Abstract
Brain metastases from gastrointestinal malignancies are exceedingly rare occurrences that carry a very poor prognosis. This holds especially true in cases where brain metastases from esophageal primaries are the initial presentation of a previously unidentified gastrointestinal malignancy. Our patient, a 60-year-old male with a past history of a right temporal teratoma, family history of breast cancer, and no smoking history, presented with a chief complaint of recurrent headaches. His history of present illness and physical examination included a two-month history of frontal headache, progressive fatigue, and unintentional weight loss. He underwent an extensive initial workup including CT-head, CT-abdomen/pelvis, CT-chest, bone scan, tumor marker analysis, and MRI-brain. The initial head CT revealed multiple intracranial lesions suspicious for malignancy. A PET scan later revealed his primary to be a malignancy of the distal esophagus. His treatment course thus far has been aggressive, consisting of surgical resection, systemic chemotherapy with capcetibine-oxaliplatin as well as paclitaxel-carboplatin, and radiation therapy. He has had several recurrences since starting treatment, but has continued to maintain a good performance status with only minor symptoms. Currently, the patient has survived for 17 months after his diagnosis of stage IV (T3, N2, M1) moderately differentiated adenocarcinoma and is undergoing treatment with trastuzumab and stereotactic radiosurgery. This report demonstrates that although cases of esophageal adenocarcinoma that present as brain metastases typically carry a poor prognosis, with early and aggressive treatment patients can survive well past one year after diagnosis.
Keywords: Gastroesophageal cancer, Brain metastases, Cancer of unknown primary, Central nervous system, Survival
Introduction
Brain metastases from gastrointestinal malignancies are a rare occurrence, seen in <4% of all tumors of the gastrointestinal tract [1]. Rarer still are brain metastases from esophageal tumors (BMET), which are seen in only 1–3% of cases of esophageal carcinoma [2]. The survival of patients with BMET is generally very poor, with a reported 1-year survival rate of 14%, and a median survival of 9.6 months in patients undergoing surgery and adjuvant radiation therapy [3]. Although the prognosis of patients with BMET is poor, early and aggressive treatment of these metastases may play a role in prolonging the survival of these patients.
Case Description
A 60-year-old male presented to the Bay Regional Medical Center with a history of fatigue lasting for several days, a 20-lb weight loss over the past 2 months, one episode of painless hematuria, and persistent headache for the past several weeks. He denied any diplopia, blurry vision, nausea, emesis, weakness, abdominal pain, blood in stool, cough, shortness of breath, alcohol use, drug use, or tobacco use. On physical examination, there was a slight bony defect noted on the lateral aspect of his right supraorbital ridge consistent with the prior resection of a temporal teratoma. His past medical history includes the surgical removal of a benign temporal teratoma and a teratoma in the right knee at the ages of 2 and 30 years, respectively. He has a family history of breast cancer in his mother and maternal grandmother. CT imaging of the head with contrast showed multiple lesions in the right frontal lobe suspicious for malignancy. CT scans of the chest, abdomen, and pelvis were negative for any primary tumor source. The patient was subsequently admitted to St. Mary's of Michigan, where laboratory testing were done including comprehensive metabolic panel, complete blood count, and liver function tests which were all within normal limits.
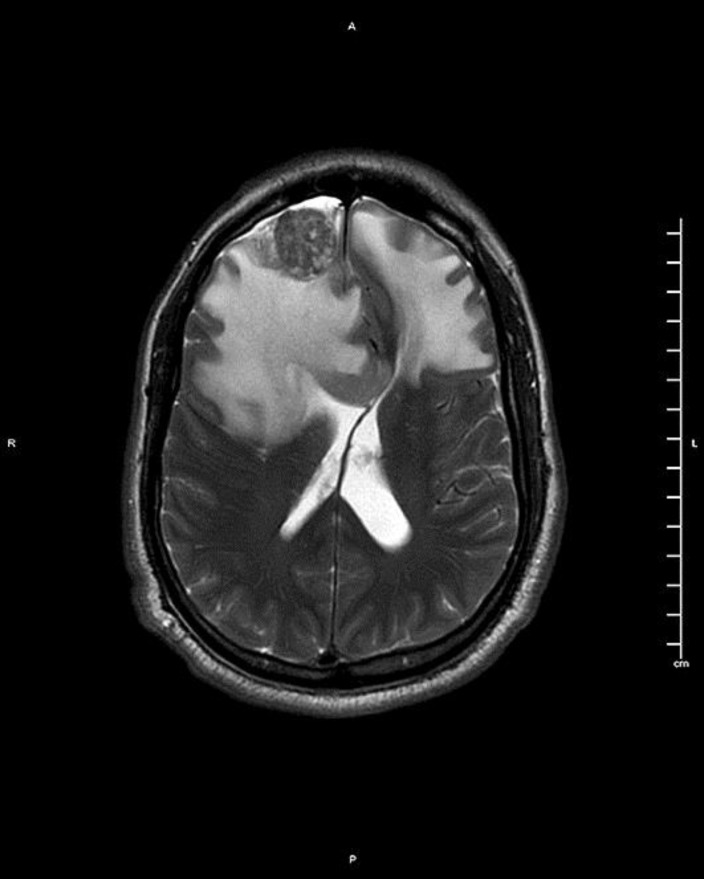
An MRI with contrast was obtained to further characterize the brain lesions and showed 4 lesions with diameters of 2.6, 1.0, 1.8, and 0.9 cm as well as vasogenic edema and an anterior midline shift of 9 mm (Fig. 1). Bone scan, scrotal duplex ultrasound, urine cytology, and diagnostic cystoscopy were all negative for any evidence of malignant processes. Three days after admission, the patient underwent diagnostic and therapeutic right frontal craniotomy for the resection of the largest mass (2.6 cm in diameter) in the right frontal lobe. The operation was successful in obtaining a gross total resection, and his recovery from surgery was uneventful. Pathologic analysis revealed the mass to be a moderately differentiated adenocarcinoma staining HER-2/neu positive, CK7 positive, CK20 positive, TTF-1 negative, and PSA negative. With no apparent source of the multiple brain metastases, the patient was diagnosed with adenocarcinoma of unknown primary site. He was discharged four days after admission and received a PET-CT in the subsequent weeks which identified a region of intense activity (18 SUV) at the distal esophagus and gastroesophageal junction (GEJ) that was identified as being highly suspect for underlying esophageal carcinoma.
Fig. 1.
MRI-brain T2-weighted image showing an anterior frontal lobe intracranial mass lesion and extensive vasogenic edema with midline shift.
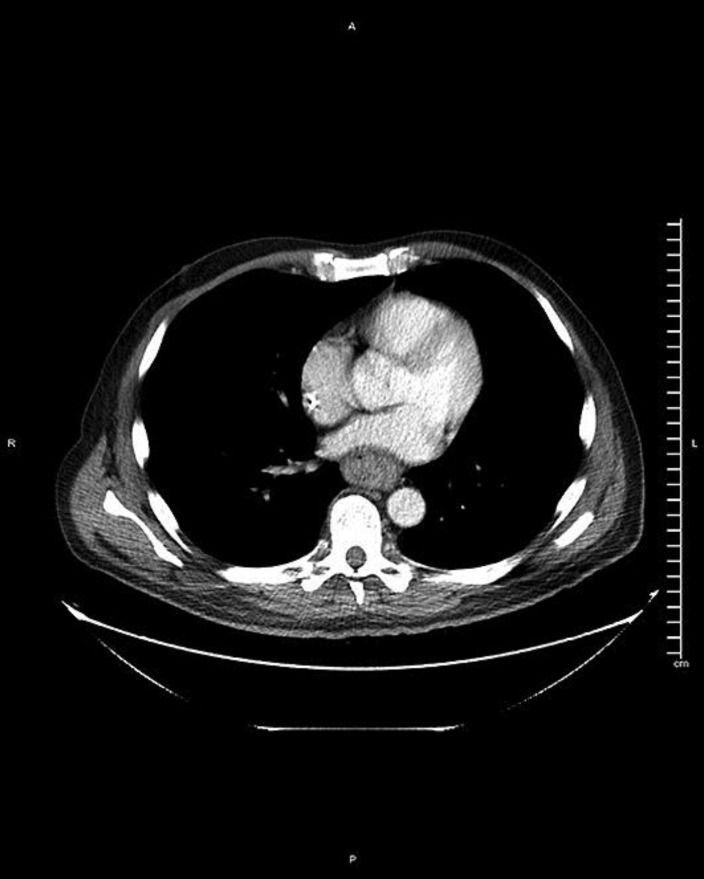
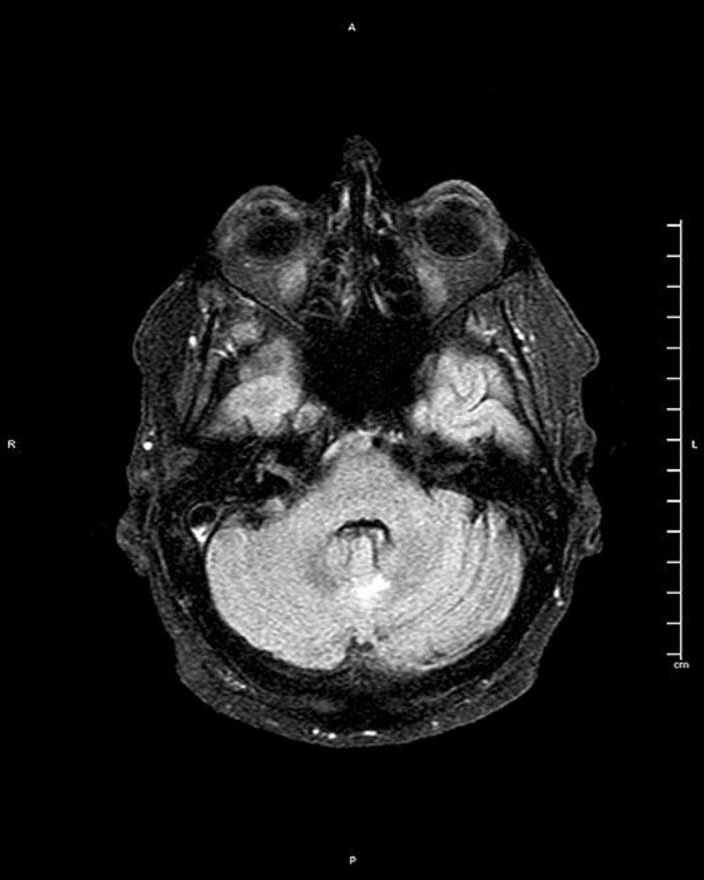
Postoperative whole brain radiation therapy and stereotactic radiosurgery (SRS) treatment of the three remaining brain masses was performed in conjunction with six cycles of capecitabine-oxaliplatin plus trastuzumab chemotherapy. Additional PET scanning to assess for response to therapy showed the mass in the lower esophagus had increased in intensity to 22.3 SUV, but had decreased in craniocaudal length from 7.5 to 5.9 cm. Post-chemoradiation CT imaging showed a partial resolution of the remaining brain lesions. Imaging was followed by endoscopy and biopsy in order to confirm the presence of an esophageal or gastric malignancy (Fig. 2). Pathologic analysis of the endoscopic biopsy sample was assessed to be a moderately differentiated adenocarcinoma. It was then decided that the patient should undergo salvage concurrent chemoradiotherapy (CRT) with a weekly paclitaxel-carboplatin regimen followed by 12 months of trastuzumab maintenance. Prior to commencing CRT, an observational MRI showed a new metastatic lesion in the cerebellar vermis (Fig. 3) which was treated via SRS therapy to a cumulative dose of 20 Gy given in two fractions of 10 Gy.
Fig. 2.
CT-abdomen showing mass-like thickening of the distal esophagus.
Fig. 3.
CT-head showing a new metastatic lesion in the cerebellar vermis.
Salvage CRT began with the administration of paclitaxel-carboplatin given in five cycles concurrently with intensity-modulated radiation therapy of the esophagus and upper abdomen with esophageal boost. MRI after salvage therapy showed a resolution of the cerebellar vermis lesion, but the enlargement of a lesion in the left frontal lobe as well as prominent white matter changes secondary to chemotherapy. Follow-up distal esophageal biopsy of the primary site showed no evidence of metaplasia or dysplasia, indicative of a complete response to CRT. This was followed by the initiation of trastuzumab therapy on a monthly basis and additional SRS to the enlarging lesion in the left frontal lobe, both of which the patient is currently undergoing at the time of writing this manuscript.
Discussion
The most common sources of malignant brain metastases are the lungs 48%, breast 15%, melanoma 9%, lymphoma 1% (mainly non-Hodgkin), gastrointestinal 3% (colon 3% and pancreatic 2%), genitourinary 11% (kidney 21%, testes 46%, cervix 5%, ovary 5%), osteosarcoma 10%, neuroblastoma 5%, and head and neck tumor 6% [4]. Of the 3% of malignant brain metastases that arise from a gastrointestinal primary malignancy, the majority are comprised of colon and pancreas primary tumors. BMET are exceedingly rare and carry a poor prognosis. Indeed, the 1-year survival rate of patients with BMET has been reportedly as low as 14%. However, our patient has sustained survival for 17 months after diagnosis with a Karnofsky Performance Score of 90%, which has been validated as a good prognostic indicator in patients with advanced malignant disease [5].
In accordance with National Comprehensive Cancer Network (NCCN) guidelines, once an MRI indicates the presence of multiple cranial metastatic lesions, the next best step in management is to proceed with biopsy or surgical resection, as was done in this patient's case, followed by whole brain radiation therapy or SRS as appropriate [6]. Pathologic analysis of the resected specimen can be used to tailor further surgery of any remaining brain lesions. An extensive workup is then required to attempt to identify the tumor's primary site. Our patient, who presented initially with metastatic brain metastases, was treated following the NCCN guidelines for central nervous system cancers for both his initial presenting metastases and the cerebellar recurrence discovered following his initial course of treatment. After discovery of the primary site at the GEJ, he was treated at that site following the NCCN guidelines for esophageal and GEJ cancers based on his stage IV (T3, N2, M1) esophageal malignancy [7].
This case is particularly impressive due to the lack of any focal neurological deficits on presentation with multiple brain metastases, the rarity of brain metastases from the gastrointestinal tract in general and as an initial finding of occult malignancy, and the primary site being a distal esophageal adenocarcinoma. Equally remarkable is the sustained survival with a high Karnofsky Performance Score despite cerebellar disease recurrence since his initial diagnosis. This patient's continued survival in the face of such a bleak prognosis supports pursuing aggressive treatment in accordance with current NCCN guidelines for treating central nervous system and esophageal malignancies.
References
- 1.Bartelt S, Momm F, Weissenberger C, Lutterbach J. Patients with brain metastases from gastrointestinal tract cancer treated with whole brain radiation therapy: prognostic factors and survival. World J Gastroenterol. 2004;10:3345–3348. doi: 10.3748/wjg.v10.i22.3345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Go PH, Klaassen A, Meadows MC, Chamberlain RS. Gastrointestinal cancer and brain metastasis – a rare and ominous sign. Cancer. 2011;117:3630–3640. doi: 10.1002/cncr.25940. [DOI] [PubMed] [Google Scholar]
- 3.Ogawa K, Takafumi T, Sueyama H, et al. Brain metastases from esophageal carcinoma. Cancer. 2002;94:759–764. doi: 10.1002/cncr.10271. [DOI] [PubMed] [Google Scholar]
- 4.Tse V.Brain metastasis. Medscape. http://emedicine.medscape.com/article/1157902-overview. Updated: Nov 14, 2016. (Accessed: May 14, 2017).
- 5.Jang RW, Caraiscos VB, Swami N, Banerjee S, Mak E, Kaya E, Rodin G, Bryson J, Ridley JZ, Le LW, Zimmermann C. Simple prognostic model for patients with advanced cancer based on performance status. J Oncol Pract. 2014;10(5):335–341. doi: 10.1200/JOP.2014.001457. [DOI] [PubMed] [Google Scholar]
- 6.National Comprehensive Cancer Network Central Nervous System Cancers. National Comprehensive Cancer Network (version 1.2016). https://www.nccn.org/professionals/physician_gls/pdf/cns.pdf (accessed: May 14, 2017).
- 7.National Comprehensive Cancer Network Esophgaeal and Esophagogastric Junction Cancers. National Comprehensive Cancer Network (version 1.2017). https://www.nccn.org/professionals/physician_gls/pdf/esophageal.pdf (accessed: May 14, 2017). [DOI] [PubMed]