Abstract
Background
Although community-dwelling persons with dementia have an increased risk of hospital readmission, no systematic review has examined the contribution of dementia to readmissions.
Summary
We examined articles in English, with no restrictions on publication dates, from Medline, PubMed, PsycINFO, CINAHL, and EMBASE. Keywords used were dementia, Alzheimer disease, frontotemporal lobar degeneration, elderly, frontotemporal dementia, executive function, brain atrophy, frontal lobe atrophy, cognitive impairment, readmission, readmit, rehospitalization, patient discharge, and return visit. Of 404 abstracts identified, 77 articles were retrieved; 12 were included. Four of 5 cohort studies showed significantly increased readmission rates in patients with dementia. On average the absolute increase above the comparison groups was from 3 to 13%. Dementia was not associated with readmission in 7 included case-control studies.
Key Message
Findings suggest a small increased risk of hospital readmission in individuals with dementia. More study is needed.
Keywords: Hospital readmissions; Dementia; Review, systematic; Older adults; Discharge
Background
In 2009, the Centers for Medicare and Medicaid Services began reporting hospital readmission rates to the public and penalizing hospitals by reducing payments for readmissions within 30 days. It is estimated that nearly 20% of all Medicare beneficiaries are readmitted within 30 days, costing the Centers for Medicare and Medicaid Services approximately USD 17.4 billion annually [1] and leading to increased mortality [2]. Risk factors for readmission include a diagnosis of congestive heart failure (CHF), pneumonia, chronic obstructive pulmonary disease, chronic kidney disease, myocardial infarction [3, 4], multiple comorbidities, functional disability, and poor social support [5].
Persons with dementia experience a 3-fold increase of preventable hospitalizations and require more healthcare services than individuals without dementia [6, 7, 8, 9, 10, 11]. Although community-dwelling persons with dementia are prone to an increased risk of readmission due to disjointed care, increased dependency, and inadequate social support and/or caregiving [12, 13], to our knowledge a systematic review has not examined the contribution of dementia to readmissions. This review addresses this gap by attempting to determine whether a diagnosis of dementia contributes to increased hospital readmission rates and discusses potential intervention strategies.
Methods
A comprehensive review of the literature was undertaken, using the following databases: Ovid Medline, PubMed, PsychINFO, CINAHL, and EMBASE. Inclusion criteria included that articles (1) be in English and define cognitive impairment by a dementia diagnosis or use of a cognitive assessment instrument such as the Mini-Mental State Examination (MMSE) and (2) include readmission rates as an outcome in those with and without cognitive impairment. Articles were excluded if they were not in English or were editorials, letters to the editor, case reports, or studies of interventions. Articles that primarily examined patients with delirium and those that included patients from long-term care facilities or geropsychiatry inpatient programs were also excluded. The initial keywords used were dementia, Alzheimer disease, frontotemporal lobar degeneration, frontotemporal dementia, executive function, brain atrophy, frontal lobe atrophy, cognitive impairment, elderly readmission, readmit, rehospital, patient discharge, and return visit.
The initial search of the included electronic databases identified abstracts of potential interest. These were assessed by one reviewer (S.P.), based on the information contained in the abstract and using the predefined inclusion and exclusion criteria. The first author (S.P.) read the title, methods, results, and conclusion sections of the abstracts. Following this review, articles were retrieved for potential inclusion and underwent a full review by two authors (S.P. and M.K.), based on the same inclusion and exclusion criteria. Studies that did not meet the inclusion criteria were further excluded from the review.
Results
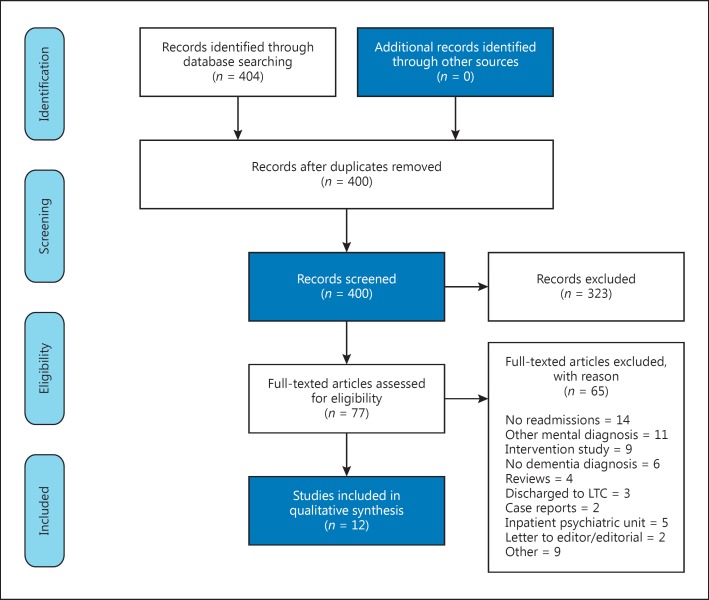
The initial search of the included electronic databases elicited 404 abstracts. After the first author's initial review, 77 articles were retrieved and underwent a full review by two authors, resulting in 12 articles for inclusion. Of these, 5 were retrospective cohort studies, comparing readmission rates in patients with and without dementia over specified periods of time (Table 1). The types of included articles and the reasons for exclusion are outlined in Figure 1. Seven of the included articles were case-control studies examining dementia or cognitive impairment as a predictor of readmission (Table 2). Dementia was defined by use of the International Classification of Diseases (ICD), 9th or 10th edition code in the electronic medical record for all cohort studies and 2 of the case-control studies. Of the remaining 5 case-control studies, 3 used brief cognitive assessments, and 2 did not specify how dementia was defined.
Table 1.
Cohort studies: are persons with dementia compared to persons without dementia at increased risk for rehospitalization?
| Authors | N | Sample characteristics | Readmission rates |
|---|---|---|---|
| Kales et al. [14] | 7,115 | Veterans ≥60 years discharged from VHA inpatient units divided into 3 groups with dementia, dementia and depression, or depression | 24-month readmission rate: Dementia 53.8% Dementia and depression 51.7% Depression 49.6% (χ2 = 9.46, df = 2, p < 0.01) |
| Draper et al. [15] | 253,000 | Patients at least ≥50 years discharged from a public hospital | 3-month readmission rate: Dementia 40% No dementia 32% (p < 0.001) |
| Daiello et al. [16] | 25,839 | Patients enrolled in Rhode Island's fee-for-service Medicare and discharged | 1-month readmission rate: Dementia 17.8% No dementia 14.5% (p < 0.001) Adjusted OR for readmission in those with dementia after controlling for confounders (1.18; 95% CI: 1.08–1.29) |
| Davydow et al. [10] | 7,031 | Patients ≥50 years participating in US Health and Retirement Study discharged from hospital with primary diagnosis of CHF, pneumonia, or MI | OR for 1-month readmission (rehospitalization rates not provided): Comorbid dementia and depression (OR: 1.58; 95% CI: 1.06–2.35) Comorbid CIND and depression (OR: 1.98; 95% CI: 1.40–2.81) Depression alone (OR: 1.37; 95% CI: 1.01–1.84) Dementia alone NS CIND alone NS Reference group: no dementia, CIND, or depression |
| Ahmedani et al. [17] | 160,169 | Persons ≥18 years in HMO health plans discharged from hospital with primary diagnosis of CHF, AMI, or pneumonia | 1-month readmission rate: Dementia: 29.6% No dementia or psychiatric diagnosis: 16.5% (p < 0.001) |
VHA, Veteran's Health Administration; OR, odds ratio; CIND, cognitive impairment, no dementia; HMO, Health Maintenance Organization; CHF, congestive heart failure; MI, myocardial infarction; AMI, acute myocardial infarction; NS, nonsignificant.
Fig. 1.
Flow chart for identification of relevant studies for inclusion in the systematic review of dementia diagnoses on hospital readmission rates and hospital underuse. LTC, long-term care.
Table 2.
Case-control studies: are patients who are rehospitalized compared to those who are not rehospitalized more likely to have dementia/cognitive impairment?
| Authors | N | Sample characteristics | Likelihood of cognitive impairment or dementia diagnosis related to readmission |
|---|---|---|---|
| Zanocchi et al. [18] | 839 | Patients ≥75 years of age discharged from a geriatric unit | Readmission within 3 months not related to dementia diagnosis |
| Bellelli et al. [19] | 1,072 | Patients ≥65 years of age discharged from rehabilitation unit | Readmission within 12 months not related to MMSE score |
| Ono et al. [20] | 326 | Patients discharged from dementia unit | Readmission within 24 months not related to cognitive status, as measured by Hasegawa's Dementia Scale |
| Watson et al. [21] | 729 | Patients discharged with primary dx of heart failure | Readmission within 3 months not related to dementia diagnosis |
| Dagani et al. [22] | 329 | Patients ≥64 years of age discharged from a geriatric unit | Readmission within 6 months not related to cognitive status, as measured by MMSE |
| Bottle et al. [23] | 70,108 | Patients discharged with primary diagnosis of heart failure extracted from the National Hospital Administrative Data for England | Readmission within 1 month not related to dementia diagnosis |
| Aljishi et al. [24] | 197 | Patients discharged from a general medicine unit | Readmission within 1 month not related to dementia diagnosis |
MMSE, Mini-Mental State Examination; dx, diagnosis.
Cohort Studies
The 5 cohort studies included 293,824 patients, 292,985 of whom were 50 years of age and older [10, 14, 15, 16]. Four studies conducted healthcare-based sampling, using large administrative databases [14, 15, 16, 17]. The remaining study used population-based sampling of persons 50 years of age and older participating in the Health and Retirement Study between 1998 and 2008 [10].
The windows for examining readmission varied across studies from 1 to 24 months. One-month readmission rates of individuals with and without dementia were compared in 3 cohort studies. One-month readmission rates were 17.8% in individuals with dementia versus 14.5% in those without (p < 0.001) in a large study of more than 25,000 patients enrolled in Rhode Island's fee-for-service Medicare program. In a study using an HMO database of more than 160,000 patients who had a primary diagnosis of CHF, myocardial infarction, or pneumonia, 1-month readmission rates for those with concurrent dementia versus without dementia were 29.6 versus 16.5%, respectively (p < 0.001) [16, 17]. The third study of 1-month readmission rates which examined patients 50 years and older participating in the US Health and Retirement Study and discharged with a primary diagnosis of CHF, myocardial infarction, or pneumonia determined that a dementia diagnosis was not significantly related to readmissions. In this study, dementia became a significant risk factor for readmission only when it was comorbid with depression (OR: 1.58; 95% CI: 1.06–2.35) [10]. Three-month readmission rates in patients 50 years of age and older discharged from a public hospital with dementia were 40%, compared with 32% (p < 0.001) in patients without dementia [15]. In a study of veterans 60 years and older discharged from Veterans Health Administration Medical Center inpatient units, the 24-month readmission rates were 53.8% in patients with dementia; 51.7% in patients with dementia and depression; and 49.6% in patients with depression (χ2 = 9.46, df = 2, p < 0.01) [14]. In summary, the absolute percent increase in readmission among individuals with dementia ranged from 3 to 13% in the 4 cohort studies that found a significant difference compared with subjects without dementia.
Case-Control Studies
The 7 case-controlled studies included 73,600 patients. Two studies were in community dwellers [19, 20], 1 study was in older adults discharged from a general medicine unit [24], 2 studies included older adults discharged from a geriatric unit [18, 22], and 2 studies focused on individuals admitted for CHF [21, 23].
None of the 7 case-control studies, which examined readmissions across variable time frames ranging from 1 to 24 months, determined that cognitive impairment was related to readmission. Two examined 1-month readmissions. The first study compared 197 patients readmitted to a matched random sample of 197 patients who were not readmitted to a general medicine ward in New Zealand. Dementia was defined as any long-term cognitive impairment documented in the medical record. Results indicate that dementia did not significantly affect the likelihood of readmission (p = 1.0) [24]. The second study evaluated data extracted from the National Hospital Administrative Data for England on 70,108 patients discharged with a primary diagnosis of CHF. A concurrent dementia diagnosis was obtained from ICD-9 and ICD-10 codes in administrative databases. This study found that readmission was not related to a diagnosis of dementia (p = 0.717) [23].
Another 2 studies examined 3-month readmissions. Zanocchi et al. [18] followed a group of adults 75 years and older discharged from a geriatric unit. This study used ICD-9 codes to identify a dementia diagnosis and found that dementia was not associated with readmission. The second study analyzed 729 patients discharged from the Massachusetts General Hospital with a primary diagnosis of CHF. Potential predictors for readmission were extracted from the electronic medical record and included mild undiagnosed dementia. Results indicate that readmission was not related to a dementia diagnosis (p = 0.19) [21].
Dagani et al. [22] studied 329 patients 64 years and older who were discharged from a geriatric unit. A standard telephone interview was used for the 6-month follow-up assessment. Cognition was assessed using the MMSE [25]. Results indicate that 6-month readmission was not related to cognitive impairment (p = 0.89).
Bellelli et al. [19] studied 1,072 patients 65 years and older who were discharged from a rehabilitation unit. They were contacted by telephone at 12 months after discharge. Cognition was assessed by MMSE scores. Absent or mild cognitive decline was defined by MMSE scores of 25–30 (50.1%); mild-to-moderate cognitive decline was defined by MMSE scores of 19–24 (27.4%); moderate-to severe cognitive decline was defined by MMSE scores of 11–18 (18.1%); and severe cognitive decline was defined by MMSE scores of 0–10 (4.4%). Results indicate that readmission within 12 months was not related to MMSE scores (23.3 ± 5.3 for 1 rehospitalization and 24.0 ± 4.6 for >2 rehospitalizations; p = 0.63).
Lastly, Ono et al. [20] studied 326 patients discharged from a dementia unit. They examined the number of times patients were readmitted once discharged from the unit. Cognition was measured by the Hasegawa's Dementia Scale [26]. Women with late readmissions had high cognition (n = 15) compared with men with late readmissions, who had low cognition (n = 5). Results indicate that 24-month readmission was not related to cognitive status (p = 0.469).
Discussion
Four of the 5 cohort studies showed statistically significant increased readmission rates in patients with dementia; however, on average, the absolute increase above comparison groups was modest, ranging from 3 to 13%. The modestly positive findings of the cohort studies are countered by negative findings regarding increased readmission rates among individuals with dementia in the case-control studies. These negative findings may be due to sampling bias, as the definitions and diagnosis of cognitive impairment varied more widely in these studies. This may have resulted in populations that did not meet the intended criteria of having significant cognitive impairment [27].
Two of the 5 cohort studies reported increased readmission rates among persons with dementia and comorbid depression. This finding suggests the need for further studies to determine whether behavioral and psychiatric problems, including substance use disorders and anxiety disorders, increase readmissions in persons with dementia.
Several studies have evaluated the impact of protocols designed to prevent or reduce 30-day readmission rates, with promising but mixed results. To date, no single intervention has been consistently associated with a reduced risk for 30-day readmission [28, 29]. In addition, many studies have excluded individuals with dementia or cognitive impairment [30, 31, 32]. In one promising social-worker-led, care transition intervention, which included 292 adults 65 years of age and older, of whom 16% had a diagnosis of Alzheimer dementia and 43% had symptoms of cognitive decline or depression, readmission rates decreased by 61%, with annual cost savings of approximately USD 628,202 [33]. In a quasi-experimental study of adults 65 years and older discharged home from an acute hospital in Connecticut, of whom 15% (n = 219) in each group had impaired cognition, participants in the restorative care model were 32% less likely to be readmitted than participants receiving usual care (conditional OR: 0.68, 95% CI: 0.43–1.08) [34].
The previously cited studies, which focused on care models in the home following discharge, typically did not specifically address the needs of those with dementia. Some recommendations to improve transitions for persons with dementia, based on the 2007 Transitions of Care Consensus Conference, include the following: (1) identify the primary caregiver, (2) determine whether the caregiver understands the discharge instructions, (3) determine whether the caregiver and patient have the resources and ability to comply with the discharge instructions, (4) arrange mental and/or medical follow-up by a visiting nurse, (5) confirm scheduling of psychiatric and/or medical follow-up appointments, (6) develop a management plan for possible behavioral problems, and (7) identify safety concerns [35].
Limitations
This review has some limitations. Most studies were based on ICD codes, chart diagnosis, or brief cognitive screening instruments, not necessarily a systematic and guideline-based diagnosis of dementia. Findings were also based on relatively few studies that occurred in a variety of settings and used different time windows for evaluating readmission rates.
Conclusions
This systematic review was undertaken to determine the association of a diagnosis of dementia with hospital readmission rates. The findings indicate that a dementia diagnosis may have a modest impact on readmission rates. This review also suggests a need for studies to determine whether behavioral and psychiatric problems, including substance use disorders, depression, and anxiety disorders, are associated with readmission rates. Future research should develop and test transitional care models specifically for persons with dementia.
Disclosure Statement
The authors report no conflicts of interest.
Acknowledgment
This material is the result of work produced with the use of facilities and resources at the Houston VA HSR&D Center for Innovations in Quality, Effectiveness and Safety (CIN13–413). The opinions expressed reflect those of the authors and not necessarily those of the Department of Veterans Affairs, the US government, or the Baylor College of Medicine.
References
- 1.Bhalla R, Kalkut G. Could Medicare readmission policy exacerbate health care system inequity? Ann Intern Med. 2010;152:114–118. doi: 10.7326/0003-4819-152-2-201001190-00185. [DOI] [PubMed] [Google Scholar]
- 2.Lum HD, Studenski SA, Degenholtz HB, Hardy SE. Early hospital readmission is a predictor of one-year mortality in community-dwelling older Medicare beneficiaries. J Gen Intern Med. 2012;27:1467–1474. doi: 10.1007/s11606-012-2116-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jenks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;350:1418–1428. doi: 10.1056/NEJMsa0803563. erratum in N Engl J Med 2011; 364: 1582. [DOI] [PubMed] [Google Scholar]
- 4.Bogaisky M, Dezieck L. Early hospital readmission of nursing home residents and community-dwelling elderly adults discharged from the geriatrics service of an urban teaching hospital: patterns and risk factors. J Am Geriatr Soc. 2015;63:548–552. doi: 10.1111/jgs.13317. [DOI] [PubMed] [Google Scholar]
- 5.Garcia-Perez L, Linertova R, Lorenzo-Riera A, Vazquez-Diaz JR, Duque-Gonzalez B, Sarria-Santamera A. Risk factors for hospital readmissions in elderly patients: a systematic review. QJM. 2011;104:639–651. doi: 10.1093/qjmed/hcr070. [DOI] [PubMed] [Google Scholar]
- 6.Bynum JP, Rabins PV, Weller W, Niefeld M, Anderson GF, Wu AW. The relationship between a dementia diagnosis, chronic illness, Medicare expenditures, and hospital use. J Am Geriatr Soc. 2004;52:187–194. doi: 10.1111/j.1532-5415.2004.52054.x. [DOI] [PubMed] [Google Scholar]
- 7.Taylor DH, Ǿstbye T, Langa KM, Weir D, Plassman BL. The accuracy of Medicare claims as an epidemiological tool: the case of dementia revisited. J Alzheimers Dis. 2009;17:807–815. doi: 10.3233/JAD-2009-1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mitchell SL, Teno JM, Kiely DK, Shaffer ML, Jones RN, Prigerson HG, Volicer L, Givens JL, Hamel MB. The clinical course of advanced dementia. N Engl J Med. 2009;361:1529–1538. doi: 10.1056/NEJMoa0902234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hurd MD, Martorell P, Langa KM. Monetary costs of dementia in the United States. N Engl J Med. 2013;369:489–490. doi: 10.1056/NEJMc1305541. [DOI] [PubMed] [Google Scholar]
- 10.Davydow DS, Zivin K, Langa KM. Hospitalization, depression and dementia in community-dwelling older Americans: findings from the National Health and Aging Trends Study. Gen Hosp Psychiatry. 2014;36:135–141. doi: 10.1016/j.genhosppsych.2013.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Medicare & Medicaid Services Medicare Current Beneficiary Survey, 2008. 2008 Health and Health Care of the Medicare Population. https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/MCBS/Data-Tables.html (accessed July 29, 2016).
- 12.Cumbler E, Carter J, Kutner J. Failure at the transition of care: challenges in the discharge of the vulnerable elderly patient. J Hosp Med. 2008;3:349–352. doi: 10.1002/jhm.304. [DOI] [PubMed] [Google Scholar]
- 13.Cummings SM. Adequacy of discharge plans and rehospitalization among hospitalized dementia patients. Health Soc Work. 1999;24:249–259. doi: 10.1093/hsw/24.4.249. [DOI] [PubMed] [Google Scholar]
- 14.Kales HC, Blow FC, Copeland LA, Bingham RC, Kammerer EE, Mellow AM. Health care utilization by older patients with coexisting dementia and depression. Am J Psychiatry. 1999;156:550–556. doi: 10.1176/ajp.156.4.550. [DOI] [PubMed] [Google Scholar]
- 15.Draper B, Karmel R, Gibson D, Peut A, Anderson P. The Hospital Dementia Services Project: age differences in hospital stays for older people with and without dementia. Int Psychogeriatr. 2011;23:1649–1658. doi: 10.1017/S1041610211001694. [DOI] [PubMed] [Google Scholar]
- 16.Daiello LA, Gardner R, Epstein-Lubow G, Butterfield K, Gravenstein S. Association of dementia with early rehospitalization among Medicare beneficiaries. Arch Gerontol Geriatr. 2014;59:162–168. doi: 10.1016/j.archger.2014.02.010. [DOI] [PubMed] [Google Scholar]
- 17.Ahmedani BK, Solberg LI, Copeland LA, Fang-Hollingsworth Y, Stewart C, Hu J, Nerenz DR, Williams K, Cassidy-Bushrow AE, Waxmonsky J, Lu CY, Waitzfelder BE, Owen-Smith AA, Coleman KJ, Lynch FL, Ahmed AT, Beck A, Rossom RC, Simon GE. Psychiatric comorbidity and 30-day readmissions after hospitalization for heart failure, AMI, and pneumonia. Psychiatr Serv. 2015;66:134–140. doi: 10.1176/appi.ps.201300518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zanocchi M, Maero B, Martinelli E, Cerrato F, Corsinovi L, Gonella M, Ponte E, Luppino A, Margolicci A, Molaschi M. Early re-hospitalization of elderly people discharged from a geriatric ward. Aging Clin Exp Res. 2005;81:63–69. doi: 10.1007/BF03324642. [DOI] [PubMed] [Google Scholar]
- 19.Bellelli G, Magnifico F, Trabucchi M. Outcomes at 12 months in a population of elderly patients discharged from a rehabilitation unit. J Am Med Dir Assoc. 2008;9:55–64. doi: 10.1016/j.jamda.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 20.Ono T, Tamai A, Takeuchi D, Tamia Y. Factors related to readmission to a ward for dementia patients: sex differences. Psychiatry Clin Neurosci. 2011;65:490–498. doi: 10.1111/j.1440-1819.2011.02251.x. [DOI] [PubMed] [Google Scholar]
- 21.Watson AJ, O'Rourke J, Jethwani K, Cami A, Stern TA, Kvedar JC, Chueh HC, Zai AH. Linking electronic health record-extracted psychosocial data in real-time to risk of readmission for heart failure. Psychosomatics. 2011;52:319–327. doi: 10.1016/j.psym.2011.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dagani J, Ferrari C, Boero ME, Geroldi C, Marco Giobbio GM, Maggi P, Melegari AL, Sattin G, Signorini M, Volpe D, Zanetti O, de Girolamo G. A prospective, multidimensional follow-up study of a geriatric hospitalized population: predictors of discharge and well-being. Aging Clin Exp Res. 2013;25:691–701. doi: 10.1007/s40520-013-0153-3. [DOI] [PubMed] [Google Scholar]
- 23.Bottle A, Aylin P, Bell D. Effect of the readmission primary diagnosis and time interval in heart failure patients: analysis of English administrative data. Eur J Heart Fail. 2014;16:846–853. doi: 10.1002/ejhf.129. [DOI] [PubMed] [Google Scholar]
- 24.Alijishi M, Parekh K. Risk factors for general medicine readmissions and association with mortality. NZ Med J. 2014;127:42–50. [PubMed] [Google Scholar]
- 25.Folstein MF, Folstein SE, McHugh PR. Mini-Mental State: a practical method for grading cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 26.Katoh S, Shimogaki M, Onodera A, Ueda H, Oikawa K, Ikeda K, Kosaka A, Imai Y. Development of the revised version of Hasegawa's dementia scale (HDS-R) (in Japanese)1. Jpn J Geriatr Psychiatry. 1991;2:1339–1347. [Google Scholar]
- 27.Hulley SB, Cummings SR, Browner WS, Grady DG, Newman TB. ed 3. Philadelphia: Lippincott Williams & Wilkins; 2007. Designing Clinical Research. [Google Scholar]
- 28.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155:520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 29.Linertová R, Garcia-Pérez L, Vézquez-Diaz JR, Lorenzo-Riers A, Sarria-Santamera A. Interventions to reduce hospital readmissions in the elderly: in-hospital or home care. A systematic review. J Eval Clin Pract. 2011;17:1167–1175. doi: 10.1111/j.1365-2753.2010.01493.x. [DOI] [PubMed] [Google Scholar]
- 30.Courtney M, Edwards H, Chang A, Parker A, Finlayson K, Hamilton K. Fewer emergency readmissions and better quality of life for older adults at risk of hospital readmission: a randomized controlled trial to determine effectiveness of a 24-week exercise and telephone follow-up program. J Am Geriatr Soc. 2009;57:395–402. doi: 10.1111/j.1532-5415.2009.02138.x. [DOI] [PubMed] [Google Scholar]
- 31.Graves N, Courtney M, Edwards H, Chang A, Parker A, Finlayson K. Cost-effectiveness of an intervention to reduce emergency re-admissions to hospital among older patients. PLoS One. 2009;4:1–9. doi: 10.1371/journal.pone.0007455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, Pauly MV, Schwartz JS. Comprehensive discharge planning and home follow-up of hospitalized elders. A randomized controlled trial. JAMA. 1999;281:613–620. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- 33.Watkins L, Hall C, Kring D. Hospital to home. A transition program for frail older adults. Prof Case Manag. 2012;17:117–123. doi: 10.1097/NCM.0b013e318243d6a7. [DOI] [PubMed] [Google Scholar]
- 34.Tinetti M, Charpentier P, Gottschalk M, Baker DI. Effect of a restorative model of posthospital home care on hospital readmissions. J Am Geriatr Soc. 2012;60:1521–1526. doi: 10.1111/j.1532-5415.2012.04060.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Epstein-Lubow G, Fulton T, Gardner R, Gravenstein S, Miller IW. Post-hospital transitions: special considerations for individuals with dementia. Geriatr Pract Phys. 2010;93:125–127. [PubMed] [Google Scholar]