Abstract
Aims and Objectives:
The lack of information among the population regarding the existence of oral squamous cell carcinoma (OSCC) and the lack of attention and expertise in examining the oral cavity of dentists and clinicians still remain very worrying and could explain the high incidence of OSCC. The aim of this study is to evaluate the level of awareness of OSCC among 600 participants from Southern Italy.
Materials and Methods:
A 13-question survey was prepared and distributed to 600 participants divided into two subgroups, the first one of 300 patients referring to the Department of Neuroscience, Reproductive, and Odontostomatological Sciences, University Federico II of Naples, for the treatment of dental pathologies, and the second one of 300 patients referring to the Department of Internal Medicine of the Second University of Naples for the diagnosis and treatment of cardiovascular diseases. Statistical analysis consisted in the calculation of percentages related to the answers given by patients. Comparison of percentages was after performed between the two subgroups.
Result:
Only 175 participants (29.1%) knew about the existence of pathologies which can affect the oral mucosa, and only 46 (7.6%) were aware that carcinoma can arise in the oral cavity; 345 (57,5%) stated that they had periodical dental visits, at least once a year but none of them stated they had a visit for the identification of oral carcinomas.
Conclusion:
The data acquired must be taken into consideration to outline essential socio-healthcare educational projects on carcinoma and its risk factors, training programs to increase dentists and clinicians’ competences, and to evaluate the feasibility and effectiveness of oral carcinoma screening programs.
KEYWORDS: Awareness, dental education, oral cancer, oral squamous cell carcinoma, prevention, screening, survey
INTRODUCTION
Almost 40% of the neoplasias of head and neck are represented by the squamous cell carcinoma (oral squamous cell carcinoma [OSCC]) of the oral cavity, which is overall the 9th most frequent tumor.[1] It represents 90% of all malignant tumours which arise on the oral mucosa.[2] The OSCC arises most frequently in participants over 45 years old although an increase of incidence among young adults (between 20 and 39 years old) has been reported.[3,4]
The World Cancer Report (WCR) has outlined some important objectives aimed at reducing the incidence and mortality rate of OSCC.[5] The study clearly states that dentists have the chance to limit the expected increase of new cases each year by establishing planned and effective checkup strategies. In the last years, despite the progress made in the diagnosis and treatment of many other malignant neoplasias, the 5-year survival rate has remained low and relatively constant: generally, <50% of these patients survive longer than 5 years. Furthermore, the treatment of such neoplasias is often debilitating and disfiguring,[6] often entailing dysfunctions of phonation, mastication, deglutition, and difficulties with interpersonal relationships.[7,8]
Moreover, along with the increase of incidence in young adults[9,10] in this population category, carcinoma often occurs with higher levels of aggressiveness, related to a higher degree of anaplasia.[11] Probably, a worse prognosis is also due to the different etiologies of the tumor, therefore also to a different biological behavior of the latter, and/or to a late diagnosis enhanced by the erroneous belief that there is a minor incidence of cancer among young people.
Nowadays, there is sufficient data to confirm the close correlation between oropharyngeal carcinoma and lifestyle. Hence, it is clear that modifying life habits by suggesting quitting smoking cigarettes, moderating the consumption of alcoholic drinks, and protecting oneself from ultraviolet radiation,[12] together with anti-HPV vaccination strategies can be considered an important primary prevention action.[13]
It has been established, in fact, that virtually all the OSCCs are preceded by clearly visible changes of the oral mucosa epithelium, among which the most common ones are white and/or red spots.[14] The identification of these precancerous lesions allows the clinician to precociously identify and treat some alterations which can be considered as intraepithelial stages of oral cancerogenesis. The oral cavity is one of the few areas on which you can perform simple and fast examinations, and this highly facilitates the operator in early diagnosis. Nevertheless, the results of the studies carried out so far highlight a totally discouraging situation: paradoxically, the percentage of OSCCs identified during diagnosis is very similar to the percentage of colon tumors (36%) although the examination of the intestinal mucosa needs endoscopic examinations.[15]
Should patients’ responsibility be emphasized or should other aspects also be examined? This delay is profoundly influenced by at least two factors: the level of attention paid by dentists and clinicians to the problem and the lack of information among the population regarding the existence of the carcinoma.[7]
First, patients affected by OSCC often have a history of missed and inaccurate diagnoses, in other words, treatment of the sole symptoms through empirical procedures which are definitely inadequate. This suggests that, in a large number of clinical cases, the clinicians do not suspect that the lesions are malignant. Moreover, such patients state that they have carried out various dental treatments for caries, parodontopathy and prosthetic rehabilitation. This leads us to assume that there are some deficiencies in the examination of the soft tissue, whereas higher attention is paid to the progression of dental and periodontal pathologies by the dentist. However, the factors related more specifically to the patient's responsibility should also be taken into consideration as possible reasons for late requests for doctors’ appointments.
A first important factor is the lack of awareness of the problem, which obviously leads to a lack of watchfulness regarding signs and symptoms on the patient's side.
It is evidently necessary to inform the population about the existence of oral carcinoma, of its risk factors and relative signs and symptoms so that people know how and when they need an appointment with a specialist. Among other factors, we mention the inability to interpret symptoms and signs of the lesion correctly, the absence of pain, especially in precancerous lesions, and in early stages of carcinoma, difficulty and incompetence to examine some areas of the oral cavity, especially in elderly patients, and sociocultural level.[9]
In this study, we evaluated the level of awareness of OSCC among 600 participants from Southern Italy; moreover, after having provided appropriate information, we examined their compliance to follow screening protocols for OSCC by carrying out an examination of the oral mucosa during periodical dental appointments.
MATERIALS AND METHODS
A 13-question survey was prepared and distributed to two groups of participants, whose age was over 40 years old, during the whole year 2008; each group consisted of 300 patients who gave their informed consent for the participation at the study. This study is an extension of our previous study,[16] approved by Review Board, Ethical Committee, Federico II of Naples (ID: 134/14). The participants were randomly enrolled in the study using hospital registries belonging to the outpatient clinic of the Department of Neuroscience, Reproductive, and Odontostomatological Sciences, Federico II University of Naples and the Department of Internal Medicine, Second University of Naples. Group 1 was formed by patients between 41 and 78 years old, referring for the treatment of dental and periodontal pathologies; Group 2 was formed by patients between 45 and 82 years old coming for cardiovascular diseases, metabolic syndrome, and gastrointestinal diseases.
The second group was designed so as to reduce as far as possible any kind of influence on the interviewees related to the fact that the interviewers were members of staff in charge of oral health, given the close correlation among the topics dealt with in the questionnaire, oral pathologies, and dental activity. The questionnaire enquires about the patients’ awareness of pathologies affecting oral mucosa, of OSCC, of the correlation among smoking, alcohol abuse, and different pathologies with special reference to oral carcinoma, and their availability to undergo oral mucosa examination during periodical dental visits. A copy of the questionnaire is reported in Questionnaire 1 (157.6KB, pdf) .
Questionnaire distributed between the two study groups
DATA ANALYSIS
To investigate the association between the group and the responses to the questionnaire, a 2 × 2 Chi-square analysis was carried out on the contingency table. Moreover, to test if “yes” and “no” responses were equally distributed independently of the group, a one-way Chi-square analysis was carried out on each question. In both analyses, when Chi-square was significant, the standardized residuals (Z-score) were computed for each cell. A level of significance of 0.05 was considered statistically significant.
RESULTS
Among the 300 participants in Group 1, only 89 (29.6%) knew about the existence of pathologies which can affect the oral mucosa, and only 25 (8.3%) were aware that carcinoma can arise in the oral cavity. The questionnaires of Group 2 gave similar results: the percentages of participants informed about the existence of oral mucosa pathologies and OSCC were, respectively, 28.6 (86/300) and 7 (21/300) [Table 1]. As shown in Table 1, the differences between the two groups were not significant [Table 1]. Therefore, the overall percentage of participants who answered in a positive way was 29.1 (175/600) and 7.6 (46/600). Among the latter, 23 (54.3%) received information about OSCC from their dentist, 15 (32.6%) from their general practitioner, 4 (8.7%) from an otolaryngologist, and 4 (8.7%) from a maxillofacial surgeon. The Chi-square analysis showed that responses were not equivalent, χ2(3) = 22.348, P < 0.001, and that the most of the patients were informed by the dentist (Z-score = 3.391), and not by otolaryngologist or maxillofacial surgeon (Z-scores = −2.212).
Table 1.
Distribution of “yes” responses as a function of the group and the question
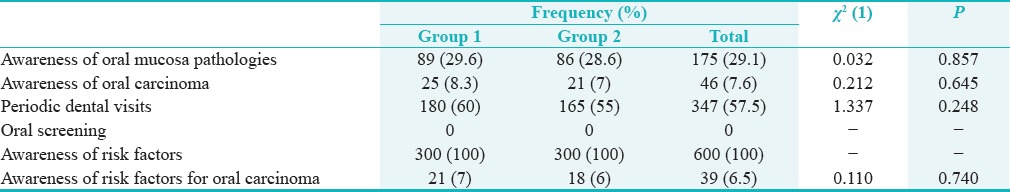
Only 60% (180/300) and 55% (165/300) of the participants in Groups 1 and 2, respectively, stated that they had periodical dental visits, at least once a year. None of them stated they had a visit for the identification of OSCCs 0% (0/600). As shown in Table 1, also in these cases, the differences between the two groups were not significant [Table 1].
Nearly 100% of the participants in both groups knew that cigarette smoking is bad for your health, as it facilitates the onset of cardiovascular pathologies, emphysema, and lung cancer. In the same way, all 600 participants (100%) were well aware of the correlation between alcohol abuse and different pathologies such as cirrhosis and liver cancer.
Unfortunately, very few participants were aware of the correlation between such life habits and OSCC: only 21 (7%) in Group 1 and 18 (6%) in Group 2, and the differences between the two groups were not significant [Table 1].
After being informed about the existence of cancerous and precancerous oral lesions, 99% of the participants (Z-score = 16.974) expressed their willingness to follow a screening program for OSCC χ2(1) = 576.240, P < 0.001. They showed great interest in the possibility of having an examination of the oral mucosa done during dental recall visits, and they believed it was an important dental preventive measure.
DISCUSSION
Only 36% of malignant tumors of the oropharynx are diagnosed at an early stage. The disappointing conclusion that this percentage has not grown over the last decades suggests that prevention programs have not been carried out adequately.[17] Hundreds of millions of dollars are spent for the treatment of patients in serious conditions, one third of which will die within 3–5 years; on the contrary, the screening for OSCC is a simple and noninvasive procedure that only requires gloves, gauzes, adequate lighting for the systematic inspection of the oral cavity, and it lasts a few minutes.[14]
Furthermore, a large part of the research into OSCC, as well as cultural, human, and financial resources, is focused on complex, expensive, and often ineffective therapeutic procedures used for OSCC at an advanced stage. Hence, the concepts of prevention, early diagnosis, and elimination of risk factors appear less frequently in literature as well as in practice.[14]
It is time to change the attitude toward this pathology and divert from such an abnormal trend. We hope that the WCR's guidelines will inspire researchers, health-care organizations, clinicians, and governments to promote new and effective strategies for the prevention and early diagnosis, allocating resources carefully.
The reasons why health-care organizations spend their resources in this direction and not on effective and inexpensive prevention programs are still not clear. However, some theories have been put forward. First of all, lack of awareness of oral carcinoma, of its signs and symptoms, and risk factors has been reported.[5,18,19,20] In particular, our study has pointed out that only 7.6% of the people interviewed knew about the existence of OSCC, and only 6.5% were informed about the correlation between smoking and alcohol abuse and this neoplasia. Consequently, it is clear that prevention cannot be carried out without prior correct information.
The lack of awareness of OSCC is considered one of the main factors which limit the possibility to carry out screening procedures, as it is closely related to the scarce availability of patients to undergo periodic visits for the early diagnosis of carcinomas.[21] In fact, many screening programs have been created, but data on their feasibility and effectiveness are so scarce that there is no sufficient proof to allow to carry out screening programs on a large scale.[22,23,24] Therefore, by highlighting the patient's responsibility, it could be explained why the majority of carcinomas is already at an advanced stage at first examination [Figure 1]: screening programs based on the population have so far failed to meet their objectives.[7]
Figure 1.

Invasive oral cancer of the buccal mucosa
The several prevention information campaigns for cardiovascular, hepatic, and respiratory pathologies carried out in the last decades have been successful in reducing the incidence and mortality related to such pathologies. On the contrary, epidemiological data referring to OSCC are disheartening due to a serious lack of awareness of this neoplasia among the population.
It is important to point out that the scarce awareness of the problem and of its possible prevention entails serious consequences: the common belief according to which the development of cancer is exclusively a matter of chance impedes the possibility to carry out prevention.[19,25] This fatalistic approach towards cancer is one of the main reasons of the incapacity to accept the specialist's advice.[19] Therefore, it compromises the patient's compliance.
Studies performed after the distribution of informative brochures to patients referring to a hospital with the aim of measuring the resulting psychological effects have produced encouraging data: the information did not cause adverse effects on the willingness to join screening programs, nor did it increase the patients’ fear of the tumor. On the contrary, the patients informed were clearly less anxious and more willing to undergo visits for the early diagnosis of carcinoma compared with the patients in the control group.[26,27,28]
We ought to remember, though, that the patients’ responsibility in the delay of the diagnosis is only one side of the problem. It is also necessary to analyze the clinicians’ commitment to the prevention and diagnosis of OSCC.
As many authors suggest, the role of the dentist is essential with regard to primary and secondary prevention of OSCC.[29,30] In fact, periodical recalls enable them to examine the mucosa very frequently, identify the carcinoma at an early stage, differentiate benign from risk lesions, perform simple biopsies, or refer patients to specialists in oral medicine and surgery.[31] Moreover, they can act upon risk factors by informing patients about the need for changing their lifestyle.
Nonetheless, studies carried out to evaluate the attention and commitment of dentists regarding this problem show a very disappointing scenario. They do not regularly perform an examination of the mucosa, they do an incomplete, inconsistent, and unacceptable screening, they pay more attention to dental and periodontal pathologies, and they do not establish sufficient preventive measures of any kind.[21,31,32,33] Some authors even report that the majority of dentists prefer not to investigate risk factors, nor do they advise to stop smoking or moderate the consumption of alcoholic drinks, as they consider these as indiscreet and inopportune indications.[31] However, there is scientific evidence which supports the role of doctors and dentists in this sense: they can play a key role in convincing their patients to reduce or remove such harmful health risks.[21,31,34] After all, this behavior should be one of the main duties of anyone who dedicates their life to safeguarding people's health.
Nonetheless, it is also important to highlight the role of general practitioners in the prevention and early diagnosis of malignancies related to the oropharyngeal area. This is due to the fact that, in any 1 year, almost 80% of participants over 40 years of age see a general practitioner, whereas only 43% of these meet a dentist within the same length of time.[35,36,37,38] Moreover, doctors have the chance to visit high-risk participants more often.[39] Hence, a complete oral screening examination would be a further excellent opportunity to check tumors of the oral cavity, especially in heavy smokers and alcoholics over 40.[40]
Despite these considerations, the results of a study aimed at examining the behavior of doctors concerning the prevention of such tumors show that only 25% of them performed examinations of the oral cavity. On the other hand, compared to dentists, they were more willing to ask their patients for information regarding cigarette smoking and excessive alcohol consumption; however, only a few of them advised suspending such bad habits.[41]
During periodic recalls, dentists can carry out a simple screening of the oral mucosa, which consists in an examination of the soft tissue that can be performed during a short dental visit. Concerning this point, we have noticed in our study that none of the participants interviewed had ever undergone a screening visit for OSCC (0/600, 0%), even if they attended periodic recalls (347/600, 57.5%). Furthermore, after having adequately informed the participants about carcinoma and the possibilities of carrying out prevention, we analyzed how they reacted to the suggestion of undergoing oral screening. The fact that 99% of those interviewed showed great interest in this, as they considered it an important preventive measure, was not a surprise. However, more in-depth studies would be worthwhile so as to measure the correlation between patients’ availability and willingness and their actual behaviour.
CONCLUSION
The data acquired must be taken into consideration to outline essential socio-health-care educational projects on carcinoma and its risk factors and to evaluate the feasibility and effectiveness of OSCC screening programs which have so far been undermined by worryingly low participation rates. It is necessary to focus on some points to plan really effective screening programs:
There is little educational material (brochures, posters, social advertising, etc.,) on oral carcinoma[27]
Informing the population, therefore increasing the awareness of the problem and reducing any visit-related anxiety, promotes compliance[27,42,43]
The examination of the mucosa is a “subjective” screening, and it is highly influenced by the level of knowledge and specialization of the examiners[17]
A thorough screening often shows the presence of precancerous lesions rather than clearly malignant lesions; therefore the lack, in terminology, of universal definitions in histologic diagnosis may influence the results of the screening[5,17]
The simple identification of participants at risk and a routine examination of the mucosa of the oral cavity are considered safer, more effective, and more economical screening methods.[14,44]
Hence, to define screening programs which are truly valid and feasible, that is to say systematically and on a large scale, the following objectives ought to be pursued:
First of all, make the population aware of the problem and of the possibility to prevent it by launching information campaigns through any kind of advertising media available
Increase doctors and dentists’ awareness of their responsibility to save their patients’ lives through simple and quick operations
Plan training and specialization courses face-to-face or web-based for doctor and dentists[45,46]
Standardize policies aimed at improving and promoting prevention and early diagnosis programs for the entire population at risk.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
ACKNOWLEDGMENT
The authors would most sincerest thank Prof. Vincenzo Paolo Senese from Psychometric Laboratory, Department of Psychology, University of Campania “Luigi Vanvitelli,” Italy, for statistical data processing and assistance.
REFERENCES
- 1.International Agency for Research on Cancer (IARC), WHO; 2000. International Agency for Research on Cancer (IARC) – WHO. GLOBOCAN 2000 Database: Cancer Incidence, Mortality and Prevalence Worldwide, Estimates for the Year 2000. [Google Scholar]
- 2.Hema KN, Smitha T, Sheethal HS, Mirnalini SA. Epigenetics in oral squamous cell carcinoma. J Oral Maxillofac Pathol. 2017;21:252–9. doi: 10.4103/jomfp.JOMFP_150_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta N, Gupta R, Acharya AK, Patthi B, Goud V, Reddy S, et al. Changing trends in oral cancer – A global scenario. Nepal J Epidemiol. 2016;6:613–9. doi: 10.3126/nje.v6i4.17255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Santos HB, dos Santos TK, Paz AR, Cavalcanti YW, Nonaka CF, Godoy GP, et al. Clinical findings and risk factors to oral squamous cell carcinoma in young patients: A 12-year retrospective analysis. Med Oral Patol Oral Cir Bucal. 2016;21:e151–6. doi: 10.4317/medoral.20770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mignogna MD, Fedele S, Lo Russo L. The World Cancer Report and the burden of oral cancer. Eur J Cancer Prev. 2004;13:139–42. doi: 10.1097/00008469-200404000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Greenlee RT, Murray T, Bolden S, Wingo PA. Cancer statistics, 2000. CA Cancer J Clin. 2000;50:7–33. doi: 10.3322/canjclin.50.1.7. [DOI] [PubMed] [Google Scholar]
- 7.Mignogna MD, Fedele S, Lo Russo L, Ruoppo E, Lo Muzio L. Oral and pharyngeal cancer: Lack of prevention and early detection by health care providers. Eur J Cancer Prev. 2001;10:381–3. doi: 10.1097/00008469-200108000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Le Campion AC, Ribeiro CM, Luiz RR, da Silva Júnior FF, Barros HC, Dos Santos KC, et al. Low survival rates of oral and oropharyngeal squamous cell carcinoma. Int J Dent. 2017;2017:5815493. doi: 10.1155/2017/5815493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hussein AA, Helder MN, de Visscher JG, Leemans CR, Braakhuis BJ, de Vet HC, et al. Global incidence of oral and oropharynx cancer in patients younger than 45 years versus older patients: A systematic review. Eur J Cancer. 2017;82:115–27. doi: 10.1016/j.ejca.2017.05.026. [DOI] [PubMed] [Google Scholar]
- 10.Scott SE, Grunfeld EA, McGurk M. Patient's delay in oral cancer: A systematic review. Community Dent Oral Epidemiol. 2006;34:337–43. doi: 10.1111/j.1600-0528.2006.00290.x. [DOI] [PubMed] [Google Scholar]
- 11.Liu X, Gao XL, Liang XH, Tang YL. The etiologic spectrum of head and neck squamous cell carcinoma in young patients. Oncotarget. 2016;7:66226–38. doi: 10.18632/oncotarget.11265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alfano MC, Horowitz AM. Professional and community efforts to prevent morbidity and mortality from oral cancer. J Am Dent Assoc. 2001;(Suppl 132):24S–9S. doi: 10.14219/jada.archive.2001.0385. [DOI] [PubMed] [Google Scholar]
- 13.Hirth JM, Chang M, Resto VA, HPV Study Group. Prevalence of oral human papillomavirus by vaccination status among young adults (18-30 years old) Vaccine. 2017;35:3446–51. doi: 10.1016/j.vaccine.2017.05.025. [DOI] [PubMed] [Google Scholar]
- 14.Mignogna MD, Fedele S, Lo Russo L, Ruoppo E, Lo Muzio L. Costs and effectiveness in the care of patients with oral and pharyngeal cancer: Analysis of a paradox. Eur J Cancer Prev. 2002;11:205–8. doi: 10.1097/00008469-200206000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Mashberg A. Diagnosis of early oral and oropharyngeal squamous carcinoma: Obstacles and their amelioration. Oral Oncol. 2000;36:253–5. doi: 10.1016/s1368-8375(00)00006-3. [DOI] [PubMed] [Google Scholar]
- 16.Leuci S, Aria M, Nicolò M, Spagnuolo G, Warnakulasuriya K, Mignogna MD, et al. Comparison of views on the need for continuing education on oral cancer between general dentists and oral medicine experts: A Delphi survey. J Int Soc Prev Community Dent. 2016;6:465–73. doi: 10.4103/2231-0762.192944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patton LL. The effectiveness of community-based visual screening and utility of adjunctive diagnostic aids in the early detection of oral cancer. Oral Oncol. 2003;39:708–23. doi: 10.1016/s1368-8375(03)00083-6. [DOI] [PubMed] [Google Scholar]
- 18.Zohoori FV, Shah K, Mason J, Shucksmith J. Identifying factors to improve oral cancer screening uptake: A qualitative study. PLoS One. 2012;7:e47410. doi: 10.1371/journal.pone.0047410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kujan O, Duxbury AJ, Glenny AM, Thakker NS, Sloan P. Opinions and attitudes of the UK's GDPs and specialists in oral surgery, oral medicine and surgical dentistry on oral cancer screening. Oral Dis. 2006;12:194–9. doi: 10.1111/j.1601-0825.2005.01188.x. [DOI] [PubMed] [Google Scholar]
- 20.Shrestha A, Marla V, Shrestha S, Agrawal D. Awareness of undergraduate dental and medical students towards oral cancer. J Cancer Educ. 2016;32:778–83. doi: 10.1007/s13187-016-1023-4. [DOI] [PubMed] [Google Scholar]
- 21.Walsh T, Liu JL, Brocklehurst P, Glenny AM, Lingen M, Kerr AR, et al. Clinical assessment to screen for the detection of oral cavity cancer and potentially malignant disorders in apparently healthy adults. Cochrane Database Syst Rev. 2013;11:CD010173. doi: 10.1002/14651858.CD010173.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boyle P, Macfarlane GJ, Blot WJ, Chiesa F, Lefebvre JL, Azul AM, et al. European school of oncology advisory report to the European commission for the Europe against cancer programme: Oral carcinogenesis in Europe. Eur J Cancer B Oral Oncol. 1995;31B:75–85. doi: 10.1016/0964-1955(95)00007-5. [DOI] [PubMed] [Google Scholar]
- 23.Sciubba JJ. Oral cancer. The importance of early diagnosis and treatment. Am J Clin Dermatol. 2001;2:239–51. doi: 10.2165/00128071-200102040-00005. [DOI] [PubMed] [Google Scholar]
- 24.Weinberg MA, Estefan DJ. Assessing oral malignancies. Am Fam Physician. 2002;65:1379–84. [PubMed] [Google Scholar]
- 25.Mignogna MD, Fedele S, Lo Russo L, Lo Muzio L. Lack of public awareness toward alcohol consumption as risk factor for oral and pharyngeal cancers. Prev Med. 2001;33:137–9. doi: 10.1006/pmed.2001.0861. [DOI] [PubMed] [Google Scholar]
- 26.London: National Institute for Health and Care Excellence (UK); 2015. National Institute for Health and Care Excellence: Clinical Guidelines. Suspected Cancer: Recognition and Referral National Collaborating Centre for Cancer (UK) [PubMed] [Google Scholar]
- 27.Humphris GM, Field EA. An oral cancer information leaflet for smokers in primary care: Results from two randomised controlled trials. Community Dent Oral Epidemiol. 2004;32:143–9. doi: 10.1111/j.0301-5661.2004.00129.x. [DOI] [PubMed] [Google Scholar]
- 28.Humphris GM, Field EA. The immediate effect on knowledge, attitudes and intentions in primary care attenders of a patient information leaflet: A randomized control trial replication and extension. Br Dent J. 2003;194:683–8. doi: 10.1038/sj.bdj.4810283. [DOI] [PubMed] [Google Scholar]
- 29.Khalili J. Oral cancer and role of general dental practitioners in its early detection. Lik Sprava. 2007;7:10–9. [PubMed] [Google Scholar]
- 30.Bregman JA. The oral cancer epidemic. Todays FDA. 2016;28:32–3. 35. [PubMed] [Google Scholar]
- 31.Horowitz AM, Canto MT, Child WL. Maryland adults’ perspectives on oral cancer prevention and early detection. J Am Dent Assoc. 2002;133:1058–63. doi: 10.14219/jada.archive.2002.0329. [DOI] [PubMed] [Google Scholar]
- 32.Noro LR, Landim JR, Martins MC, Lima YC. The challenge of the approach to oral cancer in primary health care. Cien Saude Colet. 2017;22:1579–87. doi: 10.1590/1413-81232017225.12402015. [DOI] [PubMed] [Google Scholar]
- 33.Psoter WJ, Morse DE, Sánchez-Ayendez M, Vega CM, Aguilar ML, Buxó-Martinez CJ, et al. Increasing opportunistic oral cancer screening examinations: Findings from focus groups with general dentists in Puerto Rico. J Cancer Educ. 2015;30:277–83. doi: 10.1007/s13187-014-0679-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stacey F, Heasman PA, Heasman L, Hepburn S, McCracken GI, Preshaw PM. Smoking cessation as a dental intervention – Views of the profession. Br Dent J. 2006;201:109–13. doi: 10.1038/sj.bdj.4813829. [DOI] [PubMed] [Google Scholar]
- 35.Canto MT, Horowitz AM, Drury TF, Goodman HS. Maryland family physicians’ knowledge, opinions and practices about oral cancer. Oral Oncol. 2002;38:416–24. doi: 10.1016/s1368-8375(01)00080-x. [DOI] [PubMed] [Google Scholar]
- 36.Bloom B, Simile CM, Adams PF, Cohen RA. Oral health status and access to oral health care for U.S. adults aged 18-64: National Health Interview Survey, 2008. Vital Health Stat 10. 2012;253:1–22. [PubMed] [Google Scholar]
- 37.Ahluwalia A, Crossman T, Smith H. Current training provision and training needs in oral health for UK general practice trainees: Survey of General Practitioner Training Programme Directors. BMC Med Educ. 2016;16:142. doi: 10.1186/s12909-016-0663-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Crossman T, Warburton F, Richards MA, Smith H, Ramirez A, Forbes LJ. Role of general practice in the diagnosis of oral cancer. Br J Oral Maxillofac Surg. 2016;54:208–12. doi: 10.1016/j.bjoms.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 39.Applebaum E, Ruhlen TN, Kronenberg FR, Hayes C, Peters ES. Oral cancer knowledge, attitudes and practices: A survey of dentists and primary care physicians in massachusetts. J Am Dent Assoc. 2009;140:461–7. doi: 10.14219/jada.archive.2009.0196. [DOI] [PubMed] [Google Scholar]
- 40.Ferullo A, Silk H, Savageau JA. Teaching oral health in U.S. Medical schools: Results of a national survey. Acad Med. 2011;86:226–30. doi: 10.1097/ACM.0b013e3182045a51. [DOI] [PubMed] [Google Scholar]
- 41.Brownson RC, Davis JR, Simms SG, Kern TG, Harmon RG. Cancer control knowledge and priorities among primary care physicians. J Cancer Educ. 1993;8:35–41. doi: 10.1080/08858199309528205. [DOI] [PubMed] [Google Scholar]
- 42.Chung V, Horowitz AM, Canto MT, Siriphant P. Oral cancer educational materials for the general public: 1998. J Public Health Dent. 2000;60:49–52. doi: 10.1111/j.1752-7325.2000.tb03292.x. [DOI] [PubMed] [Google Scholar]
- 43.Bastian H. Health literacy and patient information: Developing the methodology for a national evidence-based health website. Patient Educ Couns. 2008;73:551–6. doi: 10.1016/j.pec.2008.08.020. [DOI] [PubMed] [Google Scholar]
- 44.Gogarty DS, Shuman A, O’Sullivan EM, Sheahan P, Kinsella J, Timon C, et al. Conceiving a national head and neck cancer screening programme. J Laryngol Otol. 2016;130:8–14. doi: 10.1017/S0022215115003084. [DOI] [PubMed] [Google Scholar]
- 45.Nayak PP, Nayak SS, Sathiyabalan D, Aditya NK, Das P. Assessing the feasibility and effectiveness of an app in improving knowledge on oral cancer-an interventional study. J Cancer Educ. 2017;4:778–83. doi: 10.1007/s13187-017-1239-y. [DOI] [PubMed] [Google Scholar]
- 46.Awojobi O, Newton JT, Scott SE. Pilot study to train dentists to communicate about oral cancer: The impact on dentists’ self-reported behaviour, confidence and beliefs. Br Dent J. 2016;220:71–6. doi: 10.1038/sj.bdj.2016.57. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Questionnaire distributed between the two study groups


