Abstract
Purpose
Breast cancer subtypes (BCS) determined from IHC staining have been correlated with molecular subtypes and associated with prognosis/outcomes, but there are limited data correlating these BCS and axillary node involvement. This study was conducted to assess whether BCS predicted for nodal metastasis or was associated with other clinical-pathologic features at presentation.
Methods
Stage I/II patients who underwent breast-conserving surgery and axillary surgical assessment with available tissue blocks underwent a institutional pathological review and construction of a tissue microarray(TMA). The slides were stained for ER/PR/HER2-neu for classification into BCS. Nodal involvement and other clinical-pathologic features were analyzed to assess associations between BCS and patient/tumor characteristics. Outcomes were calculated a function of BCS.
Results
The study cohort consisted of 453 patients(LA 48.6%, LB 16.1%, HER2 11.0%, TN 24.2%), of which 22%(n=113) were node+. There were no significant associations with BCS and pN stage, node positivity, or absolute number of nodes involved (all p>0.05). However, there were significant associations with subtype and age at presentation (< 0.001), method of detection (p=0.049), tumor histology (p<0.001), race (p=0.041), and tumor size (pT stage, p<0.001) by univariate and multivariate analysis. As expected, 10-year outcomes differed by BCS, with TN & HER2/neu subtypes having the worse overall(p=0.03), disease-free(p=0.03) and distant metastasis-free survival(p< 0.01).
Conclusions
Our findings suggest that there is a significant association between BCS and age, T stage, histology, method of detection and race, but no associations to predict nodal involvement. If additionally validated, these findings suggest that BCS should not strongly influence regional management considerations.
Introduction
Prognostic variables for early-stage breast cancer have traditionally included number of lymph nodes involved, tumor size and extent of disease (e.g. metastasis), which subsequently has been incorporated into TNM staging (1). More recently, both morphological and immunohistochemical analyses analysis have been incorporated to determine prognosis (2,3). Molecular subtypes are predictive of responses to specific therapies and are prognostic for clinical outcomes (2,7–8). Specifically, molecular gene expression for estrogen receptor (ER), progesterone receptor (PR), and HER-2/neu (HER-2) allows a higher order of classification that has been correlated to outcomes (4,5). Subsequently, the use of immunohistochemical analysis as a surrogate for molecular profiling has been verified to estimate the prevalence of these molecular subtypes (18,36), allowing for more widespread utilization of this higher order of tumor distinction in the clinical setting to provide important insight into management strategies and risk of distant metastasis (13,32).
An additional advancement in breast cancer management has been identification of patients who are candidates for a more minimalistic approach to the axilla. In essence, sentinel lymph node biopsy (SLNB) has become the standard of care for the management of breast cancer primarily because of its accuracy in identifying the sentinel node and node negative patients, thus allowing for omission of a full axillary dissection in selected patients (6–8).
Although both tumor BCS and pN stage are both independently demonstrated as prognostic (9), there is a paucity of data describing the relationship between these two factors (10,11,12). Consequently, the primary objective of this investigation was to determine if BCS correlates to axillary node involvement in early-stage breast cancer. The secondary objectives were to investigate whether there is an association between BCS and other clinical-pathologic parameters at presentation, and finally, to conduct a confirmatory analysis of the relationship between BCS and outcomes.
Materials and Methods
Patient Population
The inclusion criteria for this study included: (1) Stage I/II breast conservation therapy patients (2) availability of paraffin-embedded tissue blocks of the primary tumor and (3) complete clinical records. All patients underwent breast conserving surgery and surgical assessment of the axilla at our institution. Systemic therapy was delivered at the discretion of the treating medical oncologist. Neoadjuvant chemotherapy patients were excluded. The radiation therapy consisted of conventionally-fractionated, whole-breast radiation delivered using 2D/3D standard tangential techniques with regional nodal radiation, if indicated, with a boost delivered to the lumpectomy cavity in the vast majority of patients as previously described (13–16). The median tumor dose for the cohort was 64 Gy.
Prior to the pathologic/molecular analysis, departmental chart reviews were conducted on the study cohort to obtain updated follow-up parameters (changes in patient demographics and outcomes such as local, regional, distant relapse and survival events). These were cross-referenced with our institutional Tumor Registry for accuracy. Institutional Review Board (IRB) approval was obtained through our institution’s Human Investigations Committee (HIC).
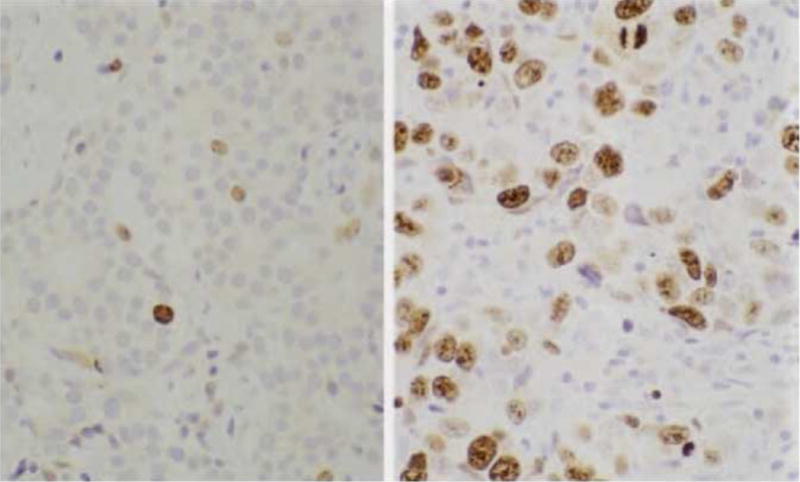
Immunohistochemical Analysis
A tissue microarray (TMA) of eligible patients was constructed by our institution’s Department of Pathology to determine BCS. The hematoxylin and eosin-stained slides of archived paraffin blocks of the primary tumor were used to develop representative tumor sections and assembled into a TMA with 2-fold redundancy for immunohistochemical analysis, as previously described(36). Antibodies included: mouse monoclonal antihuman ER antibody (DAKO) for ER, mouse monoclonal antihuman PR (DAKO) for PR, and rabbit monoclonal anti-cytokeratin 19 (Ventana) for HER-2/neu and qualitative and semi-quantitative measures were recorded (13–16). The slides were prepared at our institution and read by one pathologist (H.W.). For the purposes of this study, immunohistochemical analysis of the number of positively stained nuclei (≥10%+) determined ER/PR, and membrane staining of HER-2/neu was conducted using scores of 2 and 3 designated as positive (16).
Statistical Analysis
The categorization of BCS was as follows: luminal A (LA:ER+/PR+/HER−2−), luminal B (LB: ER+/PR+/HER-2+), HER-2+(ER−/PR/HER-2+) and triple negative(TN: ER−/PR−/HER−2−). SAS®V.9.2 Software (SAS, Cary, NC) was utilized to analyze associations between clinical-pathologic characteristics and BCS using Pearson’s chi-squared or Fisher’s exact test. Analyses of continuous variables using the ANOVA test were presented as mean ± 1SD. Multiple linear regression analysis was utilized to further explore the association between the clinical-pathologic features and BCS and the Kaplan-Meier Analysis was used for outcomes analysis. For this study, a p-value of p < 0.05 was considered as statistically significant.
Results
Of the 453 patients who met the inclusion criteria, BCS were classified as followed: 48.5% (220/453) luminal A, 16.1% (73/453) luminal B, 11.0% (50/453) HER-2/neu, and 24.3% (110/453) TN. The median follow-up time for the cohort was 8 years.
Associations between BCS and Clinical Parameters
The mean age at diagnosis was found to be significantly different across BCS with TN and HER-2 presenting at younger ages: (years: TN-47.9; HER2–48.0; LA-53.5; LB-53; p < 0.001). For method of detection at presentation, patients who had TN disease were much more likely to present with palpable masses, and mammographically-detected tumors were most likely to be LA (p=0.049). The details of this analysis are shown in Table 1. For associations with race, AA patients were significantly more likely to be of TN or HER-2/neu (p=0.041).
Table 1.
Patient and Tumor Characteristics
| Ki67 expression | ||||
|---|---|---|---|---|
|
| ||||
| Feature | Negative(%) | Positive(%) | p | |
| Age (y) | <.01 | |||
| ≤ 50 | 121 (73) | 45 (27) | ||
| > 50 | 230 (85) | 42 (15) | ||
|
| ||||
| Race | <.01 | |||
| White | 305 (83) | 61 (17) | ||
| Black | 36 (63) | 21 (37) | ||
| Other | 10 (67) | 5 (33) | ||
|
| ||||
| ER | .04 | |||
| Negative | 124 (75) | 41 (25) | ||
| Positive | 211 (83) | 42 (17) | ||
|
| ||||
| PR | .50 | |||
| Negative | 244 (79) | 64 (21) | ||
| Positive | 101 (82) | 22 (18) | ||
|
| ||||
| HER-2/neu | .01 | |||
| Negative | 297 (82) | 67 (18) | ||
| Positive | 31 (65) | 17 (35) | ||
|
| ||||
| TN* | .38 | |||
| No | 90 (78) | 26 (22) | ||
| Yes | 245 (81) | 56 (19) | ||
|
| ||||
| Hormone Therapy | .02 | |||
| No | 176 (76) | 55 (24) | ||
| Yes | 172 (85) | 31 (15) | ||
|
| ||||
| Chemotherapy | .05 | |||
| No | 239 (83) | 50 (17) | ||
| Yes | 110 (75) | 37 (25) | ||
|
| ||||
| pN stage | .17 | |||
| 0 | 213 (78) | 60 (22) | ||
| 1 | 53 (87) | 8 (13) | ||
| 2 | 3 (60) | 2 (40) | ||
|
| ||||
| pT stage | .03 | |||
| T1 | 232 (84) | 43 (16) | ||
| T2 | 100 (74) | 36 (26) | ||
|
| ||||
| Nodal Status | .12 | |||
| Negative | 188 (77) | 55 (23) | ||
| Positive | 61 (86) | 10 (14) | ||
|
| ||||
| Margin status | .92 | |||
| Positive | 29 (76) | 9 (24) | ||
| Negative | 211 (81) | 50 (19) | ||
| Close† | 41 (79) | 11 (21) | ||
| Unknown | 70 (80) | 17 (20) | ||
Triple negative (TN): Yes indicates Estrogen Receptor(−), Progesterone Receptor(−), and HER-2-neu(−)disease; No indicates that one or more markers was positive.
Defined as the closest tumor margin ≤ 2mm
As expected, there were significant variations in the delivery of systemic therapy based on BCS. The percentages of patients who received adjuvant hormonal therapy was significantly higher for LA and LB patients: 7.8% triple negative, 5.8% HER-2, 64.1% LA, and 71.6% LB (p <0.001) and the patients who received systemic chemotherapy were significantly more often TN or HER2+: 70.1% TN, 74.5% HER-2, 64.1% LA, and 71.6% LB (p <0.001). The clinical and demographic features as a function of BCS are summarized in Table 1.
Associations Between BCS and Pathologic Features
There was no association between with pN stage (pN0 vs. pN1/pN2, p=0.246). Similarly, there was no association in patients who presented with node positive vs. negative disease (p=0.694) across the four subtypes. Lastly, there were no statistically significant differences in the number of positive nodes across the four BCS (p=0.659).
However, there was a statistically significant difference in the pathologic T stage (p<0.001); of TN subtype, 44.3% presented with pT2/pT3 disease compared to 36.2% of patients with HER-2, 20.2% of patients with the LA and 26.5% of patients with LB. There was also a significant association between BCS and histology, with invasive lobular (75%) and tubular carcinoma (83%) more likely to be associated with LA whereas invasive ductal carcinoma (28%) was most often associated with TN (p<0.001). These pathologic findings are shown in Table 2.
Table 2.
Multivariate analysis of prognostic factors and 15-year outcomes
| Prognostic Factor | IBRFS | OS | CSS | DMFS | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| HR | (95% CI) | p | HR | (95% CI) | p | HR | (95% CI) | p | HR | (95% CI) | p-value | |
| Ki67 | 1.007 | 0.464–2.186 | 0.9852 | 0.982 | 0.537–1.798 | 0.9537 | 1.089 | 0.543–2.186 | 0.8106 | 1.124 | 0.608–2.078 | 0.7088 |
| ≥50 yr | 0.639 | 0.363–1.127 | 0.1221 | 1.347 | 0.857–2.119 | 0.1971 | 0.811 | 0.493–1.333 | 0.4087 | 0.591 | 0.379–0.922 | 0.0205 |
| Race | 1.302 | 0.788–2.151 | 0.3037 | 0.823 | 0.496–1.365 | 0.4505 | 0.907 | 0.520–1.579 | 0.7292 | 1.034 | 0.657–1.629 | 0.8841 |
| ER status | 0.890 | 0.477–1.660 | 0.7140 | 0.832 | 0.524–1.323 | 0.4370 | 0.609 | 0.351–1.058 | 0.0784 | 0.574 | 0.352–0.937 | 0.0264 |
| PR status | 0.712 | 0.328–1.546 | 0.3905 | 0.918 | 0.540–1.562 | 0.7533 | 0.857 | 0.449–1.633 | 0.6386 | 0.706 | 0.384–1.298 | 0.2619 |
| HER2 status | 0.648 | 0.200–2.103 | 0.4703 | 0.456 | 0.166–1.248 | 0.1264 | 0.646 | 0.233–1.789 | 0.4002 | 0.956 | 0.436–2.095 | 0.9104 |
| TN | 0.871 | 0.439–1.728 | 0.6932 | 0.665 | 0.412–1.075 | 0.0958 | 0.580 | 0.332–1.014 | 0.0560 | 0.563 | 0.338–0.938 | 0.0274 |
| pN stage | 1.504 | 0.763–2.962 | 0.2382 | 2.025 | 1.264–3.244 | 0.0034 | 2.099 | 1.257–3.507 | 0.0046 | 2.368 | 1.518–3.695 | 0.0001 |
| Tumor Size | 3.122 | 1.754–5.555 | 0.0001 | 1.871 | 1.197–2.925 | 0.0060 | 2.114 | 1.266–3.531 | 0.0042 | 3.263 | 2.072–5.139 | <.0001 |
| Margin | 3.201 | 1.359–7.543 | 0.0078 | 2.266 | 1.134–4.529 | 0.0206 | 2.643 | 1.208–5.786 | 0.0150 | 1.467 | 0.619–3.474 | 0.3840 |
| Systemic Therapy* | 0.498 | 0.165–1.505 | 0.2164 | 0.613 | 0.256–1.465 | 0.2708 | 0.615 | 0.230–1.643 | 0.3323 | 0.429 | 0.177–1.041 | 0.0614 |
Abbreviations: HR=Hazard Ratio. CI=Confidence Interval. ER=estrogen receptor. PR=progesterone receptor. HER2=human epidermal growth factor receptor 2. TN=triple negative, defined as ER(−), PR(−), HER2(−). N=node. IBRFS-Ipsilateral Breast Recurrence Free Survival; OS− Overall Survival, CSS-Cause specific survival, DMFS-Distant metastasis free survival
On multiple linear regression modeling, when incorporating age at diagnosis, race, pT stage, method of detection, tumor histology and nodal involvement (pN+/pN-, and number of +nodes), the associations between BCS that remained significant included: pT stage (p=0.011), race (p<0.001), age (p<0.001) and method of detection (p<0.001), with no statistical significance between pN status or absolute number of +nodes and BCS (p=0.846).
BCS and Survival Analysis
Outcomes analyzed included overall survival(OS), distant metastasis-free survival(DMFS) and disease-free survival(DFS). For the overall survival time in this cohort, the mean survival time was 4.9 ± 0.1 years for TN, 7.0 ± 0.2 years for HER-2, 18.6 ± 0.8 years for luminal A, and 16.7 ± 0.3 years for luminal B. As expected, there were significant differences in 10-year outcomes by BCS for OS (p=0.031), DFS (p=0.027), and DMFS (p<0.001). Details of outcomes are shown in Figure 1.
Figure 1.
Discussion
While number of positive lymph nodes and BCS are both independently well-recognized prognostic indicators, it remains unclear whether there is an association between BCS and nodal involvement(10,17). Theoretically, axillary involvement, if associated with BCS, may provide another predictive criterion for therapeutic decisions regarding nodal management. To date, the limited published literature on this topic suggests the relationship between BCS and involvement/extent of lymph node metastasis warrants investigation. In this study, we were not able to demonstrate any significant associations between BCS and lymph node positivity or extent of nodal disease for patients with early-stage disease. However, consistent with the findings of other publications, BCS was found to be associated with race, age, and outcomes, with a significant distinction in time to distant metastasis, disease free survival, and overall survival observed across the four BCS (18–20). Furthermore, a statistically significant association between tumor BCS and T stage was also identified.
While there is a paucity of data on associations between presence or extent of nodal disease across all BCS, conflicting results on the relationship between the TN subtype and nodal disease has been reported(16, 21–25). Several publications suggest that basal/TN BCS may predict a lower risk of nodal involvement (21, 24), whereas others have suggested a greater extent of nodal disease (22, 25). This study adds to the existing literature not only supporting no association between TN subtype and nodal involvement, but suggests that there is no association with any of the BCS regardless of whether the extent of disease is analyzed as node+/−, absolute number of involved lymph nodes, or pN stage. Our findings suggest that nodal involvement at time of clinical presentation be not be independently correlated to BCS.
The association between histology and lymph node involvement has been well characterized. For example, patients with the invasive lobular carcinoma have a greater likelihood of having multiple positive lymph nodes (26), and those with tubular carcinoma have significantly less lymph node involvement (16). In the current study, we demonstrated that certain histologic subtypes are more often associated with certain BCS, for example, TN are most often invasive ductal and least likely to be invasive lobular or tubular.
Tumor size, another traditional prognostic feature for outcomes, has been correlated with probability of axillary lymph node involvement, in addition to survival outcomes and recurrence free-survival rates (26–28). For patients with node negative disease, tumor size remains the most important prognostic factor (28). We found a significant association between the BCS of breast cancer and T stage, with TN tumors associated with a larger tumor size compared with other subtypes. Based on these findings, it is theoretically possible that BCS is primarily associated with characteristics of the primary tumor itself, (e.g. tumor size, histology) but not necessarily be involved in the mechanism(s) for lymph node metastasis. Certainly, tumor size is one prognostic factor that has been described to be associated with inferior outcomes observed in women with TN tumors (29).
The association between the BCS and race has been well described in the literature (18, 20, 30). African American patients are known to have an increased likelihood of TN breast cancer (15) as well as inferior overall and disease-free survival (18). Genome-wide classification studies have suggested that differential expression patterns of molecular subtypes which may account for these racial discrepancies in outcomes. The utilization of IHC tumor assessment estimates BCS and is a more practical method for estimating for molecular classification in the clinical setting (36, 18). In addition to confirming the association between BCS and African American women TN tumors that have previously been reported, our findings of larger tumor size is also consistent with the existing literature(15).
To validate the parameters recorded within our database, we conducted a confirmatory outcomes analysis by BCS. The existing literature suggests a significant association between BCS and outcomes (18, 31, 32) with the worst DFS, DMFS and OS for TN subtypes (31, 32). Our findings are consistent with the existing literature in that we demonstrated a similar association between these outcomes and BCS, with TN having worse overall outcomes. However, it is important to note that in the era in which this cohort was treated, treatment with trastuzumab or other targeted therapy for HER-2 was not available for all the patients, and the outcomes in this BCS have significantly improved in the modern treatment era.
While one of the limitations of this study is retrospective use of clinical data and tumor blocks which inevitably is associated with the possibility of selection/inclusion bias and information/misclassification bias. We attempted to overcome some of these limitations by conducting a institutional pathologic review, constructing a TMA so that categorization of the BCS could be done prospectively without intra-observer/inter-observer variability and to avoid misclassification bias, and updating the database parameters and cross-referenced it with our institutional tumor registry data prior to conducting the analysis to decrease information bias. Reassuringly, our outcomes analysis by BCS is consistent with previously published literature (4, 5, 34).
Given the relative scarcity of literature on association of BCS and clinical-pathologic findings at presentation (10, 33), this study contributes to the existing body of literature on molecular subtypes. Our findings demonstrate that BCS is associated with tumor size, method of detection, histology, race and age, but not with the presence or extent of axillary nodal disease.
In summary, in this cohort of early stage breast cancer patients that were uniformly treated with breast conserving surgery, surgical assessment of the axilla and adjuvant radiation therapy, significant differences in outcomes across the four BCS were demonstrated, as expected and as previously described (4, 5). Although a significant association between BCS and nodal involvement was not identified, this study demonstrated a significant association between BCS and primary tumor size, in addition to associations with race, age at diagnosis, method of detection, histology. This information, together with the finding that tumor BCS was predictive of outcomes, intimates that the mechanism(s) resulting in the inferior survival of TN subtype may not be solely mediated through an advanced N stage at diagnosis. Our hypothesis-generating findings contribute to the evolution of disease prognosis using BCS, and warrants further elucidation. If additionally validated, these findings suggest that the BCS of a tumor may not be a useful prognostic variable for influencing regional management considerations.
Figure 2.
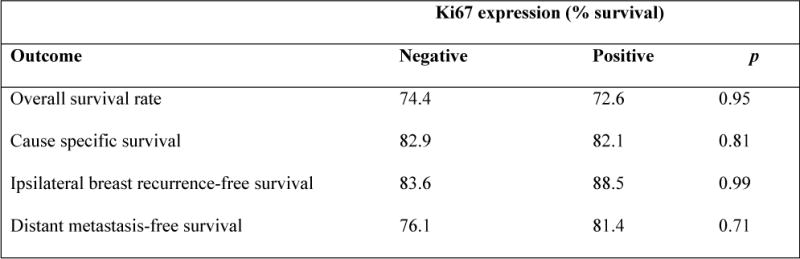
15 year Kaplan-Meier survival probability as a function of Ki67 expression.
Synopsis.
This study classified breast cancer patients into breast cancer subtypes by immunohistochemical analysis of ER/PR/HER2 and determined if there where any significant associations with extent/involvement of nodal metastasis and other clinical-pathologic features at presentation.
Acknowledgments
The authors of this manuscript would like to thank Dr. David Rimm for his assistance with the manuscript and his lab for creation of the tissue micro-array.
This study was partially funded by the Kalimeris Fund (M. S. Moran)
Footnotes
The authors of this manuscript have no conflicts of interest to disclose.
References
- 1.Edge SB, Byrd DR, Compton CC, et al. AJCC Cancer Staging Manual. (7th) 2010 doi: 10.1245/s10434-010-0985-4. [DOI] [PubMed] [Google Scholar]
- 2.Rakha EA, Reis-Filho JS, Baehner F, Dabbs DJ, Decker T, Eusebi V, et al. Breast cancer prognostic classification in the molecular era: The role of histological grade. Breast Cancer Res. 2010;12(4):207. doi: 10.1186/bcr2607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reis-Filho JS, Pusztai L. Gene expression profiling in breast cancer: Classification, prognostication, and prediction. Lancet. 2011 Nov 19;378(9805):1812–23. doi: 10.1016/S0140-6736(11)61539-0. [DOI] [PubMed] [Google Scholar]
- 4.Perou CM, Sorlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, et al. Molecular portraits of human breast tumours. Nature. 2000 Aug 17;406(6797):747–52. doi: 10.1038/35021093. [DOI] [PubMed] [Google Scholar]
- 5.Sorlie T, Tibshirani R, Parker J, Hastie T, Marron JS, Nobel A, et al. Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci U S A. 2003 Jul 8;100(14):8418–23. doi: 10.1073/pnas.0932692100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yi M, Giordano SH, Meric-Bernstam F, Mittendorf EA, Kuerer HM, Hwang RF, et al. Trends in and outcomes from sentinel lymph node biopsy (SLNB) alone vs. SLNB with axillary lymph node dissection for node-positive breast cancer patients: Experience from the SEER database. Ann Surg Oncol. 2010 Oct;17(Suppl 3):343–51. doi: 10.1245/s10434-010-1253-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Giuliano AE, Hunt KK, Ballman KV, Beitsch PD, Whitworth PW, Blumencranz PW, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: A randomized clinical trial. JAMA. 2011 Feb 9;305(6):569–75. doi: 10.1001/jama.2011.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mansel RE, Fallowfield L, Kissin M, Goyal A, Newcombe RG, Dixon JM, et al. Randomized multicenter trial of sentinel node biopsy versus standard axillary treatment in operable breast cancer: The ALMANAC trial. J Natl Cancer Inst. 2006 May 3;98(9):599–609. doi: 10.1093/jnci/djj158. [DOI] [PubMed] [Google Scholar]
- 9.Rugina VG, Mihalcea D, Pricop F. The lymph nodes status–prognostic factor in breast cancer. Rev Med Chir Soc Med Nat Iasi. 2011 Jul-Sep;115(3):839–44. [PubMed] [Google Scholar]
- 10.Reyal F, Rouzier R, Depont-Hazelzet B, Bollet MA, Pierga JY, Alran S, et al. The BCS classification is a determinant of sentinel node positivity in early breast carcinoma. PLoS One. 2011;6(5):e20297. doi: 10.1371/journal.pone.0020297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salhia B, Tapia C, Ishak EA, Gaber S, Berghuis B, Hussain KH, et al. BCS analysis determines the association of advanced breast cancer in egypt with favorable biology. BMC Womens Health. 2011 Sep 30;11:44. doi: 10.1186/1472-6874-11-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Singh Ranger G, Mokbel K. The evolving role of sentinel lymph node biopsy for breast cancer. Eur J Surg Oncol. 2003 Jun;29(5):423–5. doi: 10.1016/s0748-7983(03)00038-6. [DOI] [PubMed] [Google Scholar]
- 13.Parikh RR, Yang Q, Higgins SA, Haffty BG. Outcomes in young women with breast cancer of triple-negative phenotype: The prognostic significance of CK19 expression. Int J Radiat Oncol Biol Phys. 2008 Jan 1;70(1):35–42. doi: 10.1016/j.ijrobp.2007.05.066. [DOI] [PubMed] [Google Scholar]
- 14.Parikh RR, Housman D, Yang Q, Toppmeyer D, Wilson LD, Haffty BG. Prognostic value of triple-negative phenotype at the time of locally recurrent, conservatively treated breast cancer. Int J Radiat Oncol Biol Phys. 2008 Nov 15;72(4):1056–63. doi: 10.1016/j.ijrobp.2008.02.066. [DOI] [PubMed] [Google Scholar]
- 15.Moran BCS, Yang Q, Harris LN, Jones B, Tuck DP, Haffty BG. Long-term outcomes and clinicopathologic differences of african-american versus white patients treated with breast conservation therapy for early-stage breast cancer. Cancer. 2008 Nov 1;113(9):2565–74. doi: 10.1002/cncr.23881. [DOI] [PubMed] [Google Scholar]
- 16.Liu GF, Yang Q, Haffty BG, Moran BCS. Clinical-pathologic features and long-term outcomes of tubular carcinoma of the breast compared with invasive ductal carcinoma treated with breast conservation therapy. Int J Radiat Oncol Biol Phys. 2009 Dec 1;75(5):1304–8. doi: 10.1016/j.ijrobp.2008.12.070. [DOI] [PubMed] [Google Scholar]
- 17.Vargo JA, Beriwal S, Ahrendt GM, Soran A, Johnson RR, McGuire K, et al. Molecular class as a predictor of locoregional and distant recurrence in the neoadjuvant setting for breast cancer. Oncology. 2011;80(5–6):341–9. doi: 10.1159/000330203. [DOI] [PubMed] [Google Scholar]
- 18.Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, et al. Race, breast cancer subtypes, and survival in the carolina breast cancer study. JAMA. 2006 Jun 7;295(21):2492–502. doi: 10.1001/jama.295.21.2492. [DOI] [PubMed] [Google Scholar]
- 19.Bland KI, Scott-Conner CE, Menck H, Winchester DP. Axillary dissection in breast-conserving surgery for stage I and II breast cancer: A national cancer data base study of patterns of omission and implications for survival. J Am Coll Surg. 1999 Jun;188(6):586–95. doi: 10.1016/s1072-7515(99)00056-3. discussion 595–6. [DOI] [PubMed] [Google Scholar]
- 20.Barcenas CH, Wells J, Chong D, French J, Looney SW, Samuel TA. Race as an independent risk factor for breast cancer survival: Breast cancer outcomes from the medical college of georgia tumor registry. Clin Breast Cancer. 2010 Feb;10(1):59–63. doi: 10.3816/CBC.2010.n.008. [DOI] [PubMed] [Google Scholar]
- 21.Crabb SJ, Cheang MC, Leung S, Immonen T, Nielsen TO, Huntsman DD, et al. Basal breast cancer BCS predicts for lower incidence of axillary lymph node metastases in primary breast cancer. Clin Breast Cancer. 2008 Jun;8(3):249–56. doi: 10.3816/CBC.2008.n.028. [DOI] [PubMed] [Google Scholar]
- 22.Van Calster B, Vanden Bempt I, Drijkoningen M, Pochet N, Cheng J, Van Huffel S, et al. Axillary lymph node status of operable breast cancers by combined steroid receptor and HER-2 status: Triple positive tumours are more likely lymph node positive. Breast Cancer Res Treat. 2009 Jan;113(1):181–7. doi: 10.1007/s10549-008-9914-7. [DOI] [PubMed] [Google Scholar]
- 23.Lee JH, Suh YJ, Shim BY, Kim SH. The incidence and predictor of lymph node metastasis for patients with T1mi breast cancer who underwent axillary dissection and breast irradiation: An institutional analysis. Jpn J Clin Oncol. 2011 Oct;41(10):1162–7. doi: 10.1093/jjco/hyr128. [DOI] [PubMed] [Google Scholar]
- 24.Kim MJ, Ro JY, Ahn SH, Kim HH, Kim SB, Gong G. Clinicopathologic significance of the basal-like subtype of breast cancer: A comparison with hormone receptor and Her2/neu-overexpressing phenotypes. Hum Pathol. 2006 Sep;37(9):1217–26. doi: 10.1016/j.humpath.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 25.Liu H, Fan Q, Zhang Z, Li X, Yu H, Meng F. Basal-HER2 phenotype shows poorer survival than basal-like phenotype in hormone receptor-negative invasive breast cancers. Hum Pathol. 2008 Feb;39(2):167–74. doi: 10.1016/j.humpath.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 26.Bortolini M, Genta F, Biacchiardi CP, Zanon E, Camanni M, Deltetto F. Axillary dissection in breast cancer patients with metastatic sentinel node: To do or not to do? suggestions from our series. ISRN Oncol. 2011;2011:527904. doi: 10.5402/2011/527904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hicks DG, Kushner L, McCarthy K. Breast cancer predictive factor testing: The challenges and importance of standardizing tissue handling. J Natl Cancer Inst Monogr. 2011;2011(42):43–5. doi: 10.1093/jncimonographs/lgr003. [DOI] [PubMed] [Google Scholar]
- 28.Edge SB, Compton CC. The american joint committee on cancer: The 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010 Jun;17(6):1471–4. doi: 10.1245/s10434-010-0985-4. [DOI] [PubMed] [Google Scholar]
- 29.Anders CK, Deal AM, Miller CR, Khorram C, Meng H, Burrows E, et al. The prognostic contribution of clinical breast cancer subtype, age, and race among patients with breast cancer brain metastases. Cancer. 2011 Apr 15;117(8):1602–11. doi: 10.1002/cncr.25746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kurian AW, Fish K, Shema SJ, Clarke CA. Lifetime risks of specific breast cancer subtypes among women in four racial/ethnic groups. Breast Cancer Res. 2010;12(6):R99. doi: 10.1186/bcr2780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dawood S, Ueno NT, Valero V, Woodward WA, Buchholz TA, Hortobagyi GN, et al. Differences in survival among women with stage III inflammatory and noninflammatory locally advanced breast cancer appear early: A large population-based study. Cancer. 2011 May 1;117(9):1819–26. doi: 10.1002/cncr.25682. [DOI] [PubMed] [Google Scholar]
- 32.Dawood S, Hu R, Homes MD, Collins LC, Schnitt SJ, Connolly J, et al. Defining breast cancer prognosis based on molecular phenotypes: Results from a large cohort study. Breast Cancer Res Treat. 2011 Feb;126(1):185–92. doi: 10.1007/s10549-010-1113-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Demirci S, Broadwater G, Marks LB, Clough R, Prosnitz LR. Breast conservation therapy: The influence of BCS and margins. Int J Radiat Oncol Biol Phys. 2011 Dec 28; doi: 10.1016/j.ijrobp.2011.09.001. [DOI] [PubMed] [Google Scholar]
- 34.Calza S, Hall P, Auer G, Bjohle J, Klaar S, Kronenwett U, et al. Intrinsic molecular signature of breast cancer in a population-based cohort of 412 patients. Breast Cancer Res. 2006;8(4):R34. doi: 10.1186/bcr1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Camp RL, Charette LA, Rimm D. Validation of tissue microarray technology in breast carcinoma. Lab Invest. 2000;80(12):1943–1949. doi: 10.1038/labinvest.3780204. [DOI] [PubMed] [Google Scholar]
- 36.Nielsen T, Hsu F, Jensen K, et al. Immunohistochemical and clinical characterization of the basal-like subtype of invasive breast carcinoma. Clin Cancer Res. 2004;10:5367–5374. doi: 10.1158/1078-0432.CCR-04-0220. [DOI] [PubMed] [Google Scholar]


