Abstract
This study examines the impact of maternal depression on reductions in children’s behavior problems severity following implementation of the Brief Behavioral Intervention—a brief, manualized parent management training treatment. The parents of 87 children aged 2–6 years of age received parent management training at a metropolitan hospital. Parents of participants completed measures of externalizing behavior and maternal depression. The association between pre-post treatment change in externalizing behavior and maternal depression was examined using an autoregressive cross-lagged model. Results showed that self-reported maternal depressive symptoms at pre-treatment negatively influenced the overall magnitude of reduction of reported externalizing behaviors in children following treatment. Results indicate that aspects of family functioning not specifically targeted by parent management training, such as maternal depression, significantly affect treatment outcomes. Clinicians providing parent management training may benefit from assessing for maternal depression and modifying treatment as indicated.
Keywords: Treatment outcome, Parent management training, Externalizing, Maternal depression, Brief behavioral intervention
Maternal Depression and Parent Management Training Outcomes
Parent management training (PMT) is considered a best practice in the treatment of disruptive behaviors in young children. Factors affecting the treatment outcomes of PMT are under-researched, however, limiting our understanding of the circumstances under which such treatments produce optimal results (Eyberg, Nelson, & Boggs, 2008).
Due to the indirect nature of the PMT intervention–the therapist largely works on modification of parent behaviors, which in turn modifies child behavior–both parent and child factors may influence intervention efficacy. The most well-studied child-level predictor of treatment outcomes in PMT is the severity of child psychopathology at pretreatment. This variable has a moderate negative association with response to treatment and is the strongest known predictor of treatment outcome aside from poverty (see Reyno & McGrath, 2006).
The impact of maternal psychopathology, particularly maternal depression, on PMT is less clear. Maternal depression negatively influences parenting behavior (Jackson, Brooks-Gunn, Huang, & Glassman, 2000; Querido, Eyberg, & Boggs, 2001) and may cause parents to perceive their children’s behavior in a more negative fashion (Griest, Wells, & Forehand, 1979; but see Querido et al., 2001). Additionally, high task demands are involved in PMT (e.g., consistent implementation of behavior modification techniques in the home) and there is a large body of literature supporting the role of depression in causing task impairment (Heiligenstein, Guenther, Hsu, & Herman, 1996; Mintz, Mintz, Arruda, & Hwang, 1992). Unfortunately, few studies have compared the intervention efficacy of standard PMT to a PMT program containing adjunctive psychotherapeutic treatment of maternal depression symptoms (Chronis, Chacko, Fabiano, Wymbs, & Pelham, 2004) likely due to the time and cost involved in conducting such research. As of 2013, Chronis-Tuscano et al. (2013) were writing of the development and preliminary evaluation of such an integrated program. The recency of such efforts is notable given far earlier attempts to create such a program (e.g., Sanders & McFarland, 2001; Webster-Stratton, 1994).
This time lag is easier to understand given the significant heterogeneity in the results of the relatively few studies attempting to determine whether maternal depression significantly influences the outcome of standard PMT, i.e., PMT that does not include concurrent treatment of parental depression. A further examination of this heterogeneity suggests that the differences between positive and negative findings among these studies was related to how treatment outcome was defined.
Specifically, studies which dichotomized treatment outcome on the basis of clinical cut-offs all reported a significant association between maternal depression and treatment response (Kazdin, 1995; Webster-Stratton, 1990; 1992). These studies categorized individuals as responsive or non-responsive to treatment largely dependent on whether their post-treatment scores fell within the normal range on a standardized behavior rating scale (all participants displayed elevated scores at pre-treatment). While of clinical significance, however, measuring therapeutic change in this manner loses the descriptive richness of a continuous measure. For example, a participant with a score changing only. Ten standard deviations to fall within the normal range at post-treatment could be placed in the same category as a participant with a score change of over one standard deviation.
All attempts to relate the magnitude of clinical change to maternal depression, however, have yielded non-significant results (Beauchaine, Webster-Stratton, & Reid, 2005; Hartman, Stage, & Webster-Stratton, 2003; Kazdin & Whitely, 2006; Webster-Stratton & Hammond, 1990). Specifically, Kazdin and Whitely (2006) found that maternal depression scores did not differ between high or low treatment responders, a dichotomous outcome measure based on a median split of a continuous measure of therapeutic change rather than clinical cut-off scores. The studies of Beauchaine et al. (2005), Hartman et al. (2003), and Webster-Stratton and Hammond (1990) all attempted to relate maternal depression to treatment outcome using a continuous rather than dichotomous measure of therapeutic change. Unfortunately, all three differed in their conceptualization of treatment outcomes from the studies of Kazdin (1995) and Webster-Stratton (1990, 1992) in ways other than the use of continuous measure of change. Specifically, the latter authors conceptualized treatment outcome as consisting of change between two time-points (pre-treatment and post-treatment). Beauchaine et al. (2005) and Hartman et al. (2003), however, used change among three time points (pre-treatment, posttreatment, and one-year follow-up) to represent therapeutic change, whereas Webster-Stratton and Hammond’s (1990) treatment outcome measure contained a single time point (post-treatment score).
In summary, review of the research yields the following contradictory finding: maternal depression is significantly related to the clinical significance (as defined by clinical cut-offs) but not the magnitude of therapeutic change following PMT. However, the non-significant associations between maternal outcome and therapeutic change may have resulted from methodological differences between studies beyond the decision to measure the magnitude rather than clinical significance of change. Thus, to determine whether maternal depression influences the magnitude as well as the clinical significance of pre-post treatment change in conduct problems resulting from PMT, research is needed in which change between these two time points is treated as a continuous rather than dichotomous variable. Therefore, the purpose of the present study is to examine whether maternal depression is a significant predictor of PMT treatment outcome as defined by a continuous variable. The results will aid in clarifying the inconclusive research literature regarding the viability of parental depression as a predictor of PMT outcomes, and inform clinicians regarding parent-level factors that should be assessed prior to treatment.
Methods
Participants and Procedures
Participants were caregivers of at least one child presenting with externalizing behavior problems who had been referred for PMT at an outpatient clinic of a large children’s hospital. Inclusion criteria for the study included a T-score of 60 or higher on the intensity scale of the Eyberg Child Behavior Inventory (ECBI) and child age less than 6.5 years. Families were excluded from participation if children presented with one or more significant medical health impairments capable of affecting behavior (e.g., seizure disorder, premature birth prior to 30 weeks gestation) or severe receptive language disorder. Institutional Review Board approval was obtained from the institution and informed consent was obtained from caregivers whose child met criteria to participate in the treatment; caregivers were provided an explanation of the study and the choice to participate. Only three caregivers declined participation.
Analyses conducted for the current study were restricted to participants who completed the treatment protocol and returned post-treatment measures. Of the initial 157 participants, 137 participants completed the treatment with drop out defined as attending less than 4 of the core intervention sessions (see below). Post-intervention data was not collected from patients that dropped out of treatment. Independent samples t-tests and Chi square analyses were conducted to examine pre-intervention differences between intervention completers and dropouts in parent education, child gender, race/ethnicity, medication status, age, and scores on the two variables examined in the current evaluation. Findings revealed a higher proportion of parents with a college education or higher among participants completing the intervention (57.5 %) compared to participants who dropped out (26.3 %), χ2 = 16.59, p < .01. Other comparisons were nonsignficant.
Of the treatment completers, 87 participants returned post-intervention measures. There were no pre-intervention differences between intervention completers who returned the post-intervention measures and those who did not return the measures.
Among the 87 participants returning post-intervention measures, all caregivers participating in the study were female and educational background of the caregivers was varied: 1.2 % had not graduated from high school, 19.0 % high school graduates, 20.2 % some college, 34.5 % college graduates, and 25.0 % had obtained a post-graduate degree. The mean number of sessions attended was 6.8 with a range from 4 to 16 sessions.
Children in the sample were primarily male (83.9 %) and the mean child age at the first session of treatment was 4.75 years (SD = 11.3 months) with a range of 2.67–6.5 years of age. Racial background of the participating children was 15.1 % Hispanic, 5.8 % African-American, 1.2 % Asian or Pacific Islander, 72.1 % European American, and 5.8 % other/bi-racial. The majority of these children had diagnoses of either Disruptive Behavior Disorder-Not Otherwise Specified (DBD-NOS; 66.3 %) or Attention Deficit/Hyperactivity Disorder—Combined Type (ADHD; 18.6 %). The remaining children in the sample had received diagnoses of either Oppositional Defiant Disorder (ODD; 8.1 %) or ADHD and ODD (7.0 %). At the onset of treatment, six children were taking some form of medication for the management of behavior. During the course of treatment, twelve previously medication-naïve children started medication.
Assessment
Participants completed the Behavior Assessment System for Children, Second Edition (BASC-2; Reynolds & Kamphaus, 2004) and the Parenting Stress Index (PSI; Abidin, 1995) before and after treatment; demographic information forms were completed before treatment. The current study used the parent report form of the BASC-2 to assess child behavior.
The BASC-2 is a broad-band, norm-reference measure of behavioral, social, and emotional functioning in children. In the current study, the Externalizing Problems scale was used to indicate the degree of child engagement in oppositional, disruptive, and aggressive behaviors. This scale has been widely used for this purpose, including in other studies of PMT (e.g., Nieter, Thornberry, & Brestan-Knight, 2013). Sample items on this composite scale include: “throws tantrums” and “loses temper too easily.” Respondents indicate the frequency with which their children display these behaviors. Raw scores on this scale were converted to T-scores using the age-appropriate, same-sex, general norm sample. T-scores of 70 and above are considered “clinically significant” and T-scores between 60 and 69 are designated “at risk.” Because the scores on this measure were norm-referenced, it was unnecessary to control for child age in analyses. The psychometric properties of this scale include an intraclass coefficient ranging from .95 to .97 depending on age and a test–retest reliability ranging from .86 to .90 (Reynolds & Kamphaus, 2004).
The PSI is a questionnaire designed to measure stress in the parent–child system and consists of multiple sub-scales. Maternal depressive symptoms were measured using the 9-item parental depression scale of the PSI. According to the PSI manual, items from this scale are similar to other measures designed to assess depression. Items (e.g., “I am unhappy with the last purchase of clothing I made for myself” and “quite a few things bother me”) are scored on a five-point Likert-scale ranging from 1 = strongly disagree = to 6 = strongly agree. Total scores are found by summing items endorsed. Reliability for this scale is adequate (α = .84). Raw scores above 26 are considered elevated.
Treatment
The brief behavioral intervention (BBI) program is a manualized PMT program aimed at treatment of disruptive behavior among preschoolers. The intervention was designed specifically to have fewer sessions to limit treatment attrition associated with attending many repeated sessions. It was also designed to be easily implemented in hospital clinics and outpatient settings.
BBI consists of five core sessions, each focused on a specific behavioral management skill: exploring daily routines to help parents identify antecedents and consequences of problem behavior, and how to make schedule adjustments; parent provision of child–directed play; providing differential attention; delivering effective commands; and administration of consequences, including timeout. Sessions last from 45-min to 1-h, and there is one session per week. Participants have opportunity to attend a booster session or to repeat sessions. BBI has demonstrated feasibility in clinical settings (Axelrad, Garland, & Love, 2009) and effective outcomes across a large pilot sample (Axelrad, Butler, Dempsey, & Chapman, 2013).
Advanced psychology graduate students and postdoctoral fellows conducted the intervention. Each family worked with an individual clinician. Prior to delivering the intervention, all clinicians demonstrated competent delivery of the intervention during a standardized checkout procedure for each core session. A licensed clinical psychologist or postdoctoral fellow with at least 1 year of experience in the program provided live supervision to all clinicians to ensure treatment fidelity, with clinicians required to take a 2–5 min break halfway through each session to receive progress monitoring feedback.
Statistical Analysis
An autoregressive cross-lagged model was used to examine the reciprocal relationship between maternal depressive symptoms and externalizing behaviors in children. The auto-regressive cross-lagged model was used to examine the structural relations between two or more variables that are measured two or more times. The model is a path model, which is technically a special case of structural equation model where there is no measurement model, rather only a structural model. For the current study, we used a two wave, two variable model, which is expressed in two equations:
| (1) |
| (2) |
In these equations, the β1 and β3 terms correspond to the autoregressive effects and describe the stability of the constructs from one time to another (Selig & Little, 2011). Whereas the terms β2 and β4 correspond to the cross-lagged effects, or the residualized change parameter. Using the terms in the equation, this is the effect of X1 and Y1 on a residualized Y2 and X2, respectively. In this way, it is the unique effect of a predictor on the outcome, controlling for prior levels of the outcome, thus ruling out correlations between prior levels of the outcomes as a plausible explanation for observed effects. In other words, using this analysis it could be determined whether maternal depressive symptoms significantly predicted variability in reported externalizing problems at post-treatment while controlling for the influence of pre-treatment externalizing problems.
Full information maximum likelihood (FIML) was used to handle missing data, which Enders and Bandalos (2001) found to be superior to other methods of missing data in structural equation models in parameter bias, efficiency, and Type I error rates. This method accounts for missing data on dependent, but not independent variables. As six of the 87 families that returned post-treatment data had missing pre-treatment data on maternal depressive symptoms and child externalizing problems, the autoregressive cross-lagged model included 81 observations.
Results
Sample Characteristics
Table 1 presents the means and the standard deviation of the targeted scales of the PSI and BASC-2 for the 81 observations included in the autoregressive cross-lagged model. Briefly, parent ratings of their child averaged two standard deviations above the mean on the BASC-2 measure of externalizing behaviors (T-score of 71.2) before starting treatment. Following treatment, study participants averaged one standard deviation above the mean on this measure (T-score of 61.3). Of the 87 participants returning post-treatment measures, 85 had no missing data on pre- and post-treatment BASC-2 Externalizing Problems scales and 77 had no missing data on the parental depression scale of the PSI. Paired-sample t tests conducted on these pre- and post-treatment measures confirm that the average scores on the BASC-2 Externalizing Problems scale significantly decreased following the intervention, t(84) = 7.93, p < .001, d = .86, as did average scores on the parental depression scale of the PSI, t(76) = 5.80, p < .001, d = .66.
Table 1.
Means, standard deviations, and correlation matrix for measures
| Variable | Mean (SD) | MDS-T1 | CEP-T1 | MDS-T2 | CEP-T2 |
|---|---|---|---|---|---|
| MDS-T1 | 20.93 (5.9) | – | −.10 | .72* | .20 |
| CEP-T1 | 71.22 (11.2) | – | .00 | .55* | |
| MDS-T2 | 18.20 (5.2) | – | .20 | ||
| CEP-T2 | 61.28 (11.3) | – |
MDS maternal depressive symptoms, CEP child externalizing problems, T1 Time 1, T2 Time 2
p < .001
Treatment Gains and Maternal Depressive Symptoms
We fit the autoregressive cross-lagged model to test the reciprocal relations between maternal depressive symptoms and child problem behavior. The parameter estimates obtained from this model are presented in Fig. 1, and expressed in terms from Equations 1 and 2. Results demonstrated a significant relation between pre-and post-scores in both areas, β1 = .63(SE = .071), t = 8.93, p < .05, for depressive symptoms; β3 = .59(SE = .09), t = 6.68, p < .05, for externalizing behaviors. Regarding cross-lagged path coefficients, we found that only pretreatment maternal depressive symptoms influenced post-treatment report of externalizing problems. That is, controlling for the influence of pre-treatment externalizing problems, maternal depressive symptoms appears to significantly predict residualized variability in reported externalizing problems at post-treatment, β4 = .47(SE = .17), t = 2.80, p < .05. This influence did not appear to be reciprocal; levels of reported child externalizing problems at pre-treatment did not predict variability on post-treatment maternal report of depressive symptoms, β2 = .03(SE = .04), t = .87, p = .38.
Fig. 1.
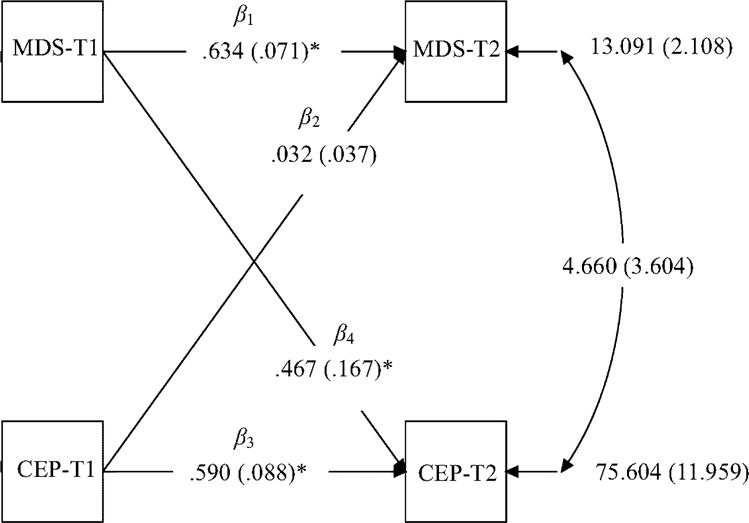
Standardized solution of the autoregressive cross-lagged model with cross-time links between child externalizing problems and symptoms of maternal depression. SE are shown in parentheses. MDS maternal depressive symptoms, CEP child externalizing problems, T1 Time 1, T2 Time 2. *p < .05
Discussion
The limited clinical significance of previous research demonstrating a negative association between maternal depressive symptoms and therapeutic change in PMT was due to change being defined by whether a child’s level of problem behavior fell below a specific cut-score on a standardized post-treatment measure (Kazdin, 1995; Webster-Stratton 1990; 1992). The current findings extend this research by showing that self-reported maternal depressive symptoms negatively influence the overall magnitude of therapeutic change without regard to predefined cut-offs and that this influence did not appear to be reciprocal, i.e., levels of reported childhood externalizing problems at pretreatment did not predict variability on post-treatment maternal self-reported depressive symptoms ratings. That is, compared to mothers reporting fewer depressive symptoms, mothers reporting higher levels of depressive symptoms reported less therapeutic change in their child, and this was true regardless of whether mothers’ post-treatment reports of level of child behavior problems was high or low.
The current study also extends the literature on maternal depressive symptoms and PMT outcomes as it indicates that the negative association between the two variables can be found across a variety of PMT programs. Specifically, the PMT program used in the current study differs from other PMT programs (Kazdin, 1995; Webster-Stratton, 1990; 1992) in which significant relations between these variables were observed. That is, the BBI program is conducted in a more usual care environment (insurance is billed for treatment) than the studies just cited. Additionally, unlike treatments used in Webster-Stratton (1990, 1992), the BBI program does not make use of video modeling and there is no peer-group component to the intervention. Thus, the heterogeneity of PMT programs in which a negative association between maternal depressive symptoms and therapeutic change has been observed suggests that this association generalizes across PMT programs.
Currently, it is unknown whether maternal depressive symptoms influences treatment effectiveness through a mechanism of understanding or application. That is, the learning/memory impairments (Burt, Zembar, & Niederehe, 1995) associated with depression may negatively impact treatment outcomes by hindering the parent’s initial acquisition of the intervention concepts (e.g., the role of attention), resulting in poor intervention integrity. Alternatively, task performance deficits associated with depression (Wang et al., 2004) may impede the parent’s implementation of the intervention components. Thus, future research should examine whether the negative influence of depression on PMT outcomes occurs through acquisition impairments, performance impairments, both, or an entirely different mechanism. This information could aid in the development and modification of PMT for use with depressed parents.
Although 87 % of participants completed the intervention, less than 50 % of enrolled subjects returned post-intervention materials. This return rate represents a limitation of the current study. To address this issue, it may be necessary to provide participant reimbursement for completion of post-intervention measures.
Another limitation of this study is the use of only one measure of depression. Additionally, future research in this area should include direct examination of correlates of depression such as attentional difficulties as this information will be useful in identifying factors mediating the link between maternal depressive symptoms and PMT outcomes. Another limitation of the study is its reliance on maternal report to measure child conduct problems, as maternal depressive symptoms may have led to the inflation of reported child conduct problems (i.e., the depression-distortion hypothesis; Gartstein, Bridgett, Dishion, & Kaufman, 2009). Future research should seek to replicate the findings of the current study using direct observational measures of child conduct problems. Future research studies would also benefit from the inclusion of direct and indirect measures of family functioning. Despite these limitations, however, the findings of the current study suggest possible modifications to existing practices in PMT. That is, assessment of maternal depressive symptoms could aid in the identification of families who may obtain greater therapeutic benefit from PMT if the parent receives treatment (e.g., parent-centered psychotherapy) aimed at reducing depressive symptoms prior to or concurrent with the course of PMT.
Acknowledgments
We would like to thank the families that participated in this study.
Footnotes
Compliance with Ethical Standards
Conflict of Interest Jack Dempsey, Samuel McQuillin, Ashley M. Butler, and Marni E. Axelrad declare they have no conflict of interest.
Human and Animal Rights and Informed Consent All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
References
- Abidin RR. Parenting stress index. 3rd. Charlottesville, VA: Pediatric Psychology Press; 1995. [Google Scholar]
- Axelrad M, Butler A, Dempsey J, Chapman S. Treatment effectiveness of a brief behavioral intervention for preschool disruptive behavior. Journal of Clinical Psychology in Medical Settings. 2013;20(3):323–332. doi: 10.1007/s10880-013-9359-y. [DOI] [PubMed] [Google Scholar]
- Axelrad ME, Garland BH, Love KB. Brief behavioral intervention for young children with disruptive behaviors. Journal of Clinical Psychology in Medical Settings. 2009;16(3):263–269. doi: 10.1007/s10880-009-9166-7. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Webster-Stratton C, Reid M. Mediators, moderators, and predictors of 1-year outcomes among children treated for early-onset conduct problems: A latent growth curve analysis. Journal of Consulting and Clinical Psychology. 2005;73(3):371–388. doi: 10.1037/0022-006X.73.3.371. [DOI] [PubMed] [Google Scholar]
- Burt D, Zembar M, Niederehe G. Depression and memory impairment: A meta-analysis of the association, its pattern, and specificity. Psychological Bulletin. 1995;117(2):285–305. doi: 10.1037/0033-2909.117.2.285. [DOI] [PubMed] [Google Scholar]
- Chronis AM, Chacko A, Fabiano GA, Wymbs BT, Pelham WE., Jr Enhancements to the behavioral parent training paradigm for families of children with ADHD: Review and future directions. Clinical Child and Family Psychology Review. 2004;7(1):1–27. doi: 10.1023/b:ccfp.0000020190.60808.a4. [DOI] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Clarke TL, O’Brien KA, Raggi VL, Diaz Y, Mintz AD, Thomas SR. Development and preliminary evaluation of an integrated treatment targeting parenting and depressive symptoms in mothers of children with attention-deficit/hyperactivity disorder. Journal of consulting and clinical psychology. 2013;81(5):918. doi: 10.1037/a0032112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders CK, Bandalos DL. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling. 2001;8(3):430–457. doi: 10.1207/S15328007SEM0803_5. [DOI] [Google Scholar]
- Eyberg SM, Nelson MM, Boggs SR. Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. Journal of Clinical Child and Adolescent Psychology. 2008;37(1):215–237. doi: 10.1080/15374410701820117. [DOI] [PubMed] [Google Scholar]
- Gartstein MA, Bridgett DJ, Dishion TJ, Kaufman NK. Depressed mood and maternal report of child behavior problems: Another look at the depression–distortion hypothesis. Journal of Applied Developmental Psychology. 2009;30(2):149–160. doi: 10.1016/j.appdev.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griest D, Wells KC, Forehand R. An examination of predictors of maternal perceptions of maladjustment in clinic-referred children. Journal of Abnormal Psychology. 1979;88:277–281. doi: 10.1037/0021-843X.88.3.277. [DOI] [PubMed] [Google Scholar]
- Hartman RR, Stage SA, Webster-Stratton C. A growth curve analysis of parent training outcomes: Examining the influence of child risk factors (inattention, impulsivity, and hyperactivity problems), parental and family risk factors. Journal of Child Psychology and Psychiatry. 2003;44(3):388–398. doi: 10.1111/1469-7610.00129. [DOI] [PubMed] [Google Scholar]
- Heiligenstein E, Guenther G, Hsu K, Herman K. Depression and academic impairment in college students. Journal of American College Health. 1996;45(2):59–64. doi: 10.1080/07448481.1996.9936863. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Child, parent and family dysfunction as predictors of outcome in cognitive-behavioral treatment of antisocial children. Behaviour Research and Therapy. 1995;33(3):271–281. doi: 10.1016/0005-7967(94)00053-M. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Whitley MK. Comorbidity, case complexity, and effects of evidence-based treatment for children referred for disruptive behavior. Journal of Consulting and Clinical Psychology. 2006;74(3):455–467. doi: 10.1037/0022-006X.74.3.455. [DOI] [PubMed] [Google Scholar]
- Mintz J, Mintz LI, Arruda MJ, Hwang S. Treatments of depression and the functional capacity to work. Archives of General Psychiatry. 1992;49(10):761–768. doi: 10.1001/archpsyc.1992.01820100005001. [DOI] [PubMed] [Google Scholar]
- Nieter L, Thornberry T, Jr, Brestan-Knight E. The effectiveness of group parent–child interaction therapy with community families. Journal of Child and Family Studies. 2013;22(4):490–501. doi: 10.1007/s10826-012-9601-5. [DOI] [Google Scholar]
- Reyno SM, McGrath PJ. Predictors of parent training efficacy for child externalizing behavior problem–a meta-analytic review. Journal of Child Psychology and Psychiatry. 2006;47(1):99–111. doi: 10.1111/j.1469-7610.2005.01544.x. [DOI] [PubMed] [Google Scholar]
- Reynolds CR, Kamphaus RW. Behavior assessment system for children. 2nd. Circle Pines, MN: American Guidance Service Inc; 2004. [Google Scholar]
- Sanders MR, McFarland M. Treatment of depressed mothers with disruptive children: A controlled evaluation of cognitive behavioral family intervention. Behavior Therapy. 2001;31:89–112. [Google Scholar]
- Selig JP, Little TD. Autoregressive and cross-lagged panel analysis. In: Laursen B, Little TD, Card NA, editors. Handbook of developmental research methods. New York: Guildford Press; 2011. pp. 265–278. [Google Scholar]
- Wang PS, Beck AL, Berglund P, McKenas DK, Pronk NP, Simon GE, Kessler RC. Effects of major depression on moment-in-time work performance. The American Journal of Psychiatry. 2004;161(10):1885–1891. doi: 10.1176/appi.ajp.161.10.1885. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C. Long-term follow-up of families with young conduct problem children: From preschool to grade school. Journal of Clinical Child Psychology. 1990;19(2):144. [Google Scholar]
- Webster-Stratton C. Individually administered videotape parent training: Who benefits? Cognitive Therapy and Research. 1992;16:31–52. [Google Scholar]
- Webster-Stratton C. Advancing videotape parent training: A comparison study. Journal of Consulting and Clinical Psychology. 1994;62(3):583–593. doi: 10.1037//0022-006x.62.3.583. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C, Hammond M. Predictors of treatment outcome in parent training for families with conduct problem children. Behavior Therapy. 1990;21:319–337. [Google Scholar]


