheet. The bite force transducer was cleaned with alcohol, and disposable latex finger cots were positioned on the biting arms as a biosecurity measure. The patients were given detailed instructions, and bite tests were performed before the actual recordings were recorded, to ensure the reliability of the procedure. The patients were then asked to bite on the bite fork three times with maximal force, with a 2-min rest interval between records. Readings were performed in the first molar (left and right) region. Maximal bite force was measured in Newton (N) and the “peak” force thus recorded was displayed on the screen. The mean value out of three records was considered as the individual's maximal bite force. The mean of the three measurements was then used as the maximum bite force for each side. Accordingly, three values were recorded for each patient both for the right and left side [Figures 16–23].[4,8]
Figure 16.

Initial design of transducer
Figure 23.

Reading of bite force on digital screen in Newtons
Figure 17.

Modified design of transducer
Figure 18.
Analog bite fork for equalization of bite
Figure 19.
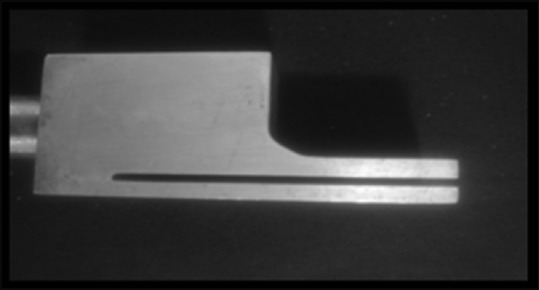
Minimum inter distance between the two elements of bite fork
Figure 20.
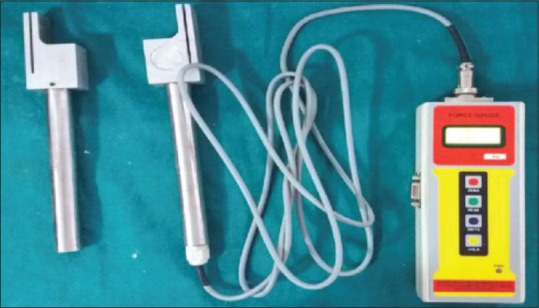
Transducer bite force measurement device with analog for bite equalization
Figure 21.

Masticatory bite force measurement (right side)
Figure 22.

Masticatory bite force measurement (left side)
Patient satisfaction questionnaire
OHIP-edent a shorter version was used for this study. The full and expanded version of OHIP consists of 49 items that cover seven domains: Functional limitation, physical pain, psychologic discomfort, physical disability, psychologic disability, social disability, and handicap. Slade has derived a subset of 14 of the original 49 items that can be used in settings where a short version is required. In the present study, satisfaction levels were measured with questionnaires adapted from the OHIP-edent index which is a more refined of compacted version. Participants were invited to express their opinions about the condition of their dentures through nine questions of the Questionnaire I, in a scale ranging from 0 (zero) to 4 (four), where 0 represents total satisfaction and 4 total dissatisfaction. The highest scores of the questionnaire I represent the worst satisfaction level of masticatory ability [Schematic Chart 3].[9]
Schematic Chart 3.
Oral Health impact profile for Edentulous Patient index
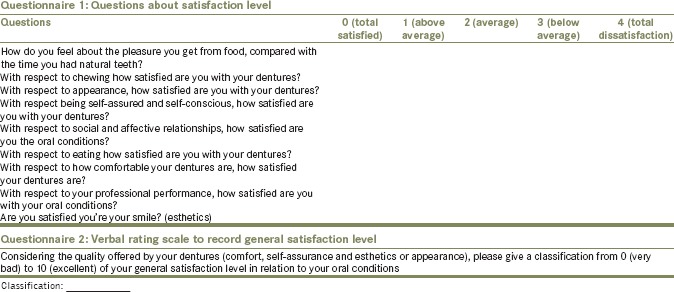
After filling out the questionnaire, the patients were also asked to give a score from 0 to 10 by verbal rating scale (VRS) to their satisfaction level [Questionnaire 2].
Statistical analysis
Descriptive statistics were calculated for all parameters by the independent t-test. The paired t-test was used for pairwise comparison of chewing efficiency evaluating the ten particle size of each participant with conventional dentures and implant-retained overdentures. The association between chewing efficiency, masticatory bite force, and satisfaction level was calculated with the Pearson correlation test. Data analysis was performed using the SPSS 17.0 statistical software (IBM) with a significance level of 5%.
RESULTS
Conventional denture versus implant overdenture
Chewing efficiency
The chewing efficiency was evaluated statistically by paired t-test in which the average particle sizes of 12 patients were calculated, and comparison was done in its dimensions. As average mean particle size Length * Width for conventional complete denture was 0.11 mm ± 0.08 mm standard deviation (SD), P = 0.001, and t-test value 4.045 and for implant-retained overdentures were 0.03 mm ± 0.01 SD, P value 0.001, and t-test value 4.045, and the paired t-test difference between the conventional dentures and implant-retained overdentures was 0.76 ± 0.06 SD, (P > 0.001) and t > 1 which clearly states the change of percentage minimum 70.45% to maximum 85.76% with mean change of percentage of 76.34% of the average particle size of implant-retained overdenture with that of conventional denture. The average number of chewing strokes was reduced to half strokes when compared to conventional denture. The chewing strokes required by conventional denture were 69 strokes and that by implant-supported overdenture which was forty strokes to get the same mean particle size [Graphs 1 and 2].
Graph 1.
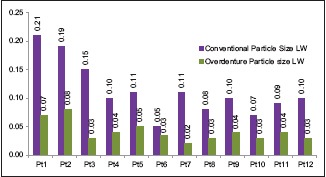
The difference of mean particle size (LW) of n = 12 patients with conventional dentures and implant-supported overdentures
Graph 2.
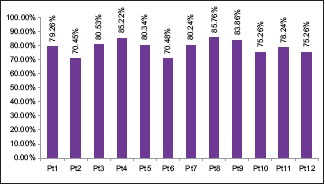
The change of percentage of mean particle size between conventional complete dentures and implant-supported overdenture of each patient n = 12
Masticatory bite force
The masticatory bite force was evaluated statistically by t-test and was found that the mean bite force of patients using implant-retained overdentures was more than double when compared to patients using conventional dentures. The mean bite force range for n = 12 patients conventional denture was from 31.10 N minimum to 88.10 N maximum and for implant-retained overdentures was 57.16 N minimum to 192.40 N maximum. The increase in masticatory bite force seen for conventional dentures in comparison to implant-supported overdenture was from 63.25 N ± 18.15 SD to 133.76 N ± 38.010 SD for the right side and 62.56 N ± 15.63–128.10 N ± 39.04 SD for the left side. The mean increase in bite force of n = 12 patients for conventional denture was 62.90 N and with implant-retained overdenture was 132.20 N. The change of percentage of bite force from conventional to implant-supported overdentures was 110.17% which indicated that bite force gets more than double after using implants [Graph 3].
Graph 3.
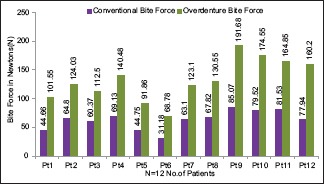
The difference of mean bite force for each patient n = 12 for conventional denture and implant-supported overdenture
Patient satisfaction
OHIP edent questionnaire used in our study is a very potent and reliable method of evaluating and comparing the satisfaction levels of edentulous patients worldwide. The patient satisfaction OHIP edent scores in our study with mandibular two implant-supported overdentures were found to be higher than patients-wearing conventional dentures. The mean score for conventional dentures was 24.92 ± 2.84 SD with (P < 0.000) which indicated the higher levels of disssatisfaction with the complete dentures and the mean for implant-retained overdenture was 16.50 ± 1.83 SD (P > 0.000) which indicated more satisfaction toward implant-retained overdenture.
VRS scores for general satisfaction indicated that complete dentures were functionally inferior than implant-retained overdentures. As for implant-supported overdenture, the mean score was 7.83 +/- 0.69 SD or 78.30% of general satisfaction which was way higher than conventional dentures with mean of 5.42 =/- 0.79 SD or 54.20% of general satisfaction.
We observed large differences in oral function among the patients and significant correlation between median particle size and maximum bite force. Maximum bite force thus explained nearly 60% of the variance in masticatory performance. From the present study, we may conclude that the provision of two mandibular implants significantly improves measures of oral function.
DISCUSSION
The present study was conducted to make quantitative comparisons regarding oral function, namely, chewing efficiency, masticatory bite force, and patient satisfaction between conventional complete denture and implant overdentures patients after 4 weeks of usage.
Edentulism is affiliated with anatomical, functional, and psychologic changes in patients. In complete dentures, the absence of stability, retention, and reduced chewing ability are common oral findings accompanied by poor quality of life. The stated benefits of an implant overdenture include bone preservation, improvement in masticatory ability, masticatory force, increased stability and retention, and significantly higher patient satisfaction. There is a great variety of methodologies describing chewing efficiency. The old methodologies, adaptations, or variations of such, methods using specific apparatus, including new descriptions, are found in this field of scientific research. In the previous studies, various methods have been used to evaluate chewing efficiency using sieve method (single sieve and multiple sieve method), chewing gum given by Poyiadjis and Likeman, chewing gum (color changing type) first done by Hayakawa et al., beads (Colorimetry) by Santos et al. and subjective methods, such as questionnaires, to assess the individual self-perception as to their ability to chew. In 2012, optical scanning in two dimensions was done by image analysis. Among these, the use of sieves system and image analysis are undoubtedly the most indicated method for measuring masticatory efficiency, even in complete dentures wearers.[10,11]
In the present study, a combination of two methods, i.e., single-sieve method and image analysis by gantry excel type VMM were used. This machine was employed for micro measurements of finest chewed particles as it provides most efficient and unique method of visual measurements. In this study, it was evaluated that there is 76.34% of decrease in average particle size of implant-retained overdenture with that of conventional denture. That means the average number of chewing strokes were reduced to more than half then that of conventional denture. The chewing strokes required for conventional denture was 69 strokes to get same mean particle size as of implant-retained overdenture by forty strokes which agrees with the findings of previous studies that the number of chewing cycle reduced to half, and chewing strokes decreased from 55 to 27 cycles for implant overdentures and the average maximum bite force doubled from 162 to 341 N.[12] Evaluation of the data from our study found that the mean bite force of patients-wearing implant-retained overdentures was more than twice as much as those wearing conventional dentures, which agrees with the findings of previous studies.[10] The mean maximal bite force measurements found in both our study readings were lower than the findings reported by other authors.[12,13] This difference may be attributed to the difference in mean age and age range of the patients in these studies. The mean age of the patients in the study (Fontijn-Tekamp et al.[9]) study was 59.1 years while the age range in the (van Kampen[14]) study was 33–56 years. Our patients’ age range was 60–75 years with a mean of 67.25 years, which was higher than in the previous studies.
The patient satisfaction scores in our study with mandibular two implant-supported overdentures were found to be higher than patients wearing conventional dentures, which is in agreement with the literature. VRS scores indicated that complete dentures are functionally inferior, i.e., the patients have the higher score for the implant-retained overdenture as compared to the conventional complete dentures which are in agreement with previous studies.[11,12,15]
CONCLUSION
From the present study, we may conclude that the provision of two mandibular implants significantly improves the measures of oral function and after implant-supported dentures, the food is chewed more efficiently before it was swallowed. In the present study, the sample size was relatively small, therefore, data should be interpreted carefully and should be impetus for further studies. Thus, the present results support the benefits of implant treatment, and patients can be informed how implant treatment with mandible overdentures will improve their oral function. Hence, the rehabilitation with a mandibular overdenture, improved chewing efficiency, masticatory bite force, and patient satisfaction in edentulous patients.
Overall, the oral function improves with the implant-supported overdenture leading to improved and satisfied quality of life.
“Part of the secret of a success in life is to eat what you like and let the food fight it out inside.”
Mark Tawain.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Boven GC, Raghoebar GM, Vissink A, Meijer HJ. Improving masticatory performance, bite force, nutritional state and patient's satisfaction with implant overdentures: A systematic review of the literature. J Oral Rehabil. 2015;42:220–33. doi: 10.1111/joor.12241. [DOI] [PubMed] [Google Scholar]
- 2.Thomason JM, Kelly SA, Bendkowski A, Ellis JS. Two implant retained overdentures – A review of the literature supporting the McGill and York consensus statements. J Dent. 2012;40:22–34. doi: 10.1016/j.jdent.2011.08.017. [DOI] [PubMed] [Google Scholar]
- 3.Sposetti VJ, Gibbs CH, Alderson TH, Jaggers JH, Richmond A, Conlon M, et al. Bite force and muscle activity in overdenture wearers before and after attachment placement. J Prosthet Dent. 1986;55:265–73. doi: 10.1016/0022-3913(86)90358-6. [DOI] [PubMed] [Google Scholar]
- 4.Koc D, Dogan A, Bek B. Bite force and influential factors on bite force measurements: A literature review. Eur J Dent. 2010;4:223–32. [PMC free article] [PubMed] [Google Scholar]
- 5.Awinashe VN, Nagda SJ. A comparative study of the masticatory efficiency in complete dentures using acrylic and metal occlusal posterior teeth-photocolorimetric analysis. J Indian Prosthodont Soc. 2010;10:112–7. doi: 10.1007/s13191-010-0028-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haraldson T, Karlsson U, Carlsson GE. Bite force and oral function in complete denture wearers. J Oral Rehabil. 1979;6:41–8. doi: 10.1111/j.1365-2842.1979.tb00403.x. [DOI] [PubMed] [Google Scholar]
- 7.Slagter AP, Bosman F, Van der Bilt A. Comminution of two artificial test foods by dentate and edentulous subjects. J Oral Rehabil. 1993;20:159–76. doi: 10.1111/j.1365-2842.1993.tb01599.x. [DOI] [PubMed] [Google Scholar]
- 8.van der Bilt A, Olthoff LW, van der Glas HW, van der Weelen K, Bosman F. A mathematical description of the comminution of food during mastication in man. Arch Oral Biol. 1987;32:579–86. doi: 10.1016/0003-9969(87)90067-7. [DOI] [PubMed] [Google Scholar]
- 9.Fontijn-Tekamp FA, Slagter AP, Van Der Bilt A, Van ’T Hof MA, Witter DJ, Kalk W, et al. Biting and chewing in overdentures, full dentures, and natural dentitions. J Dent Res. 2000;79:1519–24. doi: 10.1177/00220345000790071501. [DOI] [PubMed] [Google Scholar]
- 10.Pocztaru RL, Vidal RA, Rivaldo GE, Duarte Gavião MB, van Der Bilt A. Satisfaction level and masticatory performance of patient rehabilitated with implant-supported overdentures. Rev Odonto Ciênc. 2009;24:109–15. [Google Scholar]
- 11.Oliveira NM, Shaddox LM, Toda C, Paleari AG, Pero AC, Compagnoni MA, et al. Methods for evaluation of masticatory efficiency in conventional complete denture wearers: A systematized review. Oral Health Dent Manag. 2014;13:757–62. [PubMed] [Google Scholar]
- 12.van der Bilt A, Abbink JH, Mowlana F, Heath MR. A comparison between data analysis methods concerning particle size distributions obtained by mastication in man. Arch Oral Biol. 1993;38:163–7. doi: 10.1016/0003-9969(93)90202-w. [DOI] [PubMed] [Google Scholar]
- 13.van der Bilt A, Burgers M, van Kampen FM, Cune MS. Mandibular implant-supported overdentures and oral function. Clin Oral Implants Res. 2010;21:1209–13. doi: 10.1111/j.1600-0501.2010.01915.x. [DOI] [PubMed] [Google Scholar]
- 14.van Kampen FM, van der Bilt A, Cune MS, Fontijn-Tekamp FA, Bosman F. Masticatory function with implant-supported overdentures. J Dent Res. 2004;83:708–11. doi: 10.1177/154405910408300910. [DOI] [PubMed] [Google Scholar]
- 15.Shastry T, Anupama NM, Shetty S, Nalinakshamma M. An in vitro comparative study to evaluate the retention of different attachment systems used in implant-retained overdentures. J Indian Prosthodont Soc. 2016;16:159–66. doi: 10.4103/0972-4052.176520. [DOI] [PMC free article] [PubMed] [Google Scholar]


