Abstract
Background:
The transalveolar extraction and the use of pharmacological antibiotic therapy following the surgical procedure in management of postoperative infection go hand in hand in minor oral surgery. Attention has often been focused on antibiotic therapy administered at different time schedules (before or after surgery or both). This investigation reveals how the use of different molecules and dosages is critical in the postoperative period and has always provided positive result.
Methodology:
A prospective randomized study was carried out in 100 healthy controls of age group 20–50 years undergoing transalveolar extraction in the Department of Oral and Maxillofacial Surgery, Vivekanandha Dental College for Women. A 5-day regimen of amoxicillin or ciprofloxacin group of antibiotics along with regular analgesics was administered to the patients following transalveolar extraction. The patients were evaluated for postoperative infection, inflammation and wound care on postoperative days: day zero, day 2, day 5, day 7, day 15, day 30, and analyzed. A P < 0.05 was considered statistically significant.
Results and Conclusion:
A total of 100 patients aged 23–50 years (24.6–4.43) met the inclusion criteria. Male accounted for 44, while female were 55, giving male:female ratio 1:1.4. Postoperative infection was minimum with ciprofloxacin group as compared to amoxicillin group and was more significant (P < 0.005) on evaluation. A complete review has also been taken into an account, various strategies used such as surgical flaps, no traumatic osteotomy, and primary or secondary closure.
Keywords: Wound healing, Post operative complication, Infection control
INTRODUCTION
Antibiotics are frequently used in dental practice.[1] The discovery of antibiotics occurred in 1929 by Scottish bacteriologist Alexander Fleming, and he reported on the antibacterial action of cultures of a Penicillium species. Antibiotics are the greatest contribution of the 20th century to the field of therapeutics.[2,3] Clinical and bacteriological and epidemiological factors determine the indication of antibiotic usage in dentistry. Antibiotics are used as an adjuvant to aid the host defense in the elimination of remaining bacteria.[4,5]
In Altemeier's classification, oral surgery is often graded as Class II (clean-contaminated surgery), with a rate of local infection of 5%–15% without antibiotics and <7% with antibiotics.[6] Postoperative infection management and appropriate wound healing are utmost important in oral surgery. To prevent local infection, as the target microbiota is usually polymicrobial in nature and these infections originate from the possible surgical contamination/infection from the normal microbiota of the mouth and saliva, and from dental pathogens in the periodontal disease, thus, postoperative antibiotic usage is inexorable.[7]
Judicious use of antibiotics following surgical therapy is the most appropriate method to treatment. Narrow spectrum antibiotics should be considered the first choice as it produces less alterations in the gastrointestinal tract.[1] There is often a dilemma among the dental practitioners concerning the use of antibiotics in conjunction with dental procedures. In this article, we have compared the efficacy of ciprofloxacin over amoxicillin as a primary antibiotic following transalveolar extraction.
METHODOLOGY
A prospective randomized clinical study was carried out in the department of oral and maxillofacial surgery at our institution on 100 patients who underwent surgical removal of impacted mandibular third molar teeth. Patient with previous medical aliments was excluded from the study. A 5-day regimen of amoxicillin or ciprofloxacin group of antibiotics along with NSAID’S was administered following surgical procedure and the patients were evaluated for postoperative inflammation and wound care. All the patients included in the study were followed up during 1st, 3rd, 5th, 7th, 15th, 30th postoperative days.
Study design
Based on the type of postoperative antibiotics, the participants were randomly divided into Group A (50) and Group B (50).
Group A: Patients received only amoxicillin (500 mg) eighth hourly for 5 days in the postoperative period.
Group B: Patients received ciprofloxacin (250 mg) eighth hourly for 5 days in the postoperative period.
Criteria to assess infection
The operative site was classified as infected if following signs or symptoms were observed within 6 weeks of surgery postoperatively.
Local evidence of infection
Purulent discharge from surgical site.
If any infections occurred during the follow-up period, the patient was treated for the same by prescribing empirical antibiotics.
Statistical analysis
The statistical analysis carried out using paired t-test.
RESULTS
A total of 100 patients aged 23–50 years (24.6–4.43) met the inclusion criteria. Male accounted for 44, while female were 55, giving male:female ratio 1:1.4. Group A with a mean age of 31.81 years and standard deviation of 10.947 and in Group B with mean age of 33.14 years and standard deviation of 6.967.
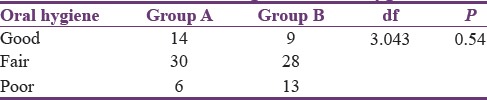
Status of oral hygiene
In Group A, oral hygiene was evaluated to be poor (n = 6), fair (n = 30), and Good (n = 14); and in Group B as poor (n = 9), fair (n = 28), and good (n = 13). The distribution of individuals with relation tically significant [Table 1].
Table 1.
Wound healing versus oral hygiene
Presence/absence of habits
Habits such as alcohol consumption, cigarette smoking, and/or chewing paan or gutka were recorded. Of all the patients in the study, adverse habits were recorded in three patients in Group A and six patients in Group B. This difference was not significant statistically.
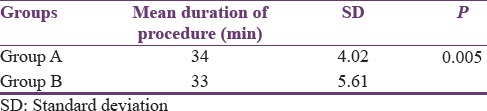
Time duration of wound healing of extraction socket
The time taken for healing of extraction socket was recorded in days. Of the patients, in Group A, the mean duration was 5.32 days, and in Group B, it was 6.72 days. This difference was significant statistically [Table 2].
Table 2.
Time duration versus wound healing
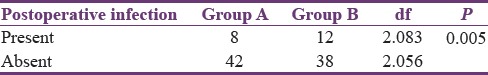
Postoperative infection rates
Of the 50 patients in Group A, 4 patients were infected and they accounted for 8% of cases within the group. In Group B, of the 6 patients were infected which accounted for 12% of cases within the group. The infection rates between these two groups were found to be statistically insignificant [Table 3].
Table 3.
Post operative infection rate
DISCUSSION
Tooth extraction is a surgical treatment to remove teeth that are affected by decay or gum disease. The other common reason for tooth extraction, performed by oral surgeons, is to remove wisdom teeth that are poorly aligned/partially impacted third molars or those causing pain or inflammation.[8] To prevent infection, the following two factors should be achieved: first, decreasing bacterial load in the surgical wound, and second, improving host defenses to prevent the bacteria that inevitably enter the wound from causing clinically evident infection.[1] As transalveolar extraction is often graded as Class II surgery (clean-contaminated surgery), the expected infection rate in clean-contaminated surgery is 10%–15%.
The most important principle in antibiotic prophylaxis is to administer the antibiotic at a time that provides high blood and tissue levels at the time of anticipated bacterial contamination of the wound. This was established by experimental studies of dermal lesions in guinea pigs in which it was found that there is a decisive period of up to 3 h after bacterial contamination during which antibiotics will prevent an infective lesion from developing.[9]
In our survey, amoxicillin was the antibiotic of first choice among dentists with a prescription rate of 45.7%.[10] Second came a combination of amoxicillin with clavulanic acid at 33.7%.[11] Ciprofloxacin was used by 14.5% of dentists. Interestingly, none of the respondents used metronidazole or a combination.
In our study, we found infection rates of 8% and 12% in Groups A (ciprofloxacin) and B (amoxicillin), respectively, suggestive of type of postoperative antibiotics has mild significance in the management of postoperative infection in transalveolar extraction. When the patient is presenting with substance abuse and habits such as smoking, it potentially alter homeostasis and the immune system, causing psychological, and physical alterations. Another contributing factor for postsurgical complications are malnutrition and behavioral issues.
ACOFS, it has been proven that prolonging antibiotic administration postsurgically does not decrease the incidence of wound infection. For short procedures, a single dose of amoxicillin preoperatively is sufficient to prevent wound infection. For longer procedures, intraoperative doses are given as necessary, followed by final dose in the POD1 and 2 is sufficient for maximum infection control.
We came across patients with inflammatory complications such as dry socket, erythema, pain and purulent discharge from the surgical site. Postoperative inflammatory complications after transalveolar extractions are reported to occur with frequencies up to 10%. In the study, we observed a postoperative infection rate of 12%, and this is consistent with other studies.[12,13]
Another important contributory factor for developing infection is time or duration of the procedure and manipulation of soft tissue. The mean duration time of procedure was 32.7 min and wound healing was 5.7 days. Although the main reason for delayed wound healing was social status, habits, and malnutrition during postoperative period, we observed that among all those patients whose duration of surgery was less than or equal to 20 min had less chance of developing infection. Only 6.9% of patients who were operated within 25 min had infection whereas 7.6% of the patients who were operated more than 30 min had infection, implying that increased duration of procedure also attributed to develop infection or postoperative complication.[14,15,16]
There are certain limitations in our study that should be addressed. As our sample was limited to the patients in and around our locality, the review was biased toward early discovery, so minor or insignificant infections were included in this study.
CONCLUSION
Our results are consistent with the previous study. The use of post opeative ciprofloxacin dose has statistically mild significant effect on management of postoperative infection rates in transalveolar extraction. Perioperative prophylactic amoxicillin have been proven to lower infection rates postoperatively and are in wide use. Larger studies with improved control of confounding variables may still need to be conducted to further prove this hypothesis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ramu C, Padmanabhan TV. Indications of antibiotic prophylaxis in dental practice- review. Asian Pac J Trop Biomed. 2012;2:749–54. doi: 10.1016/S2221-1691(12)60222-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thomas DW, Satterthwaite J, Absi EG, Lewis MA, Shepherd JP. Antibiotic prescription for acute dental conditions in the primary care setting. Br Dent J. 1996;181:401–4. doi: 10.1038/sj.bdj.4809276. [DOI] [PubMed] [Google Scholar]
- 3.Whitten BH, Gardiner DL, Jeansonne BG, Lemon RR. Current trends in endodontic treatment: Report of a national survey. J Am Dent Assoc. 1996;127:1333–41. doi: 10.14219/jada.archive.1996.0444. [DOI] [PubMed] [Google Scholar]
- 4.Pallasch TJ. Antibiotics in endodontics. Dent Clin North Am. 1979;23:737–46. [PubMed] [Google Scholar]
- 5.Abbott PV, Hume WR, Pearman JW. Antibiotics and endodontics. Aust Dent J. 1990;35:50–60. doi: 10.1111/j.1834-7819.1990.tb03028.x. [DOI] [PubMed] [Google Scholar]
- 6.Ragot Jean Pierre. Prescription of antibiotics in odontology and stomatology. Recommendations and Arguments. French agency for health safety products. 2001:8–9. [Google Scholar]
- 7.Loesche WJ, Grossman NS. Periodontal disease as a specific, albeit chronic, infection: Diagnosis and treatment. Clin Microbiol Rev. 2001;14:727–52. doi: 10.1128/CMR.14.4.727-752.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lodi G, Figini L, Sardella A, Carrassi A, Del Fabbro M, Furness S. Antibiotics to prevent complications following tooth extractions. Cochrane Database Syst Rev. 2012;11:CD003811. doi: 10.1002/14651858.CD003811.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Stone IE, Dodson TB, Bays RA. Risk factors for infection following operative treatment of mandibular fractures: A multivariate analysis. Plast Reconstr Surg. 1993;91:64–8. doi: 10.1097/00006534-199301000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Ingham HR, Hood FJ, Bradnum P, Tharagonnet D, Selkon JB. Metronidazole compared with penicillin in the treatment of acute dental infections. Br J Oral Surg. 1977;14:264–9. doi: 10.1016/0007-117x(77)90035-x. [DOI] [PubMed] [Google Scholar]
- 11.Lewis MA, Carmichael F, MacFarlane TW, Milligan SG. A randomised trial of co-amoxiclav (Augmentin) versus penicillin V in the treatment of acute dentoalveolar abscess. Br Dent J. 1993;175:169–74. doi: 10.1038/sj.bdj.4808263. [DOI] [PubMed] [Google Scholar]
- 12.Burke JF. The effective period of preventive antibiotic action in experimental incisions and dermal lesions. Surgery. 1961;50:161–8. [PubMed] [Google Scholar]
- 13.Iizuka T, Lindqvist C, Hallikainen D, Paukku P. Infection after rigid internal fixation of mandibular fractures: A clinical and radiologic study. J Oral Maxillofac Surg. 1991;49:585–93. doi: 10.1016/0278-2391(91)90340-r. [DOI] [PubMed] [Google Scholar]
- 14.Gordon PE, Lawler ME, Kaban LB, Dodson TB. Mandibular fracture severity and patient health status are associated with postoperative inflammatory complications. J Oral Maxillofac Surg. 2011;69:2191–7. doi: 10.1016/j.joms.2011.03.071. [DOI] [PubMed] [Google Scholar]
- 15.Webb LS, Makhijani S, Khanna M, Burstein MJ, Falk AN, Koumanis DJ, et al. A comparison of outcomes between immediate and delayed repair of mandibular fractures. Can J Plast Surg. 2009;17:124–6. doi: 10.1177/229255030901700401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maloney PL, Lincoln RE, Coyne CP. A protocol for the management of compound mandibular fractures based on the time from injury to treatment. J Oral Maxillofac Surg. 2001;59:879–84. doi: 10.1053/joms.2001.25021. [DOI] [PubMed] [Google Scholar]


