Abstract
Anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitides (AAV) are rare diseases characterized by a necrotizing small-vessel vasculitis and circulating ANCA that comprise granulomatosis with polyangiitis, microscopic polyangiitis, and eosinophilic granulomatosis with polyangiitis (EGPA). Acute ischemic stroke (AIS) can be a manifestation of central nervous system (CNS) involvement in these diseases. Furthermore, intracerebral hemorrhage (ICH) is a potential complication of these necrotizing vasculitides. We describe a case of AAV who presented with acute ischemic stroke and developed multiple ICHs after administration of IV tPA. We propose that patients with AAV are more prone to develop hemorrhage in the presence of IV tPA and discuss the possible underlying pathogenesis. We suggest that AAV should be considered a contraindication for administration of IV tPA.
Keywords: ANCA associated vasculitis, Intracerebral hemorrhage, Ischemic stroke, IV tPA
Highlights
-
•
ANCA-associated vasculitides (AAV) can present with acute ischemic stroke.
-
•
Intracerebral hemorrhage is a potential complication of AAV.
-
•
IV tPA can increase risk of ICH in patients with AAV.
-
•
AAV could be a relative contraindication for administration of IV tPA.
1. Introduction
Anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitides (AAV) are rare diseases, characterized by a necrotizing small-vessel vasculitis and circulating ANCA that comprise granulomatosis with polyangiitis, microscopic polyangiitis, and eosinophilic granulomatosis with polyangiitis (EGPA). Acute ischemic stroke (AIS) can be a manifestation of central nervous system (CNS) involvement [1]. In addition, intracerebral hemorrhage (ICH) is a potential complication of these necrotizing vasculitides [2]. Intravenous tissue plasminogen activator (IV tPA) is the standard treatment for AIS. Vasculitides are not listed as contraindications for its administration [3]. However, CNS vasculitis could be a contraindication to IV tPA because the risk of ICH. We describe a patient who developed multiple ICHs following IV tPA administration for AIS. The stroke was the initial presentation of AAV. We raise awareness to the dangers of IV tPA use in patients with AAV.
2. Case report
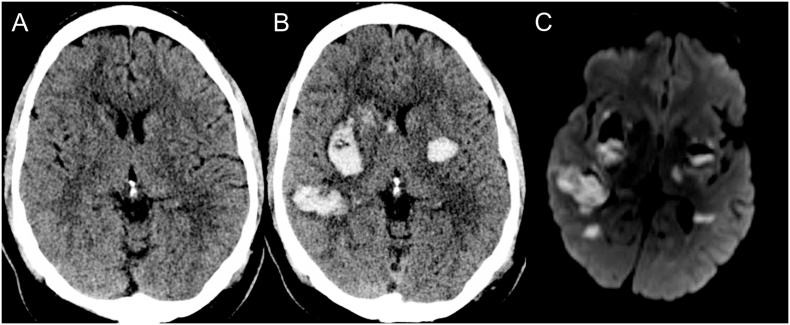
A 58-year-old man was admitted for myalgia, night sweats, low grade fevers, dark urine and urticarial rash over his trunk and extremities that progressed over two weeks. Twelve hours later, he developed acute right hemiparesis, dysarthria and right facial droop; his National Institutes of Health Stroke Scale (NIHSS) score was 4. Initial evaluation, including computed tomography (CT) scan, did not identify any contraindication and IV tPA was administered at 71 min after symptom onset (Fig. 1A). His symptoms initially resolved with IV tPA but shortly afterward he deteriorated with decreased level of arousal and required intubation. A second CT scan showed multiple bilateral ICHs (Fig. 1B). Magnetic resonance (MR) imaging showed restricted diffusion in the left internal capsule, corresponding to his presenting stroke in addition to multiple other scattered punctate strokes bilaterally (Fig. 1C).
Fig. 1.
Radiographic Findings. (A) Axial computed tomography (CT) brain without contrast prior to intravenous tissue plasminogen activator (IV tPA) negative for intracranial hemorrhage (ICH). (B) Axial CT brain without contrast after IV tPA showing ICH in the left and right putamen, right caudate head and right temporal lobe. (C) Axial diffusion weighted magnetic resonance imaging showing acute ischemic stroke (AIS) bilaterally. Also, multiple other punctate AIS in the left cerebellum, left frontal lobe and right mesial temporal lobe (not shown).
Admission labs showed elevated erythrocyte sedimentation rate (51 mm/h) and C-reactive protein (22.5 mg/dL), leukocytosis (11,500/mm3) and normal renal function. Work up revealed a very high C-ANCA (1:2560) and proteinase 3 antibody titers (> 8.0, reference: 0.0–0.3 AI), whereas myeloperoxidase antibody was negative. Dysmorphic red blood cells were identified on urine microscopy. Head and neck MR angiography, cardiac telemetry, and transesophageal echocardiogram were unremarkable, and blood cultures were negative. A diagnosis of C-ANCA-associated vasculitis was made and treatment was started with corticosteroids and rituximab. His course was complicated by renal failure, attributed to his vasculitis. He was discharged to an inpatient rehabilitation facility with marked neurological and renal improvement at 3 month follow up. His modified Rankin Scale was 3.
3. Discussion
Our case illustrates that AIS may be part of the initial presentation of AAV. If AIS is accompanied by systemic symptoms suggestive of a multisystem vasculitis, one should proceed with caution. In our patient, the diagnosis was not initially suspected. We treated the patient with IV tPA and subsequently multiple hemorrhages not reflecting the area of AIS developed. Because of the multiple hemorrhages, which may not have been secondary to acute ischemia, we evaluated him for a multisystem vasculitis including AAV. Subsequently, the elevated inflammatory markers, the C-ANCA titer, and positive proteinase 3 antibody led to the diagnosis of AAV. Thereafter, the renal and cutaneous manifestations of AAV became apparent. Our patient received immunosuppressive treatment with marked improvement in his non-neurological clinical features strengthening support for that diagnosis.
CNS involvement is rare in AAV and it usually develops as a delayed phase of the disease after onset of systemic symptoms. On occasion, it can be the initial manifestation of the disease, presenting as headache, cranial nerve palsy, seizures, altered mental status, coma, AIS and ICH [2]. Post-mortem exams in these patients have demonstrated AIS with areas of antemortem thrombi and fibrinoid changes with other areas demonstrating damaged vessels with hemorrhage [4]. We believe that in the presence of IV tPA, areas of fibrinoid necrosis are likely to make the patient more prone to hemorrhagic transformation particularly at sites of subclinical ischemia which may not be apparent on the initial non-contrast CT.
Fattahi et al. reported a patient with poorly controlled chronic EGPA who was treated with IV tPA for an AIS and developed a large ICH [5]. They proposed that IV tPA should be considered a relative contraindication in patients with AAV. Our experience with this case further supports their proposal with added caution to include patients who are still within their acute presentation of systemic vasculitis.
4. Conclusion
The risk of hemorrhage following IV tPA administration for treatment of AIS secondary to CNS involvement of AAV is not known and currently, AAV is not listed among the contraindications for IV tPA in guidelines [3]. Our case highlights the high risk of ICH associated with AAV and reinforces that IV tPA may be contraindicated in these patients.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Acknowledgments
Acknowledgments
If accepted to Open Access publication the fee will be funded by the University of Iowa.
Contributor Information
Neda Zarghami Esfahani, Email: neda-esfahani@uiowa.edu.
Daniel M. Anderson, Email: daniel-m-anderson@uiowa.edu.
Connie Pieper, Email: connie-pieper@uiowa.edu.
Harold P. Adams, Jr., Email: harold-adams@uiowa.edu.
References
- 1.Nishino H., Rubino F.A., DeRemee R.A. Neurological involvement in Wegener's granulomatosis: an analysis of 324 consecutive patients at the Mayo Clinic. Ann Neurol. 1993;33:4–9. doi: 10.1002/ana.410330103. [DOI] [PubMed] [Google Scholar]
- 2.Ghinoi A., Zuccoli G., Pipitone N. Anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis involving the central nervous system: case report and review of the literature. Clin. Exp. Rheumatol. 2010 Sep–Oct;28(5):759–766. [PubMed] [Google Scholar]
- 3.Jauch E.C., Saver J.L., Adams H.P. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870–947. doi: 10.1161/STR.0b013e318284056a. [DOI] [PubMed] [Google Scholar]
- 4.Drachman D.A. Neurological complications of Wegener's granulomatosis. Arch Neurol. 1963;8:145–155. [Google Scholar]
- 5.Fattahi P., Sheriff F., Narayanan N.S. Thrombolysis for acute stroke in patients with vasculitis: case report and literature discussion. Clin Neurol Neurosurg. 2013 doi: 10.1016/j.clineuro.2012.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]