Abstract
Aims and Objectives:
The aims and objectives of this study were to determine if an association exists between mothers work status and her children's incidence of bruxism and habits related to bruxism.
Materials and Methods:
A cross-sectional study was conducted through data collection of a questionnaire answered by 561 mothers’ about their working status and their child's habits and behaviors. The survey consisted of 5 parts with a total of 34 questions: mother's information, child's behavior, child's sleeping pattern, mother's knowledge about bruxism, and child's medical history. Odds ratios, Chi-square, and their corresponding 95% confidence intervals are reported. Statistical significance was set at P ≤ 0.05.
Results:
The work status of the mother was not statistically significant in increasing the incidence of a child to have bruxism. However, this study clearly elucidates that 7 of the 15 habits correlate significantly with a status of bruxism. According to this sample, a child, that is, reported to be aggressive is more than twice as likely to have nocturnal bruxism. Likewise, any child that bites their nails, complains of headaches, drools in their sleep, snores, complains of muscle cramps, and colic is more than twice as likely to be a nocturnal bruxer than a child that does not have these habits.
Conclusion:
The prevalence of children's bruxism in this convenient sample was 34.5% (n = 141). The concerning habits related to bruxism can serve the pediatric dentist, general dentist, general practitioner, and primary care provider of children having these red flags as indicators of bruxism. It is imperative that parents of these children be made aware these habits that may occur together, alone or even simultaneously with bruxism.
KEYWORDS: Bruxism, children, drooling, enuresis, headaches, parafunction, sleep, snoring
INTRODUCTION
Bruxism is defined as a movement disorder characterized by clenching grinding of teeth.[1] The drum was the first one to initially bring into light movement disorder as an “oral parafunction.”[2] Hence, the term parafunction was introduced as a term to discriminate between normal function of the masticatory system, whereby there is occlusal stress generated during mastication and function; and occlusal stresses that run outside of normal function. The former is known as function, and the latter as parafunction.
This habit might occur during the awake or night hours, and it could be conscious and nonconscious.[3] Awake bruxism is a jaw clenching habit that appears in reaction to anxiety and stress,[4] whereas sleep bruxism (SB) serves as a sleep-related rhythmic masticatory activity that is generally associated with arousals and being more frequent in stages 1 and 2 of the nonrapid eye movements sleep.[5,6,7] During sleep, microarousals are considered to be the main reason for night jaw-closing muscles activation which is known as bruxism.[8]
Sleep is an integral activity of human behavior intended for healing, regeneration, and generalized well-being. Although the biological function of sleep is still a gray area in the literature, it is necessary for physical rest, balanced emotions, as well as neurological harmony. Sleep deprivation poses initially short-term and later long-term side effects. The former being poor attention, delayed reflex, poor productivity among others, whereas the latter is a recipe for metabolic syndrome and premature mortality. In children, sleep problems can vary from snoring, night terrors to sleep bruxism, but together they all pose single-handedly an interruption in the quality of sleep which in turn may lead to depression, attention deficit disorder, hyperactivity, cognitive impairment, learning disability, and emotional upheaval.[9,10]
A recent study conducted in Korea in children found around 30% of nearly a 1000 children under age 18 snored, and approximately 20% of them had night terrors, sleep bruxism (SB), and enuresis. Children who snored were 4 times more likely to have sleep-disordered breathing.[11,12]
Breathing problems in childhood might exacerbate bruxism which indicates enlarged adenoids, and this, in turn, can influence dental development and cause malocclusion.[13,14,15]
Bruxism is recognized to have a multifactorial etiology. The after effects of bruxism consist of temporomandibular joint dysfunction, masticatory muscle soreness, headaches, and attrition of the teeth.[16] Grinding and sleep bruxism (SB) have been related to peripheral factors such as interference of teeth in dental occlusion, psychosocial connections such as anxiety and stress and pathophysiological or central causes involving brain neurotransmitters and basal ganglia.[17] Stress in the pathophysiology of bruxism is considered unreliable, still, it is probably the cause to which most often attributed in the etiology of oral parafunctions.[18] In children, the prevalence of bruxism ranges from 7% to 88% and in adults from 5% to 15%.[19,20] The difference in prevalence is due to a discrepancy used by different researchers in diagnostic criteria, population sample, and varying examination styles. Despite the variations, diagnosis of bruxism remains a great challenge in dentistry due to its multifactorial nature.
The ripple effect of bruxism into adulthood poses serious consequences leading to sleep disturbance, headaches, nonodontogenic orofacial pain, and temporomandibular joint disorders among others all leading to an increased financial burden on its victim as well as social discord.
Literature supports the psychological impact of anxiety and stress on aggravating headaches, orofacial pain, and temporomandibular disorder (TMD) in childhood.[21,22,23]
It is, therefore, imperative to diagnose the etiology to avoid its unwanted aftermath.
Headaches and sleep bruxism (SB) usually occur hand in hand and a 13-year follow-up study by Brattberg in children aged 8–14 years of age showed that an incidence of headache once a week guaranteed headaches in adulthood.[24]
A recent population-based study conducted on 6–8-year-old in Finland found that those children that had disrupted restless sleep were in turn more likely to have craniofacial pain. This is a term encompassing a number of conditions in the cranium and face including headaches, orofacial pain, among others.[25]
The aim of this study is to evaluate the potential effect of mothers’ work status on children's bruxism status between the ages of 4–10 in a subset of the Saudi population.
MATERIALS AND METHODS
SAMPLE SELECTION
An operator designed English as well as Arabic Language questionnaire was developed to be easily completed by mothers of the school-aged children between the ages of 4 and 10. The questionnaire was translated into Arabic and then translated back to English by another person. Any discrepancy was immediately discussed and corrected before finalizing both Arabic and English questionnaires. These questionnaires were then dispersed either through social media by use of Monkey Survey, as well as hard copy questionnaires distributed in the waiting room areas of Riyadh Colleges of Dentistry and Pharmacy in Riyadh, Saudi Arabia. During November and December 2016, a total of 581 questionnaires were distributed through the paper and online forms around Working as well as non-working mothers (NWM) in both the Arabic and English languages. Even though this study did not pose any harmful risk to its participants, ethical approval for this questionnaire style study was attained from the Institutional Review Board of Riyadh Colleges of Dentistry and Pharmacy with approval number RC/IRB/2016/161. The only link that could relate the participant to the study was through the consent form, which was attached to the paper-based questionnaire and found at the beginning of the online survey. The power of sample was 0.85.
QUESTIONNAIRE DEVELOPMENT
The questionnaire was designed to be aimed at the mother's work status and her child's habits and behaviors. The phrase “bruxism” was changed to “teeth grinding” to make it easier for mothers to understand. The following questions were developed and adapted from a cocktail of questionnaires including and not limited to Weideman's Study,[16] the sleep behavior scale by Fisher,[26] the pediatric questionnaire,[27] teeth grinding questionnaire and standardized questionnaire,[28] as well as the total design method.[29] The survey consisted of 5 categories with a total of 34 closed-ended questions: mother's information, mother's knowledge about bruxism, child's behavior, child's sleeping pattern, and child's medical history.
DATA ANALYSIS
A total of 581 questionnaires were initiated yet only 561 of those questionnaires were completed with a 97% response rate. Statistical Package for the Social Sciences software (SPSS, version 20, SPSS Inc., Chicago, IL, USA) was used to analyze the difference in the proportion of “yes” responses between the bruxer and nonbruxer groups; and Working Mothers (WM) and Non Working Mothers (NWM), and for each yes and no question; a Fisher's exact test was performed. Odds ratios (ORs) and their corresponding 95% confidence intervals (CIs) are reported. Statistical significance was set at P ≤ 0.05.
RESULTS
The majority of the participants were Saudi Arabian nationals (n = 498, 88.9%) [Figure 1]. The median age of the participants was 31–40 years (n = 307, 55%) of age and the majority had a bachelor's degree (n = 351, 63%) [Figure 2]. The median number of children was 3 (n = 75, 21.4%) with a minimum of 1 (n = 54, 15.4%) and maximum of 10 (n = 4, 1.1%), respectively. WM constituted 73% (n = 388) of the total sample (n = 529). The majority of the participants were teachers (28.9%) followed by NWM (26.7%), administrators (19.7%), engineers (14.4%), and doctors (9.5%) [Figure 3].
Figure 1.
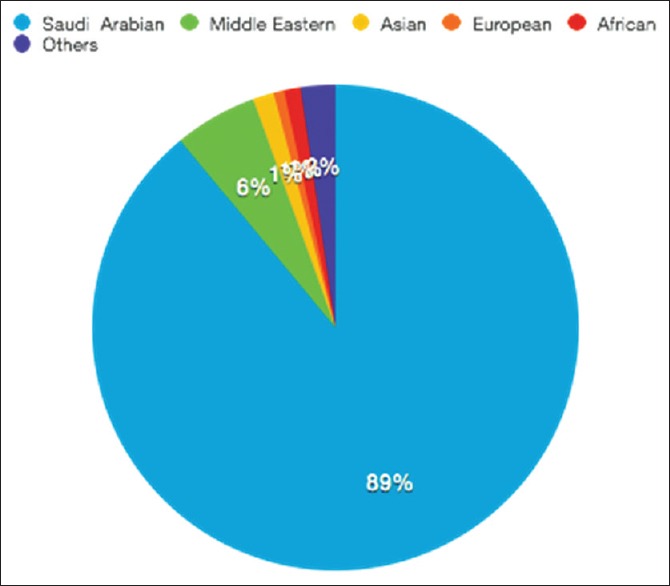
Distribution of participants nationality (n = 560)
Figure 2.
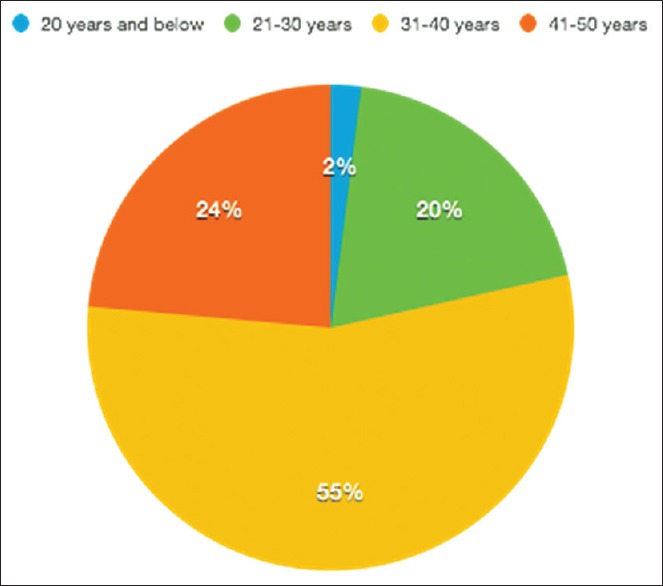
Distribution of age of participants (n = 559)
Figure 3.
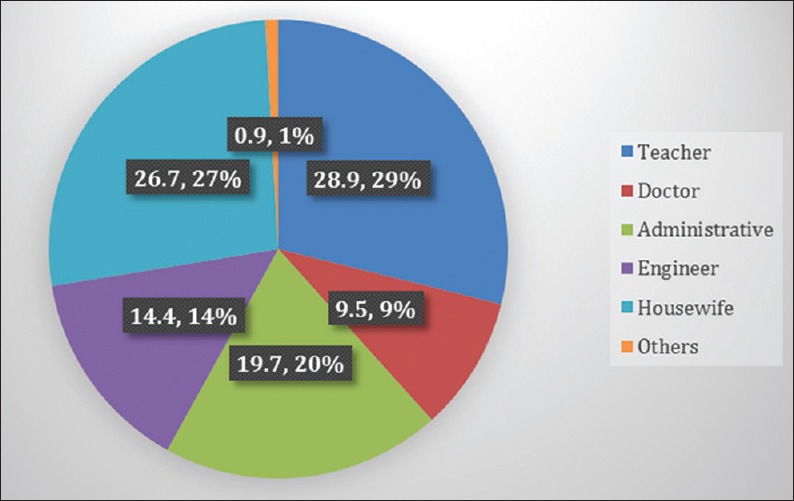
Distribution of occupation of the participants (n = 529)
Most WM worked 6 h/day (59%) followed by 8 h (35%) and 4 h (6%), respectively.
Table 1 shows the habits of the children as reported by the participants. The most common habit reported by parents was children grinding their teeth at night (n = 141, 34.56%), followed by nail biting (n = 136, 24.8%), and bedwetting – enuresis (n = 102, 22.37%). Report of headaches and aggression were least common at (n = 49, 9.8%) and (n = 40, 7.86%), respectively.
Table 1.
Habits of children
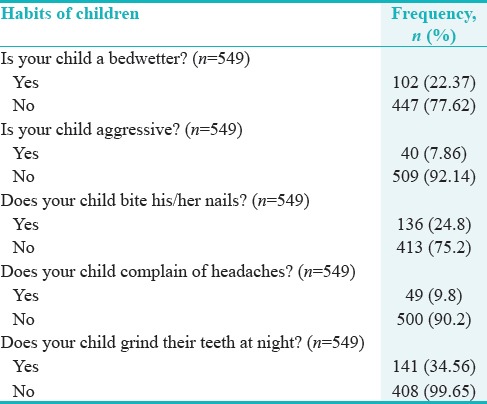
Table 2 looks at the Sleeping Habits of Children.
Table 2.
Sleeping habits of children
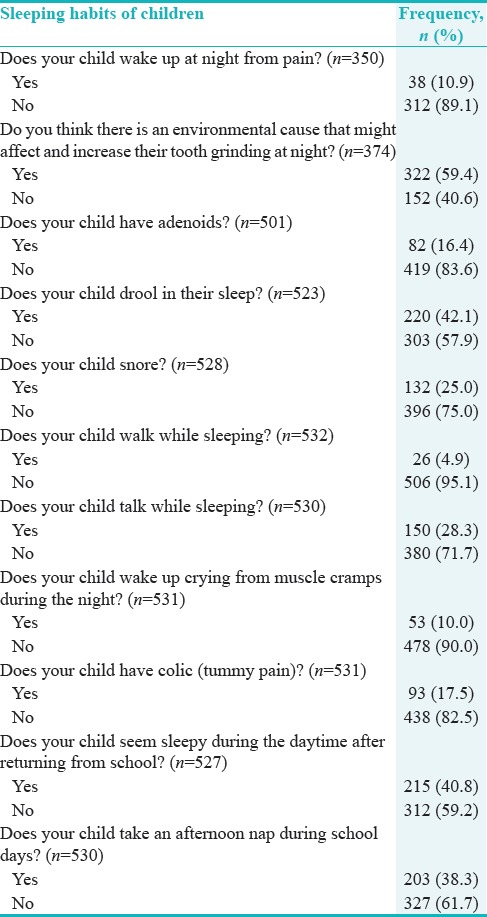
The most common habit was drooling (n = 220, 42.3%), followed by sleep talking (n = 150, 28.3%), snoring (n = 132, 25%), colic (n = 93, 17.5%), adenoids (n = 82, 16.4%), wakes up from muscle cramps (n = 53, 10%), and finally, sleepwalking (n = 26, 4.9%).
More than half the mothers (n = 322, 59.4%) think that there is an environmental cause, which is causing the tooth grinding at night. More than a third of the children seemed sleepy during the day on returning from school (n = 215, 40.8%).
Table 3 addressed the differences between WM and NWM in their knowledge of tooth grinding, where 44.1% of WM had some form of information pertaining to bruxism as opposed to 35% of NWM.
Table 3.
Association between mothers work status and their children bruxism habit
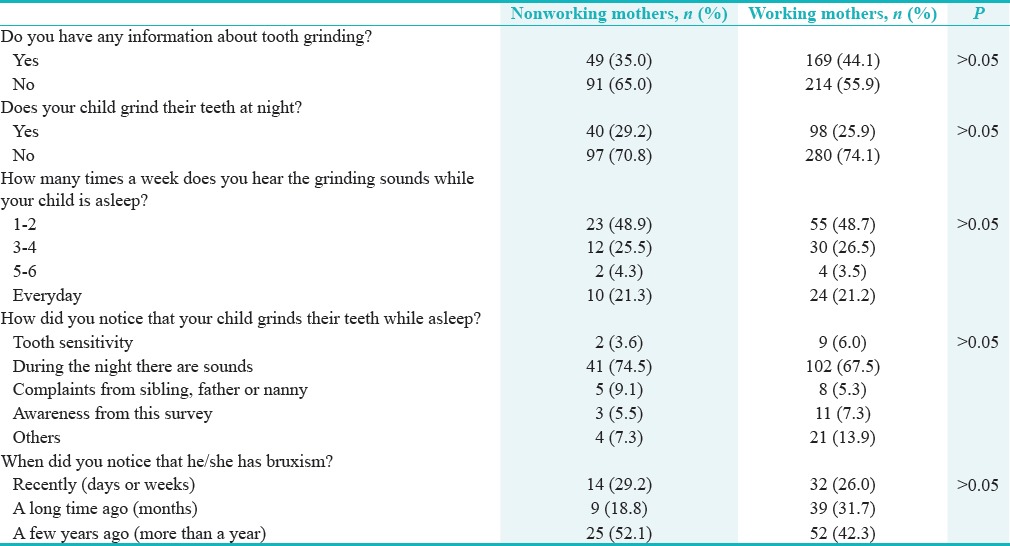
Although NWM were less likely to have information about tooth grinding, they were more cognizant of their child's bruxism status (29.2%). That is, they were more likely to notice sounds during the night when their child grinds their teeth while asleep (74.5%) and have noticed this bruxism for a few years (52.1%). On the other hand, WM were more likely to have more information about tooth grinding (44.1%) also notice the sounds at night while their child slept (67.5%) and had noticed this in the past few years (42.3%). Both WM (48.7%) and NWM (48.9%) have noticed bruxism on average around 1–2 times a week. However, the associations between mothers work status, and their children's bruxism was statistically not significant (P > 0.05) [Table 2].
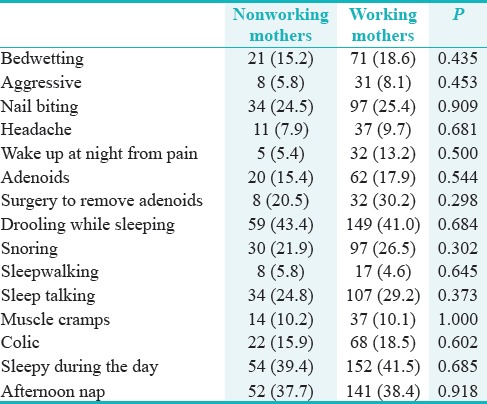
WM's children as compared to NWM children were more likely to be bedwetters, aggressive, nail biters, complain of headaches, wake up at night from pain, have adenoids, have had surgery to remove adenoids, snore, talk while sleeping, have colic (tummy pain), sleepy during the day after returning from school, take an afternoon nap during school days, and think that there is an environmental cause to tooth grinding at night. On the other hand, NWM's children are more likely to drool in their sleep, walk while sleeping, and have muscle cramps. There was no association between mother's work status and factors related to bruxism [Table 4].
Table 4.
Association between mothers work status and factors related to bruxism
Looking further into the habits reported by mothers on both bruxer and nonbruxer children; the former is more likely to be aggressive (P < 0.008), nail biters (P < 0.000), complain of headaches (P < 0.015), nocturnal drooling (P < 0.000), snore (P < 0.001), wake up crying from muscle cramps during the night (P < 0.008), have colic (tummy pain) (P < 0.001), and think environmental cause that might affect and increase their tooth grinding at night [Table 5].
Table 5.
Factors related to bruxism
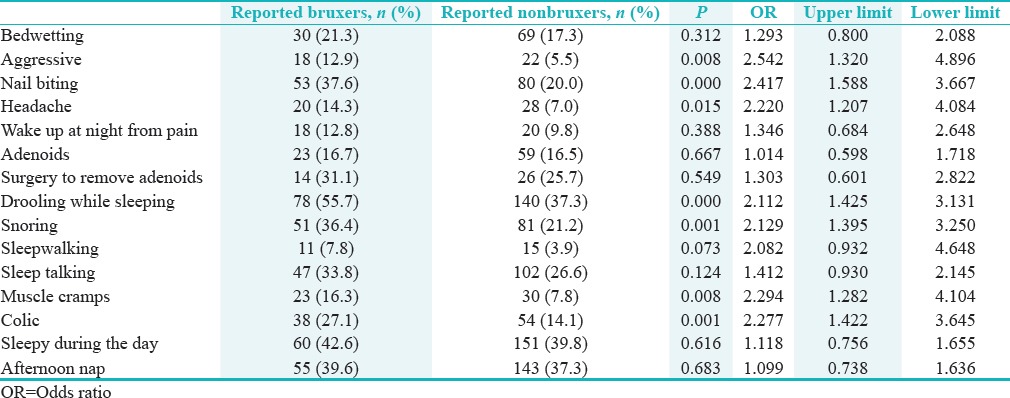
Furthermore, Table 5 reports the OR and the upper and lower limits (based on 95% CI) for each of the 15 habit questions. In the case of reporting aggressive behavior in children, an OR of 2.542 meant the bruxing child had a 2.542 times higher likelihood of being aggressive than a nonbruxing child (P < 0.008). Similarly, a child that bites his/her nails had a 2.417 OR, and therefore, a bruxing child was more than twice as likely to bite its nails than a nonbruxing child.(P < 0.000). A bruxing child that complained of headaches was more than twice as likely to complain of headache as a nonbruxing child (P < 0.015). A bruxing child was more than twice as likely to drool during sleep, snore, complain of muscle cramps, and colic as a nonbruxing child (P < 0.05).
Cronbach's alpha coefficient for the questionnaire was 0.7 meaning that this questionnaire could be used in the future as a possible tool for parents to screen for nocturnal habits in their children.
DISCUSSION
SUMMARY OF KEY FINDINGS
Nearly three quarters, 73% (n = 388), of the participants were WM. Around 35% of the children were reported to grind their teeth nocturnally.
Based on our study, there was no difference on the incidence of bruxism in children according to whether the mother worked or not. However, children with bruxism are more likely to be bedwetters, aggressive, nail biters, complain of headaches, wake up at night from pain, drool, snore, sleepwalking, talking while sleeping, wake up crying from muscle cramps during the night, and have colic (tummy pain). NWM's children are more likely to grind their teeth than WM's children. Habits in children are seen more in WM's children. NWM are less likely to have information about tooth grinding, and both of them agreed that the environmental factors have an effect on teeth bruxism.
This study clearly elucidates that 7 of the 15 habits correlate significantly with a status of bruxism. According to this sample, a child, that is, reported to be aggressive is more than twice as likely to have nocturnal bruxism. Likewise, any child that bites their nails, complains of headaches, drools in their sleep, snores, complains of muscle cramps, and colic is more than twice as likely to be a nocturnal bruxer than a child that does not have these habits.
STRENGTHS AND LIMITATIONS OF THIS STUDY
The strengths of this study were its denotation of both day and sleep habits which occur more in WM's children and their comorbidity with bruxism.
The limitation of this study was the small sample size, it was conducted in a short period, and some of the questionnaires were not completed albeit there was a high rate of compliance 97%. Relation of gender of bruxer children wasnt incorporated in the questionnaire nor the question as to whether the child was a mouth breather or not.
Furthermore, the grading of bruxism for this study was “Possible” as it is based on guardian reports, and not “Probable” when based on self-reports with neither clinical examination nor “Definitive” when based on self-report, clinical examination, and polysomnography. The future studies should aim for a higher grading in the diagnosis for SB in children.[30]
INTERPRETATION AND IMPLICATIONS IN THE CONTEXT OF TOTALITY OF EVIDENCE
The incidence of snoring (36.4%) and drooling (55.7%) in the children that are reposted as bruxists in this study was similar to other studies where the incidence of drooling (25.8%) was more common than snoring (4.5%).[31] In other studies,[14,32,33] the relation between snoring and sleep bruxism was due to increased airway resistance which is considered a symptom of obstructive sleep apnea that arouses masticatory muscle activity which in turn triggers bruxism.[33,34]
Weideman's study showed 5 factors including nocturnal muscle cramps, bedwetting, colic, drooling while asleep and sleep talking which occurred in association with bruxism.[16]
On a cross-sectional study conducted in Brazil including 12–14-year-old school children (n = 1.094) there was a strong association between sleep bruxism (SB) and parafunctional habits (OR = 1.7, 95% CI = 1.1–2.9). Among the parafunctional habits included nail/pen/pencil/lip/cheek biting, resting your head on your hand, and habitual gum chewing.[34] In this study, nail biting was indeed one of the habits, whereby a bruxing child was more than twice as likely to bite his/her nails than a child that had no bruxism.
In a study based in Tehran, nail biting was the most frequent habit with the prevalence of 12.5%.[31] Consequently, this study the prevalence was 37.6% with the most common habit being drooling at 55.7%.
Self-reported waking state oral parafunctional behaviors, including but not limited to day time clenching and nail biting, from (n = 94) in Buffalo New york, were statistically significant in association with anxiety, depression, pain intensity, and pain-related TMD.[35]
Children with headache complaints are 1.5 times more likely to develop bruxism, in comparison to those who did not complain of any headaches[36,37] as seen in this study (14.3%) where they were more than twice as likely to develop bruxism.
In an observational study conducted on 626 patients in Rome on participants aged between 20 and 70, the prevalence of parafunctional activities noted was 75.4% (n = 472) and headache 76.7% (n = 480).[38]
Temporomandibular joint disorders include both the myofascial muscles as well as the joint aspect of the disorder, this study in Spain (n = 154) investigated the impact of TMD with joint pain, TMD with muscle pain and mixed pain TMD on the quality of life, the mixed TMD had a higher impact of headache (P < 0.001) on the quality of life, and the muscle pain group had a higher headache impact than the joint pain group.[39]
From a retrospective analytical study of around a 1000 patients at the orofacial pain and TMD clinic in Brazil, aged between 12 and 83, those that had headaches were nearly twice (OR = 1.96, CI = 1.41–2.74) as likely to present with TMD (P < 0.01).[40]
In an epidemiological retrospective cohort conducted in Madrid Spain, (n = 62) on females aged between 24 and 58, those with myofascial pain, and TMD had higher risk of comorbidities including but not limited to eye disease fatigue, headaches, tinnitus, joint pain, and stiffness among others compared to their age-matched controls.[41]
Bahman also stated that there was a direct relationship between bruxism and sleepwalking 3.2%.[31] Weideman also showed that children talking during sleep were more likely to be bruxers.[16] Another study said that children who drooled and sleep talked were 1.7 and 1.6 times more likely to be bruxers than other children who did not have these habits.[42]
Goettems et al. 2017[43] investigated over 500 mothers and the effect of their mental well-being as well as any stressful environmental factors on its impact on their children, it was reported that the presence of major depressive disorder and existence of stressful events more importantly environmental changes had a significant association with bruxism in children. In this study, the mothers work status could present as a stressful environmental factor for children, and thus, the many habits seen in WM children which are associated with Bruxism. Hence, a child's emotional status and environment may be attributed to bruxism as more than half the mothers (59.4%) in this study have.
This case–control study[44] of over 300 adolescent participants in Brazil showed a clear relationship between history of verbal abuse (verbal school bullying) and its impact on nocturnal bruxism. This all leads to a possibility that SB might occur more commonly in children whose environment is not as relaxed and supportive as should be for the well-being of the child might induce or even predispose sleep bruxism. If there is any tangible tension at home, or at school, children might show habits that root to bruxism.
In a meta-analysis of 14 articles from an initial 5637,[45] the following behaviors or habits mostly precluded to bruxism; snoring, mouth breathing, restless sleep, drooling, stomach position during sleep, and lack of sleep were the risk factors related to bruxism in children. In this study, snoring and drooling were statistically significant to the incidence of SB.
Another study in Brazil, of children aged 6–17 years from a sample of n = 76, showed that those with TMD scored higher and was statistically significant on the multidimensional anxiety scale for children. This scale is based on physical symptoms, harm avoidance, social anxiety, and separation/panic.[46]
A study on 11–15-year-old adolescent students (n = 1.415) in Japan showed that the ORs of those that often ground their teeth at night (nocturnal grinder) to exhibit TMD were 2.58 (CI = 1.14–5.87) P < 0.05. Furthermore, 12.9% of the participants had at least one TMD symptom.[21]
Implication of subclinical muscle inflammation involved in TMD myalgia pathophysiology masseter muscle cytokines levels increased in TMD participants versus controls.[47]
A Systematic Review on the etiology of temporomandibular Joint disorders was conducted on studies from 1980 to 2014, 54 articles were deemed suitable, and a concordance was reached onto the multifactorial etiology of TMD, as well as a prospective worsening of TMD symptoms (pain, psychological discomfort, physical disability, and limitation of mandibular movement) in terms of chronicity and abrogating the quality of life. Authors recommend vigilance in identifying possible etiological factors that initiated, perpetuated or even aggravated the situation together with their degree of involvement to abate detrimental symptoms of TMD.[48]
This all leads to a consensus that a disruption in a child's psychological well-being is mirrored in their habits be it daytime and or nocturnal; a silent cry for help that if not addressed will prospectively affect their quality of life.
CONTROVERSIES RAISED BY THIS STUDY
In Bahman's study,[31] he found a strong relation between mother's work and the children's bruxism by 47.6% of full-time mothers and self-employed mothers. Based on our study, the result was the opposite by showing that the mother's work did not have an effect on children's bruxism, in fact, the reported children with bruxism was 29.2% for NWM verses 25.9% for WM. These results, however, are controversial as WM's children had significantly more habits than NWM's children. To elaborate, these habits in bruxer children were statistically significant, and 7 of them were indicators of the presence of bruxism. Could these results be biased by the fact that WM were less aware of their children's sleeping routine as they were preoccupied with work and their limited time at home as compared to a homemaker mother who is more cognizant of her main environment which is home?
Future Research Directions (for this particular research collaboration, underlying mechanism, and clinical research).
In the literature, there are not many published studies that highlight the relationship between the mother's work status and children's bruxism. There is a definitive need to explore this topic in greater detail and number.
Future research will inevitably pursue collaboration with pediatrics, psychiatry, and sleep medicine among others to design observational studies procuring a higher grading system for sleep bruxism together with objective psychological and behavioral appraisals of the study participants. This will help illustrate the principles of children's behavior and delineate the factors that disable the natural balance of harmony in their lives.
CONCLUSION
The prevalence of children's bruxism in this convenient sample was 34.5%. The WM's children had more habits associated with a parasomnia compared to the NWM's children 44.1%. The most common habit related to bruxism while asleep was drooling. Similarly, a child that is aggressive, bites their nails, complains of headaches, drools in their sleep, snores, complains of muscle cramps, and colic is more than twice as likely to be a nocturnal bruxer than a child that does not have these habits. The concerning habits can serve the pediatric dentist, general dentist, general practitioner, and primary care provider of children having these red flags as indicators of bruxism. It is imperative that parents of these children be made aware of these habits and assesses their child's environment both at home and school to detect any recent changes that might be rocking the harmony in their child's life. They need to be cognizant that these habits may occur together, alone or even simultaneously with Bruxism. Parents need to self-evaluate their home environment as well as child's school environment for any concerns that might be inducing, perpetuating or even aggravating their child's SB. Hearing a child grinding their teeth at night is not “normal” or a deviation of normal, it is in fact in our opinion a red flag of an underlying disruption in the child's day-to-day life. It is recommended that the parents and/or guardians of the child should seek a multidisciplinary approach in dealing with the child's concerning behavior through consultation with a pediatric dentist, orofacial pain specialist, pediatric psychiatrist, and psychologist.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
REFERENCES
- 1.Shetty S, Pitti V, Satish Babu CL, Surendra Kumar GP, Deepthi BC. Bruxism: A literature review. J Indian Prosthodont Soc. 2010;10:141–8. doi: 10.1007/s13191-011-0041-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Burton C. Thesis. University of Sydney; 1983. Bruxism. [Google Scholar]
- 3.Braham LR, Morris ME. Textbook of Pediatric Dentistry. 2nd ed. Delhi: CBS Publishers & Distributors; 1990. Oral habits and their management; p. 654. [Google Scholar]
- 4.Manfredini D, Lobbezoo F. Role of psychosocial factors in the etiology of bruxism. J Orofac Pain. 2009;23:153–66. [PubMed] [Google Scholar]
- 5.Kato T, Rompré P, Montplaisir JY, Sessle BJ, Lavigne GJ. Sleep bruxism: An oromotor activity secondary to micro-arousal. J Dent Res. 2001;80:1940–4. doi: 10.1177/00220345010800101501. [DOI] [PubMed] [Google Scholar]
- 6.Huynh N, Kato T, Rompré PH, Okura K, Saber M, Lanfranchi PA, et al. Sleep bruxism is associated to micro-arousals and an increase in cardiac sympathetic activity. J Sleep Res. 2006;15:339–46. doi: 10.1111/j.1365-2869.2006.00536.x. [DOI] [PubMed] [Google Scholar]
- 7.Machado E, Dal-Fabbro C, Cunali PA, Kaizer OB. Prevalence of sleep bruxism in children: A systematic review. Dental Press J Orthod. 2014;19:54–61. doi: 10.1590/2176-9451.19.6.054-061.oar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kostrzewa-Janicka J, Jurkowski P, Zycinska K, Przybyłowska D, Mierzwińska-Nastalska E. Sleep-related breathing disorders and bruxism. Adv Exp Med Biol. 2015;873:9–14. doi: 10.1007/5584_2015_151. [DOI] [PubMed] [Google Scholar]
- 9.Ali NJ, Pitson DJ, Stradling JR. Snoring, sleep disturbance, and behaviour in 4-5 year olds. Arch Dis Child. 1993;68:360–6. doi: 10.1136/adc.68.3.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dahl RE. The impact of inadequate sleep on children's daytime cognitive function. Semin Pediatr Neurol. 1996;3:44–50. doi: 10.1016/s1071-9091(96)80028-3. [DOI] [PubMed] [Google Scholar]
- 11.Lavigne JV, Arend R, Rosenbaum D, Smith A, Weissbluth M, Binns HJ, et al. Sleep and behavior problems among preschoolers. J Dev Behav Pediatr. 1999;20:164–9. doi: 10.1097/00004703-199906000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Kim DS, Lee CL, Ahn YM. Sleep problems in children and adolescents at pediatric clinics. Korean J Pediatr. 2017;60:158–65. doi: 10.3345/kjp.2017.60.5.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Góis EG, Ribeiro HC, Júnior, Vale MP, Paiva SM, Serra-Negra JM, Ramos-Jorge ML, et al. Influence of nonnutritive sucking habits, breathing pattern and adenoid size on the development of malocclusion. Angle Orthod. 2008;78:647–54. doi: 10.2319/0003-3219(2008)078[0647:IONSHB]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 14.Sjöholm TT, Lowe AA, Miyamoto K, Fleetham JA, Ryan CF. Sleep bruxism in patients with sleep-disordered breathing. Arch Oral Biol. 2000;45:889–96. doi: 10.1016/s0003-9969(00)00044-3. [DOI] [PubMed] [Google Scholar]
- 15.Giannasi LC, Santos IR, Alfaya TA, Bussadori SK, Leitão-Filho FS, de Oliveira LV, et al. Effect of a rapid maxillary expansion on snoring and sleep in children: A pilot study. Cranio. 2015;33:169–73. doi: 10.1179/2151090314Y.0000000029. [DOI] [PubMed] [Google Scholar]
- 16.Weideman CL, Bush DL, Yan-Go FL, Clark GT, Gornbein JA. The incidence of parasomnias in child bruxers versus nonbruxers. Pediatr Dent. 1996;18:456–60. [PubMed] [Google Scholar]
- 17.Bader G, Lavigne G. Sleep bruxism; an overview of an oromandibular sleep movement disorder. Review article. Sleep Med Rev. 2000;4:27–43. doi: 10.1053/smrv.1999.0070. [DOI] [PubMed] [Google Scholar]
- 18.Malki GA, Zawawi KH, Melis M, Hughes CV. Prevalence of bruxism in children receiving treatment for attention deficit hyperactivity disorder: A pilot study. J Clin Pediatr Dent. 2004;29:63–7. doi: 10.17796/jcpd.29.1.3j86338656m83522. [DOI] [PubMed] [Google Scholar]
- 19.Cash RC. Bruxism in children: Review of the literature. J Pedod. 1988;12:107–27. [PubMed] [Google Scholar]
- 20.Pingitore G, Chrobak V, Petrie J. The social and psychologic factors of bruxism. J Prosthet Dent. 1991;65:443–6. doi: 10.1016/0022-3913(91)90240-w. [DOI] [PubMed] [Google Scholar]
- 21.Karibe H, Shimazu K, Okamoto A, Kawakami T, Kato Y, Warita-Naoi S, et al. Prevalence and association of self-reported anxiety, pain, and oral parafunctional habits with temporomandibular disorders in Japanese children and adolescents: A cross-sectional survey. BMC Oral Health. 2015;15:8. doi: 10.1186/1472-6831-15-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.List T, Wahlund K, Larsson B. Psychosocial functioning and dental factors in adolescents with temporomandibular disorders: A case-control study. J Orofac Pain. 2001;15:218–27. [PubMed] [Google Scholar]
- 23.Kröner-Herwig B, Gassmann J. Headache disorders in children and adolescents: Their association with psychological, behavioral, and socio-environmental factors. Headache. 2012;52:1387–401. doi: 10.1111/j.1526-4610.2012.02210.x. [DOI] [PubMed] [Google Scholar]
- 24.Brattberg G. Do pain problems in young school children persist into early adulthood? A 13-year follow-up. Eur J Pain. 2004;8:187–99. doi: 10.1016/j.ejpain.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 25.Vierola A, Suominen AL, Eloranta AM, Lintu N, Ikävalko T, Närhi M, et al. Determinants for craniofacial pains in children 6-8 years of age: The PANIC study. Acta Odontol Scand. 2017;75:453–60. doi: 10.1080/00016357.2017.1339908. [DOI] [PubMed] [Google Scholar]
- 26.Fisher BE, Pauley C, McGuire K. Children's sleep behavior scale: Normative data on 870 children in grades 1 to 6. Percept Mot Skills. 1989;68:227–36. doi: 10.2466/pms.1989.68.1.227. [DOI] [PubMed] [Google Scholar]
- 27.Minnesota Regional Sleep Disorders Center, Hennepin County Medical Center: Pediatric Questionnaire. Hennepin, MN. 1991 [Google Scholar]
- 28.Lindqvist B. Bruxism and emotional disturbance. Odontol Revy. 1972;23:231–42. [PubMed] [Google Scholar]
- 29.Dillman D. Mail and Telephone Surveys: The Total Design Method. Washington: John Wiley & Sons, Inc; 1977. [Google Scholar]
- 30.Lobbezoo F, Ahlberg J, Glaros AG, Kato T, Koyano K, Lavigne GJ, et al. Bruxism defined and graded: An international consensus. J Oral Rehabil. 2013;40:2–4. doi: 10.1111/joor.12011. [DOI] [PubMed] [Google Scholar]
- 31.Seraj B, Shahrabi M, Ghadimi S, Ahmadi R, Nikfarjam J, Zayeri F, et al. The prevalence of bruxism and correlated factors in children referred to dental schools of Tehran, based on parent's report. Iran J Pediatr. 2010;20:174–80. [PMC free article] [PubMed] [Google Scholar]
- 32.Sheldon SH, editor. Sleep Medicine Clinics. Philadelphia: Elsevier; 2010. Obstructive sleep apnea and bruxism in children; pp. 163–8. [Google Scholar]
- 33.Itani O, Kaneita Y, Ikeda M, Kondo S, Yamamoto R, Osaki Y, et al. Disorders of arousal and sleep-related bruxism among Japanese adolescents: A nationwide representative survey. Sleep Med. 2013;14:532–41. doi: 10.1016/j.sleep.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 34.Fernandes G, Franco-Micheloni AL, Siqueira JT, Gonçalves DA, Camparis CM. Parafunctional habits are associated cumulatively to painful temporomandibular disorders in adolescents. Braz Oral Res. 2016;30:pii: S1806-83242016000100214. doi: 10.1590/1807-3107BOR-2016.vol30.0015. [DOI] [PubMed] [Google Scholar]
- 35.Khawaja SN, Nickel JC, Iwasaki LR, Crow HC, Gonzalez Y. Association between waking-state oral parafunctional behaviours and bio-psychosocial characteristics. J Oral Rehabil. 2015;42:651–6. doi: 10.1111/joor.12302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nahás-Scocate AC, Coelho FV, de Almeida VC. Bruxism in children and transverse plane of occlusion: Is there a relationship or not? Dental Press J Orthod. 2014;19:67–73. doi: 10.1590/2176-9451.19.5.067-073.oar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Simoes-Zenari M, Bitar ML. Factors associated to bruxism in children 4-6 years. Pro Fono. 2010;22:465–72. doi: 10.1590/s0104-56872010000400018. [DOI] [PubMed] [Google Scholar]
- 38.Franco R, Basili M, Venditti A, Chiaramonte C, Ottria L, Barlattani A, Jr, et al. Statistical analysis of the frequency distribution of signs and symptoms of patients with temporomandibular disorders. Oral Implantol (Rome) 2016;9:190–201. doi: 10.11138/orl/2016.9.4.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gil-Martínez A, Grande-Alonso M, López-de-Uralde-Villanueva I, López-López A, Fernández-Carnero J, La Touche R, et al. Chronic temporomandibular disorders: Disability, pain intensity and fear of movement. J Headache Pain. 2016;17:103. doi: 10.1186/s10194-016-0690-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ferreira CL, Silva MA, Felício CM. Signs and symptoms of temporomandibular disorders in women and men. Codas. 2016;28:17–21. doi: 10.1590/2317-1782/20162014218. [DOI] [PubMed] [Google Scholar]
- 41.de-Pedro-Herráez M, Mesa-Jiménez J, Fernández-de-Las-Peñas C, de-la-Hoz-Aizpurua JL. Myogenic temporomandibular disorders: Clinical systemic comorbidities in a female population sample. Med Oral Patol Oral Cir Bucal. 2016;21:784–92. doi: 10.4317/medoral.21249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cheifetz AT, Osganian SK, Allred EN, Needleman HL. Prevalence of bruxism and associated correlates in children as reported by parents. J Dent Child (Chic) 2005;72:67–73. [PubMed] [Google Scholar]
- 43.Goettems ML, Poletto-Neto V, Shqair AQ, Pinheiro RT, Demarco FF. Influence of maternal psychological traits on sleep bruxism in children. Int J Paediatr Dent. 2017;27:469–75. doi: 10.1111/ipd.12285. [DOI] [PubMed] [Google Scholar]
- 44.Serra-Negra JM, Pordeus IA, Corrêa-Faria P, Fulgêncio LB, Paiva SM, Manfredini D, et al. Is there an association between verbal school bullying and possible sleep bruxism in adolescents? J Oral Rehabil. 2017;44:347–53. doi: 10.1111/joor.12496. [DOI] [PubMed] [Google Scholar]
- 45.Guo H, Wang T, Li X, Ma Q, Niu X, Qiu J, et al. What sleep behaviors are associated with bruxism in children? A systematic review and meta-analysis. SSleep Breath. 2017;21:1013–23. doi: 10.1007/s11325-017-1496-3. [DOI] [PubMed] [Google Scholar]
- 46.Kobayashi FY, Gavião MB, Marquezin MC, Fonseca FL, Montes AB, Barbosa TS, et al. Salivary stress biomarkers and anxiety symptoms in children with and without temporomandibular disorders. Braz Oral Res. 2017;31:e78. doi: 10.1590/1807-3107BOR-2017.vol31.0078. [DOI] [PubMed] [Google Scholar]
- 47.Louca Jounger S, Christidis N, Svensson P, List T, Ernberg M. Increased levels of intramuscular cytokines in patients with jaw muscle pain. J Headache Pain. 2017;18:30. doi: 10.1186/s10194-017-0737-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chisnoiu AM, Picos AM, Popa S, Chisnoiu PD, Lascu L, Picos A, et al. Factors involved in the etiology of temporomandibular disorders – A literature review. Clujul Med. 2015;88:473–8. doi: 10.15386/cjmed-485. [DOI] [PMC free article] [PubMed] [Google Scholar]


